Abstract
This study aimed to obtain dependable epidemiologic data of the variation in cause and characteristics of maxillofacial fractures by identifying, describing, and quantifying trauma. This retrospective study was conducted in the state of Uttar Pradesh, India, over 1 year, based on a systematic computer-assisted database search from March 2015 to March 2016 for maxillofacial fractures. The demographics, etiology, geographic distribution, date of injury, site and number of fractures, and type of intervention were recorded for each. The study population consisted of 1000 patients with 1543 fractures. The male:female ratio was 8:1. A peak incidence of fractures was seen in the third decade (mean age: 30.3) with maximum patients younger than 40 years (80.8%). The incidence of fractures was highest in spring (42.9%). Road traffic accidents were the most common cause of trauma (64.4%) and mainly involved two wheelers (60.2%). Single-site fractures were most common. Mostly zygomatic (45.1%) and mandibular fractures (44.4%) were encountered, accounting for approximately 90% of all fractures. The main site of mandibular fractures was the body (34.4%); 46.2% of fractures underwent open reduction and internal fixation (ORIF) while 53.8% were treated by closed methods. The study provides important data to contrive future plans for injury prevention. The trend of most traffic-related injuries continues with the increasing traffic on roads. Zygomatic complex and mandibular fractures remain the most frequent. The major populations at risk are young men and those driving two wheelers. The use of helmets could achieve a large reduction in maxillofacial fractures. Awareness for preventive measures and safety guidelines should be propagated and legislation on traffic rules strictly reinforced.
Trauma accounts for the principal etiologic factor of mortality in the first 40 years of life. According to the World Health Organization (WHO), almost 1 million people die and approximately 15 to 20 million are injured annually in road traffic accidents (RTAs) [1]. In India, the world’s second most populated country, the trauma “epidemic” claims lakhs of lives every year [2]. We are experiencing an increasing trend in injuries, particularly due to road traffic accident (RTA), at an alarming annual rate of 3% [3]. Studies have found that maxillofacial injuries occur in approximately 5 to 33% of patients experiencing severe trauma [4].
Indians with injuries are reported to be six times more at risk of death as compared with their counterparts from developed countries [5]. Therefore, maxillofacial injury management requires adequate patient documentation, injury surveillance, and re-creation of data that adequately describe the whole spectrum of injuries [6]. This would enable health planners and providers to specifically address the burden of maxillofacial injuries, and thus develop suitable preventive programs aimed at lowering the incidence of these through more efficient planning for resource allocation and delivering adequate care [7,8,9]. The etiology of facial trauma also affects the incidence, clinical presentation, and treatment modalities of the facial fracture, and it is influenced by sociodemographic, economic, and cultural factors of the population being studied [8].
The aim of this unicenter-based retrospective study conducted over a period of 1 year was to obtain a dependable epidemiologic data focusing on the analysis of the variation in causes and characteristics of maxillofacial fractures managed at our center, to highlight the underlying principles and formulate treatment guidelines by identifying, describing and quantifying trauma for use in planning and evaluation of preventive programs.
Materials and Methods
The present study was conducted in the Department of Oral and Maxillofacial Surgery, King George’s Medical University, Lucknow, Uttar Pradesh, India. No ethical committee approval was obtained as this was a retrospective study taken from departmental medical records. This study was based on a systematic computer-assisted database search that allowed extraction of retrospective data of the patients who reported to our outpatient unit and emergency department (ED) including those who were hospitalized, from March 2015 to March 2016. Patients of both sexes and all age groups with clinically and radiographically diagnosed maxillofacial fractures (with or without contiguous bodily fractures/injuries) were included in this study. Exclusion of patients with incomplete records was done.
The following data were recorded for each patient: demographics (sex, age), etiology, geographic distribution, date of injury, site of facial fractures, number of fractures (single, two, or multiple), associated soft tissue and dentoalveolar injury, and type of intervention.
No formal sample size was calculated and all 1,000 patients who met the inclusion criteria during the study period were included. The patients’ age ranged from 0 to 94 years, and they were divided into eight age groups: 0 to 10, 11 to 20, 21 to 30, 31 to 40, 41 to 50, 51 to 60, 61 to 70, and older than 80 years. The following categories of cause of injury were considered: physical assaults (PAs), falls, and RTA. RTAs were analyzed and recorded according to type of vehicle, that is, two wheeler, four wheeler (heavy motor/light motor vehicle), position of the victim (driver/pillion rider). The dates of injury were grouped and analyzed according to the month of occurrence.

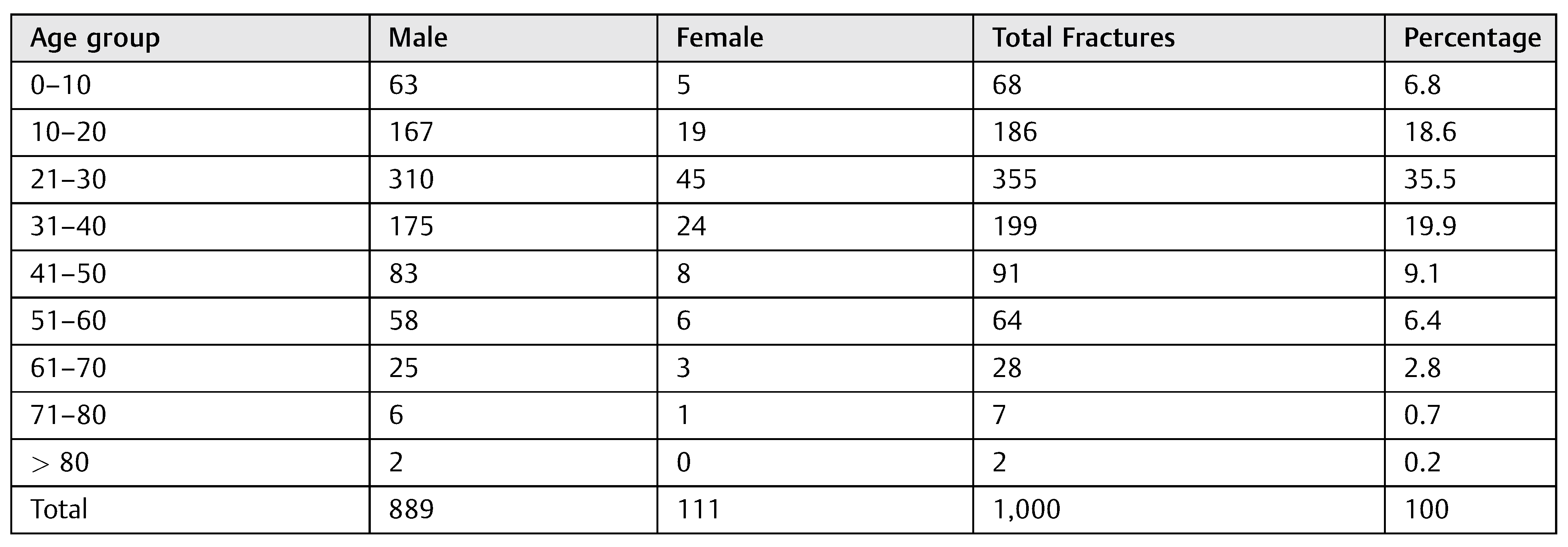
Table 1.
Age and sex distribution.
Table 1.
Age and sex distribution.
 |
Fractures were evaluated for site and number that had been determined with clinical evaluation assisted with conventional radiographs and computed tomography (CT) scans and classified as fractures of the mandible, orbital-zygomaticmaxillary complex (OZMC), orbit, nose, LeFort, and nasoorbital-ethmoid (NOE) fracture. Mandibular fractures included fractures of the symphysis, parasymphysis, body, angle, ramus, coronoid, and condyle. Patients with isolated skull fractures and only minor superficial soft tissue injuries were excluded from our study. Sex-wise distribution of site of facial injuries was also done. Treatment was broadly divided into those who had undergone open reduction and internal fixation (ORIF) and those who had been treated conservatively by closed reduction.
Data were presented using descriptive analyses. Multiple logistic regression analyses were used to identify demographic and injury-related factors associated with outcome. Statistical Package for the Social Sciences (SPSS version 16, IBM, Chicago, IL) was used for all analyses and a p value of ≤0.05 was considered statistically significant.
Results
A total of 1,000 patients presented with maxillofacial fractures in the 1-year period and amounted to an overall total of 1,543 fractures. A significant majority of affected males (889) over females (111) was noted (M:F= 8:1, p < 0.05).
Age and Sex
The age of patients at the time of injury ranged from 2 to 94 years, with a mean age of 30.3 years. No statistically significant difference was observed between male and female mean ages (p > 0.05). Most fractures occurred in patients younger than 40 years, which accounted for 80.8% of the entire sample population (Table 1). Pediatric fractures accounted for 16.6%. The age-specific distribution in patients shows an increasing trend till the third decade with subsequent decreasing incidence with each new decade: 68 injuries (6.8%) occurred in the first decade, 186 (18.6%) in the second, 355 (35.5%) in the third, 199 (19.9%) in the fourth, 91 (9.1%) in the fifth, 64 (6.4%) in the sixth, 28 (2.8%) in the seventh, 7 (0.7%) in the eighth, and 2 (0.2%) in the ninth and tenth.

Table 2.
Sex-wise distribution and mode of trauma.
Table 2.
Sex-wise distribution and mode of trauma.
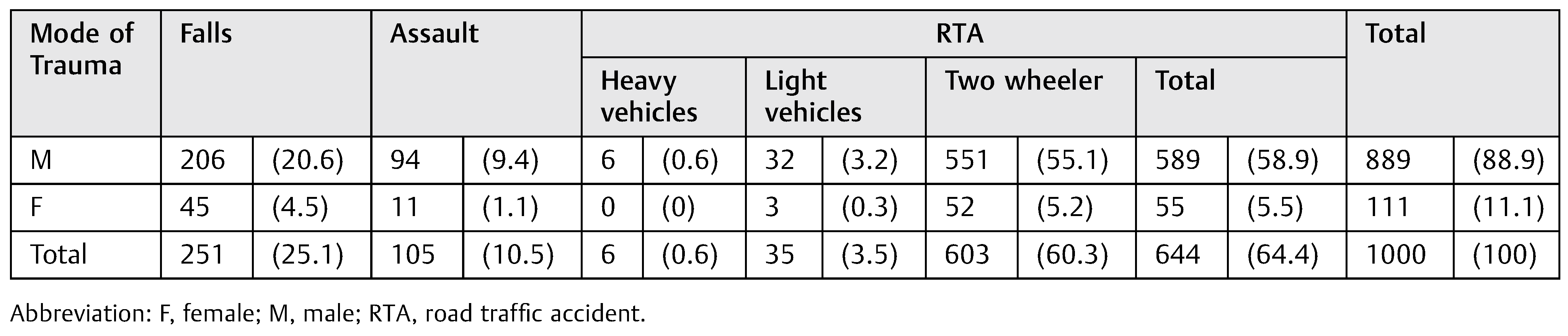 |
Mechanism of Trauma
The major etiology of maxillofacial fractures (Table 2) was RTA, 64.4% with significantly higher difference between males and females (10.7:1). The second leading cause was falls (25.1%, M:F = 4.6:1) either due to accidental falls (commonly in patients with extremes of age) or falls from height. Only 10.5% maxillofacial fractures were due to PA, with significant predominance in males (9.4%, M:F = 8.6:1). Both in males and females, RTAs were the predominant cause of injury (M, F = 589/889, 55/111). Pearson chi square demonstrated significant statistical association (p ≤ 0.05) between males and females.

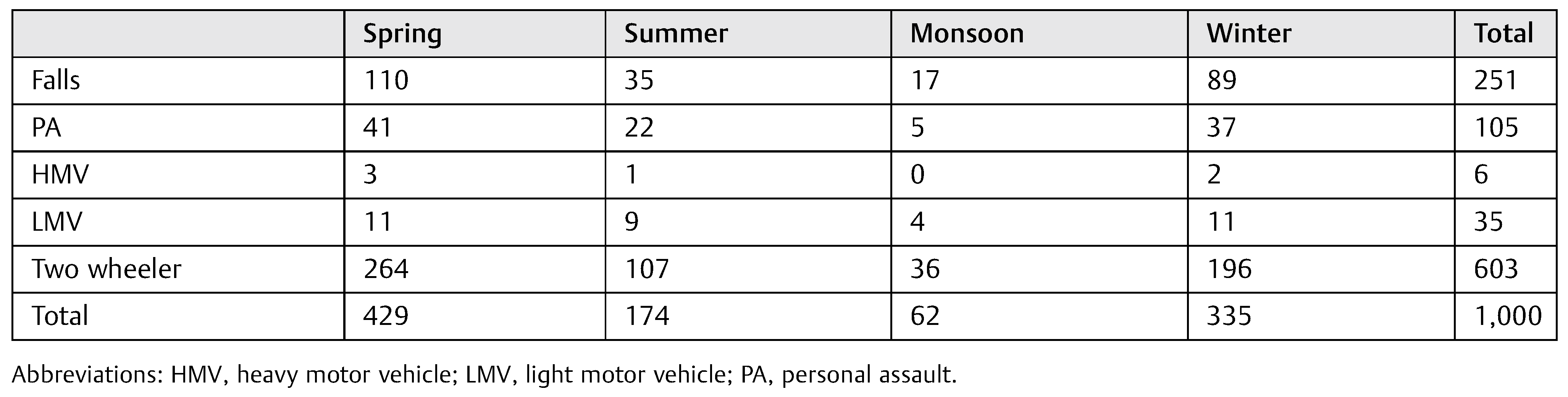
Table 3.
RTA distribution—personnel wise.
Table 3.
RTA distribution—personnel wise.
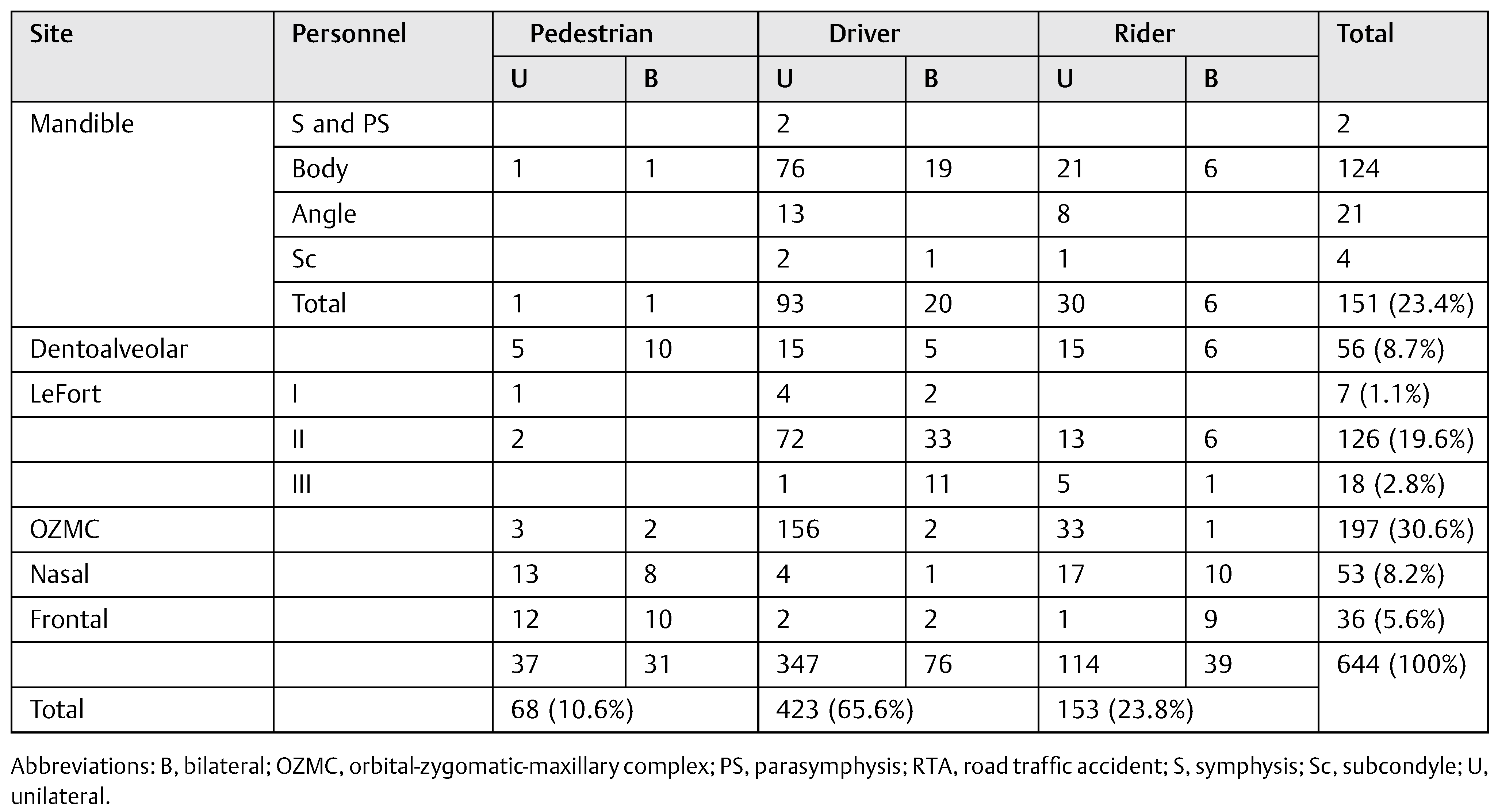 |
Regarding the age and etiology, RTA was the main etiologic factor for all age groups. Two-wheeler accidents were the most common accounting for 60.2% facial trauma. Heavy (0.6%) and light vehicular trauma cases (3.5%) were relatively uncommon. The patients who sustained fractures in RTAs were mostly the ones riding the vehicle (65.6%); a substantial magnitude of trauma was encountered by the pillion riders (23.8%) and only 10.6% by the pedestrians (Table 3). The most common fracture in drivers was the fracture of the OZMC followed by mandibular fractures. Riders suffered an almost equal number of mandibular and OZMC fractures with no symphysis, parasymphysis, or LeFort I fractures. Pedestrians mostly suffered nasal and dentoalveolar fractures and all others were very rare. Bilateral fractures were more common in drivers, most being at LeFort II level or in the mandible. In riders and pedestrians, bilateral fractures were more common in nasal and frontal bones.
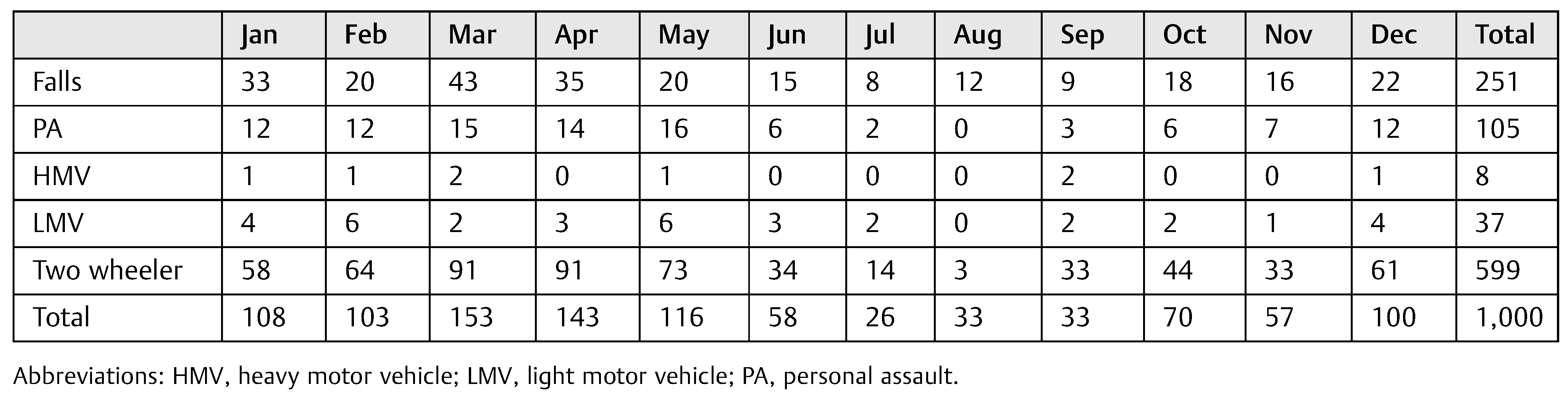
Distribution over Time
A peak in incidence was noted in March (15.3%) with maximum PAs, falls, and RTAs, closely followed by April (14.3%). Minimum trauma (2.6%) was noted in July (Table 4). The seasonal distribution (Table 5) showed that spring (42.9%) and winter (33.5%) were the seasons with greatest percentage of maxillofacial fractures. Most fractures (76.4%) occurred during these two seasons. The least number were noted in the monsoons (6.2%).

Table 4.
Month-wise distribution of mode of trauma.
Table 4.
Month-wise distribution of mode of trauma.
 |
Site of Fracture
Among the facial fractures, the mandibular fractures (Table 6) amounted to 686 (44.5%) and the most common site of fracture was the mandibular body (34.4%—46 bilateral, 81 left, and 109 right). 115 subcondyle (16.8%), 3 ramus (0.4%), 108 angle (15.7%), 236 body (34.4%), 180 parasymphysis (26.2%), 26 symphysis (3.7%), and 18 dentoalveolar fractures (2.6%) were encountered. Among the 857 (55.5%) fractures of the midface, OZMC fractures were most common (45%). A total of 13 (15.2%) LeFort I, 306 (35.7%) LeFort II, 7 (0.8%) LeFort III, 386 (45%) OZMC, 63 (7.3%) nasal, 22 (2.5%) NOE, 5 (0.9%) frontal, 85 (9.9%) temporal, and 55 (6.4%) maxillary dentoalveolar fractures were observed.
Fractures of the right side were more common (556, 36.03%) than left (508, 32.9%) and bilateral fractures were least common (425, 27.5%). Left subcondylar fractures outnumbered the ones on the right (1.4:1) and parasymphysis fractures were encountered equally on both sides. Most common bilateral fractures were those of the mandibular body (6.7%).
The mandibular fracture pattern showed that isolated mandibular fractures were most common (457, 29.6%), 222 (14.38%) patients had fractures at two locations and more than two fractures were seen in 7(0.45%) patients (Table 7). Among midface fractures, the number of patients with single, double, and multiple fractures was 480 (31.10%), 367 (23.78%), 10 (0.64%), respectively. Most common isolated fractures were nasal and OZMC. Males encountered a total of 862 (55.87%) fractures whereas females had 681 (44.13%) fractures; 937 patients had a single isolated facial fracture (60.7%), 589 (38.17%) had two sites fractured, whereas only 17 patients had more than 2 (1.1%) fractures.

Table 5.
Seasonal distribution of mode of trauma.
Table 5.
Seasonal distribution of mode of trauma.
 |
Treatment
Approximately 713 fractures (42.8%) in 415 patients (41.5%) underwent ORIF, whereas 830 (53.8%) fractures in 585 (58.5%) patients underwent closed reduction (Table 8). A larger proportion of fractures in males (626/862 = 72.6%) underwent ORIF than those in females (87/681 = 12.8%). More mandibular fractures (439/686 = 64%) were treated by open reduction as compared with midface fractures (274/857 = 32%).
Discussion
The epidemiology of maxillofacial fractures is considerably variable [9,10,11]. Frequencies differ both within and between countries depending on contributing entities such as environmental, cultural, and socioeconomic factors [10,11]. Our study demonstrates the pattern of trauma in a population of Uttar Pradesh, India, over a period of 1 year.
Our patients were predominantly male, as in previous studies [12]. The male:female ratio (8:1) was higher than those reported in developed countries (3:1) [12] but corresponded to those of developing ones (7:1) [13]. The demographic characteristics of maxillofacial fractures differs significantly between both genders [14]. The majority of fractures seen in males were most likely due to higher physical activity, more involvement in road accidents, altercations, and work-related casualties [8]. Lesser incidence of maxillofacial fractures in females could be because of lesser reporting of injuries [15]—due to either the sex-based neglect still prevalent in many rural areas or domestic abuse.

Table 6.
Distribution of mandibular and midface fractures.
Table 6.
Distribution of mandibular and midface fractures.
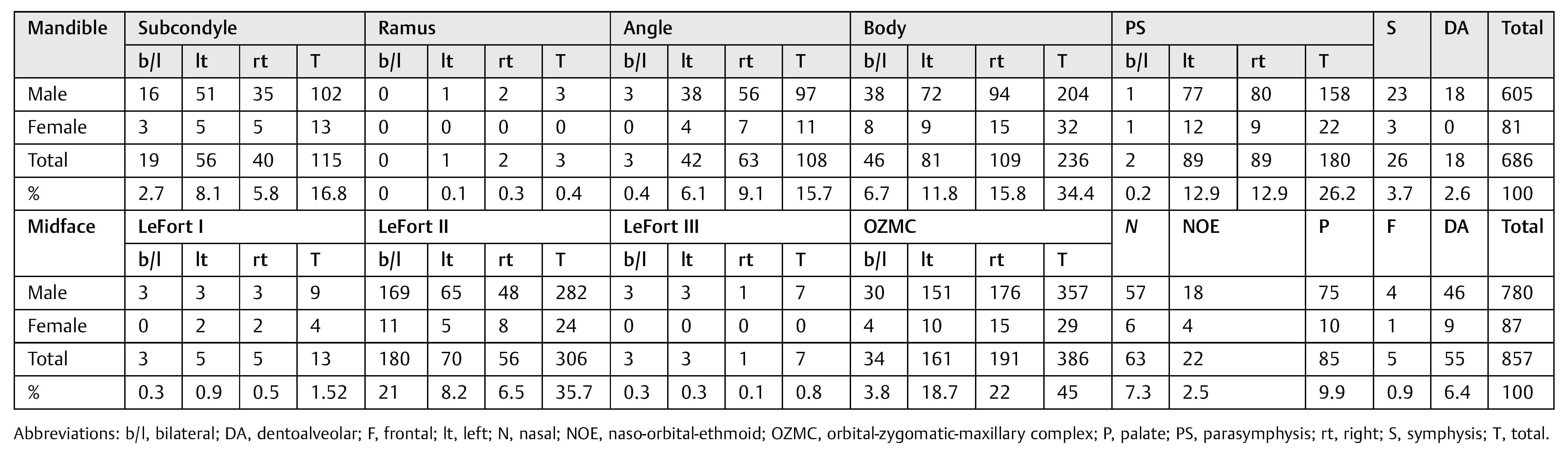 |

Table 7.
Number of fractures.
Table 7.
Number of fractures.
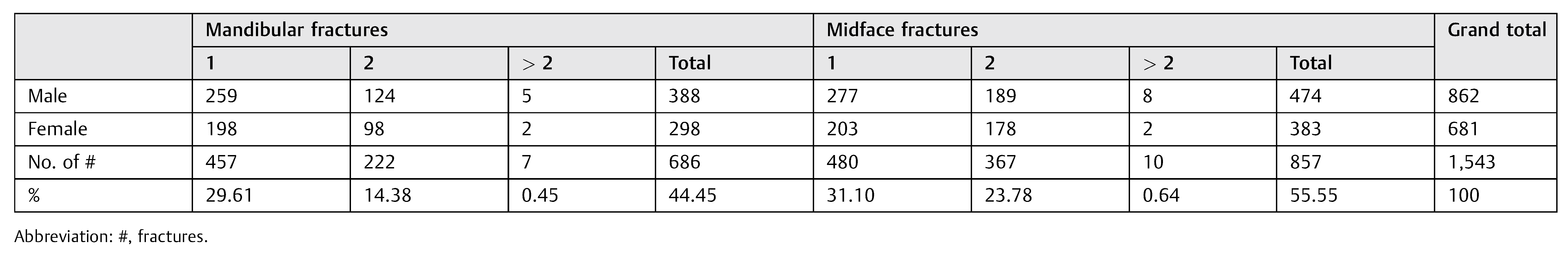 |

Table 8.
Treatment distribution of mandibular and midface fractures.
Table 8.
Treatment distribution of mandibular and midface fractures.
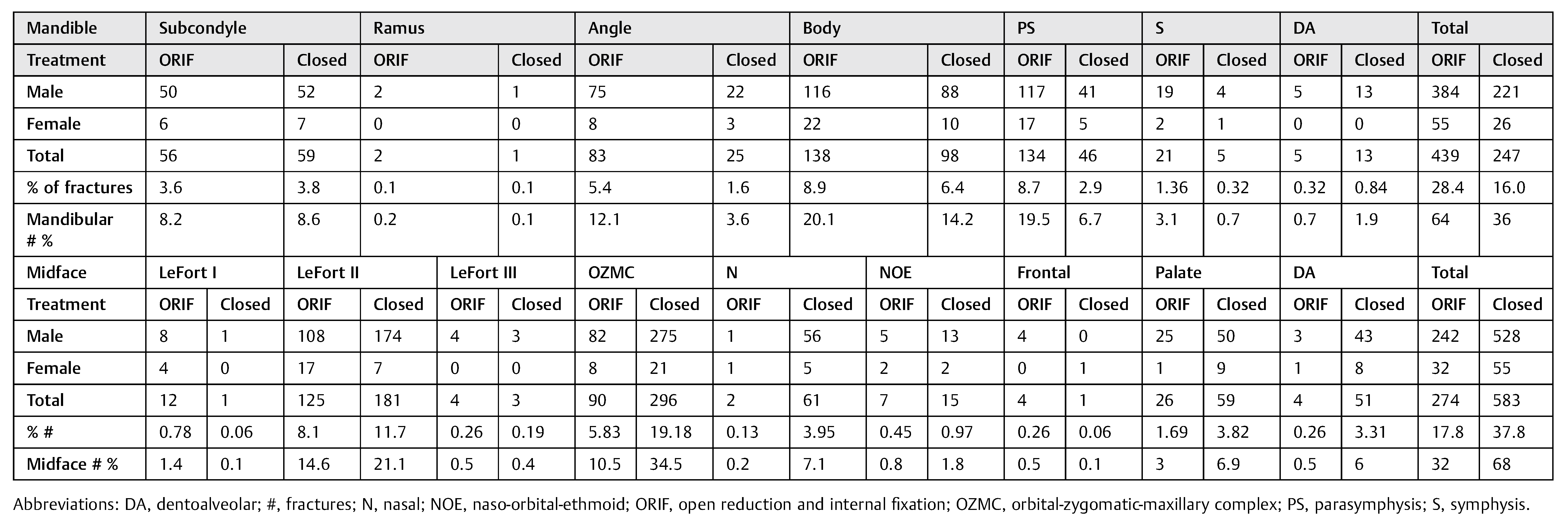 |
Most fractures occurred between the first and fourth decades, as reported earlier [16]. The observation that men aged between 21 and 30 years had the highest frequency of facial fractures is consistent with literature [10,17,18,19,20,21]. Pediatric fractures accounted for 16.6% in our study (predominantly due to falls). In agreement with previous studies, we observed the rarity of facial fractures before 5 years of age, while their incidence progressively increases with the beginning of school and adolescence [22].
A peak in incidence of maxillofacial fractures in March to April was in accordance with many authors [7] with peak seasonal distribution observed in spring and winter in contrast to studies in which most injuries are reported during summer [8,16,23].
RTAs, assaults, and falls are the leading causes of maxillofacial fractures worldwide. The main cause of fractures in males was RTA [19,20,24]. It was striking that male vehicle drivers sustaining facial fractures far outnumbered female drivers, confirming the risk-taking behavior of young men [25]. Inadequate road safety awareness, unsuitable road conditions, violation of speed limits, ill-maintained vehicles without safety features, failure to wear seat belts or helmets, entry into opposite traffic lanes, violation of the highway code, use of alcohol or other intoxicating agents, behavioral disorders, and socioeconomical insufficiencies of some drivers are the cardinal reasons for the large numbers of RTA in India. Two-wheeler accidents predominate as a result of inattention and poor road conditions [4].
Fall-related facial injuries were the second most common cause of facial bone fractures, seen predominantly in elderly population, especially affecting the mandible, was similar to previous studies [22,26]. Assault was the third most common cause of facial injury, the magnitude of which is lesser (10.5%) compared with that reported (13–90%) by other countries [27,28] and reported as the leading cause by a few countries [22,29].
There is a stark difference between the incidence and etiology of trauma in developed and developing countries. In American, African, and Asian countries, road traffic crashes have been shown to be the predominant cause [24]. The EURMAT (European Maxillofacial Trauma) collaboration highlights the changing trend in maxillofacial trauma epidemiology in European countries, with trauma caused by assaults and falls now outnumbering those due to RTA [29]. The longevity of the European population, in addition to strict road and work legislation, could be responsible for this change [29]. In Oceania assaults are predominant [24]. This variation in etiology of trauma across the globe warrants the knowledge of different laws (regarding factors, e.g., traffic, vehicles, sports, and interpersonal violence) in different countries to allow for improvement in maxillofacial trauma incidence rates.
Fractures that occur most frequently following the assault include the nasal bones, mandible, zygoma, and midface in descending order [30]. Nasal bone fractures have been reported as the most frequent midfacial fractures [14] because of facial prominence, lack of soft tissue, and being an easy target in violence attacks, making them the most fragile facial bones. Remarkably, fewer nasal bone fractures were noted in this study. In the midface, the zygoma was frequently involved, as it is an anatomic structure susceptible to injury by external force [8,31]. The majority of fractures were of the midface [4,12,26], the larger proportion of which were bilateral, more commonly being caused by high velocity trauma of RTAs. When analyzing fractures individually, the most common site was the mandible, consistent with studies [12,31,32], probably as it occupies a larger vulnerable area in the facial skeleton. A majority of patients (60.7%) experienced trauma to a single bone, in contrast to previous research [21].
As plate osteosynthesis has become the state of the art in the treatment of facial fractures, 46.2% of cases were treated with the open method with use of plating systems [27,33]. Most mandibular fractures (64%) were treated by open reduction [21,34]. Open reduction can prevent unwanted sequelae such as body weight reduction, poor oral hygiene, speech difficulties, and periodontal disease associated with the closed reduction. Our results correspond with previous studies [10,19,35] in which open reduction was lesser frequently used. This can be attributed to closed reduction being economically profitable for people in developing countries in poorer living standards. The disparity in ORIF rates with only 32% midface fractures undergoing ORIF can be due to more amounts of nasal, frontal, and zygomatic arch fractures being treated by closed reduction. Also, this is the choice of management in medically compromised or noncompliant patients [34].
Limitations of the study is that being retrospective, it may be subject to information bias due to inaccurate initial examination and incomplete or incorrect documentation. Also, the study population was obtained from a single trauma center and could possibly not reflect the experience at centers with a concoction of presentations. Details of drinking and driving and use of helmets were not included.
However, the results provide vital information required to excogitate plans for preventive measures to reduce the frequency of maxillofacial fractures, which when associated with other injuries due to RTA, are grueling to treat. Socioeconomic consequences of facial fractures include the cost of treatment and hospital admission, hospital resources, and loss of revenue [36]. Consequences for patients include functional, psychological, aesthetic, emotional, and financial problems. India, a developing nation with a humongous population and rising economy, has massive traffic issues with increasing number of accidents every year, mostly due to the complete disregard of traffic rules and dismal abidance of laws for compulsory helmet and seat belt use. Most drivers are unlicensed, uneducated, do not maintain vehicles, and drive under the influence of alcohol [37].
The only cure for the trauma epidemic is injury prevention. Preventive measures such as wearing helmets and using restraints reduce facial injuries by 65% [38] and 25% [36], respectively. Lower limits of motor vehicle speed in urban areas, road safety training for adolescents, and lanes to segregate two wheelers from motor vehicles [39] should also prove helpful. Strict enforcement of existing traffic regulations, formulation of new staunch traffic policies, reinforcement of legislation aimed to prevent RTA, and educating people about safety guidelines before and after vehicles purchase are the need of the hour in our country to reduce traffic accidents. The trauma burden due to falls and PA could also be reduced by better care and vigilance of the elderly population and harsher laws for those engaging in interpersonal violence.
Conclusion
The study provides important data to contrive future plans for injury prevention. The trend of most RTA-related injuries continues with the increasing traffic on roads. Zygomatico complex and mandibular fractures remain the most frequent fractures. The major populations at risk are young men and those driving two wheelers. The use of helmets could achieve a large reduction in maxillofacial fractures. Awareness for preventive measures and safety guidelines should be propagated and legislation on traffic rules strictly reinforced.
Funding
This research received no external funding.
Ethical Approval
Not required.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Bither, S.; Mahindra, U.; Halli, R.; Kini, Y. Incidence and pattern of mandibular fractures in rural population: A review of 324 patients at a tertiary hospital in Loni, Maharashtra, India. Dent Traumatol 2008, 24, 468–470. [Google Scholar] [CrossRef] [PubMed]
- Mohan, D. Road traffic injuries & fatalities in India—A modern epidemic. Indian J Med Res 2006, 123, 1–4. [Google Scholar]
- Joshipura, M.K.; Shah, H.S.; Patel, P.R.; Divatia, P.A.; Desai, P.M. Trauma care systems in India. Injury 2003, 34, 686–692. [Google Scholar] [CrossRef]
- Shahim, F.N.; Cameron, P.; McNeil, J.J. Maxillofacial trauma in major trauma patients. Aust Dent J 2006, 51, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Mock, C.N.; Jurkovich, G.J.; nii-Amon-Kotei, D.; Arreola-Risa, C.; Maier, R.V. Trauma mortality patterns in three nations at different economic levels: Implications for global trauma system development. J Trauma 1998, 44, 804–812; discussion 812–814. [Google Scholar] [CrossRef]
- Kloss, F.R.; Stigler, R.G.; Brandstätter, A.; et al. Complications related to midfacial fractures: Operative versus non-surgical treatment. Int J Oral Maxillofac Surg 2011, 40, 33–37. [Google Scholar] [CrossRef]
- van Hout, W.M.; Van Cann, E.M.; Abbink, J.H.; Koole, R. An epidemiological study of maxillofacial fractures requiring surgical treatment at a tertiary trauma centre between 2005 and 2010. Br J Oral Maxillofac Surg 2013, 51, 416–420. [Google Scholar] [CrossRef]
- Mijiti, A.; Ling, W.; Tuerdi, M.; et al. Epidemiological analysis of maxillofacial fractures treated at a university hospital, Xinjiang, China: A 5-year retrospective study. J Craniomaxillofac Surg 2014, 42, 227–233. [Google Scholar] [CrossRef] [PubMed]
- Hächl, O.; Tuli, T.; Schwabegger, A.; Gassner, R. Maxillofacial trauma due to work-related accidents. Int J Oral Maxillofac Surg 2002, 31, 90–93. [Google Scholar] [CrossRef]
- Al Ahmed, H.E.; Jaber, M.A.; Abu Fanas, S.H.; Karas, M. The pattern of maxillofacial fractures in Sharjah, United Arab Emirates: A review of 230 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004, 98, 166–170. [Google Scholar] [CrossRef]
- Iida, S.; Kogo, M.; Sugiura, T.; Mima, T.; Matsuya, T. Retrospective analysis of 1502 patients with facial fractures. Int J Oral Maxillofac Surg 2001, 30, 286–290. [Google Scholar] [CrossRef]
- van den Bergh, B.; Karagozoglu, K.H.; Heymans, M.W.; Forouzanfar, T. Aetiology and incidence of maxillofacial trauma in Amsterdam: A retrospective analysis of 579 patients. J Craniomaxillofac Surg 2012, 40, e165–e169. [Google Scholar] [CrossRef] [PubMed]
- Al-Khateeb, T.; Abdullah, F.M. Craniomaxillofacial injuries in the United Arab Emirates: A retrospective study. J Oral Maxillofac Surg 2007, 65, 1094–1101. [Google Scholar] [CrossRef]
- Zhou, H.H.; Liu, Q.; Yang, R.T.; Li, Z.; Li, Z.B. Maxillofacial fractures in women and men: A 10-year retrospective study. J Oral Maxillofac Surg 2015, 73, 2181–2188. [Google Scholar] [CrossRef] [PubMed]
- Al-Dajani, M.; Quiñonez, C.; Macpherson, A.K.; Clokie, C.; Azarpazhooh, A. Epidemiology of maxillofacial injuries in Ontario, Canada. J Oral Maxillofac Surg 2015, 73, 693.e1–693.e9. [Google Scholar] [CrossRef] [PubMed]
- Boffano, P.; Roccia, F.; Gallesio, C.; Karagozoglu, K.H.; Forouzanfar, T. Bicycle-related maxillofacial injuries: A double-center study. Oral Surg Oral Med Oral Pathol Oral Radiol 2013, 116, 275–280. [Google Scholar] [CrossRef]
- Naveen Shankar, A.; Naveen Shankar, V.; Hegde NSharma Prasad, R. The pattern of the maxillofacial fractures—A multicentre retrospective study. J Craniomaxillofac Surg 2012, 40, 675–679. [Google Scholar] [CrossRef]
- Bede, S. Mandibular fractures in Iraq: An epidemiological study. Craniomaxillofac Trauma Reconstr 2015, 8, 59–63. [Google Scholar] [CrossRef]
- Ansari, M.H. Maxillofacial fractures in Hamadan province, Iran: A retrospective study (1987–2001). J Craniomaxillofac Surg 2004, 32, 28–34. [Google Scholar] [CrossRef]
- Ugboko, V.I.; Odusanya, S.A.; Fagade, O.O. Maxillofacial fractures in a semi-urban Nigerian teaching hospital. A review of 442 cases. Int J Oral Maxillofac Surg 1998, 27, 286–289. [Google Scholar] [CrossRef]
- Cabalag, M.S.; Wasiak, J.; Andrew, N.E.; Tang, J.; Kirby, J.C.; Morgan, D.J. Epidemiology and management of maxillofacial fractures in an Australian trauma centre. J Plast Reconstr Aesthet Surg 2014, 67, 183–189. [Google Scholar] [CrossRef]
- Boffano, P.; Roccia, F.; Zavattero, E.; et al. European Maxillofacial Trauma (EURMAT) in children: A multicenter and prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol 2015, 119, 499–504. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Cho, B.K.; Park, W.J. A 4-year retrospective studyof facial fractures on Jeju, Korea. J Craniomaxillofac Surg 2010, 38, 192–196. [Google Scholar] [CrossRef] [PubMed]
- Boffano, P.; Kommers, S.C.; Karagozoglu, K.H.; Forouzanfar, T. Aetiology of maxillofacial fractures: A review of published studies during the last 30 years. Br J Oral Maxillofac Surg 2014, 52, 901–906. [Google Scholar] [CrossRef]
- DeJoy, D.M. An examination of gender differences in traffic accident risk perception. Accid Anal Prev 1992, 24, 237–246. [Google Scholar] [CrossRef] [PubMed]
- Down, K.E.; Boot, D.A.; Gorman, D.F. Maxillofacial and associated injuries in severely traumatized patients: Implications of a regional survey. Int J Oral Maxillofac Surg 1995, 24, 409–412. [Google Scholar] [CrossRef]
- Schön, R.; Roveda, S.I.; Carter, B. Mandibular fractures in Townsville, Australia: Incidence, aetiology and treatment using the 2.0 AO/ASIF miniplate system. Br J Oral Maxillofac Surg 2001, 39, 145–148. [Google Scholar] [CrossRef]
- Ozkaya, O.; Turgut, G.; Kayali, M.U.; Uğurlu, K.; Kuran, I.; Baş, L. A retrospective study on the epidemiology and treatment of maxillofacial fractures. Ulus Travma Acil Cerrahi Derg 2009, 15, 262–266. [Google Scholar]
- Boffano, P.; Roccia, F.; Zavattero, E.; et al. European Maxillofacial Trauma (EURMAT) project: A multicentre and prospective study. J Craniomaxillofac Surg 2015, 43, 62–70. [Google Scholar] [CrossRef]
- Haug, R.H.; Prather, J.; Indresano, A.T. An epidemiologic survey of facial fractures and concomitant injuries. J Oral Maxillofac Surg 1990, 48, 926–932. [Google Scholar] [CrossRef]
- Yamamoto, K.; Matsusue, Y.; Horita, S.; Murakami, K.; Sugiura, T.; Kirita, T. Maxillofacial fractures sustained in bicycle accidents. J Oral Maxillofac Surg 2011, 69, e155–e160. [Google Scholar] [CrossRef] [PubMed]
- Erol, B.; Tanrikulu, R.; Görgün, B. Maxillofacial fractures. Analysis of demographic distribution and treatment in 2901 patients (25-year experience). J Craniomaxillofac Surg 2004, 32, 308–313. [Google Scholar] [CrossRef] [PubMed]
- de Matos, F.P.; Arnez, M.F.; Sverzut, C.E.; Trivellato, A.E. A retrospective study of mandibular fracture in a 40-month period. Int J Oral Maxillofac Surg 2010, 39, 10–15. [Google Scholar] [CrossRef]
- Bormann, K.H.; Wild, S.; Gellrich, N.C.; et al. Five-year retrospective study of mandibular fractures in Freiburg, Germany: Incidence, etiology, treatment, and complications. J Oral Maxillofac Surg 2009, 67, 1251–1255. [Google Scholar] [CrossRef] [PubMed]
- Bakardjiev, A.; Pechalova, P. Maxillofacial fractures in Southern Bulgaria—A retrospective study of 1706 cases. J Craniomaxillofac Surg 2007, 35, 147–150. [Google Scholar] [CrossRef]
- Huelke, D.F.; Compton, C.P. Facial injuries in automobile crashes. J Oral Maxillofac Surg 1983, 41, 241–244. [Google Scholar] [CrossRef]
- Chandra Shekar, B.R.; Reddy, C. A five-year retrospective statistical analysis of maxillofacial injuries in patients admitted and treated at two hospitals of Mysore city. Indian J Dent Res 2008, 19, 304–308. [Google Scholar] [CrossRef]
- Thompson, D.C.; Rivara, F.P.; Thompson, R. Helmets for preventing head and facial injuries in bicyclists [Review]. Cochrane Database Syst Rev 2000, 2, CD001855. [Google Scholar]
- Davidson, J.A. Epidemiology and outcome of bicycle injuries presenting to an emergency department in the United Kingdom. Eur J Emerg Med 2005, 12, 24–29. [Google Scholar] [CrossRef]
© 2016 by the author. The Author(s) 2016.