Thromboprophylaxis in Head and Neck Microvascular Reconstruction
Abstract
:Methods
Results
Mechanical Methods
Aspirin
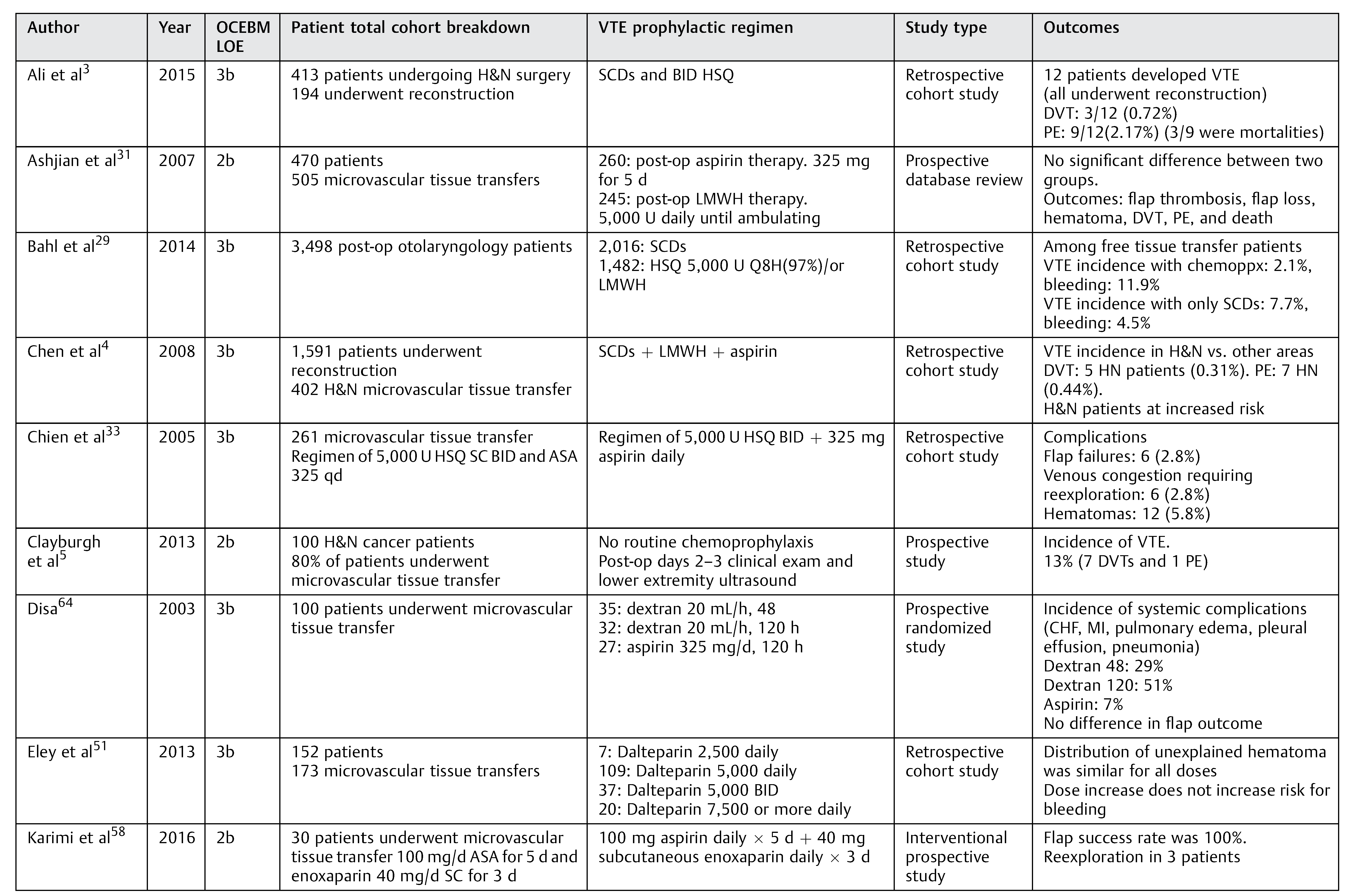  |
Unfractionated Heparin Formulations
Subcutaneous Heparin
Intravenous Heparin
Low-Molecular-Weight Heparins
Dextran
Warfarin
Inferior Vena Cava Filter
Discussion

Conclusions
Acknowledgments
Conflicts of Interest
References
- Agnelli, G. Prevention of venous thromboembolism in surgical patients. Circulation 2004, 110 (Suppl 1), IV4–IV12. [Google Scholar] [PubMed]
- Geerts, W.H.; Pineo, G.F.; Heit, J.A.; et al. Prevention of venous thromboembolism: The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004, 126, 338S–400S. [Google Scholar] [CrossRef] [PubMed]
- Ali, N.S.; Nawaz, A.; Junaid, M.; Kazi, M.; Akhtar, S. Venous thromboembolism-incidence of deep venous thrombosis and pulmonary embolism in patients with head and neck cancer: A tertiary care experience in Pakistan. Int Arch Otorhinolaryngol 2015, 19, 200–204. [Google Scholar]
- Chen, C.M.; Disa, J.J.; Cordeiro, P.G.; Pusic, A.L.; McCarthy, C.M.; Mehrara, B.J. The incidence of venous thromboembolism after oncologic head and neck reconstruction. Ann Plast Surg 2008, 60, 476–479. [Google Scholar]
- Clayburgh, D.R.; Stott, W.; Cordiero, T.; et al. Prospective study of venous thromboembolism in patients with head and neck cancer after surgery. JAMA Otolaryngol Head Neck Surg 2013, 139, 1143–1150. [Google Scholar]
- Garritano, F.G.; Lehman, E.B.; Andrews, G.A. Incidence of venous thromboembolism in otolaryngology-head and neck surgery. JAMA Otolaryngol Head Neck Surg 2013, 139, 21–27. [Google Scholar]
- Kakei, Y.; Akashi, M.; Hasegawa, T.; Minamikawa, T.; Usami, S.; Komori, T. Incidence of venous thromboembolism after oral oncologic surgery with simultaneous reconstruction. J Oral Maxillofac Surg 2016, 74, 212–217. [Google Scholar]
- Moreano, E.H.; Hutchison, J.L.; McCulloch, T.M.; Graham, S.M.; Funk, G.F.; Hoffman, H.T. Incidence of deep venous thrombosis and pulmonary embolism in otolaryngology-head and neck surgery. Otolaryngol Head Neck Surg 1998, 118, 777–784. [Google Scholar] [PubMed]
- Thai, L.; McCarn, K.; Stott, W.; et al. Venous thromboembolism in patients with head and neck cancer after surgery. Head Neck 2013, 35, 4–9. [Google Scholar]
- Pugh, C.M.; Dennis, R.H.I.I.; Massac, E.A. Evaluation of intraoperative anticoagulants in microvascular free-flap surgery. J Natl Med Assoc 1996, 88, 655–657. [Google Scholar]
- Gould, M.K.; Garcia, D.A.; Wren, S.M.; et al. Prevention of VTE in nonorthopedic surgical patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012, 141 (Suppl), e227S–e277S. [Google Scholar] [CrossRef] [PubMed]
- Garritano, F.G.; Andrews, G.A. Current practices in venous thromboembolism prophylaxis in otolaryngology-head and neck surgery. Head Neck 2016, 38 (Suppl. 1), E341–E345. [Google Scholar] [CrossRef] [PubMed]
- Innis, W.P.; Anderson, T.D. Deep venous thrombosis and pulmonary embolism in otolaryngologic patients. Am J Otolaryngol 2009, 30, 230–233. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Alexander, A.; Higgins, K.; Geerts, W. The Sunnybrook experience: Review of deep vein thrombosis and pulmonary embolism in otolaryngology. J Otolaryngol Head Neck Surg 2008, 37, 547–551. [Google Scholar]
- Lighthall, J.G.; Cain, R.; Ghanem, T.A.; Wax, M.K. Effect of postoperative aspirin on outcomes in microvascular free tissue transfer surgery. Otolaryngol Head Neck Surg 2013, 148, 40–46. [Google Scholar] [CrossRef]
- Roderick, P.; Ferris, G.; Wilson, K.; et al. Towards evidence-based guidelines for the prevention of venous thromboembolism: Systematic reviews of mechanical methods, oral anticoagulation, dextran and regional anaesthesia as thromboprophylaxis. Health Technol Assess 2005, 9, iii. [Google Scholar] [CrossRef]
- Clagett, G.P.; Anderson FAJr Levine, M.N.; Salzman, E.W.; Wheeler, H.B. Prevention of venous thromboembolism. Chest 1992, 102 (Suppl. 4), 391S–407S. [Google Scholar] [CrossRef]
- Kruse, A.L.; Luebbers, H.T.; Grätz, K.W.; Obwegeser, J.A. Factors influencing survival of free-flap in reconstruction for cancer of the head and neck: A literature review. Microsurgery 2010, 30, 242–248. [Google Scholar] [CrossRef]
- Yeung, J.K.; Harrop, R.; McCreary, O.; et al. Delayed mobilization after microsurgical reconstruction: An independent risk factor for pneumonia. Laryngoscope 2013, 123, 2996–3000. [Google Scholar] [CrossRef]
- Undas, A.; Brummel-Ziedins, K.E.; Mann, K.G. Antithrombotic properties of aspirin and resistance to aspirin: Beyond strictly antiplatelet actions. Blood 2007, 109, 2285–2292. [Google Scholar] [CrossRef]
- Wakefield, T.W.; Obi, A.T.; Henke, P.K. An aspirin a day to keep the clots away: Can aspirin prevent recurrent thrombosis in extended treatment for venous thromboembolism? Circulation 2014, 130, 1031–1033. [Google Scholar] [CrossRef]
- Becattini, C.; Agnelli, G.; Schenone, A.; et al. WARFASA Investigators. Aspirin for preventing the recurrence of venous thromboembolism. N Engl J Med 2012, 366, 1959–1967. [Google Scholar] [CrossRef]
- Brighton, T.A.; Eikelboom, J.W.; Mann, K.; et al. ASPIRE Investigators. Low-dose aspirin for preventing recurrent venous thromboembolism. N Engl J Med 2012, 367, 1979–1987. [Google Scholar] [CrossRef]
- Johnson, P.C.; Barker, J.H. Thrombosis and antithrombotic therapy in microvascular surgery. Clin Plast Surg 1992, 19, 799–807. [Google Scholar] [CrossRef]
- Khouri, R.K.; Cooley, B.C.; Kunselman, A.R.; et al. A prospective study of microvascular free-flap surgery and outcome. Plast Reconstr Surg 1998, 102, 711–721. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Cooley, B.C. Effect of anticoagulation and inhibition of platelet aggregation on arterial versus venous microvascular thrombosis. Ann Plast Surg 1995, 35, 165–169. [Google Scholar] [CrossRef]
- Spiegel, J.H.; Polat, J.K. Microvascular flap reconstruction by otolaryngologists: Prevalence, postoperative care, and monitoring techniques. Laryngoscope 2007, 117, 485–490. [Google Scholar] [CrossRef] [PubMed]
- Blackwell, K.E. Unsurpassed reliability of free flaps for head and neck reconstruction. Arch Otolaryngol Head Neck Surg 1999, 125, 295–299. [Google Scholar] [CrossRef] [PubMed]
- Bahl, V.; Shuman, A.G.; Hu, H.M.; et al. Chemoprophylaxis for venous thromboembolism in otolaryngology. JAMA Otolaryngol Head Neck Surg 2014, 140, 999–1005. [Google Scholar] [CrossRef]
- Lee, K.T.; Mun, G.H. The efficacy of postoperative antithrombotics in free flap surgery: A systematic review and meta-analysis. Plast Reconstr Surg 2015, 135, 1124–1139. [Google Scholar]
- Ashjian, P.; Chen, C.M.; Pusic, A.; Disa, J.J.; Cordeiro, P.G.; Mehrara, B.J. The effect of postoperative anticoagulation on microvascular thrombosis. Ann Plast Surg 2007, 59, 36–39. [Google Scholar] [PubMed]
- Dort, J.C.; Farwell, D.G.; Findlay, M.; et al. Optimal perioperative care in major head and neck cancer surgery with free flap reconstruction: A consensus review and recommendations from the enhanced recovery after surgery society. JAMA Otolaryngol Head Neck Surg 2017, 143, 292–303. [Google Scholar] [PubMed]
- Chien, W.; Varvares, M.A.; Hadlock, T.; Cheney, M.; Deschler, D.G. Effects of aspirin and low-dose heparin in head and neck reconstruction using microvascular free flaps. Laryngoscope 2005, 115, 973–976. [Google Scholar] [PubMed]
- Veravuthipakorn, L.; Veravuthipakorn, A. Microsurgical free flap and replantation without antithrombotic agents. J Med Assoc Thai 2004, 87, 665–669. [Google Scholar]
- Kumar, S.; Moorthy, R. New oral anticoagulants—A guide for ENT surgeons. J Laryngol Otol 2016, 130, 324–328. [Google Scholar]
- Askari, M.; Fisher, C.; Weniger, F.G.; Bidic, S.; Lee, W.P. Anticoagulation therapy in microsurgery: A review. J Hand Surg Am 2006, 31, 836–846. [Google Scholar]
- Stockmans, F.; Stassen, J.M.; Vermylen, J.; Hoylaerts, M.F.; Nyström, A. A technique to investigate microvascular mural thrombus formation in arteries and veins: II. Effects of aspirin, heparin, r-hirudin, and G-4120. Ann Plast Surg 1997, 38, 63–68. [Google Scholar]
- Motakef, S.; Mountziaris, P.M.; Ismail, I.K.; Agag, R.L.; Patel, A. Emerging paradigms in perioperative management for microsurgical free tissue transfer: Review of the literature and evidence-based guidelines. Plast Reconstr Surg 2015, 135, 290–299. [Google Scholar] [CrossRef]
- Xipoleas, G.; Levine, E.; Silver, L.; Koch, R.M.; Taub, P.J. A survey of microvascular protocols for lower-extremity free tissue transfer I: Perioperative anticoagulation. Ann Plast Surg 2007, 59, 311–315. [Google Scholar]
- Lecoq, J.P.; Senard, M.; Hartstein, G.M.; Lamy, M.; Heymans, O. Thromboprophylaxis in microsurgery. Acta Chir Belg 2006, 106, 158–164. [Google Scholar]
- Pan, X.L.; Chen, G.X.; Shao, H.W.; Han, C.M.; Zhang, L.P.; Zhi, L.Z. Effect of heparin on prevention of flap loss in microsurgical free flap transfer: A meta-analysis. PLoS ONE 2014, 9, e95111. [Google Scholar]
- Fan, K.L.; Patel, K.M.; Mardini, S.; Attinger, C.; Levin, L.S.; Evans, K.K. Evidence to support controversy in microsurgery. Plast Reconstr Surg 2015, 135, 595e–608e. [Google Scholar] [PubMed]
- Akl, E.A.; Kahale, L.; Sperati, F.; et al. Low molecular weight heparin versus unfractionated heparin for perioperative thromboprophylaxis in patients with cancer. Cochrane Database Syst Rev 2014, CD009447. [Google Scholar]
- Bahl, V.; Hu, H.M.; Henke, P.K.; Wakefield, T.W.; Campbell, D.A., Jr.; Caprini, J.A. A validation study of a retrospective venous thromboembolism risk scoring method. Ann Surg 2010, 251, 344–350. [Google Scholar]
- Kroll, S.S.; Miller, M.J.; Reece, G.P.; et al. Anticoagulants and hematomas in free flap surgery. Plast Reconstr Surg 1995, 96, 643–647. [Google Scholar]
- Nelson, J.A.; Chung, C.U.; Bauder, A.R.; Wu, L.C. Prevention of thrombosis in hypercoagulable patients undergoing microsurgery: A novel anticoagulation protocol. J Plast Reconstr Aesthet Surg 2017, 70, 307–312. [Google Scholar] [PubMed]
- Malm, K.; Dahlbäck, B.; Arnljots, B. Low-molecular-weight heparin (dalteparin) effectively prevents thrombosis in a rat model of deep arterial injury. Plast Reconstr Surg 2003, 111, 1659–1666. [Google Scholar]
- Green, D.; Hirsh, J.; Heit, J.; Prins, M.; Davidson, B.; Lensing, A.W. Low molecular weight heparin: A critical analysis of clinical trials. Pharmacol Rev 1994, 46, 89–109. [Google Scholar]
- De, A.; Roy, P.; Garg, V.K.; Pandey, N.K. Low-molecular-weight heparin and unfractionated heparin in prophylaxis against deep vein thrombosis in critically ill patients undergoing major surgery. Blood Coagul Fibrinolysis 2010, 21, 57–61. [Google Scholar]
- Blackburn, T.K.; Java, K.R.; Lowe, D.; Brown, J.S.; Rogers, S.N. Safety of a regimen for thromboprophylaxis in head and neck cancer microvascular reconstructive surgery: Non-concurrent cohort study. Br J Oral Maxillofac Surg 2012, 50, 227–232. [Google Scholar]
- Eley, K.A.; Parker, R.J.; Watt-Smith, S.R. Low molecular weight heparin in patients undergoing free tissue transfer following head and neck ablative surgery: Review of efficacy and associated complications. Br J Oral Maxillofac Surg 2013, 51, 610–614. [Google Scholar] [CrossRef] [PubMed]
- Mulloy, B.; Hogwood, J.; Gray, E.; Lever, R.; Page, C.P. Pharmacology of heparin and related drugs. Pharmacol Rev 2016, 68, 76–141. [Google Scholar]
- Nader, H.B.; Walenga, J.M.; Berkowitz, S.D.; Ofosu, F.; Hoppensteadt, D.A.; Cella, G. Preclinical differentiation of low molecular weight heparins. Semin Thromb Hemost 1999, 25 (Suppl. 3), 63–72. [Google Scholar] [PubMed]
- Planes, A.; Vochelle, N.; Darmon, J.Y. Out-of-hospital prophylaxis with low-molecular-weight heparin in hip surgery: The French study– venographic outcome at 35 days. Chest 1998, 114 (Suppl Evidence), 125S–129S. [Google Scholar] [CrossRef] [PubMed]
- Spiro, T.E.; Johnson, G.J.; Christie, M.J.; et al. Enoxaparin Clinical Trial Group. Efficacy and safety of enoxaparin to prevent deep venous thrombosis after hip replacement surgery. Ann Intern Med 1994, 121, 81–89. [Google Scholar] [CrossRef]
- Levine, M.N.; Hirsh, J.; Gent, M.; et al. Prevention of deep vein thrombosis after elective hip surgery. A randomized trial comparing low molecular weight heparin with standard unfractionated heparin. Ann Intern Med 1991, 114, 545–551. [Google Scholar] [CrossRef]
- Lemaine, V.; McCarthy, C.; Kaplan, K.; et al. Venous thromboembolism following microsurgical breast reconstruction: An objective analysis in 225 consecutive patients using low-molecular-weight heparin prophylaxis. Plast Reconstr Surg 2011, 127, 1399–1406. [Google Scholar] [CrossRef]
- Karimi, E.; Ardestani, S.H.; Jafari, M.; Hagh, A.B. Testing a new anticoagulation method for free flap reconstruction of head and neck cancers. Clin Exp Otorhinolaryngol 2016, 9, 370–373. [Google Scholar] [CrossRef]
- Reiter, M.; Kapsreiter, M.; Betz, C.S.; Harréus, U. Perioperative management of antithrombotic medication in head and neck reconstruction-a retrospective analysis of 137 patients. Am J Otolaryngol 2012, 33, 693–696. [Google Scholar] [CrossRef]
- Pršić, A.; Kiwanuka, E.; Caterson, S.A.; Caterson, E.J. Anticoagulants and statins as pharmacological agents in free flap surgery: Current rationale. Eplasty 2015, 15, e51. [Google Scholar]
- Salemark, L.; Wieslander, J.B.; Dougan, P.; Arnljots, B. Studies of the antithrombotic effects of dextran 40 following microarterial trauma. Br J Plast Surg 1991, 44, 15–22. [Google Scholar] [PubMed]
- Scholz, T.; Evans, G.R. Impact of hypertonic and hyperoncotic saline solutions on ischemia-reperfusion injury in free flaps. Plast Reconstr Surg 2008, 122, 85–94. [Google Scholar]
- Wieslander, J.B.; Dougan, P.; Stjernquist, U.; Aberg, M.; Bergentz, S.E. The influence of dextran and saline solution upon platelet behavior after microarterial anastomosis. Surg Gynecol Obstet 1986, 163, 256–262. [Google Scholar] [PubMed]
- Disa, J.J.; Polvora, V.P.; Pusic, A.L.; Singh, B.; Cordeiro, P.G. Dextran-related complications in head and neck microsurgery: Do the benefits outweigh the risks? A prospective randomized analysis. Plast Reconstr Surg 2003, 112, 1534–1539. [Google Scholar] [PubMed]
- Jayaprasad, K.; Mathew, J.; Thankappan, K.; et al. Safety and efficacy of low molecular weight dextran (dextran 40) in head and neck free flap reconstruction. J Reconstr Microsurg 2013, 29, 443–448. [Google Scholar]
- Ridha, H.; Jallali, N.; Butler, P.E. The use of dextran post free tissue transfer. J Plast Reconstr Aesthet Surg 2006, 59, 951–954. [Google Scholar]
- Riva, F.M.; Chen, Y.C.; Tan, N.C.; et al. The outcome of prostaglandin-E1 and dextran-40 compared to no antithrombotic therapy in head and neck free tissue transfer: Analysis of 1,351 cases in a single center. Microsurgery 2012, 32, 339–343. [Google Scholar]
- Sun, T.B.; Chien, S.H.; Lee, J.T.; Cheng, L.F.; Hsu, L.P.; Chen, P.R. Is dextran infusion as an antithrombotic agent necessary in microvascular reconstruction of the upper aerodigestive tract? J Reconstr Microsurg 2003, 19, 463–466. [Google Scholar]
- Hardin, C.K.; Kirk, W.C.; Pederson, W.C. Osmotic complications of low-molecular-weight dextran therapy in free flap surgery. Microsurgery 1992, 13, 36–38. [Google Scholar]
- Hein, K.D.; Wechsler, M.E.; Schwartzstein, R.M.; Morris, D.J. The adult respiratory distress syndrome after dextran infusion as an antithrombotic agent in free TRAM flap breast reconstruction. Plast Reconstr Surg 1999, 103, 1706–1708. [Google Scholar]
- Kaplan, A.I.; Sabin, S. Dextran 40: Another cause of drug-induced noncardiogenic pulmonary edema. Chest 1975, 68, 376–377. [Google Scholar]
- Machado, M.A.; Volpe, P.; Lima M das, G.; et al. [Anaphylaxis after dextran 40 infusion: Report of a case and review of the literature]. Rev Hosp Clin Fac Med Sao Paulo 1993, 48, 167–169. [Google Scholar]
- Parry, S.W.; Toth, B.A.; Elliott, L.F. Microvascular free-tissue transfer in children. Plast Reconstr Surg 1988, 81, 838–840. [Google Scholar] [PubMed]
- Francis, C.W.; Pellegrini, V.D., Jr.; Stulberg, B.N.; Miller, M.L.; Totterman, S.; Marder, V.J. Prevention of venous thrombosis after total knee arthroplasty. Comparison of antithrombin III and low-dose heparin with dextran. J Bone Joint Surg Am 1990, 72, 976–982. [Google Scholar] [PubMed]
- Mätzsch, T.; Bergqvist, D.; Fredin, H.; Hedner, U. Low molecular weight heparin compared with dextran as prophylaxis against thrombosis after total hip replacement. Acta Chir Scand 1990, 156, 445–450. [Google Scholar]
- Oertli, D.; Hess, P.; Durig, M.; et al. Prevention of deep vein thrombosis in patients with hip fractures: Low molecular weight heparin versus dextran. World J Surg 1992, 16, 980–984. [Google Scholar]
- Feldman, D.S.; Zuckerman, J.D.; Walters, I.; Sakales, S.R. Clinical efficacy of aspirin and dextran for thromboprophylaxis in geriatric hip fracture patients. J Orthop Trauma 1993, 7, 1–5. [Google Scholar] [PubMed]
- Büller, H.R.; Agnelli, G.; Hull, R.D.; Hyers, T.M.; Prins, M.H.; Raskob, G.E. Antithrombotic therapy for venous thromboembolic disease: The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004, 126 (Suppl. 3), 401S–428S. [Google Scholar]
- Jaggi, R.; Taylor, S.M.; Trites, J.; Anderson, D.; MacDougall, P.; Hart, R.D. Review of thromboprophylaxis in otolaryngology-head and neck surgery. J Otolaryngol Head Neck Surg 2011, 40, 261–265. [Google Scholar]
- Gavriel, H.; Thompson, E.; Kleid, S.; Chan, S.; Sizeland, A. Safety of thromboprophylaxis after oncologic head and neck surgery. Study of 1018 patients. Head Neck 2013, 35, 1410–1414. [Google Scholar]
- Moubayed, S.P.; Eskander, A.; Mourad, M.W.; Most, S.P. Systematic review and meta-analysis of venous thromboembolism in otolaryngology-head and neck surgery. Head Neck 2017, 39, 1249–1258. [Google Scholar] [PubMed]
- Ah-See, K.W.; Kerr, J.; Sim, D.W. Prophylaxis for venous thromboembolism in head and neck surgery: The practice of otolaryngologists. J Laryngol Otol 1997, 111, 845–849. [Google Scholar] [PubMed]
- Pallister, C.; Watson, M. Haematology, 2nd ed.; Scion Publishing, 2010. [Google Scholar]
- Shuman, A.G.; Hu, H.M.; Pannucci, C.J.; Jackson, C.R.; Bradford, C.R.; Bahl, V. Stratifying the risk of venous thromboembolism in otolaryngology. Otolaryngol Head Neck Surg 2012, 146, 719–724. [Google Scholar] [PubMed]
- Davison, S.P.; Venturi, M.L.; Attinger, C.E.; Baker, S.B.; Spear, S.L. Prevention of venous thromboembolism in the plastic surgery patient. Plast Reconstr Surg 2004, 114, 43E–51E. [Google Scholar] [PubMed]
- Young, T.; Aukes, J.; Hughes, R.; Tang, H. Vena caval filters for the prevention of pulmonary embolism. Cochrane Database Syst Rev 2007, CD006212. [Google Scholar]
- Robert, F. The potential benefits of low-molecular-weight heparins in cancer patients. J Hematol Oncol 2010, 3, 3. [Google Scholar] [PubMed]
- Lee, A.Y.Y.; Levine, M.N.; Baker, R.I.; et al. Randomized Comparison of Low-Molecular-Weight Heparin versus Oral Anticoagulant Therapy for the Prevention of Recurrent Venous Thromboembolism in Patients with Cancer (CLOT) Investigators. Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med 2003, 349, 146–153. [Google Scholar]
- Akl, E.A.; Terrenato, I.; Barba, M.; et al. Low-molecular-weight heparin vs unfractionated heparin for perioperative thromboprophylaxis in patients with cancer: A systematic review and meta-analysis. Arch Intern Med 2008, 168, 1261–1269. [Google Scholar]
- Wikner, J.; Beck-Broichsitter, B.E.; Schlesinger, S.; et al. Thromboelas-tometry: A contribution to perioperative free-flap management. J Craniomaxillofac Surg 2015, 43, 1065–1071. [Google Scholar]
- Benes, J.; Zatloukal, J.; Kletecka, J. Viscoelastic methods of blood clotting assessment—A multidisciplinary review. Front Med 2015, 2, 62. [Google Scholar]
- Luddington, R.J. Thrombelastography/thromboelastometry. Clin Lab Haematol 2005, 27, 81–90. [Google Scholar] [PubMed]
- Wikkelsø, A.; Wetterslev, J.; Møller, A.M.; Afshari, A. Thromboelasto-graphy (TEG) or rotational thromboelastometry (ROTEM) to monitor haemostatic treatment in bleeding patients: A systematic review with meta-analysis and trial sequential analysis. Anaesthesia 2017, 72, 519–531. [Google Scholar] [PubMed]
© 2017 by the author. The Author(s) 2017.
Share and Cite
Abraham, M.; Badhey, A.; Hu, S.; Kadakia, S.; Rasamny, J.K.; Moscatello, A.; Ducic, Y. Thromboprophylaxis in Head and Neck Microvascular Reconstruction. Craniomaxillofac. Trauma Reconstr. 2018, 11, 85-95. https://doi.org/10.1055/s-0037-1607068
Abraham M, Badhey A, Hu S, Kadakia S, Rasamny JK, Moscatello A, Ducic Y. Thromboprophylaxis in Head and Neck Microvascular Reconstruction. Craniomaxillofacial Trauma & Reconstruction. 2018; 11(2):85-95. https://doi.org/10.1055/s-0037-1607068
Chicago/Turabian StyleAbraham, Manoj, Arvind Badhey, Shirley Hu, Sameep Kadakia, J. K. Rasamny, Augustine Moscatello, and Yadranko Ducic. 2018. "Thromboprophylaxis in Head and Neck Microvascular Reconstruction" Craniomaxillofacial Trauma & Reconstruction 11, no. 2: 85-95. https://doi.org/10.1055/s-0037-1607068
APA StyleAbraham, M., Badhey, A., Hu, S., Kadakia, S., Rasamny, J. K., Moscatello, A., & Ducic, Y. (2018). Thromboprophylaxis in Head and Neck Microvascular Reconstruction. Craniomaxillofacial Trauma & Reconstruction, 11(2), 85-95. https://doi.org/10.1055/s-0037-1607068



