Abstract
Mandibular fractures are rare, most commonly occurring in young male patients who present with facial trauma. The etiology, incidence, and presentation vary among previous publications depending on cultural and socioeconomic factors of the region of origin. This multi-institutional study aims to present demographic characteristics, surgical treatment, and clinical outcomes of surgical repair of mandible fractures in the United States. An analysis of the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) adult databases of the years 2006 through 2014 was performed identifying 940 patients with an International Classification of Diseases, version 9 (ICD-9) diagnosis of either closed or open fracture of the mandible. Preoperative, perioperative, and postoperative details were categorized and evaluated for these two cohorts. Multivariate analysis was performed to detect risk factors related to any complications. Patients were predominantly male (85.7%), young with a mean age of 34.0 ± 14.8 years, and relatively healthy with body mass index of 23.6 ± 8.2 and an American Society of Anesthesiologists (ASA) class of 1 or 2 (84.4%). However, more than half were regular smokers (51.1%). The top five most frequent procedures performed for mandibular repair were exclusively open surgical approaches with internal, external, or interdental fixation in both cohorts. Patients with open fractures were more often admitted as emergencies, treated inpatient, required longer operative times, and presented with more contaminated wounds (p < 0.05). Overall, medical (1.7%) and surgical complications (3.7%) were low. A high ASA class 3 or above and emergency operations were identified as risk factors for medical adverse events. Despite frequent concomitant injuries after trauma and a diverse array of mandibular injury types, our patient sample demonstrated favorable outcomes and low complication rates. Open surgical techniques were the most common procedures in this study representing the American population.
Although infrequent in the general population, mandibular fractures are a proportionally common finding in patients suffering from facial trauma [1]. Aside from rare cases of malignancy [2]. or osteonecrosis, motor vehicle accidents, violence, and sports account for the majority of cases involving damage to the mandible, its teeth, and the surrounding soft tissue [3,4]. Younger men are particularly prone to such injuries due to their affinity to high-risk professional and leisure activities, as well as more violent behaviors [5,6,7].
Mandibular fractures are categorized based on the location of bone disruption. Therefore, possible classifications of fractures include condylar, subcondylar, coronoid process, ramus, angle, body, parasymphysis, or symphysis. Greenstick fractures are a category exclusively found in young children. Further differentiations are made in terms of complexity (simple or comminuted), soft-tissue involvement (open or closed), and teeth dislocation or misalignment [8].
During patient assessment, it is vital to first identify any concomitant, possible life-threatening injuries [1], the most important being airway obstructions, prior to treatment of the mandible [9]. Next, history, focused physical exam, and imaging studies determine the extent and type of facial injury. Definitive treatment for a mandible fracture includes observation, conservative closed approaches, or various open surgical procedures to achieve a cosmetically and functionally satisfactory result.
While previous publications reported on the therapy of mandibular fractures, many studies solely provide treatment algorithms from authors’ personal experiences [5,10,11,12], evaluate small patient samples [13,14], or confine themselves to specific populations [1,15]. With this in mind, we utilized the nationwide multi-institutional American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) adult database to design a retrospective study exploring the surgical treatment of mandible fractures across the United States. The purpose of this study was to determine which procedures are commonly performed for the treatment of mandibular fractures, analyze the surgical outcomes and complications of these operations, and detect risk factors for adverse events.
Methods
The ACS NSQIP databases of the years 2006 through 2014 are the source of the data presented in this report [16]. This national multicentric program included more than 750,000 surgical cases for 2014 alone, is steadily growing in participating institutions and case numbers, and thus ideally suited to conduct high-quality evidence-based research. Anonymized patient information is continuously uploaded to the ACS and includes variables, such as preoperative comorbidities, perioperative details, and postoperative follow-up.
Based on the International Classification of Diseases, version 9 (ICD-9) [17], we performed a retrospective analysis of the NSQIP and created two cohorts screening for codes 802.2 (closed fracture of mandible) and 802.3 (open fracture of mandible). Descriptive calculations were done for each cohort with regard to demographics and preoperative details. Primary surgical procedures performed were deciphered using the American Medical Association Current Procedural Terminology (CPT) [18] codes. Next, perioperative data analysis revealed information, such as the surgical specialty performing the procedure, operative time, or length of hospitalization.
In addition to readmission, reoperation, and mortality, primary outcomes of interest were separated into two global categories: medical and surgical complications. Adverse events are documented and reported only to NSQIP if they occurred within the standard 30 days after surgery. Pulmonary complications included reintubation, failure to postoperatively wean off the ventilator within 48 h, and pneumonia. Cardiac events consisted of cardiac arrest requiring cardiopulmonary resuscitation (CPR) and myocardial infarction. Urinary tract infections, renal failure, and renal insufficiency were cases of renal complications. Hematologic complications included deep vein thrombosis (DVT) and pulmonary embolism (PE), while infectious events were defined as sepsis or septic shock. Surgical complications consisted of surgical site infection (superficial, deep incisional, organ space), wound dehiscence, and bleeding requiring transfusion. This study was approved by our institutional review board. The authors adhered to the Declaration of Helsinki at all times.
Statistics
Descriptive statistics were calculated and analyzed for all patients meeting the aforementioned inclusion criteria. Univariate analysis compared the two cohorts for preoperative risk factors, patient comorbidities, procedures, and their final outcomes. Statistical level of significance was set at 5% (p < 0.05) for all analyses using the unpaired sample t-test for continuous and the chi-square test for categorical variables. Factors with p-values less than 0.10, in addition to clinically pertinent factors, were gathered for a multivariate logistical regression analysis to control for confounders and to quantify the influence of various factors on complication rates. Statistics were conducted using SPSS version 24.0 (IBM Corp., Armonk, NY, USA).
Results
A total of 750 patients with closed fracture and 190 with open fracture of the mandible were identified in our study leading to a total of 940 cases. The mean age was 34.0 ± 14.8 years and 85.7% of the patients were male (Figure 1). Pre-operatively, 51.1% of the included patients were regular smokers, while 5.4% reported regular consumption of alcohol. Mean body mass index (BMI) was 23.6 ± 8.2. With regard to medical comorbidities, hypertension and diabetes were the most common diseases: 11.6 and 3.4%, respectively. None of the demographic variables reached significance between our two cohorts, except for smoking that was statistically more prevalent (p = 0.023) with patients who suffered a closed fracture (Table 1).
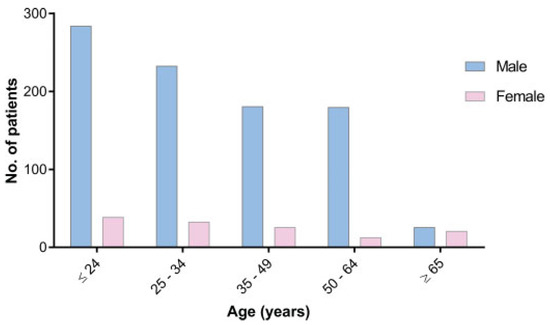
Figure 1.
Age and gender distribution of patients with mandibular fracture.

Table 1.
Demographics and comorbidities.
The five most common procedures performed in both the closed and open fracture cohort were exclusively open surgical approaches listed in Table 2 with no statistical difference in procedure performed based on type of fracture, open or closed. Furthermore, the distribution of American Society of Anesthesiologists (ASA) classifications (ASA 1 + 2: 84.4%), length of hospitalization (1.3 ± 4.2 days), and specialty involved (otolaryngology: 62.6%, plastic surgery: 34.1%) were similar for closed and open fracture patients. However, open fractures were significantly more often emergency cases (p = 0.002), more frequently treated on an inpatient basis (p = 0.010), and required a longer operative time (p < 0.001) as displayed in Table 2.

Table 2.
Operative factors.
Medical complications within the NSQIP’s 30-day follow-up period were low in both cohorts arising in 1.5% of closed and in 2.6% of open fracture patients (overall: 1.7%). Surgical complications occurred in 4.0% of closed and 2.6% of open cases (overall: 3.7%). The wounds of patients with open fractures were classified significantly higher, meaning more contaminated, than those of patients with a closed mandibular fracture (p < 0.001). Readmission (closed: 2.3%, open: 2.1%) and reoperation rates (closed: 1.5%, open: 0.5%) were at similarly low levels. Only one fatality (0.1%) occurred in this study in a patient with a closed fracture of the mandible. There were no significant differences between the groups in terms of adverse outcomes (Table 3).

Table 3.
Outcomes and complications.
The subsequent multivariate regression analysis revealed only a statistical association between a high ASA class 3+ (odds ratio [OR] = 7.74, p = 0.003), as well as emergency operations (OR = 3.62, p = 0.032), and the risk of suffering from medical complications following surgical mandible fracture repair (OR = 7.74, p = 0.003). Age, type of fracture, operative time, and smoking were not related to medical adverse events (Table 4). Despite a larger number of surgical complications in both our cohorts (n = 35), no factors were identified that could be associated with more prevalent surgical complications (Table 5).

Table 4.
Multivariate regression analysis of medical complications (n = 16).

Table 5.
Multivariate regression analysis of surgical complications (n = 35).
Discussion
Which Patients Present with Mandibular Fractures?
Owing to its prominence11 and lack of soft-tissue protection, the mandible is the most frequently broken bone in patients admitted for facial fractures [1,7,19]. Incidence rises in children resulting in a peak incidence in the 16- to 20-year age bracket [20]. Furthermore, adolescents and men make up the vast majority (75–90%) of patients with such injuries [9,21,22], which is typically explained by their more risky behavior [11]. Unlike children, who are more likely to suffer mandibular fractures due to falls, adults are more likely to sustain these injuries from motor vehicle accidents or assaults [7]. While the NSQIP database does not provide details on the cause of injury, our age (mean: 34.0 ± 14.8 years) and gender (85.7% male) distribution is comparable to that of world literature (Figure 1). [3,7,23]. The patients in this study demonstrated limited comorbidities, a BMI within the normal weight range, and primarily an ASA classification of 1 or 2. Interestingly, greater than half of these patients were smokers (Table 1). A previous retrospective study determined similarly high rates of smokers (35.4%) in their patients treated for mandibular fractures [24].
Treatment of Open versus Closed Fracture: Does It Make a Difference?
In our study, patients with open mandibular fractures were significantly more likely to be admitted with emergency status (p = 0.002), provided care as inpatient (p = 0.010), and ultimately required longer operative times (p < 0.001). The former two findings can be related to the patients’ wound classifications. Those with an open fracture more frequently presented with a contaminated wound class 3 or higher (p < 0.001) and subsequently required more urgent operative interventions and received closer postoperative monitoring. The latter likely results from damage to the mandibular soft-tissue envelope and requirement for washouts, debridements, or facial reconstruction procedures that are represented by secondary CPT codes not included in our analyses.
Despite these discrepancies, primary procedure types in the closed and open fracture cohorts and the mean length of hospitalization were similar. A large multicenter European study on mandibular fractures showed higher hospitalization times (2.0–10.6 days), although these variations can be due to differences in health care systems [25]. The NSQIP data suggested that otolaryngology appeared as the service predominantly providing operative treatment of the jaw in both our groups. This finding may be partly explained by the fewer number of plastic surgeons (6942) as compared to otolaryngologists (9320) board certified in the United States as of 2013 [18]. Due to the lack of oromaxillofacial surgery (OMFS) data in the ACS NSQIP databases, their global role in and influence on the treatment of jaw fractures cannot be assessed in this study. According to a study analyzing emergency treatment at a single institution, OMFS was preferred for referrals of mandibular fractures [26], yet, these trends may vary between different regions and institutions in the United States.
Choice of Operative Technique
Multiple publications from diverse specialties have described closed conservative treatment for simple and closed mandibular mandibular fractures. This may include closed reduction in combination with either interdental wiring [11] or maxillomandibular fixation [12] if patients present with stable teeth. Closed procedures have been described in publications of OMFS institutions for the treatment of isolated mandibular fractures [7,9]. Interestingly, no conservative closed management for mandibular fracture made it to the list of five most prevalent procedures based on the data provided by the NSQIP. Similar to a European multicenter study [22], the open approach was the predominant (>87%) procedure for both open and closed fractures. This involves direct visualization and the reduction of the mandibular fragments combined with interdental fixation, and internal fixation with screws and plates (rigid) [14] or transosseous wires (nonrigid) [21] and is typically described for any more complex mandibular fractures. In our study, 70.9% of all fractures were treated by open technique with some form of internal and/or interdental fixation, which is typically necessary for any osseous or joint instability. In only 11.2% of cases, such fixation was not included in the open operative procedure suggesting a rather stable fracture. In addition, these data suggest that the choice for an open procedure was not based on the patient’s dental health alone. External fixation, which was used in 2.9% of cases, is reserved for the most complicated fractures with large soft-tissue defects or when immediate jaw bone repair is not possible [13] These surgical details and the distribution of procedures in this study indicate that our patient sample was in fact suffering from more complex fracture patterns, given that conservative treatment was so infrequently applied (Table 2). Ultimately, however, the management of the fracture is tailored for the individual based on fracture pattern and concomitant injuries and varies between distinct patients.
Complications from Mandibular Fractures
Complications of trauma leading to fracture of the mandible can be related to either concomitantly sustained injuries of other body parts or directly to the jawbone injury. The latter includes infection and bone nonunion [13], improper repair requiring revisions [1,14], malocclusion [10,14], paresthesia [14], and unsatisfactory aesthetic results.1 Patient comorbidities and the universal burden of anesthesia, surgery, and hospitalization can furthermore lead to multiple medical adverse outcomes and should not be underestimated. Prior author groups have published complication rates between 0.0 and 20.0% [1,7,14,19,24,27,28,29], yet vary in their criteria of what is considered such. The complication rates in our study, 1.7% for medical and 3.7% for surgical events, were on the lower end of that range, potentially because of the limited follow-up in the NSQIP database. No statistical difference in complications was detected between the closed and open fracture cohorts, although the latter did receive scores 3+ on their classification of wound contamination (Table 3). Smoking, alcohol consumption, and substance abuse have been detected as risk factors for postoperative complications of mandibular surgery by other authors [24,28]. Multivariate regression analysis of our data, however, only showed a high ASA class and emergency operations associated with a risk for medical complications (Table 4). The majority of calculations did not lead to significance considering the rarity of adverse occurrences. Smokers (51.1%) had no statistically increased risk for adverse events than nonsmokers. Their extremely high prevalence in our patient sample did not lead to high complications. The patients’ young age, low BMI, and low ASA class may compensate for the risks associated with smoking.
Finally and similar to other studies, our data failed to demonstrate any significance between operative techniques in terms of complications [21]. Due to the anonymity of the databases, the cause of death of the one deceased patient (0.1% fatality) cannot be determined. Based on the findings of previous publications, it was likely due to a concomitant injury of vital organs and not related to the mandibular repair [30].
This report is not without certain limitations. The NSQIP databases are tended to by the institutions and their staff who upload patient data that are dependent on accurate documentation. The 940 surgical cases included in our study came from a variety of institutions, which are de-identified by design. The results in this report may therefore not be representative for every clinical setting. Furthermore, surgical treatment performed by OMFS, a historically dental specialty, is not included in the ACS NSQIP databases and this might distort results. Finally, patients are monitored only for 30 days after surgery by NSQIP standards. Any complication, readmission, and reoperation afterward would be missed and reported as an entirely new case. This study is, therefore, not able to evaluate the long-term functional and cosmetic outcomes of mandible repair and potential facial reconstruction.
Conclusions
Mandibular fractures remain a rare entity within the average population and are almost exclusively a consequence of external trauma to the face. In our NSQIP databank review, the 30-day outcomes were very favorable: complication rates were 1.7% for medical and 3.7% for surgical events. High ASA class and emergency operations were identified as risk factors associated with nonsurgical complications. The open reduction and internal fixation are the most common approaches in surgical management, regardless of open or closed fracture. This report presents the first study with multi-institutional patient data representative for adult patients in the United States.
Funding
No funding was received for the work presented in this manuscript.
Institutional Review Board Statement
The work described in this article was approved by our institutional review board (Protocol number Pro00011704: “Observational Research in the Department of Plastic and Reconstructive Surgery”). The authors adhered to the Declaration of Helsinki at all times.
Data Availability Statement
American College of Surgeons National Surgical Quality Improvement Program and the hospitals participating in the ACS NSQIP are the source of the data used herein; these data have not been verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Conflicts of Interest
None of the authors, nor their close family members, have a financial interest in any of the products, devices, or drugs mentioned in this manuscript. Furthermore, the authors declare that no commercial associations or financial disclosures exist that might pose or create a conflict of interest with information presented in this manuscript.
References
- Ferreira, P.C.; Amarante, J.M.; Silva, P.N.; et al. Retrospective study of 1251 maxillofacial fractures in children and adolescents. Plast Reconstr Surg 2005, 115, 1500–1508. [Google Scholar]
- Moura, L.B.; Gabrielli, M.F.; Gabrielli, M.A.; Filho, V.A. Pathologic mandibular fracture as first sign of multiple myeloma. J Craniofac Surg 2016, 27, e138–e139. [Google Scholar]
- Afrooz, P.N.; Bykowski, M.R.; James, I.B.; Daniali, L.N.; Clavijo-Alvarez, J.A. The epidemiology of mandibular fractures in the United States, Part 1: A review of 13,142 cases from the US National Trauma Data Bank. J Oral Maxillofac Surg 2015, 73, 2361–2366. [Google Scholar] [PubMed]
- Morris, C.; Bebeau, N.P.; Brockhoff, H.; Tandon, R.; Tiwana, P. Mandibular fractures: An analysis of the epidemiology and patterns of injury in 4,143 fractures. J Oral Maxillofac Surg 2015, 73, 951.e1–951.e12. [Google Scholar] [PubMed]
- Murray, J.M. Mandible fractures and dental trauma. Emerg Med Clin North Am 2013, 31, 553–573. [Google Scholar] [PubMed]
- Kruger, E.; Tennant, M. Fractures of the mandible and maxilla: A 10-year analysis. Australas Med J 2016, 9, 17–24. [Google Scholar]
- Atilgan, S.; Erol, B.; Yaman, F.; Yilmaz, N.; Ucan, M.C. Mandibular fractures: A comparative analysis between young and adult patients in the southeast region of Turkey. J Appl Oral Sci 2010, 18, 17–22. [Google Scholar]
- Banks, P.; Brown, A. Fractures of the Facial Skeleton; Wright: Oxford, UK, 2001. [Google Scholar]
- Infante Cossio, P.; Espin Galvez, F.; Gutierrez Perez, J.L.; Garcia-Perla, A.; Hernandez Guisado, J.M. Mandibular fractures in children. A retrospective study of 99 fractures in 59 patients. Int J Oral Maxillofac Surg 1994, 23 Pt 1, 329–331. [Google Scholar]
- Cole, P.; Kaufman, Y.; Izaddoost, S.; Hatef, D.A.; Hollier, L. Principles of pediatric mandibular fracture management. Plast Reconstr Surg 2009, 123, 1022–1024. [Google Scholar]
- Goth, S.; Sawatari, Y.; Peleg, M. Management of pediatric mandible fractures. J Craniofac Surg 2012, 23, 47–56. [Google Scholar]
- Hackenberg, B.; Lee, C.; Caterson, E.J. Management of subcondylar mandible fractures in the adult patient. J Craniofac Surg 2014, 25, 166–171. [Google Scholar] [PubMed]
- Alpert, B.; Kushner, G.M.; Tiwana, P.S. Contemporary management of infected mandibular fractures. Craniomaxillofac Trauma Reconstr 2008, 1, 25–29. [Google Scholar] [PubMed]
- Burm, J.S.; Hansen, J.E. The use of microplates for internal fixation of mandibular fractures. Plast Reconstr Surg 2010, 125, 1485–1492. [Google Scholar] [PubMed]
- Rémi, M.; Christine, M.C.; Gael, P.; Soizick, P.; Joseph-André, J. Mandibular fractures in children: Long term results. Int J Pediatr Otorhinolaryngol 2003, 67, 25–30. [Google Scholar]
- American College of Surgeons. ACS NSQIP Participant Use Data File. 2014. Available online: https://www.facs.org/~/media/files/quality%20programs/nsqip/nsqip_puf_userguide_2014.ashx (accessed on 13 November 2016).
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 9th ed.; World Health Organization: New York, NY, USA, 1977. [Google Scholar]
- American Association of Medical Colleges. Physician Specialty Data Book. 2014. Available online: https://members.aamc.org/eweb/upload/Physician%20Specialty%20Databook%202014.pdf (accessed on 13 November 2016).
- Kelley, P.; Crawford, M.; Higuera, S.; Hollier, L.H. Two hundred ninetyfour consecutive facial fractures in an urban trauma center: Lessons learned. Plast Reconstr Surg 2005, 116, 42e–49e. [Google Scholar]
- Azevedo, A.B.; Trent, R.B.; Ellis, A. Population-based analysis of 10,766 hospitalizations for mandibular fractures in California, 1991 to 1993. J Trauma 1998, 45, 1084–1087. [Google Scholar]
- Nasser, M.; Pandis, N.; Fleming, P.S.; Fedorowicz, Z.; Ellis, E.; Ali, K. Interventions for the management of mandibular fractures. Cochrane Database Syst Rev 2013, 2013, CD006087. [Google Scholar]
- Boffano, P.; Kommers, S.C.; Roccia, F.; Forouzanfar, T. Mandibular trauma treatment: A comparison of two protocols. Med Oral Patol Oral Cir Bucal 2015, 20, e218–e223. [Google Scholar]
- Boffano, P.; Kommers, S.C.; Karagozoglu, K.H.; Gallesio, C.; Forouzanfar, T. Mandibular trauma: A two-centre study. Int J Oral Maxillofac Surg 2015, 44, 998–1004. [Google Scholar]
- Serena-Gómez, E.; Passeri, L.A. Complications of mandible fractures related to substance abuse. J Oral Maxillofac Surg 2008, 66, 2028–2034. [Google Scholar]
- Boffano, P.; Roccia, F.; Zavattero, E.; et al. European Maxillofacial Trauma (EURMAT) project: A multicentre and prospective study. J Craniomaxillofac Surg 2015, 43, 62–70. [Google Scholar] [PubMed]
- Le, B.T.; Holmgren, E.P.; Holmes, J.D.; Ueeck, B.A.; Dierks, E.J. Referral patterns for the treatment of facial trauma in teaching hospitals in the United States. J Oral Maxillofac Surg 2003, 61, 557–560. [Google Scholar]
- Kanno, T.; Sukegawa, S.; Nariai, Y.; et al. Surgical treatment of comminuted mandibular fractures using a low-profile locking mandibular reconstruction plate system. Ann Maxillofac Surg 2014, 4, 144–149. [Google Scholar] [PubMed]
- Furr, A.M.; Schweinfurth, J.M.; May, W.L. Factors associated with longterm complications after repair of mandibular fractures. Laryngoscope 2006, 116, 427–430. [Google Scholar] [PubMed]
- Gokkulakrishnan, S.; Singh, S.; Sharma, A.; Shahi, A.K. An analysis of postoperative complications and efficacy of 3D miniplates in fixation of mandibular fractures. Dent Res J 2012, 9, 414–421. [Google Scholar]
- Plaisier, B.R.; Punjabi, A.P.; Super, D.M.; Haug, R.H. The relationship between facial fractures and death from neurologic injury. J Oral Maxillofac Surg 2000, 58, 708–712, Discussion 712–713. [Google Scholar]
© 2017 by the author. The Author(s) 2017.