In 2013, motorcycle helmets saved an estimated 1,630 lives and
$2.8 billion in economic costs and
$17.3 billion in comprehensive costs. Protective helmets have been shown to reduce the risk of death by up to 37% in motorcyclists [
1]. Due to the inherent nature of the activities, motorcyclists and bicyclists are at risk for multiple body injuries. Precautions such as protective helmets aim to limit the threat of injury. Many studies have shown the proven benefits of wearing protective helmets [
2,
3,
4,
5]. Specifically, many studies have shown that helmets reduce the odds of head and brain injuries by 63 to 88% and reduce the odds of upper and midface injuries by 65% in bicyclists [
2]. Despite this, laws and regulations requiring helmet use are not adopted by all states. Furthermore, the pattern of craniofacial skeletal trauma in these settings has not been well defined.
Helmets come in many different styles. One study observed that bicycle helmets helped prevent serious upper and middle facial injury, but did not result in fewer lower face injuries [
3]. Other data show that full-face motorcycle helmets provide a significant reduction in brain injury risk compared with an unprotected rider [
4]. Lopes Albuquerque et al. found that open-faced helmet riders had higher rates of traumatic brain injuries than closed-faced helmet riders, but openfaced and closed-faced helmets had similar facial injury severity scores (FISS) [
5]. Another study found that open-faced helmet riders were twice as likely to require an operation as those wearing full-faced helmets [
6].
To get further insight into the clinical outcomes and pattern of craniofacial skeleton trauma among helmeted and unhelmeted patients, we sought to review our institutional experience.
Methods
Patient Selection and Outcomes Measurement
After IRB approval, a retrospective review of electronic medical records of all trauma patients who presented to the Mayo Clinic Emergency Department (ED) and required level 1, level 2, or level 3 trauma activations was performed. The electronic medical records of trauma patients were queried for documented helmet wear or lack thereof at the time of accident and were included. A total of 417 patients who presented to the ED between January 1999 and September 2015 and had documented helmet use were included. Patients who died at the scene or before arrival to the ED were not captured.
Data involving patient demographics, age at injury, mode of injury, protective helmet wear at the time of injury, Glasgow Coma Score (GCS) at ED presentation, injury severity score (ISS), and need for hospitalization were collected. In addition, scalp lacerations and hematomas, skull and facial skeletal fractures, intracranial hemorrhage, need for surgical intervention, death after presentation to the ED, extracranial trauma, period of follow-up, and occurrence of traumatic brain injury (TBI) and need for rehabilitation during follow-up were evaluated.
The Mayo Classification for TBI severity was utilized [
3]. In brief, this system defines TBI as “traumatically induced injury that contributed to physiological disruption of brain function,” and assigns a mild TBI (probable), a symptomatic (possible) TBI, or a moderate-severe (definite) TBI based on several indicators. For example, a moderate-severe (definite) TBI is assigned if there was death due to the TBI, loss of consciousness of 30 min or more, posttraumatic antero-grade amnesia of 24 h or more, GCS <13 in the first 24 h, intracerebral hematoma, subdural hematoma, epidural hematoma, cerebral contusion, hemorrhagic contusion, penetrating injury, subarachnoid hemorrhage, or brain stem injury [
7]. All data were managed using REDCap (Research Electronic Data Capture) hosted at our institution [
8].
Statistical Analysis
Descriptive statistics were reported in the form of mean ± standard deviation (SD), median (interquartile range, IQR), or counts (percentages) as applicable. Associationsofhelmet wear with different studied outcomes were evaluated and summarized with odd ratios (OR) and 95% confidence intervals (CIs). Statistical analyses were performed using the JMP 10.0 version software package (SAS Institute, Cary, NC). All tests were two-sided and a p-value of <0.05 was considered significant.
Results
Demographics and Mode of Injury
A total of 417 patients were included (82% male). Median age at the time of injury was 22.9 years [IQR: 15.2–44.2]. Median duration of follow-up was 26 months ([IQR: 2.2–64.8]).
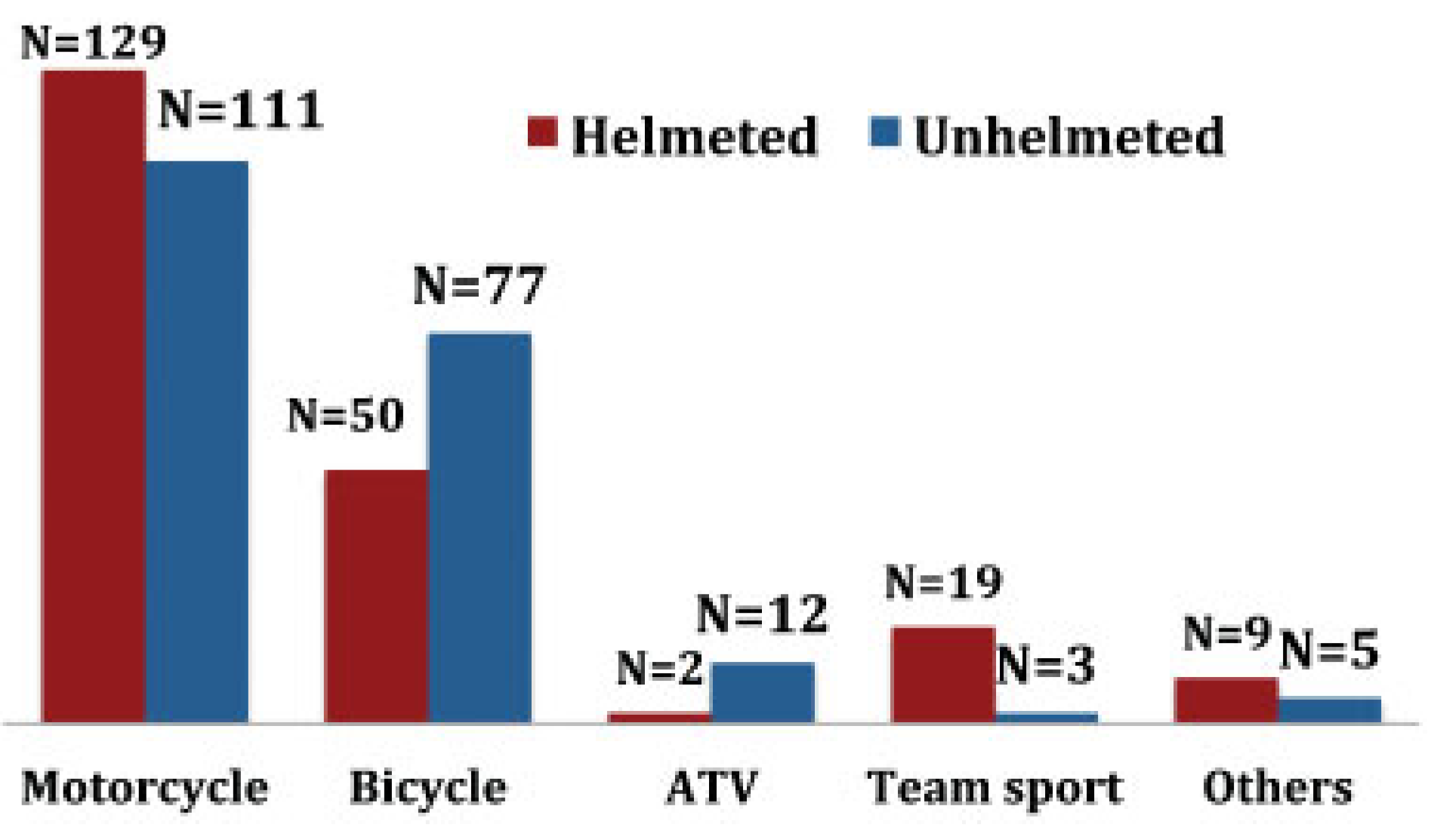
The majority of accidents involved cyclists (87.8%). Motorcycle accidents accounted for 57.6%, followed by bicycles (30.2%), contact sport-related accidents (5%), all-terrain vehicle (ATV)-related accidents (3.3%), and other modes of injury (3.9%) ([snowboard [
n = 8], snowmobile [
n = 4], fall from a horse [
n = 2], and skateboarding [
n = 1]). The majority of sport-related injuries involved football (
n = 16), followed by hockey (
n = 4) and baseball (
n = 1) (
Figure 1).
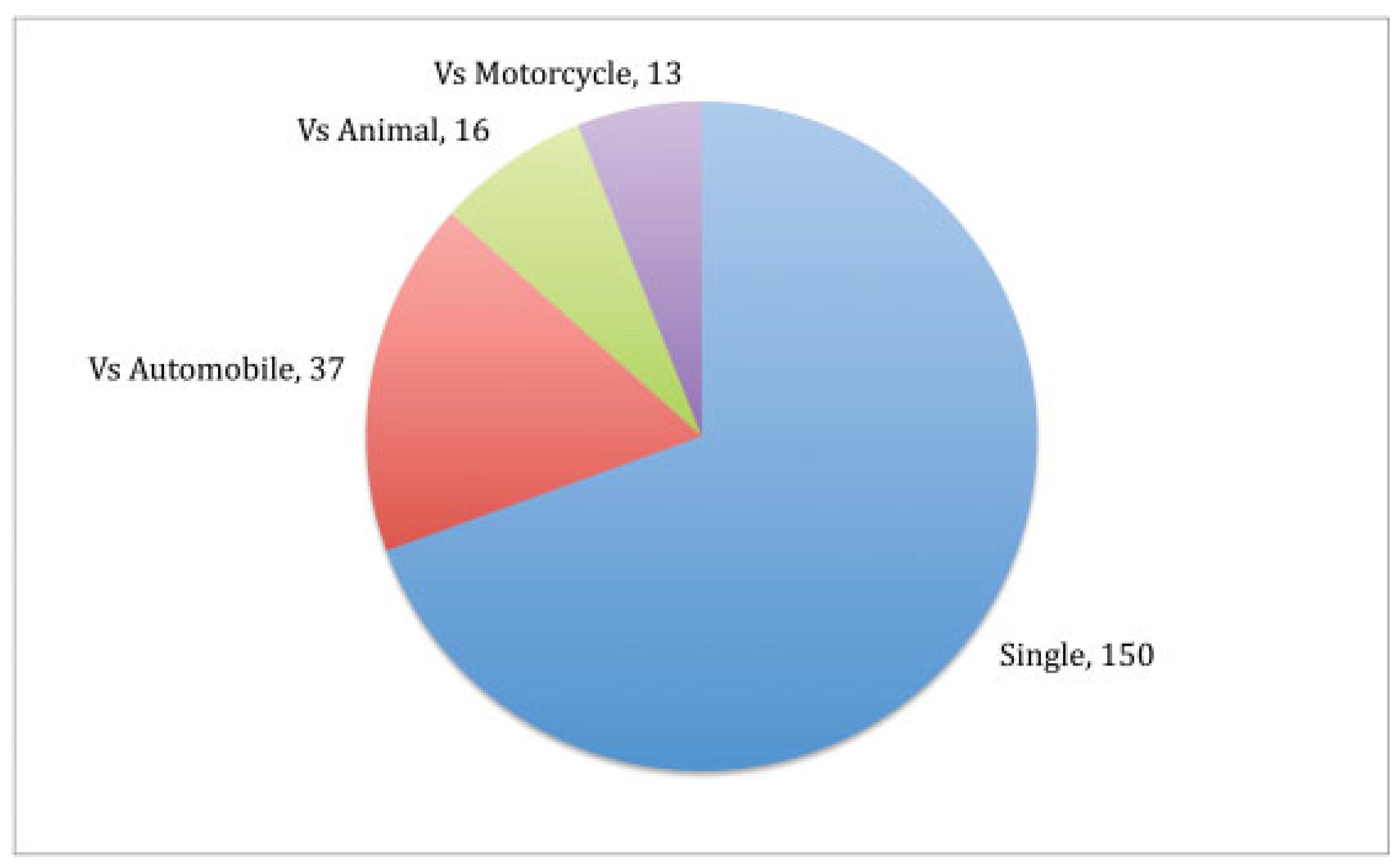
The most common mode of motorcycle injury was a single motorcyclist crash (due to intoxication, loss of control, or motorcycle malfunction;
n = 150, helmeted = 58.7%), followed by motorcycle versus automobile (
n = 37, helmeted = 29.7%), motorcycle versus animal (
n = 16, helmeted = 37.5%), and motorcycle versus motorcycle (
n = 13, helmeted = 92.3%) (
Figure 2).
Helmet Wear
At the time of injury, 209 (50%) patients were wearing a protective helmet. Age and gender were not associated with protective helmet use (p > 0.05).
Only 38.6% of bicyclists were wearing helmets (n = 49), compared with 53.8% of motorcyclists (n = 129, p = 0.0061).
Severity of Injury
Mean GCS at the time of presentation was 14.2 (SD ± 2.4). Difference in the mean GCS between helmeted and unhelmeted patients was not statistically significant (14.4 vs. 13.9,
p = 0.096). The mean Injury Severity Score (ISS) was 10.2 (SD 7.5). The difference in the mean ISS between helmeted and unhelmeted patients was not statistically significant (8.6 vs. 9.2,
p = 0.64). There was no difference in mean GCS between different modes of trauma. Motorcyclists and bicyclists presented with an average GCS of 14.1 and 14.5, respectively (
p = 0.08). However, patients involved in motorcycle accidents had statistically significant higher mean ISS compared with patients involved in sport-related accidents (11.1 vs. 5.0,
p = 0.048), bicycle accidents (11.1 vs. 8.4,
p = 0.015), and ATV accidents (11.1 vs. 6.5,
p = 0.048). The different types of injuries seen are outlined in
Table 1.
Hospital Admission, Length of Stay, In-hospital Mortality, and After-Dismissal Placement
A total of 247 (59%) patients required admission to the hospital (68% unhelmeted, 50.7% helmeted, p < 0.0001). Unhelmeted patients (n = 140, 68%) stayed in the hospital an average 2 days longer than helmeted patients (3.8 vs. 5.9 days, p = 0.0721).
Motorcyclists were more likely to be admitted to the hospital (74.4%, n = 177) compared with bicyclists (44%, n = 56, p < 0.0001). Additionally, motorcyclists’ length of stay was 5.9 days versus 2.6 days for bicyclists’ (p = 0.0207).
On discharge, only two helmeted patients required skilled nursing facility placement for long-term rehabilitation. The remainders were able to return home. Among unhelmeted patients, four required short-term rehabilitation facility placement, seven required skilled nursing facility placement for long-term rehabilitation, two were sent home with home health, one was sent to jail, and one required inpatient psychiatry admission. In-hospital mortality was 0.8% (2/247) and was confined to unhelmeted patients.
Patterns of Craniofacial Injuries
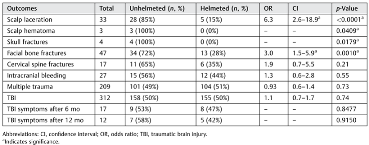
Scalp Laceration
A total of 33 patients (7.9%) sustained scalp lacerations (unhelmeted = 28, 84.8%) and 29 patients (unhelmeted, n = 25, 86.2%) required laceration repair. Eight patients (unhelmeted = 7, 87.5%) required scalp laceration repair in the operating room. Unhelmeted patients were more likely to sustain scalp lacerations compared with helmeted patients (RR = 5.6, p < 0.0001). There was no statistical difference in the incidence of scalp lacerations between motorcyclists (10.8%, n = 26) and bicyclists (6.4%, n = 8, p = 0.18).
Skull Fracture
Only four patients (1%) sustained skull fractures (motorcycle = 3, ATV = 1) as the result of the accident. All skull fractures occurred in unhelmeted patients (p = 0.0179). Only one skull fracture was open.
There was no statistical difference of incidence of skull fracture between motorcyclists (1.3%, n = 3) and bicyclists (0%, n = 0, p = 0.554).
Facial Fractures
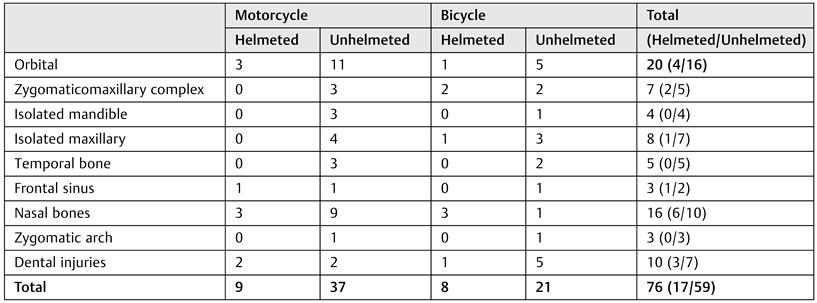
Forty-seven (11.3%) patients sustained 76 facial fractures (8% unhelmeted, 3% helmeted, OR = 3.0, 95% CI: 1.5–5.9,
p = 0.001). Thirteen out of 47 facial fractures (27.7%) required surgical repair. Eight out of these 13 (61.5%) patients were not wearing a protective helmet. A total of 14 patients (unhelmeted = 8, 57.1%) had bilateral facial fractures. The laterality of fractures did not differ between helmeted and unhelmeted patients (
p = 0.163). Sites and frequency of facial fractures between helmeted and unhelmeted patients are outlined in
Table 2.
There was no statistical difference in the incidence of facial fractures or laterality between motorcyclists (11.25%, n = 27) and bicyclists (15.0%, n = 19, p = 0.323).
Traumatic Brain Injury, Need for Rehabilitation, and Intracranial Hemorrhage
Loss of consciousness was reported in 232 (59%) patients and TBI was identified in 312 (75%) patients (mild in 150, moderate-severe in 21, and severity not documented in 141). There was no difference in TBI incidence between unhelmeted and helmeted patients (157 vs. 155, RR: 1.1, 95% CI: 0.7–1.07, p = 0.74). Among patients identified as having TBI at presentation or during admission, follow-up information at 6 months and 1 year after injury was available in 214 (92.2%) and 198 (85.3%) patients, respectively. Persistent symptoms of TBI at 6 months and 1 year were reported in 17 (8%) and 12 (6%) patients. Intracranial bleeding was reported in 27 patients (6.5%) (unhelmeted = 15, 55.5%). The most common type of intracranial bleeding was subdural (n = 11, 40.7%, unhelmeted = 8, 72.7%), subarachnoid (n = 10, 37.0% unhelmeted = 6, 60%), intraparenchymal (n = 9, 33.3% unhelmeted = 4, 44.4%), and epidural (n = 3, 11.1%, unhelmeted = 2, 66.7%). The most common mode of injury in patients diagnosed with TBI was motorcycle accidents (n = 17, 7.0% of total motorcycle accidents), followed by bicycle accidents (n = 8, 6.3% of total bicycle accidents), and ATV accidents (n = 8, 57.1% of all ATV accidents).
There was no statistical difference in the incidence of TBI between motorcyclists (72.1%, n = 173) and bicyclists (77.8%, n = 98, p = 0.234). Additionally, there was no statistical difference in intracranial bleeding between motorcyclists (7.1%, n = 17) and bicyclists (6.4%, n = 8, p = 0.78).
Cervical Spine Fractures
Cervical spine fractures were sustained in 17 patients (4.1%, unhelmeted = 11, 64.7%). The most common mode of cervical spine injuries was associated with motorcycle accidents (n = 15, 88.2%, unhelmeted = 10, 58.8%), followed by bicycle accidents (n = 2, 11.8%). The most common level of C-spine injury was C-7 (n = 8), followed by C-6 (n = 7). Incidence of cervical spine fracture did not differ between helmeted and unhelmeted patients (p > 0.05).
Motorcyclists had statistically significant higher rates of cervical spine fractures (6.3%, n = 15) compared with bicyclists (1.57%, n = 2, p = 0.0275).
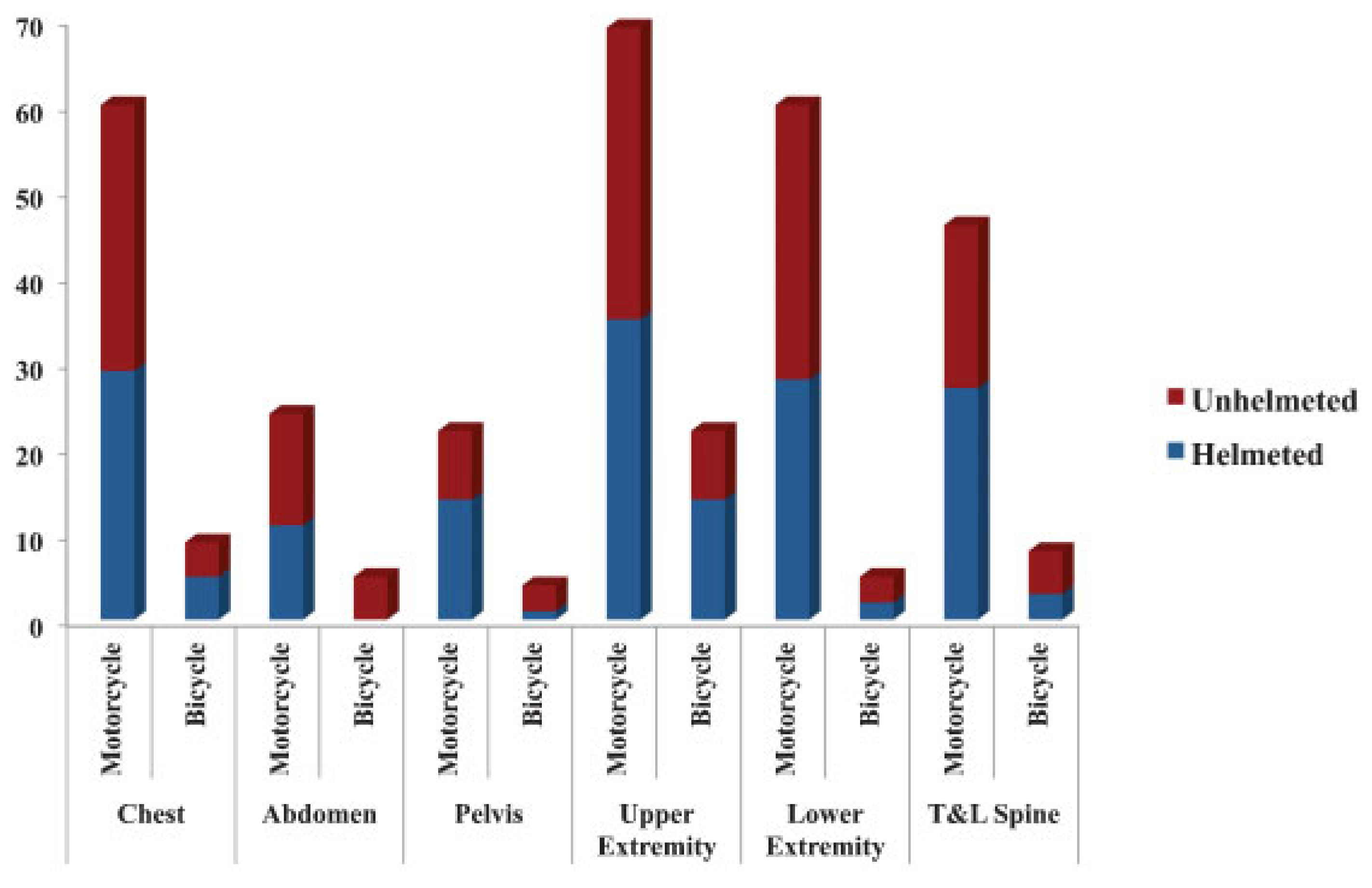
Extracranial Trauma (Chest, Abdomen, Pelvis, Thoracolumbar Spine, and Extremities)
Multitrauma was noted in 205 (49.3%) patients (unhelmeted = 100,
p = 0.69). The most common mode of injury in patients who sustained multiple sites of trauma was motorcycle accidents (77%) followed by bicycles (18%) and ATV (3%). Sport-related accidents and snowmobile accidents comprised 1% each. No statistical difference in multitrauma patients was seen between helmeted and unhelmeted patients (
Figure 3).
Motorcyclists had statistically significant higher rates (65.8%, n = 158) of extracranial trauma compared with bicyclists (30.2%, n = 38, p < 0.0001).
Discussion
Despite the presence of recent reports addressing trauma outcomes and costs of health care among helmeted and unhelmeted patients [
2,
3,
4,
5,
7], only 19 states have universal helmet laws that require all motorcyclists to wear helmets at the time of preparation of this article. Twenty-eight states require some motorcyclists to wear helmets, and three states (New Hampshire, Illinois, and Iowa) have no laws regarding motorcycle helmet use [
9]. Additionally, there are only 21 states with laws that require bicyclists under a certain age to wear helmets. Twenty-nine states have no bicycle law [
10]. The state of Minnesota had a universal helmet law in the past, but it was repealed in 1977. Current Minnesota laws require helmet use in motorcyclists with a permit or motorcyclists younger than 18 years. Additionally, the state of Minnesota does not have a law requiring bicycle helmet use, despite being ranked second in the nation as a “Bicycle Friendly State.” [
11].
In our study, the median age at injury was 22.9 years and 88% of these injuries were related to motorcycle or bicycle accidents, which underpins the relatively young age group at risk in recreational and sports cycling accidents [
12]. In addition, the relatively low percentage of helmet wearers (50%) reflects the need for state and national legislation to implement helmet laws for riders. A recent literature review of 12 studies involving many different helmet-associated activities showed that while there is strong evidence to support the efficacy of helmet use against severe intracranial injury, the majority of published studies did not show a statistically significant association between helmet use and reduction in concussion incidence and symptoms [
13]. The lack of difference between the two groups could represent selection bias, underpowered design of the studies, and lack of standardization as patients with less severe head injuries are more likely to survive the initial trauma and may not seek further medical care.
Despite the similarities in GCS, ISS, and TBI scores between helmeted and unhelmeted patients, unhelmeted patients were more likely to require admission to the hospital, stay longer in the hospital, require out-of-home placement after dismissal, sustain scalp lacerations and hematomas, and sustain facial and skull fractures than their helmeted counterparts. The lower incidence of the aforementioned events among helmeted patients, despite the similarities in ISSs among cyclists, indicates that the protective role of helmet wear cannot be ignored. Several reports revealed the protective effect of helmets against facial and brain injury, but the patterns of facial fractures were less clearly defined.14–16 In this study, we identified a pattern of facial fractures by site and mode of injury between helmeted and unhelmeted patients, a finding that will be helpful in assessing different helmet types on the pattern of facial injuries in future studies.
In our series, only 27 patients had intracranial bleeding, and no statistical significance was associated with helmet use. This finding is likely due to the small sample size of our study and selection bias as the helmet status of riders who had significant intracranial bleeding and died at the scene of the accident was not captured in our study. Rostas et al. reported a decrease in the odds ratio of intracranial hemorrhage from 22% to 3.5% with helmet use in ATV accidents [
17]. Similarly, the effect of helmet use on head and facial injury reduction in bicyclists was recently reported in a metaanalysis. The authors included 40 studies in the meta-analysis (64,000 injured cyclists) and reported the odds ratio of severe and fatal head injuries in helmeted bicyclists to be =0.31 and =0.35, respectively [
18]. Therefore, we believe that wearing a protective helmet in cyclists is beneficial in reducing severe head injury and intracranial hemorrhage.
There were no differences between the helmeted and unhelmeted patient population and the rates of cervical spine fractures. A recent single institution’s review of more than 1331 patients and 135 cervical spine injuries found no significant decrease in risk or severity of C-spine fractures with helmet use [
19]. However, a national trauma database review found that helmeted motorcyclists were less likely to suffer cervical spine injury in crashes [
20]. As expected, there was no difference in multiple site traumas (chest, abdomen, pelvis, thoracolumbar spine, and extremities) between helmeted and unhelmeted patients.
When comparing multiple state data, states with universal helmet laws for motorcyclists had increased reported helmet use from 42 to 88%; hospital costs and injuries to the brain, head, and face were higher in partial law states. Median charges for emergency department visits in states with partial helmet laws were
$1,987 compared with
$1443 for states with universal helmet laws. Median inpatient costs in partial law states were
$31,506, whereas inpatient costs for states with universal helmet law were
$25,949 [
21]. A recent study showed that helmet use in different recreational vehicles decreased hospital admission rates (50.7% vs. 59.5%), decreased admission to the ICU (25% vs. 35%), decreased length of hospital stay, and had lower readmission rates [
22]. Another national study showed that unhelmeted patients had higher rates of admission (39.9 vs.% 32.8%) with longer duration of hospital stay. Furthermore, unhelmeted motorcyclists incurred an estimated
$3056 more in hospital charges than helmeted patients [
23].
Different countries have different traffic legislations and helmet laws. The use of helmets in cyclists was mandated in Australia and New Zealand [
24,
25]. Despite multiple studies demonstrating clear reduction in head injuries after mandatory helmet laws (MHL), opponents of MHL argue that MHL may decrease participation rates in public bike-sharing programs and potentially may lead to under participation in cycling. Despite this ongoing debate, the benefits of wearing a protective helmet in all cyclists cannot be overlooked and the impact of head injury on the quality of life on injured cyclists and its societal cost cannot be understated [
26]. Several limitations apply to this study. This is a retrospective study, and therefore we relied on correct diagnosis codes and documentation from emergency department physicians, residents, and primary care providers. We relied on the physicians to correctly diagnose and grade traumatic brain injuries. Additionally, we captured only 417 patients and due to the small sample size, some injuries, such as intracranial bleeding, were likely underrepresented and our data lacked statistical power to prove significance. Additionally, there were potential confounders that we could not adjust for or capture such as speed at thetime of injury, helmet type (partial or full-face), and alcohol and illicit substance use at the time of injury. Moreover, the higher GCS in the majority of patients may indicate that patients with severe injuries may have died on thescene. Our study did not capturethis patient population. Despite these limitations, our study has demonstrated key differences in the frequency, pattern, and impact of craniofacial injuries among helmeted and unhelmeted patients and provides a unique contribution to the literature.