Hyperferritinemia Is Associated with Higher Adiposity, Metabolic Syndrome, and Hepatic Dysfunction, Mainly Affecting Men: A Study in Southern Brazil
Abstract
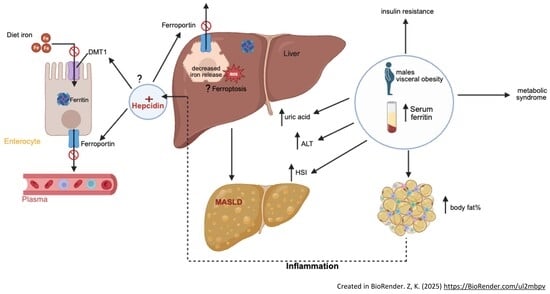
1. Introduction
2. Materials and Methods
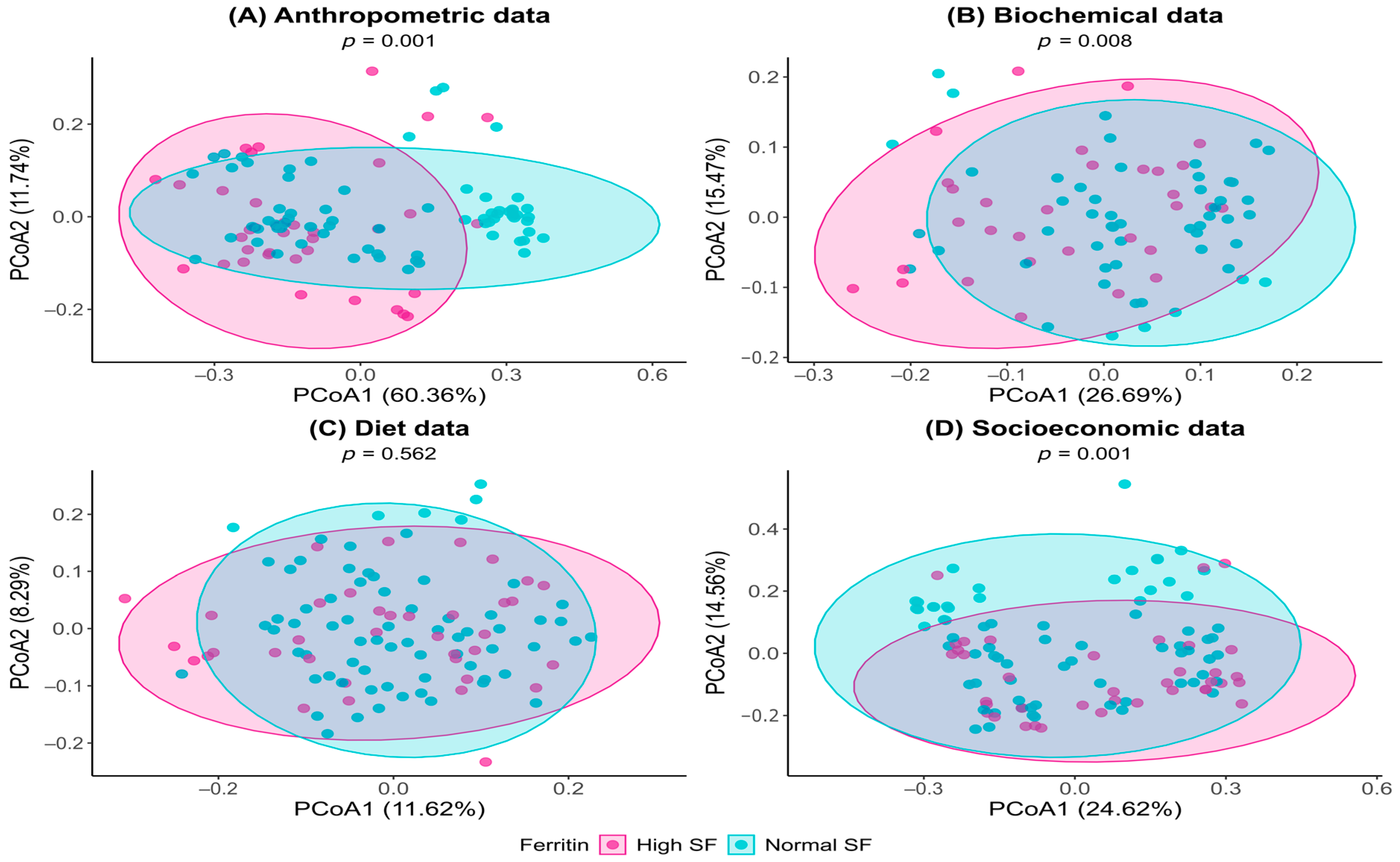
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| SF | Serum ferritin |
| TG | Tryglicerídes |
| TC | Total cholesterol |
| HDL | High density lipoprotein |
| LDL | Low density lipoprotein |
| IR | Insulin resistance |
| TyG | Glucose and triglycerides index |
| ESR | Erythrocyte sedimentation rate |
| CRP | C-reactive protein |
| UA | Uric acid |
| SBP | Systolic blood pressure |
| DPB | Diastolic blood pressure |
| ALT | Alanine transaminase |
| AST | Aspartate transaminase |
| HIS | Hepatic steatosis index |
| FIB-4 | Hepatic fibrose factor score |
| MS | Metabolic syndrome |
| BMI | Body mass index |
| WC | Waist circumference |
| WHR | Waist-to-hip ratio |
| BF | Body fat |
| LM | Lean mass |
| 24HR | 24-h diet recall |
| Kcal | kilocalories |
| g | Grams |
| SFA | Saturated fatty acid |
| MUFA | Monounsaturated fatty acid |
| PUFA | Polyunsaturated fatty acid |
| mg | Milligrams |
| ml | Milliliter |
Appendix A
| Variable | Category | Normal SF Median (Q1–Q3) | High SF Median (Q1–Q3) | p-Value |
|---|---|---|---|---|
| SBP (mmHg) | - | 117.5 (107.2–127) | 132 (113.2–140.2) | 0.952 b |
| DBP (mmHg) | - | 74.5 (68.2–80.8) | 81 (68.5–86.8) | 0.394 b |
| Glucose (mg/dL) | - | 77 (72–89) | 87 (80.2–97) | 0.127 b |
| TG (mg/dL) | - | 86 (61.5–117) | 114.5 (88.2–190.2) | 0.788 b |
| TyG | - | 4.4 (4.2–4.6) | 4.6 (4.5–4.9) | 0.927 b |
| TC (mg/dL) | - | 170.8 (147–192.5) | 185 (156.2–203) | 0.788 b |
| HDL (mg/dL) | - | 45 (41–48) | 40 (38–44.8) | 0.909 b |
| LDL (mg/dL) | - | 105.4 (81.9–124.7) | 105.7 (90.2–128.2) | 0.927 b |
| AST (U/L) | - | 27 (21–34) | 29 (22–38) | 0.679 b |
| ALT (U/L) | - | 20 (15–25.8) | 26 (20–35.6) | 0.630 b |
| FIB4 | - | 0.7 (0.5–1.2) | 0.9 (0.7–1.1) | 0.315 b |
| UA (mg/dL) | - | 4.2 (3.2–4.9) | 4.8 (3.6–6.1) | 0.648 b |
| ESR (mm) | - | 15 (10–24.8) | 12 (10–16) | 0.206 b |
| Platelets (mil/mm3) | - | 235 (209–283) | 249 (221–266) | 0.436 b |
| Leukocytes (mm3) | - | 6400 (5550–7800) | 6400 (5599.8–8950) | 0.788 b |
| Rod neutrophils (mm3) | - | 57 (40–72) | 61 (0–75) | 0.836 b |
| Eosinophils(mm3) | - | 144 (104–226.5) | 137 (69.2–191.2) | 0.648 b |
| Segmented neutrophils (mm3) | - | 3510 (3000–4298) | 3650 (2669–4929) | 0.788 b |
| Monocytes (mm3) | - | 300 (220–388) | 312 (252–456) | 0.527 b |
| Lymphocytes (mm3) | - | 2280 (1912–2668.5) | 2171.5 (2018–2606.8) | 0.927 b |
| HSI | - | 34.2 (30.9–38.6) | 39.9 (35.5–45.4) | 0.788 b |
| Variable | Category | Normal SF n (%) | High SF n (%) | p-Value |
|---|---|---|---|---|
| Cookies, cakes | Never or rarely | 15 (20.8%) | 7 (18.4%) | 0.744 a |
| Monthly | 12 (16.7%) | 4 (10.5%) | ||
| Weekly | 34 (47.2%) | 19 (50%) | ||
| Daily | 11 (15.3%) | 8 (21.1%) | ||
| Masses | Never or rarely | 5 (6.9%) | 4 (10.5%) | 0.534 b |
| Monthly | 9 (12.5%) | 5 (13.2%) | ||
| Weekly | 55 (76.4%) | 25 (65.8%) | ||
| Daily | 3 (4.2%) | 4 (10.5%) | ||
| Whole grains | Never or rarely | 32 (44.4%) | 13 (34.2%) | 0.257 b |
| Monthly | 3 (4.2%) | 3 (7.9%) | ||
| Weekly | 26 (36.1%) | 11 (28.9%) | ||
| Daily | 11 (15.3%) | 11 (28.9%) | ||
| Candy | Never or rarely | 12 (16.7%) | 6 (16.2%) | 0.091 b |
| Monthly | 5 (6.9%) | 6 (16.2%) | ||
| Weekly | 31 (43.1%) | 20 (54.1%) | ||
| Daily | 24 (33.3%) | 5 (13.5%) | ||
| Butter, bacon, lard, lard | Never or rarely | 29 (40.8%) | 11 (29.7%) | 0.212 b |
| Monthly | 3 (4.2%) | 3 (8.1%) | ||
| Weekly | 17 (23.9%) | 15 (40.5%) | ||
| Daily | 22 (31%) | 8 (21.6%) | ||
| Margarine, mayonnaise | Never or rarely | 34 (47.2%) | 14 (37.8%) | 0.428 b |
| Monthly | 3 (4.2%) | 0 (0%) | ||
| Weekly | 20 (27.8%) | 13 (35.1%) | ||
| Daily | 15 (20.8%) | 10 (27%) | ||
| Snacks | Never or rarely | 13 (18.1%) | 7 (18.9%) | 0.426 b |
| Monthly | 29 (40.3%) | 9 (24.3%) | ||
| Weekly | 28 (38.9%) | 19 (51.4%) | ||
| Daily | 2 (2.8%) | 2 (5.4%) | ||
| Preserved food | Never or rarely | 46 (63.9%) | 21 (56.8%) | 0.8 b |
| Monthly | 13 (18.1%) | 6 (16.2%) | ||
| Weekly | 12 (16.7%) | 9 (24.3%) | ||
| Daily | 1 (1.4%) | 1 (2.7%) | ||
| Fried foods | Never or rarely | 28 (38.9%) | 11 (29.7%) | 0.675 b |
| Monthly | 10 (13.9%) | 8 (21.6%) | ||
| Weekly | 29 (40.3%) | 16 (43.2%) | ||
| Daily | 5 (6.9%) | 2 (5.4%) | ||
| Vegetables | Never or rarely | 4 (5.6%) | 2 (5.4%) | 0.663 b |
| Monthly | 1 (1.4%) | 1 (2.7%) | ||
| Weekly | 25 (34.7%) | 17 (45.9%) | ||
| Daily | 42 (58.3%) | 17 (45.9%) | ||
| Beans | Never or rarely | 3 (4.2%) | 0 (0%) | 0.287 b |
| Monthly | 2 (2.8%) | 3 (7.9%) | ||
| Weekly | 23 (31.9%) | 15 (39.5%) | ||
| Daily | 44 (61.1%) | 20 (52.6%) | ||
| Leafy greens | Never or rarely | 3 (4.2%) | 2 (5.4%) | 1 b |
| Monthly | 1 (1.4%) | 0 (0%) | ||
| Weekly | 20 (27.8%) | 11 (29.7%) | ||
| Daily | 48 (66.7%) | 24 (64.9%) | ||
| Tubers | Never or rarely | 3 (4.2%) | 1 (2.7%) | 0.702 b |
| Monthly | 2 (2.8%) | 2 (5.4%) | ||
| Weekly | 55 (76.4%) | 25 (67.6%) | ||
| Daily | 12 (16.7%) | 9 (24.3%) | ||
| Fruits | Never or rarely | 1 (1.4%) | 3 (8.1%) | 0.376 b |
| Monthly | 1 (1.4%) | 1 (2.7%) | ||
| Weekly | 21 (29.2%) | 9 (24.3%) | ||
| Daily | 49 (68.1%) | 24 (64.9%) | ||
| Soft drinks, juices | Never or rarely | 28 (38.9%) | 18 (48.6%) | 0.557 b |
| Monthly | 6 (8.3%) | 1 (2.7%) | ||
| Weekly | 30 (41.7%) | 13 (35.1%) | ||
| Daily | 8 (11.1%) | 5 (13.5%) | ||
| Sweetener | Never or rarely | 66 (91.7%) | 33 (89.2%) | 1 b |
| Weekly | 1 (1.4%) | 1 (2.7%) | ||
| Daily | 5 (6.9%) | 3 (8.1%) | ||
| Diet e light | Never or rarely | 69 (95.8%) | 31 (83.8%) | 0.073 b |
| Monthly | 2 (2.8%) | 2 (5.4%) | ||
| Weekly | 1 (1.4%) | 2 (5.4%) | ||
| Daily | 0 (0%) | 2 (5.4%) | ||
| Ready-made seasonings | Never or rarely | 53 (73.6%) | 28 (75.7%) | 0.681 b |
| Monthly | 1 (1.4%) | 2 (5.4%) | ||
| Weekly | 6 (8.3%) | 3 (8.1%) | ||
| Daily | 12 (16.7%) | 4 (10.8%) | ||
| Sugar | Never or rarely | 21 (29.2%) | 15 (40.5%) | 0.024 b |
| Monthly | 0 (0%) | 3 (8.1%) # | ||
| Weekly | 18 (25%) | 4 (10.8%) | ||
| Daily | 33 (45.8%) | 15 (40.5%) | ||
| Oilseeds | Never or rarely | 36 (50%) | 16 (43.2%) | 0.857 a |
| Monthly | 9 (12.5%) | 6 (16.2%) | ||
| Weekly | 16 (22.2%) | 10 (27%) | ||
| Daily | 11 (15.3%) | 5 (13.5%) |
References
- Alshwaiyat, N.; Ahmad, A.; Wan Hassan, W.M.R.; Al-Jamal, H. Association between obesity and iron deficiency (Review). Exp. Ther. Med. 2021, 22, 1268. [Google Scholar] [CrossRef]
- Jomova, K.; Valko, M. Importance of iron chelation in free radical-induced oxidative stress and human disease. Curr. Pharm. Des. 2011, 17, 3460–3473. [Google Scholar] [CrossRef] [PubMed]
- Nairz, M.; Weiss, G. Iron in health and disease. Mol. Asp. Med. 2020, 75, 100906. [Google Scholar] [CrossRef]
- Knovich, M.A.; Storey, J.A.; Coffman, L.G.; Torti, S.V.; Torti, F.M. Ferritin for the clinician. Blood Rev. 2009, 23, 95–104. [Google Scholar] [CrossRef] [PubMed]
- Sandnes, M.; Ulvik, R.J.; Vorland, M.; Reikvam, H. Hyperferritinemia-A Clinical Overview. J. Clin. Med. 2021, 10, 2008. [Google Scholar] [CrossRef]
- Ding, X.; Bian, N.; Wang, J.; Chang, X.; An, Y.; Wang, G.; Liu, J. Serum Ferritin Levels Are Associated with Adipose Tissue Dysfunction-Related Indices in Obese Adults. Biol. Trace Elem. Res. 2023, 201, 636–643. [Google Scholar] [CrossRef]
- Liu, J.; Li, Q.; Yang, Y.; Ma, L. Iron metabolism and type 2 diabetes mellitus: A meta-analysis and systematic review. J. Diabetes Investig. 2020, 11, 946–955. [Google Scholar] [CrossRef]
- Fonseca, Ó.; Ramos, A.S.; Gomes, L.T.S.; Gomes, M.S.; Moreira, A.C. New Perspectives on Circulating Ferritin: Its Role in Health and Disease. Molecules 2023, 28, 7707. [Google Scholar] [CrossRef] [PubMed]
- Ganz, T. Macrophages and Iron Metabolism. Microbiol. Spectr. 2016, 4, 101128. [Google Scholar] [CrossRef]
- Cohen, L.A.; Gutierrez, L.; Weiss, A.; Leichtmann-Bardoogo, Y.; Zhang, D.L.; Crooks, D.R.; Sougrat, R.; Morgenstern, A.; Galy, B.; Hentze, M.W.; et al. Serum ferritin is derived primarily from macrophages through a nonclassical secretory pathway. Blood 2010, 116, 1574–1584. [Google Scholar] [CrossRef]
- Valenti, L.; Corradini, E.; Adams, L.A.; Aigner, E.; Alqahtani, S.; Arrese, M.; Bardou-Jacquet, E.; Bugianesi, E.; Fernandez-Real, J.M.; Girelli, D.; et al. Consensus Statement on the definition and classification of metabolic hyperferritinaemia. Nat. Rev. Endocrinol. 2023, 19, 299–310. [Google Scholar] [CrossRef] [PubMed]
- Caputo, T.; Gilardi, F.; Desvergne, B. From chronic overnutrition to metaflammation and insulin resistance: Adipose tissue and liver contributions. FEBS Lett. 2017, 591, 3061–3088. [Google Scholar] [CrossRef]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in underweight and obesity from 1990 to 2022: A pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet 2024, 403, 1027–1050. [Google Scholar] [CrossRef]
- González-Domínguez, Á.; Visiedo-Garcí, F.M.; Domínguez-Riscart, J.; González-Domínguez, R.; Mateos, R.M.; Lechuga-Sancho, A.M. Iron Metabolism in Obesity and Metabolic Syndrome. Int. J. Mol. Sci. 2020, 21, 5529. [Google Scholar] [CrossRef]
- Rubino, F.; Cummings, D.E.; Eckel, R.H.; Cohen, R.V.; Wilding, J.P.H.; Brown, W.A.; Stanford, F.C.; Batterham, R.L.; Farooqi, I.S.; Farpour-Lambert, N.J.; et al. Definition and diagnostic criteria of clinical obesity. Lancet Diabetes Endocrinol. 2025, 13, 221–262. [Google Scholar] [CrossRef]
- Kawai, T.; Autieri, M.V.; Scalia, R. Adipose tissue inflammation and metabolic dysfunction in obesity. Am. J. Physiol. Cell Physiol. 2021, 320, C375–C391. [Google Scholar] [CrossRef]
- Eslam, M.; Newsome, P.N.; Sarin, S.K.; Anstee, Q.M.; Targher, G.; Romero-Gomez, M.; Zelber-Sagi, S.; Wai-Sun Wong, V.; Dufour, J.F.; Schattenberg, J.M.; et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J. Hepatol. 2020, 73, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Anderson, E.R.; Shah, Y.M. Iron homeostasis in the liver. Compr. Physiol. 2013, 3, 315–330. [Google Scholar] [CrossRef] [PubMed]
- Purdy, J.C.; Shatzel, J.J. The hematologic consequences of obesity. Eur. J. Haematol. 2021, 106, 306–319. [Google Scholar] [CrossRef]
- Camaschella, C.; Nai, A.; Silvestri, L. Iron metabolism and iron disorders revisited in the hepcidin era. Haematologica 2020, 105, 260–272. [Google Scholar] [CrossRef]
- Sakurai, Y.; Kubota, N.; Yamauchi, T.; Kadowaki, T. Role of Insulin Resistance in MAFLD. Int. J. Mol. Sci. 2021, 22, 4156. [Google Scholar] [CrossRef]
- Jehn, M.; Clark, J.M.; Guallar, E. Serum ferritin and risk of the metabolic syndrome in U.S. adults. Diabetes Care 2004, 27, 2422–2428. [Google Scholar] [CrossRef]
- Chang, J.S.; Lin, S.M.; Huang, T.C.; Chao, J.C.; Chen, Y.C.; Pan, W.H.; Bai, C.H. Serum ferritin and risk of the metabolic syndrome: A population-based study. Asia Pac. J. Clin. Nutr. 2013, 22, 400–407. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Jiang, L.; Wang, H.; Shen, Z.; Cheng, Q.; Zhang, P.; Wang, J.; Wu, Q.; Fang, X.; Duan, L.; et al. Hepatic transferrin plays a role in systemic iron homeostasis and liver ferroptosis. Blood 2020, 136, 726–739. [Google Scholar] [CrossRef]
- Ru, Q.; Li, Y.; Chen, L. Iron homeostasis and ferroptosis in human diseases: Mechanisms and therapeutic prospects. Signal Transduct. Target. Ther. 2024, 9, 271. [Google Scholar] [CrossRef]
- Mo, M.; Pan, L.; Deng, L.; Liang, M.; Xia, N.; Liang, Y. Iron Overload Induces Hepatic Ferroptosis and Insulin Resistance by Inhibiting the Jak2/stat3/slc7a11 Signaling Pathway. Cell Biochem. Biophys. 2024, 82, 2079–2094. [Google Scholar] [CrossRef]
- Wang, H.; Sun, R.; Yang, S.; Ma, X.; Yu, C. Association between serum ferritin level and the various stages of non-alcoholic fatty liver disease: A systematic review. Front. Med. 2022, 9, 934989. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.U.; Cho, H.J. Body iron, serum ferritin, and nonalcoholic fatty liver disease. Korean J. Hepatol. 2012, 18, 105–107. [Google Scholar] [CrossRef]
- WHO. Guideline on Use of Ferritin Concentrations to Assess Iron Status in Individuals and Populations; World Health Organization: Geneva, Switzerland, 2020; Available online: https://www.who.int/publications/i/item/9789240000124 (accessed on 11 May 2023).
- ABEP. Critério de Classificação Econômica Brasil [Internet]; Associação Brasileira de Empresas de Pesquisa: São Paulo, Brazil, 2022; Available online: https://www.abep.org/criterioBr/01_cceb_2022.pdf (accessed on 10 June 2024).
- WHO. Guidelines on Physical Activity and Sedentary Behaviour [Internet]; World Health Organization: Geneva, Switzerland, 2020; Available online: https://www.who.int/publications/i/item/9789240015128 (accessed on 8 June 2023).
- Barroso, W.K.S.; Rodrigues, C.I.S.; Bortolotto, L.A.; Mota-Gomes, M.A.; Brandão, A.A.; Feitosa, A.D.M.; Machado, C.A.; Poli-de-Figueiredo, C.E.; Amodeo, C.; Mion Júnior, D.; et al. Diretrizes Brasileiras de Hipertensão Arterial—2020. Arq. Bras. De Cardiol. 2021, 116, 516–658. [Google Scholar] [CrossRef]
- Cotrim, H.P.; Parise, E.R.; Figueiredo-Mendes, C.; Galizzi-Filho, J.; Porta, G.; Oliveira, C.P. Nonalcoholic fatty liver disease Brazilian society of hepatology consensus. Arq. Gastroenterol. 2016, 53, 118–122. [Google Scholar] [CrossRef] [PubMed]
- Malta, D.C.; Gomes, C.S.; Almeida Alves, F.T.; Vasconcelos de Oliveira, P.P.; de Freitas, P.C.; Andreazzi, M. O uso de cigarro, narguilé, cigarro eletrônico e outros indicadores do tabaco entre escolares brasileiros: Dados da Pesquisa Nacional de Saúde do Escolar 2019. Rev. Bras. Epidemiol. 2022, 25, e220014. [Google Scholar] [CrossRef] [PubMed]
- Gordon, C.C.; Chumlea, W.C.; Roche, A.F. Stature, Recumbent Length, and Weight. In Anthropometric Standardization Reference Manual; Lohman, T.G., Roche, A.F., Martorell, R., Eds.; Human Kinetics Books: Champaign, IL, USA, 1988; pp. 3–8. [Google Scholar]
- WHO. Obesity: Preventing and Managing the Global Epidemic. Report of a WHO Consultation. World Health Organ. Tech. Rep. Ser. 2000, 894, 1–253. [Google Scholar]
- Callaway, C.W. Anthropometric Measurements. In Anthropometric Standardization Reference Manual; Lohman, T.G., Roche, A.F., Martorell, R., Eds.; Human Kinetics Books: Champaign, IL, USA, 1988; pp. 39–54. [Google Scholar]
- Biodynamics Corporation. Manual de Instrução do Monitor de Composição Corporal Biodynamics Modelo 450, Version v.5.1; International TBW: São Paulo, Brazil, 2007. [Google Scholar]
- Lohman, T.G. Advances in Body Composition Assessment: Current Issues in Exercise Science; Human Kinetics Publishers: Champaign, IL, USA, 1992. [Google Scholar]
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimation of the Concentration of Low-Density Lipoprotein Cholesterol in Plasma, without Use of the Preparative Ultracentrifuge. Clin. Chem. 1972, 18, 499–502. [Google Scholar] [CrossRef]
- Guerrero-Romero, F.; Villalobos-Molina, R.; Jiménez-Flores, J.R.; Simental-Mendía, L.E.; Méndez-Cruz, R.; Murguía-Romero, M.; Rodríguez-Morán, L. Fasting Triglycerides and Glucose Index as a Diagnostic Test for Insulin Resistance in Young Adults. Arch. Med. Res. 2016, 47, 382–387. [Google Scholar] [CrossRef]
- Simental-Mendía, L.E.; Guerrero-Romero, F. The Correct Formula for the Triglycerides and Glucose Index. Eur. J. Pediatr. 2020, 179, 1171. [Google Scholar] [CrossRef]
- Kratz, A.; Plebani, M.; Peng, M.; Lee, Y.K.; McCafferty, R.; Machin, S.J.; International Council for Standardization in Haematology (ICSH). ICSH Recommendations for Modified and Alternate Methods Measuring the Erythrocyte Sedimentation Rate. Int. J. Lab. Hematol. 2017, 39, 448–457. [Google Scholar] [CrossRef] [PubMed]
- International Diabetes Federation (IDF). The IDF Consensus Worldwide Definition of the Metabolic Syndrome; IDF Communications: Brussels, Belgium, 2006; Available online: https://idf.org/media/uploads/2023/05/attachments-30.pdf (accessed on 25 October 2025).
- Précoma, D.B.; Oliveira, G.M.M.; Simão, A.F.; Dutra, O.P.; Coelho, O.R.; Izar, M.C.O.; Póvoa, R.M.D.S.; Giuliano, I.C.B.; Alencar Filho, A.C.; Machado, C.A.; et al. Updated Cardiovascular Prevention Guideline of the Brazilian Society of Cardiology—2019. Arq. Bras. Cardiol. 2019, 113, 787–891. [Google Scholar] [CrossRef]
- Wetteland, P.; Roger, M.; Solberg, H.E.; Iversen, O.H. Population-Based Erythrocyte Sedimentation Rates in 3,910 Subjectively Healthy Norwegian Adults: A Statistical Study Based on Men and Women from the Oslo Area. J. Intern. Med. 1996, 240, 125–131. [Google Scholar] [CrossRef]
- Khedr, D.; Nabil, S.; Abdulrazek, A.A.; Abdelnaby, A.; Lotfy, S. The C-Reactive Protein/Albumin Ratio as an Early Diagnostic Marker of Neonatal Sepsis in Preterm Neonates: A Case-Control Study. Pediatr. Sci. J. 2024, 4, 103–110. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, D.; Kim, H.J.; Lee, C.H.; Yang, J.I.; Kim, W.; Kim, Y.J.; Yoon, J.H.; Cho, S.H.; Sung, M.W.; et al. Hepatic Steatosis Index: A Simple Screening Tool Reflecting Nonalcoholic Fatty Liver Disease. Dig. Liver Dis. 2010, 42, 503–508. [Google Scholar] [CrossRef]
- Shah, A.G.; Lydecker, A.; Murray, K.; Tetri, B.N.; Contos, M.J.; Sanyal, A.J.; Nash Clinical Research Network. Comparison of Noninvasive Markers of Fibrosis in Patients With Nonalcoholic Fatty Liver Disease. Clin. Gastroenterol. Hepatol. 2009, 7, 1104–1112. [Google Scholar] [CrossRef]
- Instituto Brasileiro de Geografia e Estatística (IBGE). Pesquisa de Orçamentos Familiares (POF 2008-2009): Tabela de Medidas Referidas Para os Alimentos Consumidos no Brasil; Rio de Janeiro, 2011. Available online: https://biblioteca.ibge.gov.br/visualizacao/livros/liv50000.pdf (accessed on 20 May 2023).
- Pinheiro, A.B.V.; Lacerda, E.M.; Benzecry, E.H.; da Costa e Marisa Conceição da S, V.M. Tabela Para Avaliação Alimentar em Medidas Caseiras, 5th ed.; Atheneu: São Paulo, Brazil, 2008; p. 131. [Google Scholar]
- Universidade de São Paulo (USP), Food Research Center (FoRC). Tabela Brasileira de Composição de Alimentos (TBCA); Universidade de São Paulo (USP), Food Research Center (FoRC): São Paulo, Brazil, 2023; Version 7.2.; Available online: http://www.fcf.usp.br/tbca (accessed on 17 June 2023).
- Monsen, E.R.; Hallberg, L.; Layrisse, M.; Hegsted, M.D.; Cook, J.D.; Mertz, W.; Finch, C.A. Estimation of Available Dietary Iron. Am. J. Clin. Nutr. 1978, 31, 134–141. [Google Scholar] [CrossRef]
- Datz, C.; Müller, E.; Aigner, E. Iron overload and non-alcoholic fatty liver disease. Minerva Endocrinol. 2016, 42, 173–183. [Google Scholar] [CrossRef]
- Shang, X.; Zhang, R.; Wang, X.; Yao, J.; Zhao, X.; Li, H. The relationship of hyperferritinemia to metabolism and chronic complications in type 2 diabetes. Diabetes Metab. Syndr. Obes. Targets Ther. 2022, 15, 175–182. [Google Scholar] [CrossRef]
- Huenur, J.F.; Parodi Cruzat, M.; Aravena González, C.; Eymin Lago, G.; Triantafilo Cerda, N.; Walkowiak Navas, S.; Valenzuela Suárez, A.; Corsi Sotelo, O. Hyperferritinemia in a Chilean Academic Healthcare Network: A Retrospective Study. Rev. Méd. Chile 2023, 151, 412–419. [Google Scholar] [CrossRef]
- Akgun, Y. Association Between Race and Blood Ferritin Level of Whole Blood Donors. Cureus. 2025, 17, e82926. [Google Scholar] [CrossRef] [PubMed]
- Ding, J.; Xu, Z.; Liang, R.; Xie, S. Association Between Dietary Inflammatory Index and Triglyceride Glucose-Body Mass Index with Iron Deficiency in Reproductive Age Women: Evidence from NHANES 2005–2018. Int. J. Women’s Health 2025, 17, 355–367. [Google Scholar] [CrossRef] [PubMed]
- Thiele, S.; Mensink, G.B.; Beitz, R. Determinants of Diet Quality. Public Health Nutr. 2004, 7, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Hiza, H.A.; Casavale, K.O.; Guenther, P.M.; Davis, C.A. Diet Quality of Americans Differs by Age, Sex, Race/Ethnicity, Income, and Education Level. J. Acad. Nutr. Diet. 2013, 113, 297–306. [Google Scholar] [CrossRef]
- Milman, N.; Kirchhoff, M. Relationship Between Serum Ferritin, Alcohol Intake, and Social Status in 2235 Danish Men and Women. Ann. Hematol. 1996, 72, 145–151. [Google Scholar] [CrossRef]
- Koppe, T.; Doneda, D.; Siebert, M.; Paskulin, L.; Camargo, M.; Tirelli, K.M.; Vairo, F.; Daudt, L.; Schwartz, I.V. The Prognostic Value of the Serum Ferritin in a Southern Brazilian Cohort of Individuals with Gaucher Disease. Genet. Mol. Biol. 2016, 39, 30–34. [Google Scholar] [CrossRef]
- Park, S.K.; Ryoo, J.H.; Kim, M.G.; Shin, J.Y. Association of Serum Ferritin and the Development of Metabolic Syndrome in Middle-Aged Korean Men: A 5-Year Follow-Up Study. Diabetes Care 2012, 35, 2521–2526. [Google Scholar] [CrossRef] [PubMed]
- Iglesias-Vázquez, L.; Arija, V.; Aranda, N.; Aglago, E.K.; Cross, A.J.; Schulze, M.B.; Quintana Pacheco, D.; Kühn, T.; Weiderpass, E.; Tumino, R.; et al. Factors Associated with Serum Ferritin Levels and Iron Excess: Results from the EPIC-EurGast Study. Eur. J. Nutr. 2022, 61, 101–114. [Google Scholar] [CrossRef] [PubMed]
- Hu, P.J.; Ley, S.H.; Bhupathiraju, S.N.; Li, Y.; Wang, D.D. Associations of Dietary, Lifestyle, and Sociodemographic Factors with Iron Status in Chinese Adults: A Cross-Sectional Study in the China Health and Nutrition Survey. Am. J. Clin. Nutr. 2017, 105, 503–512. [Google Scholar] [CrossRef]
- Suárez-Ortegón, M.F.; Ensaldo-Carrasco, E.; Shi, T.; McLachlan, S.; Fernández-Real, J.M.; Wild, S.H. Ferritin, Metabolic Syndrome and Its Components: A Systematic Review and Meta-Analysis. Atherosclerosis 2018, 275, 97–106. [Google Scholar] [CrossRef]
- Miao, R.; Fang, X.; Zhang, Y.; Wei, J.; Zhang, Y.; Tian, J. Iron Metabolism and Ferroptosis in Type 2 Diabetes Mellitus and Complications: Mechanisms and Therapeutic Opportunities. Cell Death Dis. 2023, 14, 186. [Google Scholar] [CrossRef]
- Stockwell, B.R.; Friedmann Angeli, J.P.; Bayir, H.; Bush, A.I.; Conrad, M.; Dixon, S.J.; Fulda, S.; Gascón, S.; Hatzios, S.K.; Kagan, V.E.; et al. Ferroptosis: A Regulated Cell Death Nexus Linking Metabolism, Redox Biology, and Disease. Cell 2017, 171, 273–285. [Google Scholar] [CrossRef]
- Tsuchiya, H.; Ebata, Y.; Sakabe, T.; Hama, S.; Kogure, K.; Shiota, G. High-Fat, High-Fructose Diet Induces Hepatic Iron Overload via a Hepcidin-Independent Mechanism Prior to the Onset of Liver Steatosis and Insulin Resistance in Mice. Metabolism 2013, 62, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.C.C.; Huang, Y.F.; Wang, J.D. Hyperferritinemia and Hyperuricemia May Be Associated with Liver Function Abnormality in Obese Adolescents. PLoS ONE 2012, 7, e48645. [Google Scholar] [CrossRef]
- Ghio, A.J.; Ford, E.S.; Kennedy, T.P.; Hoidal, J.R. The Association Between Serum Ferritin and Uric Acid in Humans. Free Radic. Res. 2005, 39, 337–342. [Google Scholar] [CrossRef]
- Lombardi, R.; Pisano, G.; Fargion, S. Role of Serum Uric Acid and Ferritin in the Development and Progression of NAFLD. Int. J. Mol. Sci. 2016, 17, 548. [Google Scholar] [CrossRef]
- Bae, M.; Kim, K.M.; Jin, M.H.; Yoon, J.H. Synergistic Impact of Serum Uric Acid and Ferritin on MAFLD Risk: A Comprehensive Cohort Analysis. Sci. Rep. 2025, 15, 18936. [Google Scholar] [CrossRef]
- Mota, J.F.; Medina, W.L.; Moreto, F.; Burini, R.C. Influência da Adiposidade Sobre o Risco Inflamatório em Pacientes com Glicemia de Jejum Alterada. Rev. Nutr. 2009, 22, 351–357. [Google Scholar] [CrossRef][Green Version]
- Moriles, K.E.; Zubair, M.; Azer, S.A. Alanine Aminotransferase (ALT) Test. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK559278 (accessed on 27 February 2024).
- He, A.; Zhou, Z.; Huang, L.; Yip, K.C.; Chen, J.; Yan, R.; Li, R. Association Between Serum Iron and Liver Transaminases Based on a Large Adult Women Population. J. Health Popul. Nutr. 2023, 42, 69. [Google Scholar] [CrossRef]
- Priego-Parra, B.A.; Triana-Romero, A.; Martínez-Pérez, G.P.; Reyes-Díaz, S.A.; Ordaz-Álvarez, H.R.; Bernal-Reyes, R.; Icaza-Chávez, M.E.; Martínez-Vázquez, S.E.; Cano-Contreras, A.D.; Vivanco-Cid, H.; et al. Hepatic Steatosis Index (HSI): A Valuable Biomarker in Subjects with Metabolic Dysfunction-Associated Fatty Liver Disease (MAFLD). Ann. Hepatol. 2024, 29, 101391. [Google Scholar] [CrossRef]
- Shah, R.A.; Kowdley, K.V. Serum Ferritin as a Biomarker for NAFLD: Ready for Prime Time? Hepatol. Int. 2019, 13, 110–112. [Google Scholar] [CrossRef] [PubMed]
- Armandi, A.; Sanavia, T.; Younes, R.; Caviglia, G.P.; Rosso, C.; Govaere, O.; Liguori, A.; Francione, P.; Gallego-Duràn, R.; Ampuero, J.; et al. Serum Ferritin Levels Can Predict Long-Term Outcomes in Individuals with Metabolic Dysfunction-Associated Steatotic Liver Disease. Gut 2024, 73, 825–834. [Google Scholar] [CrossRef]
- Buzzetti, E.; Petta, S.; Manuguerra, R.; Luong, T.V.; Cabibi, D.; Corradini, E.; Craxì, A.; Pinzani, M.; Tsochatzis, E.; Pietrangelo, A. Evaluating the Association of Serum Ferritin and Hepatic Iron with Disease Severity in Non-Alcoholic Fatty Liver Disease. Liver Int. 2019, 39, 1662–1670. [Google Scholar] [CrossRef]
- Pietrangelo, A. Iron and the Liver. Liver Int. 2016, 36, 116–123. [Google Scholar] [CrossRef]
- Shen, X.; Yu, Z.; Wei, C.; Hu, C.; Chen, J. Iron metabolism and ferroptosis in nonalcoholic fatty liver disease. Am. J. Physiol. Endocrinol. Metab. 2024, 326, E767–E775. [Google Scholar] [CrossRef] [PubMed]
- Pellegrini, M.; Rahimi, F.; Boschetti, S.; Devecchi, A.; De Francesco, A.; Mancino, M.V.; Toppino, M.; Morino, M.; Fanni, G.; Ponzo, V.; et al. Pre-operative Micronutrient Deficiencies in Individuals with Severe Obesity Candidates for Bariatric Surgery. J. Endocrinol. Investig. 2021, 44, 1413–1423. [Google Scholar] [CrossRef]
- Institute of Medicine. Dietary Reference Intakes: The Essential Guide to Nutrient Requirements; National Academies Press: Washington, DC, USA, 2006. [Google Scholar] [CrossRef]
- Dutt, S.; Hamza, I.; Bartnikas, T.B. Molecular Mechanisms of Iron and Heme Metabolism. Annu. Rev. Nutr. 2022, 42, 311–335. [Google Scholar] [CrossRef]
- Piskin, E.; Cianciosi, D.; Gulec, S.; Tomas, M.; Capanoglu, E. Iron Absorption: Factors, Limitations, and Improvement Methods. ACS Omega 2022, 7, 20441–20456. [Google Scholar] [CrossRef]
- Young, I.; Parker, H.M.; Rangan, A.; Prvan, T.; Cook, R.L.; Donges, C.E.; Steinbeck, K.S.; O’Dwyer, N.J.; Cheng, H.L.; Franklin, J.L.; et al. Association between Haem and Non-Haem Iron Intake and Serum Ferritin in Healthy Young Women. Nutrients 2018, 10, 81. [Google Scholar] [CrossRef]
- Teucher, B.; Olivares, M.; Cori, H. Enhancers of Iron Absorption: Ascorbic Acid and Other Organic Acids. Int. J. Vitam. Nutr. Res. 2004, 74, 403–419. [Google Scholar] [CrossRef] [PubMed]
- Weschenfelder, C.; Berryman, C.E.; Hennigar, S.R. Dietary Iron Intake and Obesity-Related Diseases. Curr. Diab. Rep. 2025, 25, 34. [Google Scholar] [CrossRef] [PubMed]
- Li, H. Iron and the Intestinal Microbiome. Adv. Exp. Med. Biol. 2025, 1480, 345–360. [Google Scholar] [CrossRef] [PubMed]
- Badenhorst, C.E.; Dawson, B.; Cox, G.R.; Laarakkers, C.M.; Swinkels, D.W.; Peeling, P. Acute Dietary Carbohydrate Manipulation and the Subsequent Inflammatory and Hepcidin Responses to Exercise. Eur. J. Appl. Physiol. 2015, 115, 2521–2530. [Google Scholar] [CrossRef]
- Hayashi, N.; Ishibashi, A.; Iwata, A.; Yatsutani, H.; Badenhorst, C.; Goto, K. Influence of an Energy Deficient and Low Carbohydrate Acute Dietary Manipulation on Iron Regulation in Young Females. Physiol. Rep. 2022, 10, e15351. [Google Scholar] [CrossRef]
- Ludwig, D.S.; Ebbeling, C.B. The Carbohydrate-Insulin Model of Obesity: Beyond “Calories In, Calories Out”. JAMA Intern. Med. 2018, 178, 1098–1103. [Google Scholar] [CrossRef]
- Palmer, B.F.; Clegg, D.J. The Sexual Dimorphism of Obesity. Mol. Cell. Endocrinol. 2015, 402, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Brasil Ministério da Saúde. Manual de Atenção à Mulher no Climatério/Menopausa; Editora do Ministério da Saúde: Brasília, Brazil, 2008. Available online: https://bvsms.saude.gov.br/bvs/publicacoes/manual_atencao_mulher_climaterio.pdf (accessed on 28 June 2025).
- Raina, S.K. Limitations of 24-Hour Recall Method: Micronutrient Intake and the Presence of the Metabolic Syndrome. N. Am. J. Med. Sci. 2013, 5, 498. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Cheng, Z. Cross-Sectional Studies: Strengths, Weaknesses, and Recommendations. Chest 2020, 158, S65–S71. [Google Scholar] [CrossRef] [PubMed]
- Mörwald, K.; Aigner, E.; Bergsten, P.; Brunner, S.M.; Forslund, A.; Kullberg, J.; Ahlström, H.; Manell, H.; Roomp, K.; Schütz, S.; et al. Serum Ferritin Correlates with Liver Fat in Male Adolescents with Obesity. Front. Endocrinol. 2020, 18, 340. [Google Scholar] [CrossRef]
- Aguree, S.; Reddy, M.B. Inflammatory Markers and Hepcidin are Elevated but Serum Iron is Lower in Obese Women of Reproductive Age. Nutrients 2021, 13, 217. [Google Scholar] [CrossRef]

| Serum Biochemistry | Classification | Reference |
|---|---|---|
| SF | Normal (15 a 150 ng/mL for female and 15 a 200 ng/mL for male) High SF (>150 ng/mL for female and >200 ng/mL for male). | WHO [29]. |
| Glucose | Normal (<100 mg/dL); High (>100 mg/dL), for both sexes. | International Diabetes Federation (IDF) [44]. |
| TG | Normal (<150 mg/dL); High (>150 mg/dL), for both sexes. | IDF [44]. |
| TC | Normal (<190 mg/dL); High (>190 mg/dL), for both sexes. | Précoma et al. [45]. |
| HDL | Normal (female > 50 mg/dL and male > 40 mg/dL); Decreased (<50 mg/dL female and <40 mg/dL male). | IDF [44]. |
| LDL | Normal (<130 mg/dL); High (>130 mg/dL), for both sexes. | Précoma et al. [45]. |
| TyG | >4.55 to female and >4.68 to male were indicative of IR. | Guerrero-Romero et al. [41]. |
| ESR | Normal (female < 20 mm and High > 20 mm); Normal (male < 10 mm and High > 10 mm). | Wetteland et al. [46]. |
| CRP | <5mg/dL (Negative); >5 mg/dL (Positive). | Khedr et al. [47]. |
| UA | Decreased (<1.5 mg/dL); Normal (1.5 to 6 mg/dL); High (>6 mg/dL), for both sexes. | Laboratory |
| Hypertension | No (SBP: <130 mmHg and DBP < 85 mmHg); Yes (SBP: >130 mmHg and DBP > 85 mmHg) or in hypertension treatment, for both sexes. | IDF [44]. |
| AST and ALT | Decreased (<10 U/L); Normal (10 a 37 U/L); High (>37 U/L), for both sexes. | Laboratory. |
| HSI | Yes (>36) No (<36) | Lee et al. [48]. |
| FIB-4 | No risk of fibrosis (score < 1.3); Risk of fibrosis (>1.3), for both sexes. | Shah et al. [49]. |
| Variable | Category | Normal SF n (%) | High SF n (%) | p-Value |
|---|---|---|---|---|
| Sex | Female | 67 (89.3%) # | 20 (52.6%) | <0.0001 a |
| Male | 8 (10.7%) | 18 (47.4%) # | ||
| Age | - | 31 (23–41.5) | 41 (31.2–49.8) | 0.315 c |
| Marital Status | Single | 40 (53.3%) # | 8 (21.1%) | 0.012 b |
| Married/Civil Union | 28 (37.4%) | 25 (65.7%) # | ||
| Divorced | 4 (5.3%) | 3 (7.9%) | ||
| Widower | 3 (4%) | 2 (5.3%) | ||
| Education | Incomplete Elementary Education | 6 (8%) | 6 (15.8%) | 0.009 b |
| Complete Elementary Education | 1 (1.3%) | 0 (0%) | ||
| Incomplete High School | 2 (2.7%) | 1 (2.6%) | ||
| Complete High School | 15 (20%) | 16 (42.1%) # | ||
| Incomplete Higher Education | 27 (36%)# | 2 (5.3%) | ||
| Complete Higher Education | 19 (25.3%) | 11 (28.9%) | ||
| Posgraduate | 5 (6.7%) | 2 (5.3%) | ||
| Family Income Class | AB | 14 (26.3%) | 10 (18.9%) | 0.387 a |
| C | 43 (60.5%) | 23 (58.1%) | ||
| DE | 17 (13.2%) | 5 (23%) | ||
| Smoker | No | 69 (92%) | 35 (92.1%) | 0.984 a |
| Yes | 6 (8%) | 3 (7.9%) | ||
| Alcohol Consumption | No | 41 (54.7%) | 20 (52.6%) | 0.838 a |
| Yes | 34 (45.3%) | 18 (47.4%) | ||
| Classification of Alcohol Consumption | Not Excessive | 68 (90.7%) | 37 (97.4%) | 0.189 a |
| Excessive | 7 (9.3%) | 1 (2.6%) | ||
| Physical Activity | No | 27 (36%) | 16 (42.1%) | 0.528 a |
| Yes | 48 (64%) | 22 (57.9%) | ||
| Minutes per week | - | 150 (0–300) | 120 (0–281.2) | 0.661 c |
| Active | No | 36 (48%) | 22 (57.9%) | 0.320 a |
| Yes | 39 (52%) | 16 (42.1%) |
| Variable | Category | Normal SF n (%) | High SF n (%) | p-Value |
|---|---|---|---|---|
| BMI | Underweight | 3 (4%) | 0 (0%) | 0.003 b |
| Eutrophic | 31 (41.3%) # | 5 (13.2%) | ||
| Overweight | 20 (26.7%) | 12 (31.6%) | ||
| Obesity | 21 (28%) | 21 (55.3%) # | ||
| WC | No Risk | 37 (49.3%) # | 8 (21.1%) | 0.004 a |
| With Risk | 38 (50.7%) | 30 (78.9%) # | ||
| WHR | No Risk | 57 (77%) | 28 (73.7%) | 0.874 a |
| With Risk | 17 (23%) | 10 (26.3%) | ||
| BF% | Acceptable | 40 (54.8%) # | 9 (24.3%) | 0.002 a |
| High | 33 (45.2%) | 28 (75.7%) # | ||
| LM% | - | 70 ± 8.1 | 68.4 ± 6.8 | 0.301 c |
| Variable | Category | Normal SF n (%) | High SF n (%) | p-Value |
|---|---|---|---|---|
| Glucose | Normal | 67 (91.8%) # | 29 (76.3%) | 0.023 a |
| High | 6 (8.2%) | 9 (23.7%) # | ||
| TG | Normal | 65 (86.7%) # | 24 (63.2%) | 0.003 a |
| High | 10 (13.3%) | 14 (36.8%) # | ||
| TC | Normal | 54 (70.1%) | 21 (58.3%) | 0.216 a |
| High | 23 (29.9%) | 15 (41.7%) | ||
| HDL | Normal | 13 (17.3%) | 9 (23.7%) | 0.420 a |
| Decreased | 62 (82.7%) | 29 (76.3%) | ||
| LDL | Normal | 58 (77.3%) | 28 (73.7%) | 0.667 a |
| High | 17 (22.7%) | 10 (26.3%) | ||
| IR | No | 52 (71.2%) # | 19 (50%) | 0.027 a |
| Yes | 21 (28.8%) | 19 (50%) # | ||
| CRP | Negative | 40 (66.7%) | 24 (68.6%) | 0.849 a |
| Positive | 20 (33.3%) | 11 (31.4%) | ||
| ESR | Normal | 31 (53.4%) | 20 (57.1%) | 0.729 a |
| High | 27 (46.6%) | 15 (42.9%) | ||
| Hypertension | Yes | 16 (21.3%) | 19 (50%) # | 0.001 a |
| No | 59 (78.7%) # | 19 (50%) | ||
| MS | No | 59 (78.7%) # | 18 (47.4%) | 0.001 a |
| Yes | 16 (21.3%) | 20 (52.6%) # |
| Variable | Category | Normal SF n (%) | High SF n (%) | p-Value |
|---|---|---|---|---|
| UA | Decreased | 1 (1.5%) | 0 (0%) | 0.016 b |
| Normal | 60 (88.2%) # | 27 (71%) | ||
| High | 7 (10.3%) | 11 (29%) # | ||
| AST | Normal | 58 (82.8%) | 27 (73%) | 0.228 a |
| High | 12 (17.2%) | 10 (27%) | ||
| ALT | Decreased | 1 (1.4%) | 0 (0%) | 0.008 b |
| Normal | 66 (94.3%) # | 29 (78.4%) | ||
| High | 3 (4.3%) | 8 (21.6%) # | ||
| FIB4 | No Risk fibrosis | 56 (83.6%) | 30 (83.3%) | 0.974 a |
| With Risk fibrosis | 11 (16.4%) | 6 (16.7%) | ||
| HSI > 36 | No | 39 (55.7%) # | 12 (32.4%) | 0.022 a |
| Yes | 31 (44.3%) | 25 (67.6%) # |
| Variable | Normal SF Median (Q1–Q3) | High SF Median (Q1–Q3) | p-Value |
|---|---|---|---|
| Energy (kcal) | 1692 (1315–1995) | 1718 (1076.2–2411.2) | 0.412 a |
| Carbohydrate (g) | 189.5 (146.7–278.5) | 212.2 (129.9–287.1) | 0.024 a |
| Protein (g) | 68.6 (52.3–97.2) | 79.5 (60.7–107) | 0.788 a |
| Lipids (g) | 55.7 (40–74.8) | 64.3 (36–88.1) | 0.164 a |
| SFA (g) | 17.8 (11.8–25) | 18.2 (12.6–28) | 0.315 a |
| MUFA (g) | 15.6 (11.2–22.9) | 18.4 (11.4–24.7) | 0.412 a |
| PUFA (g) | 12.3 (9.2–17.6) | 12.9 (9.3–18.4) | 0.927 a |
| Cholesterol (mg) | 261.9 (167.8–426.9) | 270.1 (178.3–477.3) | 0.527 a |
| Fibers (g) | 18.3 (10.9–25.4) | 22.7 (15.8–30.4) | 0.073 a |
| Per capita oil (ml) | 10 (6.6–15) | 10 (6.1–15) | 0.970 a |
| Per capita lard (g) | 5.5 (2.6–14.7) | 5.6 (4.2–8.3) | 0.558 a |
| Total vitamin C (mg) | 49.2 (20.4–119) | 57.1 (25.5–137.3) | 0.648 a |
| Total meat (g) | 120 (60–217.5) | 150 (100.5–200) | 0.927 a |
| Total iron (mg) | 10.9 (7.5–14.4) | 10.1 (6.5–13.1) | 0.164 a |
| Total heme iron (mg) | 0.9 (0.3–1.8) | 0.8 (0.3–1.9) | 0.788 a |
| Total non-heme iron (mg) | 9.3 (6.8–12.5) | 9.2 (5.6–12.6) | 0.164 a |
| Total iron absorbed (mg) | 0.7 (0.5–1.1) | 0.6 (0.5–0.9) | 0.315 a |
| Source | Value | Pr > χ2 | OR [IC 95%] * |
|---|---|---|---|
| Intercept | −2.46 | <0.0001 | |
| Sex-Female | 0.00 | ||
| Sex-Male | 2.82 | <0.0001 | 16.82 [4.48–63.1] |
| BF%-Acceptable | 0.00 | ||
| BF%-Elevated | 2.02 | 0.004 | 7.5 [1.94–29.03] |
| HSI < 36-No | 0.00 | ||
| HSI > 36-Yes | −0.43 | 0.47 | 0.65 [0.20–2.11] |
| MS-No | 0.00 | ||
| MS-Yes | 0.55 | 0.29 | 1.74 [0.62–4.84] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zanuzo, K.; Nishiyama, M.F.; Koehnlein, E.A.; Grassiolli, S. Hyperferritinemia Is Associated with Higher Adiposity, Metabolic Syndrome, and Hepatic Dysfunction, Mainly Affecting Men: A Study in Southern Brazil. Pathophysiology 2025, 32, 64. https://doi.org/10.3390/pathophysiology32040064
Zanuzo K, Nishiyama MF, Koehnlein EA, Grassiolli S. Hyperferritinemia Is Associated with Higher Adiposity, Metabolic Syndrome, and Hepatic Dysfunction, Mainly Affecting Men: A Study in Southern Brazil. Pathophysiology. 2025; 32(4):64. https://doi.org/10.3390/pathophysiology32040064
Chicago/Turabian StyleZanuzo, Késia, Márcia Fernandes Nishiyama, Eloá Angélica Koehnlein, and Sabrina Grassiolli. 2025. "Hyperferritinemia Is Associated with Higher Adiposity, Metabolic Syndrome, and Hepatic Dysfunction, Mainly Affecting Men: A Study in Southern Brazil" Pathophysiology 32, no. 4: 64. https://doi.org/10.3390/pathophysiology32040064
APA StyleZanuzo, K., Nishiyama, M. F., Koehnlein, E. A., & Grassiolli, S. (2025). Hyperferritinemia Is Associated with Higher Adiposity, Metabolic Syndrome, and Hepatic Dysfunction, Mainly Affecting Men: A Study in Southern Brazil. Pathophysiology, 32(4), 64. https://doi.org/10.3390/pathophysiology32040064