Abstract
Faciomaxillary and ocular trauma is a common entity in most emergency and trauma units. We came across a 68-year-old female patient with a history of bull horn injury over the right eye. Examination revealed an empty orbital socket with unreliable perception of light present. Imaging showed that the eye had displaced posteroinferomedially to be lying in the ethmoid air cells in the nasal cavity. Under nasal endoscopic guidance, the eye was reposited back into the orbital socket and conjunctival sutures were taken to stabilize the position. The patient had vision of counting fingers at 1.5 m on the first postoperative day which improved to 6/24 on last follow-up. Such is the rarity that never before has such a case been described in literature where traumatic displacement of eyeball into the nose has been successfully repositioned by an endonasal endoscope with appreciable regaining of vision. It also further promotes endonasal endoscopic approach in the management of orbital blow out injuries.
A trauma unit sees a varied number of facial trauma cases. Blow out fractures of the orbit are not a rare entity. A study in the United States has shown that there is a 50% increase in orbital fractures in the past decade. [1] Indian studies have shown an orbital trauma prevalence of 2.5 to 4.5%. [2,3] Agricultural injuries in the form of blunt trauma seems to be the most common mode. It must be noted here that such injuries are preventable causes of blindness. Pure orbital blowout fractures are seen at the weakest point of the orbit. A study shows that isolated medial wall fracture is seen most commonly followed by combined medial wall and floor orbit fractures. [4] Medial wall of orbit fractures is commonly associated with fractures of nasoethmoid complex. However, to the best of our knowledge, no literature has documented a complete luxation of the eyeball medially into the nasal cavity, and more so its successful surgical correction and complete regaining of vision. Luxation of the eye is quite rare. Prompt surgical intervention is crucial and can save vision.
Case History
A 68-year-old female, member of low socioeconomic community, presented to the casualty with history of hit over the right eye by a bull horn during her daily agricultural activities. She complained of sudden and painful loss of vision in the right eye. She also had a history of minimal amount of right nose bleed which was spontaneously controlled without any intervention. No other significant injuries were noted. She had no known comorbidities.
Clinical Findings
Patient was vitally stable with a good general condition. Ophthalmological examination revealed an empty right eye socket with both upper and lower lid edema (Figure 1). The right eye could not be located. An unreliable perception of light was marked in the same eye. A palpable fracture of the inferior orbital rim was noted. Nose examination revealed blood clots in the right nostril. Other examinations seemed normal.
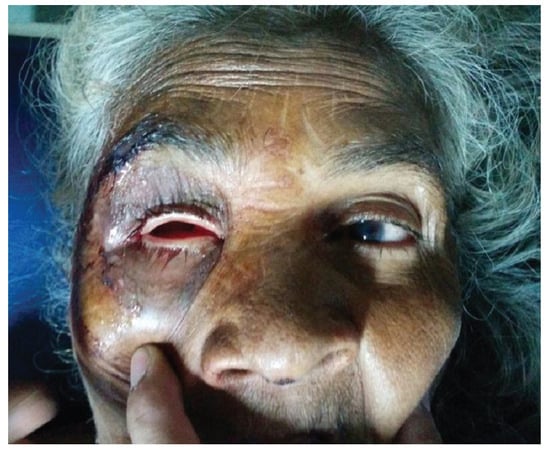
Figure 1.
Presenting image of patient where the right orbital socket is empty.
Diagnostic Assessment
Ultrasonographic B scan was done which revealed the right eye to be displaced posteroinferomedially with restricted movements but a normal lens in situ. Computed tomography scan was done which showed orbital blow-out fracture involving the medial wall and floor, with the right eye lying in the right anterior ethmoid cells going into the anterior part of the right nasal cavity (Figure 2 and Figure 3). Fortunately, the respective optic nerve was seen in contact and was in continuity with the displaced eyeball and it seemed to be intact.
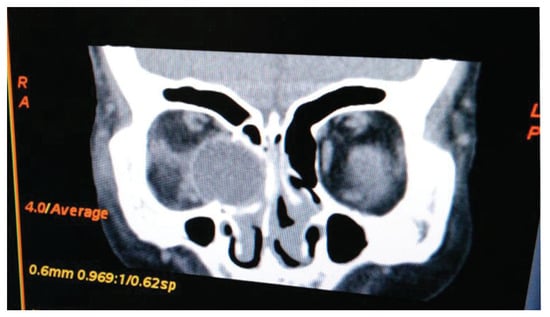
Figure 2.
Coronal CT scan of the orbit showing posteroinferomedial displacement of the right eyeball into the nasal cavity.
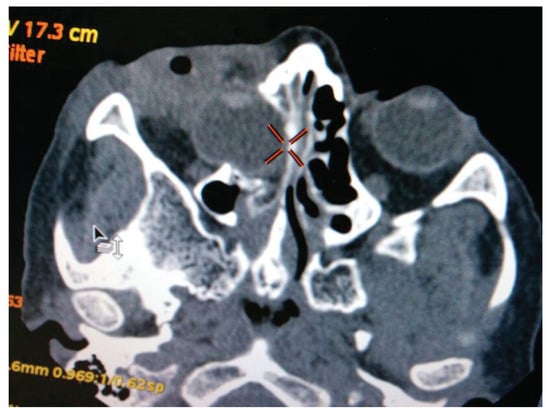
Figure 3.
Axial CT scan of the orbit showing posteroinferomedial displacement of the right eyeball into the nasal cavity.
Therapeutic Intervention
Hence interventional surgery was planned under general anesthesia. Nasal endoscopy showed a globular bulge on the lateral wall of the nose displacing the uncinate process, middle turbinate and fractured pieces of ethmoids medially. Uncinectomy was done and fractured lamina papyracea was observed. The soft-tissue bulge caused by the eyeball was pushed laterally and anteriorly back into its socket with utmost care and precision using a Freer elevator. Simultaneously, our ophthalmology colleagues took a loop suture over the lateral rectus and pulled the eye in its position (Figure 4). Lose fragments of fractured ethmoids were removed. The septal cartilage was harvested by giving a Freer incision. The cartilage was then kept over the defect on the lateral wall as a support. The size of the septal cartilage was approximately 2 × 2 cm. The cartilage was encased within a Surgicel and was kept over the lateral nasal wall defect by insinuating between the fractured edges of lamina papyracea between the orbital fat and lamina papyracea and it was supported by merocele anterior nasal pack.
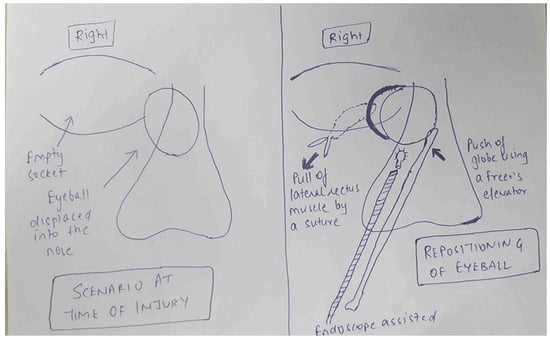
Figure 4.
Schematic image of the operative intervention by pushing the globe laterally using the Freer elevator and pulling it by the loop suture attached to the lateral rectus muscle.
On table findings revealed an intact globe with a clear healthy cornea. Multiple conjunctival tears with muscle lacerations were seen (Figure 5). Pupil was 3 mm dilated, not reactive to light, and there was immature cataract.

Figure 5.
On table findings of the right eye after successful reposition of the globe.
Follow-Up and Outcome
On the first postoperative day, the woman gained a visual acuity of counting fingers at 1.5 m for distance and N18 (Faculty’s Roman test types notation) or J10 (Jaeger notation) for near in the operated right eye. Postoperative edema was present with congestion and chemosis. There was mechanical ptosis with restricted movements and exotropia. There was no diplopia. Slitlamp examination showed a clear cornea, quiet anterior chamber, and a 3-mm diameter pupil sluggishly reactive to light. Intraocular pressure was normal (12 mm Hg). Finally, fundus examination showed a normal optic disc and macula.
Subsequent follow-ups showed an improvement in visual acuity achieving 6/24 (Snellen’s visual acuity) or –0.6 (log equity relative to 20/20) or 4.0 (minimal angle of resolution [MAR]) vision in distance and N18 (Faculty’s Roman test types notation) or J10 (Jaeger notation) in near. Ptosis also improved. Pupil became fully reactive to light. Mild exotropia with restriction of movements, however, persisted.
The latest follow-up done at 8 months has showed a visual acuity of 6/18 (Snellen’s visual acuity) or –0.5 (Log equity relative to 20/20) or 3.0 (MAR) for distance and N18 (Faculty’s Roman test types notation) or J10 (Jaeger notation) for near. There is minimal restricted movement. And on the latest follow-up, there is no ptosis at all. With mild restriction in left lateral gaze, there is occasional diplopia on lateral gaze of the opposite side due to compression of the medial rectus at the time of the injury. However, the patient does not find it much troublesome and her daily routine life is not affected (Figure 6). Follow-up CT scan also shows a normally placed globe (Figure 7 and Figure 8).
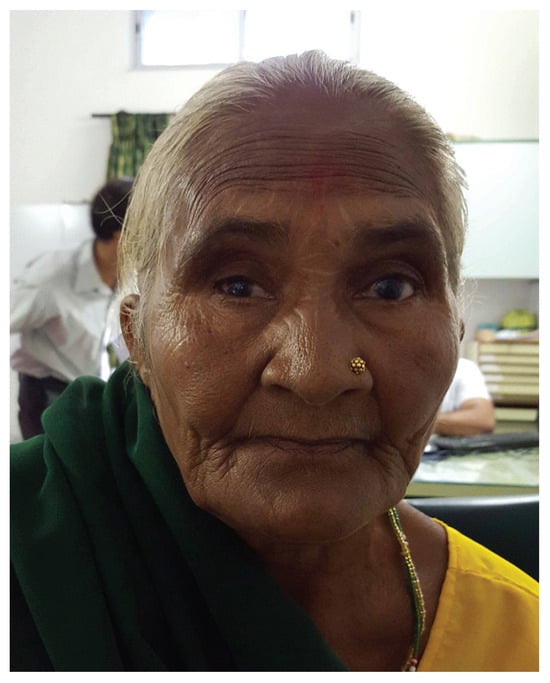
Figure 6.
Patient’s condition at 8 months postoperative period.
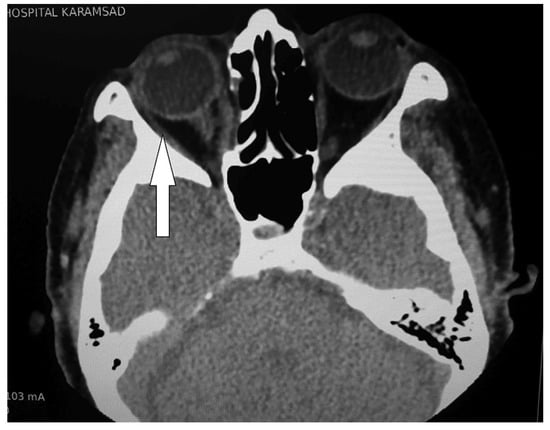
Figure 7.
Axial CT scan of orbit showing normally placed eyeball with healed ethmoid fracture at 8-month follow-up.

Figure 8.
Coronal CT scan of orbit showing normally placed eyeball with healed ethmoid fracture at 8-month follow-up.
Discussion
Orbital blow-out fractures are quite common and are on the rise due to increasing vehicular accidents. [5] Most cases of medial orbital blow-out injuries present with diplopia and enophthalmos. [6] Enophthalmos has shown a proportionate relation with medial wall fractures as compared with floor. [7]
However, this case was uncommon, as there was an absolute absence of eyeball from its socket which initially made an impression of complete destruction of the eye. An isolated history of ipsilateral nose bleed without any cranial signs did give us a clue in the diagnosis. Cases of displaced eyeball have been reported most commonly in floor orbit fractures with enophthalmos and bulge into the maxillary sinus. [8] A study has shown a bull gore injury causing displacement of the eye into the maxillary antrum which they reposited successfully but vision could not be restored due to optic atrophy. [9] Two research groups have described intracranial displacement of the orbital contents, by a fracture in the roof of the orbit. Though both suggest successful reposition of the eye into its socket, neither could achieve vision. [10,11] Only one similar case of medial orbital blowout fracture has been documented in which the eye had been displaced into the ethmoid sinus. Again they could not achieve vision. [12]
Immediate imaging probably played the most vital role in the rapid diagnosis. Computed tomography plays the most important role in these cases. An intact optic nerve is the most important factor that would predict postoperative vision regainment. All four studies documenting displacement of eye could not regain vision due to optic nerve injury or atrophy. [9,10,11,12] Retinal ischemia due to globe displacement was another cause stated by one of the studies. [12] A normal disc and macula on fundus examination on immediate postoperative day was a positive predictive factor. Computed tomography also gives us precise knowledge of the displacement of the eyeball that acts like a road map during the exploratory procedure. Ultrasonography which told us about a normal axial diameter and lens further boosted the idea that vision could be saved. Early operative intervention was crucial. Fractures diagnosed and treated early have a better prognosis than those treated late. [8]
A Korean study has documented that endonasal endoscopic reduction (EER) is quite effective and a safe procedure with good results. [13] Two other studies have compared EER combined with a transorbital subconjunctival approach to isolated conventional approach through the medial canthus. [14,15] Both have got excellent results in treatment of combined orbital floor and medial wall blow out fractures. Patients having persistent diplopia were sent for intraorbital surgery. Globe movement restriction was a drawback that has been noted by most studies, as seen by us as well. These studies have used external synthetic mesh to support the orbital wall along with Merocel packing. The mesh has to be removed in the postoperative period as documented by one study. [16] In contrast, we used the nasal septal cartilage as an allograft to support the lateral nasal wall which is easily available, most suitably accepted and does not require to be removed. It must be intercepted here that all these studies included cases having minimal orbital displacement, none so far documenting complete luxation of the eyeball in the nose. Rhee and Chen have illustrated endoscopic facial fracture reduction in an elaborate fashion. [17]
Conventionally, medial orbital wall fractures were approached by Lynch technique; however, it has a postoperative cutaneous scar. In comparison, EER has an excellent cosmetic result. [18]
Bull horn injuries are quite uncommon but are usually devastating and may lead to unilateral blindness. Most studies show lacerations and open globe injuries with poor visual outcomes. [19,20,21] Eye safety gear is recommended to all personnel involved in animal husbandry. Coagulation of calf horns after birth has also been advised.
Conclusion
Early surgical intervention is the key to good visual outcome in orbital blowout fractures. Endonasal endoscopic approach to medial orbital blow out fractures gives a promising result and must be promoted due to multilevel benefits. Preoperative evaluation of retina and optic nerve gives a clue on the likely visual prognosis. Thus, we recommend that every patient of displaced eye deserves a surgical intervention.
References
- Ko, M.J.; Morris, C.K.; Kim, J.W.; Lad, S.P.; Arrigo, R.T.; Lad, E.M. Orbital fractures: national inpatient trends and complications. Ophthal Plast Reconstr Surg 2013, 29, 298–303. [Google Scholar] [CrossRef] [PubMed]
- Vats, S.; Murthy, G.V.; Chandra, M.; Gupta, S.K.; Vashist, P.; Gogoi, M. Epidemiological study of ocular trauma in an urban slum population in Delhi, India. Indian J Ophthalmol 2008, 56, 313–316. [Google Scholar] [PubMed]
- Nirmalan, P.K.; Katz, J.; Tielsch, J.M.; et al.; Aravind Comprehensive Eye Survey Ocular trauma in a rural south Indian population: the Aravind Comprehensive Eye Survey. Ophthalmology 2004, 111, 1778–1781. [Google Scholar] [CrossRef]
- Burm, J.S.; Chung, C.H.; Oh, S.J. Pure orbital blowout fracture: new concepts and importance of medial orbital blowout fracture. Plast Reconstr Surg 1999, 103, 1839–1849. [Google Scholar] [CrossRef]
- Motamedi, M.H.; Dadgar, E.; Ebrahimi, A.; Shirani, G.; Haghighat, A.; Jamalpour, M.R. Pattern of maxillofacial fractures: a 5-year analysis of 8,818 patients. J Trauma Acute Care Surg 2014, 77, 630–634. [Google Scholar] [CrossRef] [PubMed]
- Boffano, P.; Roccia, F.; Gallesio, C.; Karagozoglu, K.H.; Forouzanfar, T. Diplopia and orbital wall fractures. J Craniofac Surg 2014, 25, e183–e185. [Google Scholar] [CrossRef]
- Yab, K.; Tajima, S.; Ohba, S. Displacements of eyeball in orbital blowout fractures. Plast Reconstr Surg 1997, 100, 1409–1417. [Google Scholar] [CrossRef]
- Converse, J.M.; Smith, B.; Obear, M.F.; Wood-Smith, D. Orbital blowout fractures: a ten-year survey. Plast Reconstr Surg 1967, 39, 20–36. [Google Scholar] [CrossRef]
- Singh, R.I.; Thomas, R.; Alexander, T.A. An unusual case of bull gore injury. Aust N Z J Ophthalmol 1986, 14, 377–379. [Google Scholar] [CrossRef]
- Miabi, Z.; Nezami, N.; Midia, M.; Midia, R. Intracranial displacement of the eye after blunt trauma. J Neuroophthalmol 2009, 29, 311. [Google Scholar] [CrossRef]
- Gollapudi, P.R.; Nandigama, P.K.; Maila, S.K.; Karla, R.; Kotakadira, S. Traumatic intracranial prolapse of eye ball a case report. Br J Neurosurg 2013, 27, 114–116. [Google Scholar] [CrossRef]
- Kang, B.D.; Jang, M.H. A case of blowout fracture of the orbital wall with eyeball entrapped within the ethmoid sinus. Korean J Ophthalmol 2003, 17, 149–153. [Google Scholar] [CrossRef]
- Jin, H.R.; Shin, S.O.; Choo, M.J.; Choi, Y.S. Endonasal endoscopic reduction of blowout fractures of the medial orbital wall. J Oral Maxillofac Surg 2000, 58, 847–851. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wu, W.; Yan, W.; Cannon, P.S.; Jiang, A.C. Endoscopic transethmoidal and transconjunctival inferior fornix approaches for repairing the combined medial wall and orbital floor blowout fractures. J Craniofac Surg 2011, 22, 537–542. [Google Scholar] [CrossRef] [PubMed]
- Shi, W.; Jia, R.; Li, Z.; He, D.; Fan, X. Combination of transorbital and endoscopic transnasal approaches to repair orbital medial wall and floor fractures. J Craniofac Surg 2012, 23, 71–74. [Google Scholar] [CrossRef] [PubMed]
- Jeon, S.Y.; Kwon, J.H.; Kim, J.P.; et al. Endoscopic intranasal reduction of the orbit in isolated blowout fractures. Acta Otolaryngol Suppl 2007, 102–109. [Google Scholar] [CrossRef]
- Rhee, J.S.; Chen, C.T. Endoscopic approach to medial orbital wall fractures. Facial Plast Surg Clin North Am 2006, 14, 17–23. [Google Scholar] [CrossRef]
- Humphrey, C.D.; Kriet, J.D. Surgical approaches to the orbit. Oper Tech Otolaryngol–Head Neck Surg 2008, 19, 132–139. [Google Scholar] [CrossRef]
- Goldblum, D.; Frueh, B.E.; Koerner, F. Eye injuries caused by cow horns. Retina 1999, 19, 314–317. [Google Scholar] [CrossRef]
- Onyekwe, L.O.; Ohaegbulam, S.C. Penetrating orbito-cranial and ocular cow-horn injuries. Niger J Clin Pract 2007, 10, 177–179. [Google Scholar]
- Ibrahim, O.; Olusanya, B. Occupational cow horn eye injuries in Ibadan, Nigeria. Ann Med Health Sci Res 2014, 4, 959–961. [Google Scholar] [PubMed]
© 2016 by the author. The Author(s) 2016.