Immediate Surgical Management of Traumatic Dislocation of the Eye Globe into the Maxillary Sinus: Report of a Rare Case and Literature Review
Abstract
- One was enucleated 2 months after misdiagnosis as traumatic enucleation [32].
Acknowledgments
References
- Pelton, R.W.; Rainey, A.M.; Lee, A.G. Traumatic subluxation of the globe into the maxillary sinus. AJNR Am. J. Neuroradiol. 1998, 19, 1450–1451. [Google Scholar] [PubMed]
- Ahmad, F.; Kirkpatrick, W.N.; Lyne, J.; Urdang, M.; Garey, L.J.; Waterhouse, N. Strain gauge biomechanical evaluation of forces in orbital floor fractures. Br. J. Plast. Surg. 2003, 56, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Jellab, B.; Baha, A.T.; Moutaouakil, A.; et al. Management of a severe cranio-orbito-facial trauma with a dislocation of the globe into the maxillary sinus. Bull. Soc. Belge. Ophtalmol. 2008, 309–310, 37–41. [Google Scholar]
- Amaral, M.B.; Carvalho, M.F.; Ferreira, A.B.; Mesquita, R.A. Traumatic globe luxation associated with orbital fracture in a child: A case report and literature review. J. Maxillofac. Oral. Surg. 2015, 14 (Suppl. S1), 323–330. [Google Scholar] [CrossRef] [PubMed]
- Morris, W.R.; Osborn, F.D.; Fleming, J.C. Traumatic evulsion of the globe. Ophthal Plast. Reconstr. Surg. 2002, 18, 261–267. [Google Scholar] [CrossRef]
- Kreiner, B.; Amer, R.; Sharfi, G.; Solomon, A.; Ilsar, M. Traumatic displacement of the globe into the paranasal sinuses: Case report and guidelines for treatment. J. Oral. Maxillofac. Surg. 2008, 66, 826–830. [Google Scholar] [CrossRef]
- Reuling, F.H.; Hadlund, R.L. Traumatic luxation of the globe. Eye Ear Nose Throat Mon. 1970, 49, 129–130. [Google Scholar]
- Pillai, S.; Mahmood, M.A.; Limaye, S.R. Complete evulsion of the globe and optic nerve. Br. J. Ophthalmol. 1987, 71, 69–72. [Google Scholar] [CrossRef] [PubMed]
- van der Wal, K.G.; van der Pol, B.A. Traumatic luxation of the eyeball. J. Craniomaxillofac Surg. 1991, 19, 205–207. [Google Scholar] [CrossRef]
- Zengin, N.; Karakurt, A.; Gültan, E.; Kural, G. Traumatic globe luxation. Acta Ophthalmol. 1992, 70, 844–846. [Google Scholar] [CrossRef]
- Arkin, M.S.; Rubin, P.A.; Bilyk, J.R.; Buchbinder, B. Anterior chiasmal optic nerve avulsion. AJNR Am. J. Neuroradiol. 1996, 17, 1777–1781. [Google Scholar] [PubMed]
- Kiratli, H.; Tümer, B.; Bilgiç, S. Management of traumatic luxation of the globe: A case report. Acta Ophthalmol. Scand. 1999, 77, 340–342. [Google Scholar] [CrossRef]
- Bajaj, M.S.; Kedar, S.; Sethi, A.; Gupta, V. Traumatic globe luxation with optic nerve transection. Orbit 2000, 19, 165–170. [Google Scholar] [CrossRef]
- Alp, B.; Yanyali, A.; Elibol, O.; Talu, H.; Karabas, L. A case of traumatic globe luxation. Eur. J. Emerg. Med. 2001, 8, 331–332. [Google Scholar] [CrossRef] [PubMed]
- Bajaj, M.S.; Pushker, N.; Nainiwal, S.K.; Balasubramanya, R. Traumatic luxation of the globe with optic nerve avulsion. Clin. Experiment Ophthalmol. 2003, 31, 362–363. [Google Scholar] [CrossRef]
- Song, A.; Carter, K.D. Bilateral traumatic globe subluxation. Ophthal Plast. Reconstr. Surg. 2006, 22, 136–137. [Google Scholar] [CrossRef]
- Lelli, G.J., Jr.; Demirci, H.; Frueh, B.R. Avulsion of the optic nerve with luxation of the eye after motor vehicle accident. Ophthal Plast. Reconstr. Surg. 2007, 23, 158–160. [Google Scholar] [CrossRef]
- de Saint Sardos, A.; Hamel, P. Traumatic globe luxation in a 6-year-old girl playing with a tube of wrapping paper. J. AAPOS 2007, 11, 406–407. [Google Scholar] [CrossRef] [PubMed]
- Roldan-Valadez, E.; Corona-Cedillo, R.; Rojas-Marin, C.; Valdivieso Cardenas, G.; Sanchez-Sanchez, J.M.; Quiroz-Mercado, H. Tomographic findings in traumatic globe evulsion caused by blunt head trauma. Br. J. Radiol. 2007, 80, e247–e249. [Google Scholar] [CrossRef]
- Shimia, M.; Sayyahmelli, S. Traumatic Displacement of the Globe into Brain. RMJ 2009, 34, 234–235. [Google Scholar]
- Vahdati, S.S.; Sadeghi, H. Orbital roof fracture: Dislocation of globe into the anterior cranial fossa. JAEMCR 2011, 2, 47–49. [Google Scholar] [CrossRef]
- Gollapudi, P.R.; Nandigama, P.K.; Maila, S.K.; Karla, R.; Kotakadira, S. Traumatic intracranial prolapse of eye ball—A case report. Br. J. Neurosurg. 2013, 27, 114–116. [Google Scholar] [CrossRef] [PubMed]
- Risco, J.M.; Stratas, B.A.; Knott, R.H. Prolapse of the globe into the ethmoid sinus. Am. J. Ophthalmol. 1984, 97, 659–660. [Google Scholar] [CrossRef] [PubMed]
- Moon, M.; Pietris, G.; Shapter, M. Dislocation of the globe into the ethmoid sinuses. Aust. N. Z. J. Ophthalmol. 1997, 25, 175–176. [Google Scholar] [CrossRef]
- Kang, B.D.; Jang, M.H. A case of blowout fracture of the orbital wall with eyeball entrapped within the ethmoid sinus. Korean J. Ophthalmol. 2003, 17, 149–153. [Google Scholar] [CrossRef]
- Okabe, H.; Kimura, K.; Sonoda, S.; Sakamoto, T. Displacement of globe into ethmoid sinus by orbital medial wall fracture with good recovery of vision. Jpn. J. Ophthalmol. 2005, 49, 426–428. [Google Scholar] [CrossRef]
- Tranfa, F.; Di Matteo, G.; Di Salle, F.; Strianese, D.; Bonavolontà, G. Traumatic displacement of the globe into the ethmoid sinus. Am. J. Ophthalmol. 2000, 130, 253–254. [Google Scholar] [CrossRef]
- Berkowitz, R.A.; Putterman, A.M.; Patel, D.B. Prolapse of the globe into the maxillary sinus after orbital floor fracture. Am. J. Ophthalmol. 1981, 91, 253–257. [Google Scholar] [CrossRef]
- Smit, T.J.; Koornneef, L.; Zonneveld, F.W. A total orbital floor fracture with prolapse of the globe into the maxillary sinus manifesting as postenucleation socket syndrome. Am. J. Ophthalmol. 1990, 110, 569–570. [Google Scholar] [CrossRef]
- Ziccardi, V.B.; Patterson, G.T.; Ramasastry, S.; Sotereanos, G.C. Management of a severe zygomatico-orbital fracture with dislocation of the globe into the antrum. J. Craniofac Surg. 1993, 4, 95–101. [Google Scholar] [CrossRef]
- Tung, T.C.; Chen, Y.R.; Santamaria, E.; Chen, C.T.; Lin, C.J.; Tsai, T.R. Dislocation of anatomic structures into the maxillary sinus after cranio-facial trauma. Plast. Reconstr. Surg. 1998, 101, 1904–1908. [Google Scholar] [CrossRef]
- Saleh, T.; Leatherbarrow, B. Traumatic prolapse of the globe into the maxillary sinus diagnosed as traumatic enucleation of the globe. Eye 1999, 13 Pt 5, 678–680. [Google Scholar] [CrossRef] [PubMed]
- Avadhanam, V.S.; Sreedhara, S.P.; Ameerally, P.; El-Ghazali, K.M.S. Traumatic globe dislocations-Significance of early intervention. Inj. Extra 2008, 39, 356–358. [Google Scholar] [CrossRef][Green Version]
- Kim, S.; Baek, S. Traumatic dislocation of the globe into the maxillary sinus associated with extraocular muscle injury. Graefes Arch. Clin. Exp. Ophthalmol. 2005, 243, 1280–1283. [Google Scholar] [CrossRef] [PubMed]
- Abrishami, M.; Aletaha, M.; Bagheri, A.; Salour, S.H.; Yazdani, S. Traumatic subluxation of the globe into the maxillary sinus. Ophthal Plast. Reconstr. Surg. 2007, 23, 156–158. [Google Scholar] [CrossRef]
- Müller-Richter, U.D.; Kohlhof, J.K.; Driemel, O.; Wagener, H.; Reichert, T.E. Traumatic dislocation of the globe into the maxillary sinus. Int. J. Oral. Maxillofac. Surg. 2007, 36, 1207–1210. [Google Scholar] [CrossRef]
- Ramstead, C.; McCabe, J.; Alkahtani, M.; Leong-Sit, J.; Morhart, M. Traumatic dislocation of the globe into the maxillary sinus. Can. J. Ophthalmol. 2008, 43, 364–366. [Google Scholar] [CrossRef]
- Akhaddar, A.; Elmostarchid, B.; Boucetta, M. Images in emergency medicine. Traumatic intraorbital stone with globe displacement into the maxillary sinus. Emerg. Med. J. 2010, 27, 828. [Google Scholar] [CrossRef]
- Damasceno, N.A.P.; Damasceno, E.F. Traumatic orbital fracture with intact ocular globe displacement into the maxillary sinus. Rev. Bras. Oftalmol. 2010, 69, 52–54. [Google Scholar] [CrossRef]
- Zhang-Nunes, S.X.; Jarullazada, I.; Mancini, R. Late central visual recovery after traumatic globe displacement into the maxillary sinus. Ophthal Plast. Reconstr. Surg. 2012, 28, e17–e19. [Google Scholar] [CrossRef]
- Xu, B.; Xu, X.L.; Yan, J. Treatment of traumatic globe dislocated completely into the maxillary sinus. Int. J. Ophthalmol. 2013, 6, 106–107. [Google Scholar] [PubMed]
- Haggerty, C.J.; Roman, P. Repositioning of a traumatically displaced globe with maxillary antrostomy: Review of the literature and treatment recommendations. J. Oral. Maxillofac. Surg. 2013, 71, 1915–1922. [Google Scholar] [CrossRef] [PubMed]
- Roth, J.; Hingst, V.; Lenz, J.H. Blindness following severe midfacial trauma—Case report and review. J. Craniomaxillofac Surg. 2012, 40, 608–613. [Google Scholar] [CrossRef] [PubMed]



| Age | Sex | Visual Acuity | Motility | Pupillary Defect | Diplopia | |
|---|---|---|---|---|---|---|
| Berkowitz et al (1981) | 12 | F | Recovery 20/20 | NA | NA | NA |
| Smit et al (1990) | 28 | M | No | NA | NA | NA |
| Ziccardi et al (1993) | 35 | M | Recovery 20/20 | Restricted motility | NA | Yes (primary gaze) |
| Pelton et al (1998) | 19 | M | NA | NA | NA | NA |
| Tung et al (1998) | 17 | M | No | Minimal horizontal gaze and no vertical gaze | NA | NA |
| Saleh and Leatherbarrow (1999) | 29 | M | No | NA | NA | NA |
| Kim and Baek (2005) | 68 | M | No | Restricted motility | Nonreactive mydriatic pupil | NA |
| Müller-Richter et al (2007) | 62 | M | Recovery 20/20 | Reduced motility | Anisocoria with dilation of the pupil | Yes (lateral gaze and upward) |
| Abrishami et al (2007) | 18 | M | No | Limited in all gazes | Nonreactive mydriatic pupil | NA |
| Avadhanam et al (2008) | 30 | F | No | Good motility in all gazes | Nonreactive mydriatic pupil | NA |
| Kreiner et al (2008) | 50 | M | No | loss of ocular motility | Nonreactive mydriatic pupil | NA |
| Ramstead et al (2008) | 32 | M | Recovery 20/ 200 | Minimal horizontal gaze and no vertical gaze | Afferent pupillary defect | NA |
| Jellab et al (2008) | 24 | M | Light perception | Reduced motility | NA | NA |
| Jellab et al (2008) | 50 | F | NA | NA | NA | NA |
| Akhaddar et al (2010) | 62 | M | NA | NA | NA | NA |
| Damasceno and Damasceno (2010) | 42 | M | Recovery 20/20 | Loss of ocular motility (except for abduction) | No | Yes |
| Zhang-Nunes et al (2012) | 20 | M | Recovery 20/25 | NA | Afferent pupillary defect | NA |
| Xu et al (2013) | 46 | F | Light perception | Restricted motility | NA | NA |
| Haggerty and Roman (2013) | 35 | M | Light perception | Restricted motility | Nonreactive mydriatic pupil | NA |
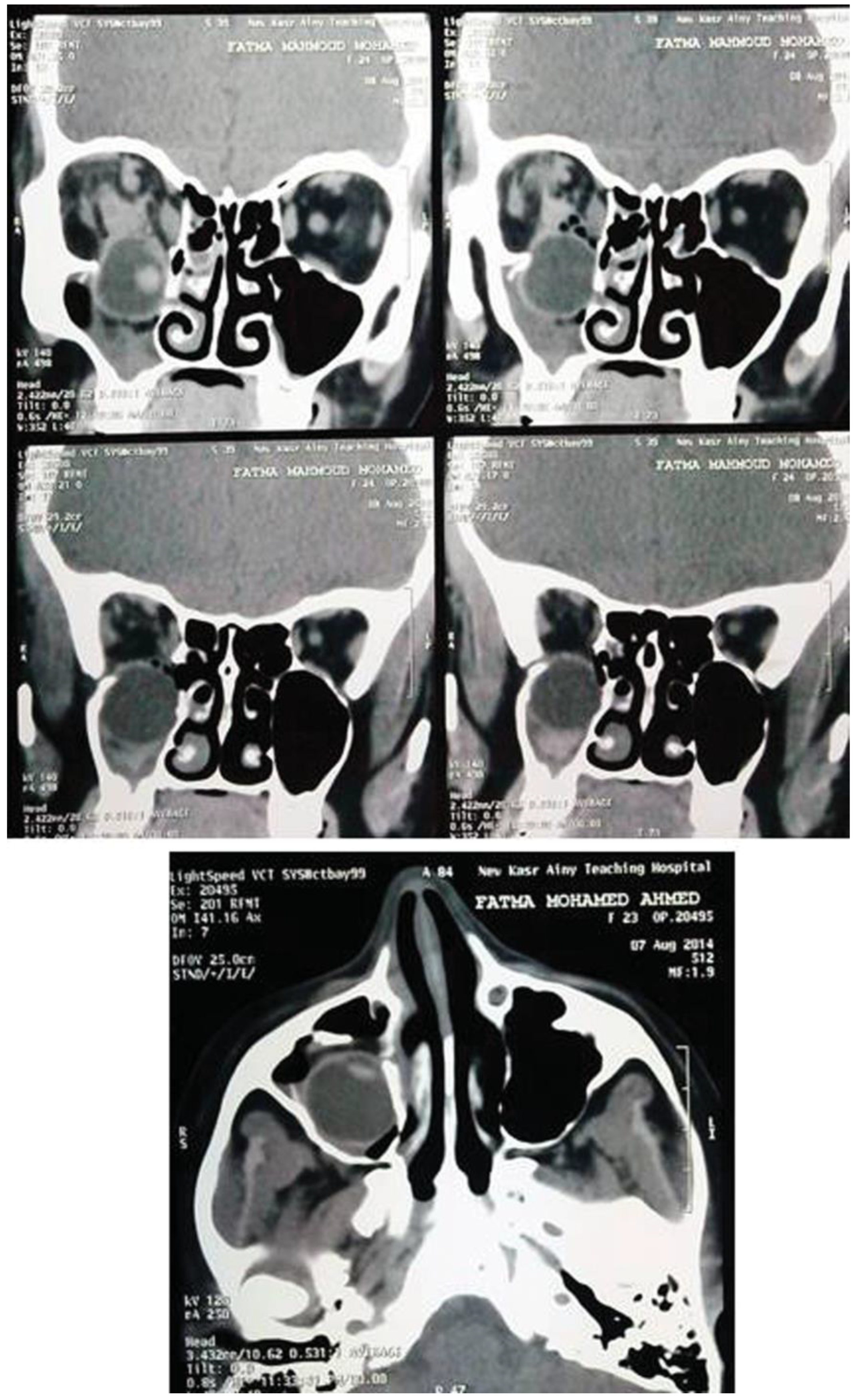
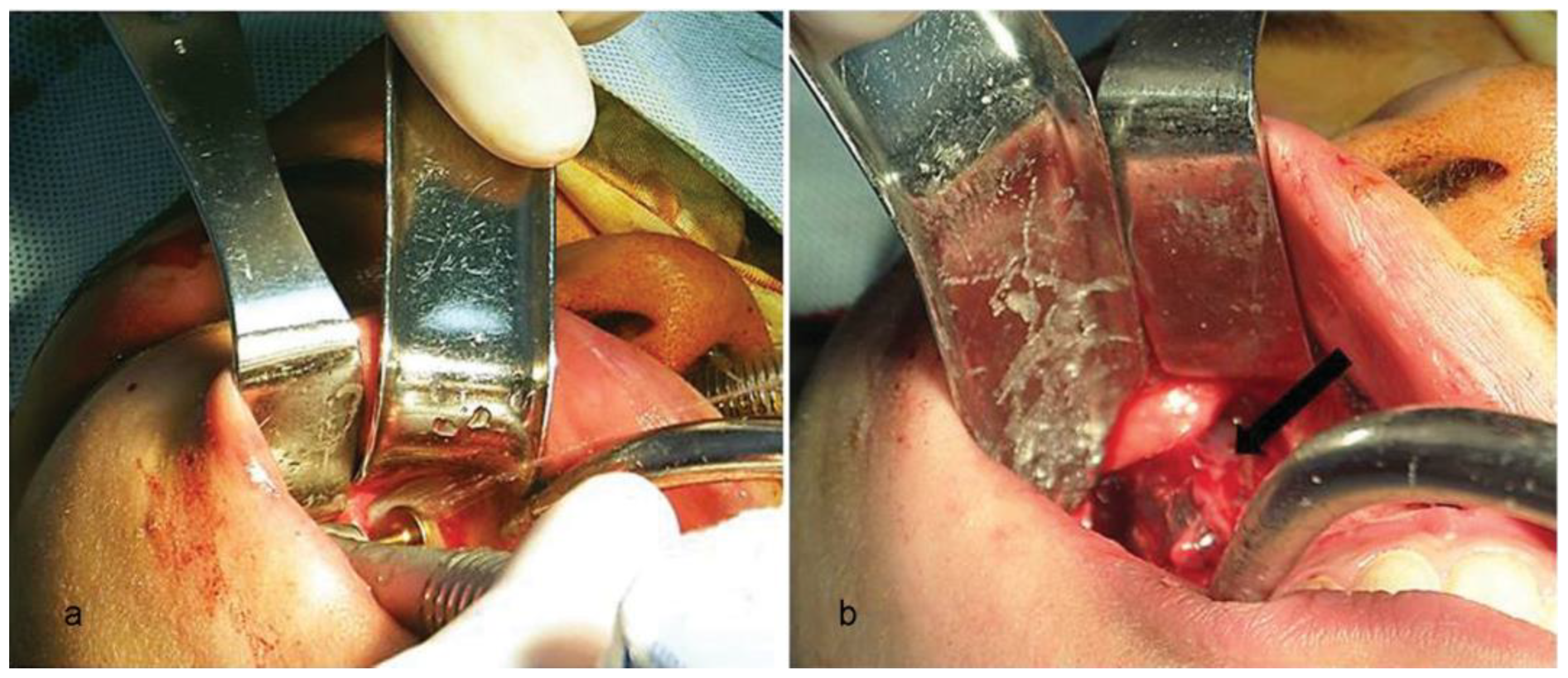
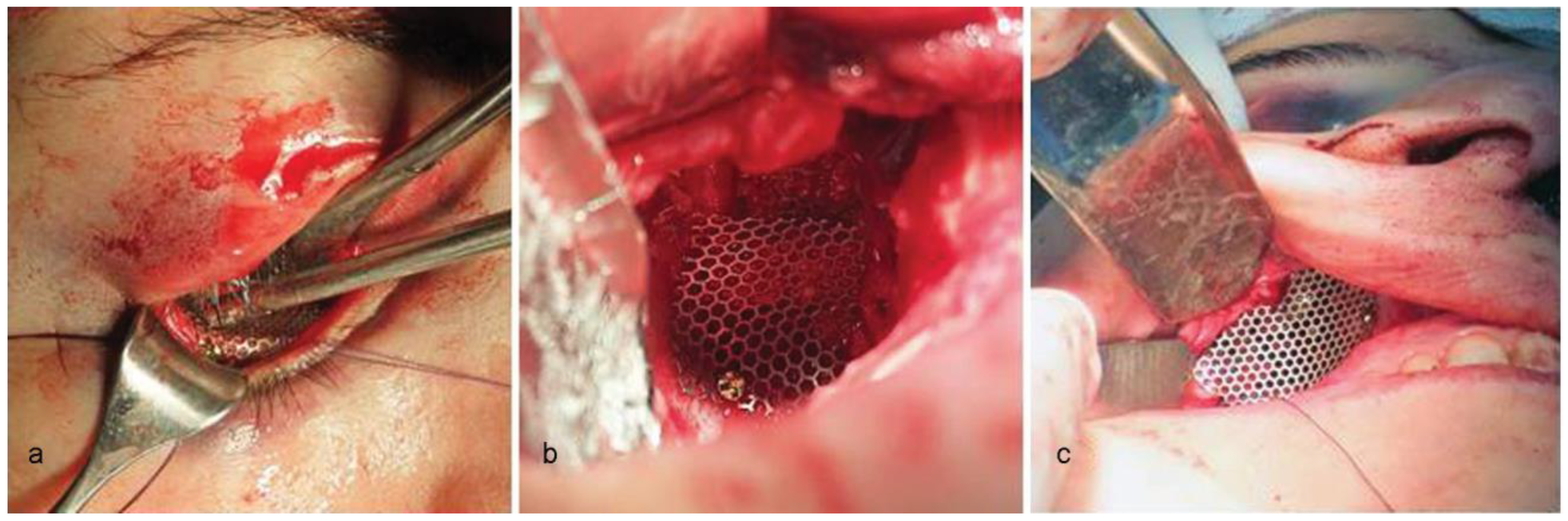
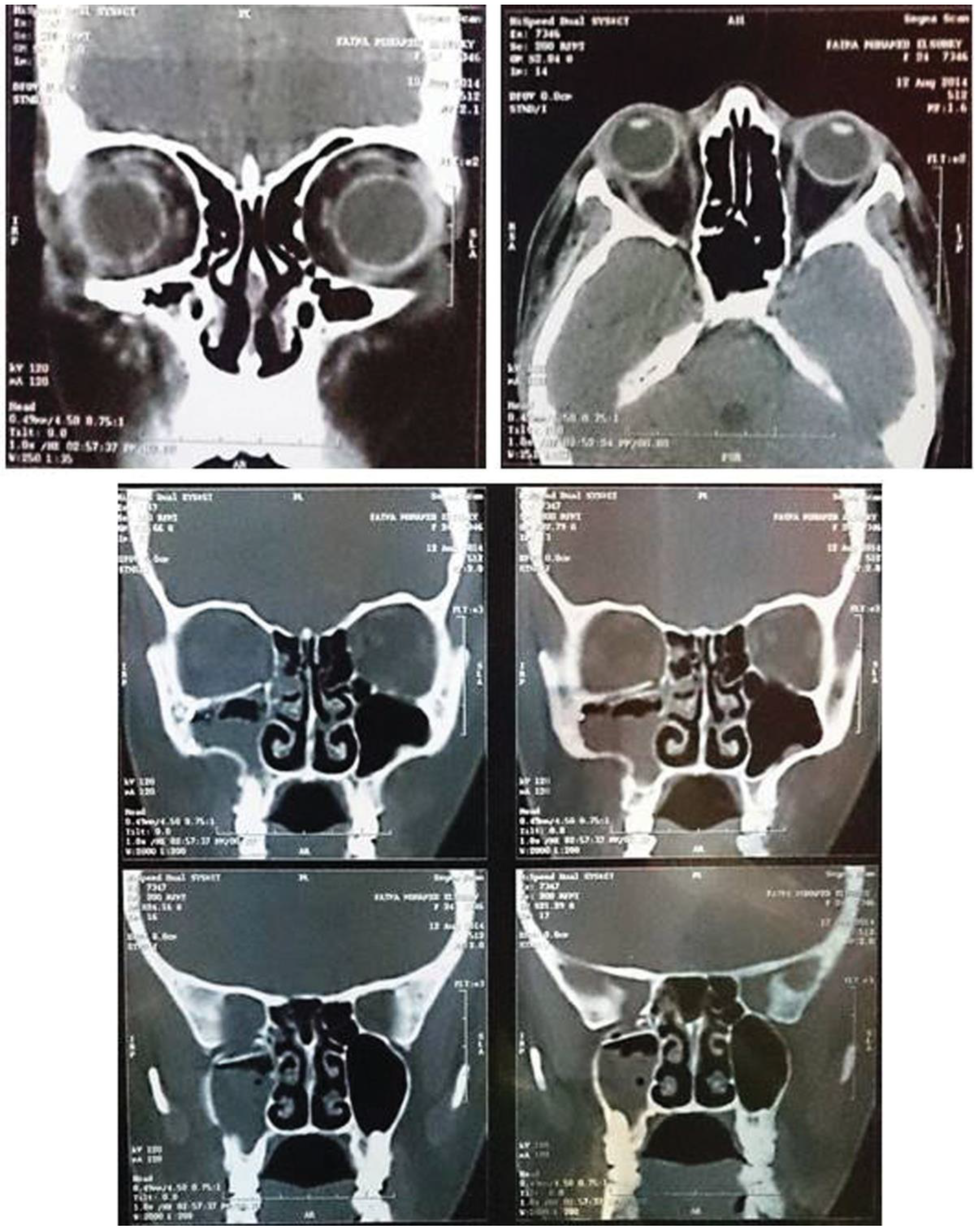
| Noman and Shindy (2015) | 24 | F | Recovery 20/40 | Reduced motility in lateral gaze | Afferent pupillary defect | Yes (lateral gaze) |
© 2016 by the authors. The Author(s) 2016.
Share and Cite
Noman, S.A.; Shindy, M.I. Immediate Surgical Management of Traumatic Dislocation of the Eye Globe into the Maxillary Sinus: Report of a Rare Case and Literature Review. Craniomaxillofac. Trauma Reconstr. 2017, 10, 151-158. https://doi.org/10.1055/s-0036-1584393
Noman SA, Shindy MI. Immediate Surgical Management of Traumatic Dislocation of the Eye Globe into the Maxillary Sinus: Report of a Rare Case and Literature Review. Craniomaxillofacial Trauma & Reconstruction. 2017; 10(2):151-158. https://doi.org/10.1055/s-0036-1584393
Chicago/Turabian StyleNoman, Samer Abduljabar, and Mostafa Ibrahim Shindy. 2017. "Immediate Surgical Management of Traumatic Dislocation of the Eye Globe into the Maxillary Sinus: Report of a Rare Case and Literature Review" Craniomaxillofacial Trauma & Reconstruction 10, no. 2: 151-158. https://doi.org/10.1055/s-0036-1584393
APA StyleNoman, S. A., & Shindy, M. I. (2017). Immediate Surgical Management of Traumatic Dislocation of the Eye Globe into the Maxillary Sinus: Report of a Rare Case and Literature Review. Craniomaxillofacial Trauma & Reconstruction, 10(2), 151-158. https://doi.org/10.1055/s-0036-1584393



