Abstract
Encephalocele is defined as protrusion of cranial contents beyond the normal confines of the skull. Although most encephalocele cases have a congenital etiology, fractures of the skull base can cause traumatic encephalocele. In most encephalocele cases, the bone defect presents reduced dimensions and the endoscopic treatment is generally performed to reconstruct the area using mucosal and/or fat grafts. This article sought to report on a rare case of traumatic encephalocele associated with an extensive defect of the anterior skull base. This case was treated via transcranial access, and reconstruction was performed using titanium mesh in conjunction with a pericranium flap.
Encephaloceles are didactically defined as herniation of the brain or meninges (meningoencephalocele) through a skull base defect and are classified according to the anatomical position of these bone defects [1,2].
These anomalies can be congenital or acquired secondary to tumor, hydrocephalus, or develop spontaneously. Ence-phaloceles associated with fractures of the skull base (basal fractures) are relatively rare and occur in patients who have suffered facial trauma [2]. They can be associated with dura mater injuries, frontal sinus fractures, sinusitis, pulsatile or nonpulsatile proptosis, orbital apex syndrome, cerebrospinal fluid (CSF) leaks, and meningitis [3].
The therapeutic choices for traumatic encephaloceles can be performed via intraor extracranial access, depending on the anatomy of the fistula and the defect [4]. Treatment objectives include surgical reconstruction of the skull base, prevent cranial deformities, seal CSF leaks, and prevent chronic sinusitis [4].
The choice of the reconstruction technique has not been clearly established, particularly with respect to the kind of the material [5]. Numerous local and distant pedicled flaps have been described for these purposes; however, in larger defects, these flaps may not provide structural support for the size of the bony defect [5]. Bone grafts are optimally biocompatible; however, due to problems with bone resorption and recurrence, titanium plates have been reported [6]. In these cases, the association of a titanium mesh with soft-tissue flaps (sandwich technique) has been described to restore a three-dimensional (3D) contour in defects with poor recipient bed from repeated infection, bone destruction, multiple surgeries, or previous radiation [5,7].
Therefore, this study sought to report on a case of large traumatic encephalocele associated with a CSF leak, dura mater injury, and an extensive bone defect of the anterior skull base. The treatment was performed with dura mater repair and reconstruction of the cranial anterior base with titanium mesh in conjunction with a pericranium flap.
Case Report
A 26-year-old male patient with a history of motorcycle accident presented with trauma in the naso-orbital-ethmoid region. The patient’s Glasgow coma scale score was 13/15 upon admission to the emergency room. Clinical examinations revealed CSF rhinorrhea, frontonasal sinking, and anosmia (Figure 1a). Computed tomography (CT) demonstrated multiple facial fractures, skull base defect in the cribriform plate region, and fractures of the posterior wall of the frontal sinus (Figure 1b–d and Figure 2a–c).
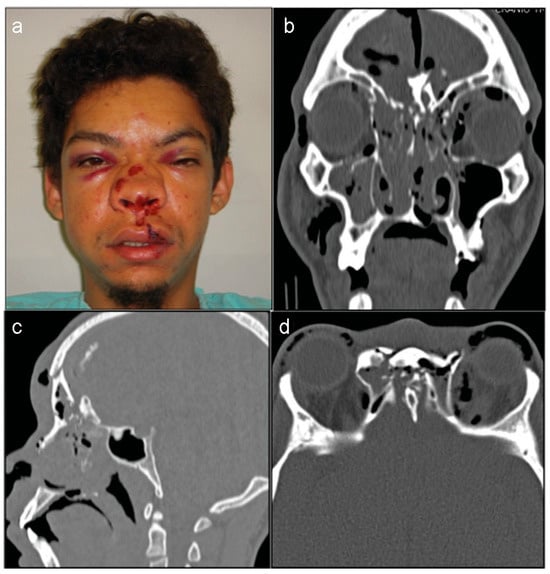
Figure 1.
(a) A 26-year-old male patient with CSF rhinorrhea, frontonasal sinking caused by a motorcycle accident. (b–d) Computed tomo-graphic scans showed a facial fractures, skull base defect in the cribriform plate region.
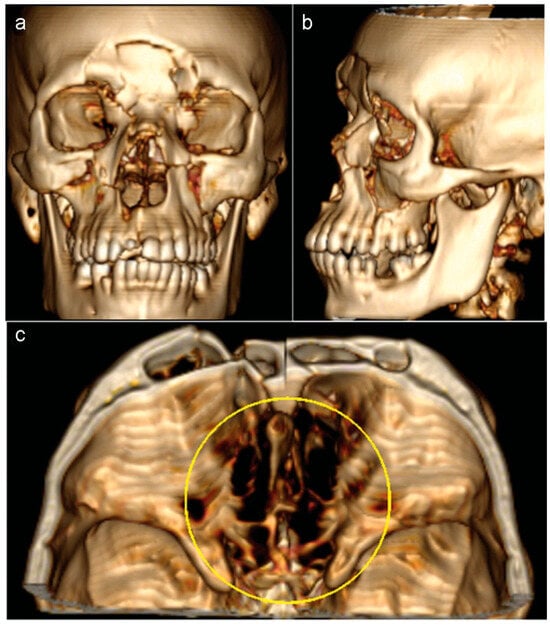
Figure 2.
(a,b) Three-dimensional volume rendering images showing the forehead deformity and retrusion. (c) The size of the skull base defect.
The proposed surgical treatment aimed at reducing fractures and correcting the dura mater injuries. After anesthesia was induced, antibiotic prophylaxis was made with cefuroxime and clindamycin, and a lumbar catheter was installed to shunt CSF externally, reduce the intra dural CSF, and allow the anterior cranial base view by the brain retraction.
After that, due to the need for visualization and correction of both dura mater and the fractures, the procedure was performed via bicoronal access, involving the opening of a pericranial flap and a bifrontal craniotomy (Figure 3a). The craniotomy allowed a subfrontal approach and the immediate visualization of dura mater injuries.
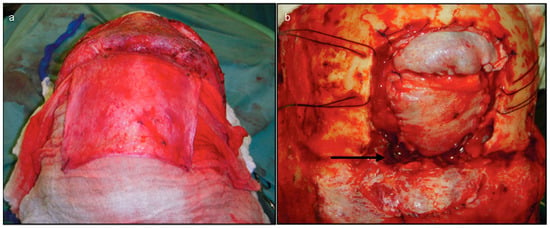
Figure 3.
(a) The procedure started with coronal approach, dissection of the loose areolar tissue layer between galea and pericranium. Opening of the pericranial flap that will be the soft-tissue layer above the bony anterior skull base. (b) The frontal craniotomy was performed and the dura mater corrected with galea aponeurotica from parietal region. Note the bone defect below the brain (black arrow).
Subsequently, the anterior portion of the brain was gently retracted to correct dura mater injuries with primary sutures and soft-tissue graft. In this occasion, a repair was performed using only soft tissue like galea aponeurotica from the parietal region (Figure 3b). The supraorbital portion of the craniotomy was replaced and the pericranial flap was used to cover the skull base defect (Figure 4a). Cranialization of the frontal sinus was done, and the remaining mucosa was removed to avoid mucoceles. The superior portion of the craniotomy was fixed with 1.5-mm titanium plates and mesh (Figure 4b–d).
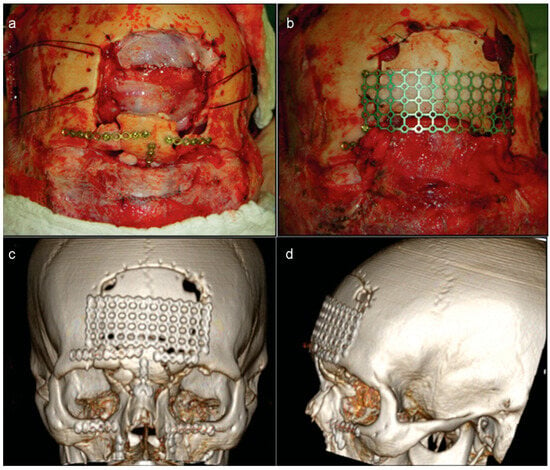
Figure 4.
(a) The supraorbital portion of the craniotomy was replaced. (b) The pericranial flap covered the skull base defect and the remaining craniotomy was set above the flap. (c and d) Three-dimensional volume rendering images showing the forehead reestablishment using cranial mesh.
After 5 days of the procedure, the lumbar drain was removed and the patient was discharged on the sixth day. Some authors recommend keeping the lumbar drain for 5 to 7 days after complex reconstructive procedures and to continue antibiotic therapy. These measures allow the repair of the dura mater and the pericranium flap properly [7].
After 18 days, the same patient returned with pulsatile headache, dizziness, and nausea. Besides this clinical sign, a new CT scan revealed a large encephalocele associated with an extensive defect of the anterior skull base (Figure 5a–d).
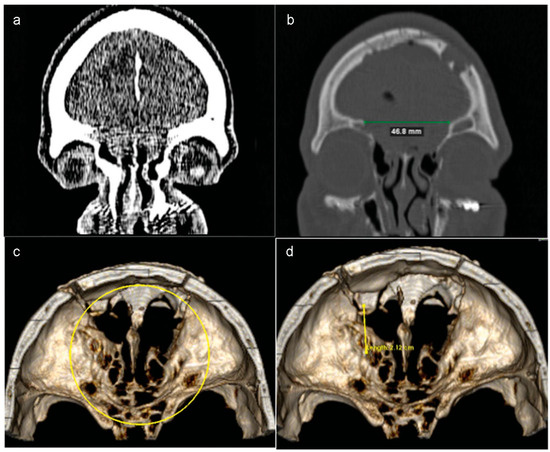
Figure 5.
(a and b) Eighteen days after the procedure, the patient returned and a new CT scan revealed a large encephalocele. The protrusion of the brain through the nasal cavity was associated with an extensive defect of the anterior skull base. (c and d) Three-dimensional volume rendering images showed that the osseous defect had increased after first surgery.
Faced with this diagnosis and due to a large bilateral bone defect, another surgery was proposed to reconstruct the bone defect and reduce the protrusion of the brain using “sandwich” technique (Figure 6a). This technique aims to cover the defect and reinforce the anterior cranial base using local or free flaps with a tailored piece of titanium mesh, respectively.
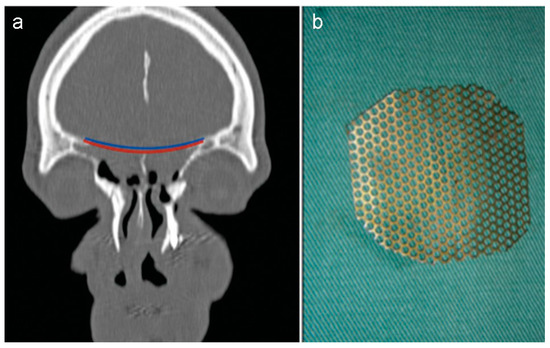
Figure 6.
(a) The planning of the reconstruction included the placement of a pericranial flap (red layer) on the defect, the titanium mesh (blue layer). (b) The titanium mesh was contoured previously for a more accurate implant.
Before the second procedure, the dimensions of bone defect were measured using 3D computer software and the titanium mesh contoured for a more accurate implant (Figure 6b). Thus, the operation was planned as shown in Figure 7. The planned reconstruction started with the same steps of the first procedure. Then, the contoured mesh was placed over the anterior skull base defect with the help of 4-mm screws (Figure 8a,b).
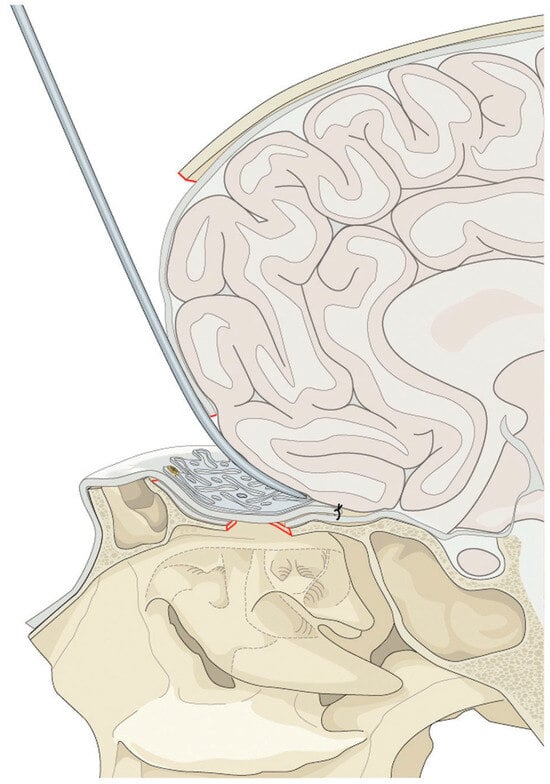
Figure 7.
The pericranial flap is brought in to reline the bone defect of the anterior skull base. The flap should be sutured to the dura to eliminate dead space. The titanium mesh is placed with a screw on the frontal bone over the pericranial flap to reinforce the reconstruction.
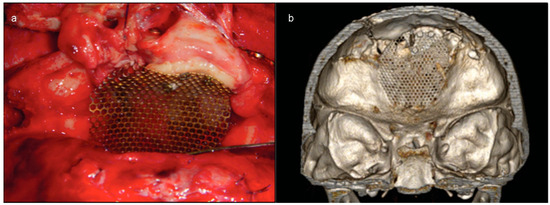
Figure 8.
(a) The contoured mesh placed over the anterior skull base defect with the help of 4-mm screws. After that, the mesh was removed, the pericranial flap lined the skull base, and the mesh returned to position above the flap. (b) Three-dimensional volume rendering images showed a good position of the mesh.
After that, due to the need of pericranial flap under the implant, the mesh was removed and the supraorbital portion of the craniotomy was replaced. The next step consisted of interposition of the pericranium flap between the bone defect and the dura mater (with primary sutures) and finally, the mesh was fixed above the pericranium ensuring the complete sealing of the defect and a watertight closure. After that, the remaining craniotomy was fixed with a titanium mesh and 4-mm screws.
Following this second operation, the patient remained in the hospital receiving antibiotics (cefuroxime and clindamycin) for 5 days and a postoperative CT revealed that with support from the titanium mesh, the anterior skull base had been successfully reconstructed (Figure 9a–c). The patient was discharged on the sixth day and exhibited good postoperative recovery, with no episodes of pulsatile headache, dizziness, and nausea (Figure 10). A 12-month postoperative CT did not demonstrate any alterations (Figure 11a–c).
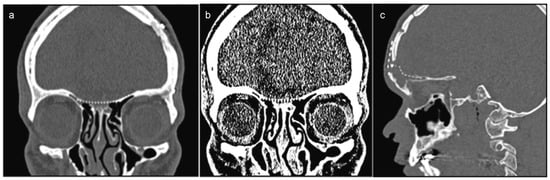
Figure 9.
(a–c) Postoperative result of CT scan shows separation of the brain from the nasal cavity with the help of the mesh.

Figure 10.
Postoperative frontal view showing the good aesthetic appearance and no functional sequelae.
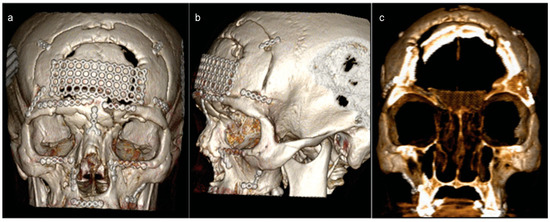
Figure 11.
(a and b) Three-dimensional (3D) volume rendering images showing the second wider craniotomy. (c) A coronal cut of 3D volume rendering evidencing good position of the mesh.
Discussion
Traumatic encephaloceles are rare conditions that typically occur in patients with skull base fractures or arise iatrogenically after a sinonasal procedure. These encephaloceles can cause brain herniation in paranasal sinuses and the nasal region [8,9]. Approximately 5% of patients with frontobasal fractures can have encephalocele [2].
The basic treatment approach involves promoting the “waterproof” sealing of the defect. For the repair of certain defects, this objective may be achieved by utilizing free grafts or flaps for endoscopic reconstruction [8,9]. The endoscopic approach should also be used in cases where the olfactory function is preserved after the trauma to avoid injury to the olfactory nerve [7]. However, defects that are large or involve the orbital roof can be repaired with bone grafts or titanium mesh via the transcranial or subcranial route [2,4,7,10].
The transcranial approach is commonly performed through a bicoronal incision for a frontal craniotomy. This is advantageous because intracranial injuries can also be dealt with at the same time [11]. After performing this approach, the pericranial flap is dissected from the outer layer of the skull [7]. Next, as in this case, the realization of a bifrontal craniotomy allows the retraction of both frontal lobes and exposes the anterior skull base. The presence of preoperative anosmia allowed the complete release of dura around the crista galli exposing the cribriform plate and the cranial defect [7].
The “sandwich” technique associates the soft-tissue flap with titanium mesh and allows an anatomical reconstruction of the bone defect. In addition, it ensures adequate separation of the brain from the nasal cavity and can be used safely in large skull base defects with low risk of infection [5,7].
Numerous local and distant pedicled flaps have been described for these purposes with some success. Reconstruction with vascularized tissue transfer has become a preferred treatment for many large skull base defects [5]. In most cases, the pericranium flap can be used safely to cover the anterior skull base as much as possible [7]. For this purpose, the pericranium flap must be dissected carefully to avoid tearing of the tissue and jeopardizing treatment. In cases of recurrent infections, multiple surgeries, or previous radiation, the anterior skull base reconstruction requires a fascia lata graft or even a radial forearm free flap [5,7].
Authors used with success titanium mesh/radial forearm flap for reconstruction of large skull base defects in patients with poor recipient bed [5].
In the past, bone grafts have been the mainstay of repair of large defects. Bone grafts are optimally biocompatible and radiopaque, have a smooth surface from which periorbita can be easily dissected in secondary reconstruction, and have no additional cost [6,10,11]. The disadvantages are longer operating time, additional donor site (calvarium, ribs, iliac crest) with the attendant morbidity, and increased operating time and chances of resorption. As a result of the concern for bone graft resorption, titanium plates have been reported for reconstruction of the orbit [5,6,10,11].
The ease with which titanium mesh may be adapted to the conditions present in traumatic encephalocele cases allows for the 3D reconstruction of traumatized areas, even if it contacts the paranasal sinuses and dura mater [10,11]. Shaped titanium mesh can be very effective in reconstructing the defect without the increased risk of resorption.
Conclusion
The treatment of traumatic encephaloceles associated with extensive skull base defects can be performed using titanium mesh and pericranium flap properly and safely. This technique represents an alternative to bone grafts and produce highly functional results with re-establishment of the anatomy of the region.
References
- Secci, F.; Consales, A.; Merciadri, P.; et al. Naso-ethmoidal encephalocele with bilateral orbital extension: Report of a case in a western country. Childs Nerv. Syst. 2013, 29, 1947–1952. [Google Scholar] [PubMed]
- Morihara, H.; Zenke, K.; Shoda, D.; Fujiwara, S.; Suehiro, S.; Hatakeyama, T. Intraorbital encephalocele in an adult patient presenting with pulsatile exophthalmos. Case report. Neurol. Med. Chir. 2010, 50, 1126–1128. [Google Scholar]
- Martello, J.Y.; Vasconez, H.C. Supraorbital roof fractures: A formidable entity with which to contend. Ann. Plast. Surg. 1997, 38, 223–227. [Google Scholar] [CrossRef] [PubMed]
- Ailawadhi, P.; Agrawal, D.; Mahapatra, A.K. Novel treatment of traumatic CSF rhinnorhea using titanium mesh and onlay graft. J. Pediatr. Neurosci. 2010, 5, 25–26. [Google Scholar] [PubMed]
- Biron, V.L.; Gross, M.; Broad, R.; Seikaly, H.; Wright, E.D. Radial forearm free flap with titanium mesh sandwich reconstruction in complex anterior skull base defects. J. Craniofac Surg. 2012, 23, 1763–1765. [Google Scholar] [PubMed]
- Dale, E.L.; Strait, T.A.; Sargent, L.A. Orbital reconstruction for pulsatile exophthalmos secondary to sphenoid wing dysplasia. Ann. Plast. Surg. 2014, 72, S107–S111. [Google Scholar] [PubMed]
- König, S.A.; Ranguis, S.; Gramlich, V.; Spetzger, U. Reconstruction of the anterior skull base after major trauma or extensive tumour resection. Acta Neurochir. 2015, 157, 139–144. [Google Scholar] [PubMed]
- Boseley, M.E.; Tami, T.A. Endoscopic management of anterior skull base encephaloceles. Ann. Otol. Rhinol. Laryngol. 2004, 113, 30–33. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.J.; Chang, P.H.; Huang, C.C.; Chuang, C.C. Endoscopic treatment of traumatic basal encephaloceles: A report of 8 cases. J. Neurosurg. 2008, 108, 729–735. [Google Scholar] [PubMed]
- Kuttenberger, J.J.; Hardt, N. Long-term results following reconstruction of craniofacial defects with titanium micro-mesh systems. J. Craniomaxillofac Surg. 2001, 29, 75–81. [Google Scholar] [PubMed]
- Mokal, N.J.; Desai, M.F. Titanium mesh reconstruction of orbital roof fracture with traumatic encephalocele: A case report and review of literature. Craniomaxillofac Trauma. Reconstr. 2012, 5, 11–18. [Google Scholar] [CrossRef] [PubMed]
© 2016 by the authors. The Author(s) 2016.