Diffusion Tensor Tractography Shows White Matter Tract Changes in Breast Cancer Survivors with Balance Impairment
Abstract
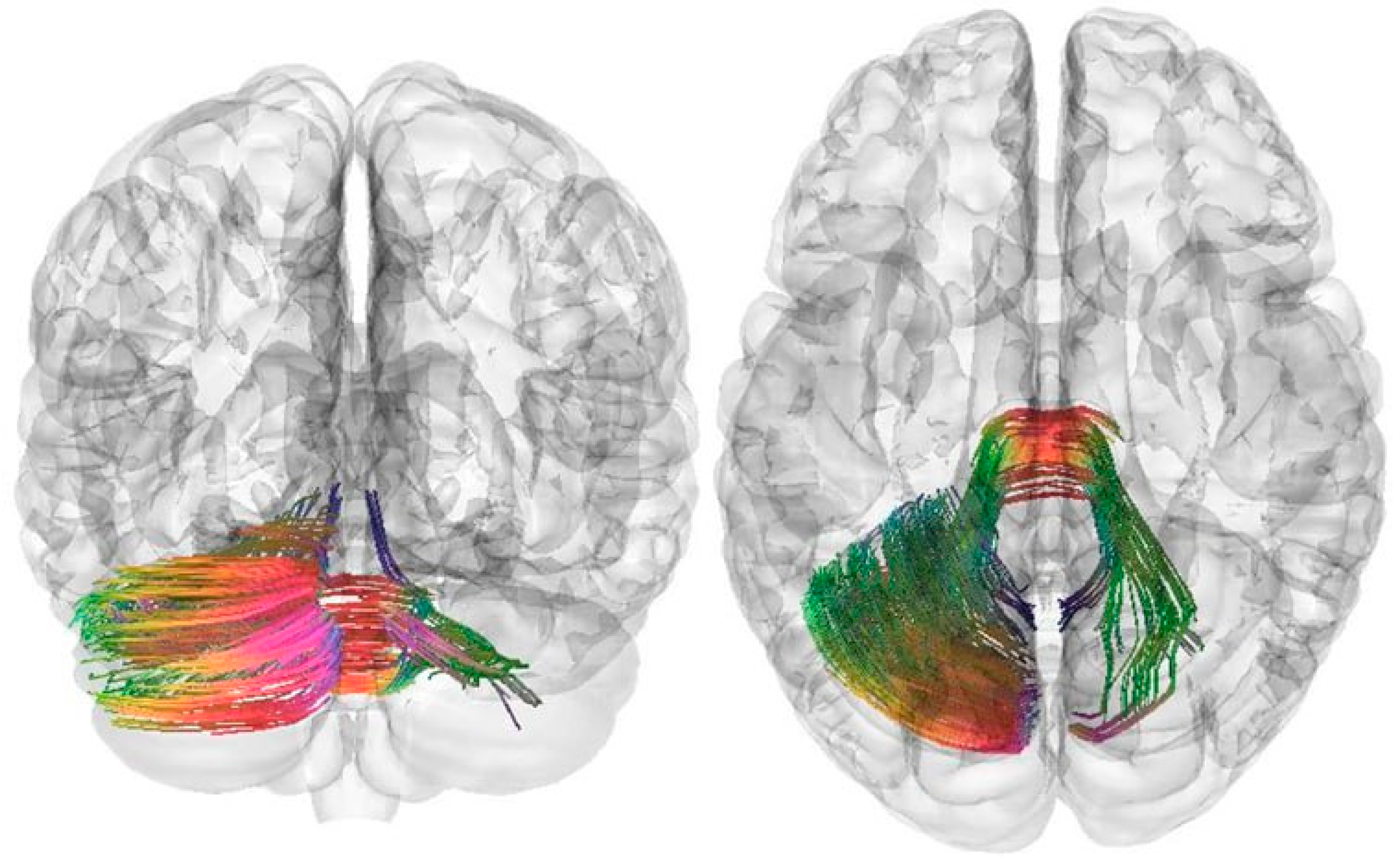
1. Introduction
2. Materials and Methods
2.1. Patients and Healthy Volunteers
2.2. MRI Study
2.3. Therapy of Balance Disorders
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CNS | Central Nervous System |
| DTI tractography | Diffusion Tensor Tractography |
| DWI | Diffusion-Weighted Imaging |
| MRI | Magnetic Resonance Imaging |
| QA | Quantitative Anisotropy |
| WM | White Matter |
References
- Santucci, C.; Carioli, G.; Bertuccio, P.; Malvezzi, M.; Pastorino, U.; Boffetta, P.; Negri, E.; Bosetti, C.; La Vecchia, C. Progress in Cancer Mortality, Incidence, and Survival: A Global Overview. Eur. J. Cancer Prev. 2020, 29, 367–381. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Bray, F.; Laversanne, M.; Sung, H.; Ferlay, J.; Siegel, R.L.; Soerjomataram, I.; Jemal, A. Global Cancer Statistics 2022: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2024, 74, 229–263. [Google Scholar] [CrossRef]
- Benitez Fuentes, J.D.; Morgan, E.; De Luna Aguilar, A.; Mafra, A.; Shah, R.; Giusti, F.; Vignat, J.; Znaor, A.; Musetti, C.; Yip, C.H.; et al. Global Stage Distribution of Breast Cancer at Diagnosis: A Systematic Review and Meta-Analysis. JAMA Oncol. 2024, 10, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Katsura, C.; Ogunmwonyi, I.; Kankam, H.K.N.; Saha, S. Breast Cancer: Presentation, Investigation and Management. Br. J. Hosp. Med. 2022, 83, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Shien, T.; Iwata, H. Adjuvant and Neoadjuvant Therapy for Breast Cancer. Jpn. J. Clin. Oncol. 2020, 50, 225–229. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.; Yadav, D.; Jain, M.; Singh, P.K.; Jin, J.-O. Immunotherapy for Breast Cancer Treatment: Current Evidence and Therapeutic Options. Endocr. Metab. Immune Disord. Drug Targets 2022, 22, 212–224. [Google Scholar] [CrossRef]
- Carreira, H.; Williams, R.; Dempsey, H.; Stanway, S.; Smeeth, L.; Bhaskaran, K. Quality of Life and Mental Health in Breast Cancer Survivors Compared with Non-Cancer Controls: A Study of Patient-Reported Outcomes in the United Kingdom. J. Cancer Surviv. 2021, 15, 564–575. [Google Scholar] [CrossRef]
- Salati, S.A.; Alsulaim, L.; Alharbi, M.H.; Alharbi, N.H.; Alsenaid, T.M.; Alaodah, S.A.; Alsuhaibani, A.S.; Albaqami, K.A. Postmastectomy Pain Syndrome: A Narrative Review. Cureus 2023, 15, e47384. [Google Scholar] [CrossRef]
- Ren, Y.; Kong, X.; Yang, Q.; Ouyang, L.; Liu, Q.; Dong, H.; Wang, Z.; Fang, Y.; Wang, J. Incidence, Risk Factors, Prevention and Treatment of Postmastectomy Pain Syndrome in Breast Cancer: A Multicenter Study. Int. J. Surg. 2022, 106, 106937. [Google Scholar] [CrossRef]
- Zhou, X.; Zhang, X.; Zhong, T.; Zhou, M.; Gao, L.; Chen, L. Prevalence and Associated Factors of Chemotherapy-Related Cognitive Impairment in Older Breast Cancer Survivors. J. Adv. Nurs. 2024, 80, 484–499. [Google Scholar] [CrossRef] [PubMed]
- Bennedsgaard, K.; Grosen, K.; Attal, N.; Bouhassira, D.; Crombez, G.; Jensen, T.S.; Bennett, D.L.; Ventzel, L.; Andersen, I.S.; Finnerup, N.B. Neuropathy and Pain after Breast Cancer Treatment: A Prospective Observational Study. Scand. J. Pain 2022, 23, 49–58. [Google Scholar] [CrossRef]
- Colvin, L.A. Chemotherapy-Induced Peripheral Neuropathy: Where Are We Now? Pain 2019, 160 (Suppl. S1), S1–S10. [Google Scholar] [CrossRef]
- Atkins, S.L.P.; Zimmer, A.S. Neurologic Complications of Breast Cancer. Cancer 2023, 129, 505–520. [Google Scholar] [CrossRef]
- Biparva, A.J.; Raoofi, S.; Rafiei, S.; Masoumi, M.; Doustmehraban, M.; Bagheribayati, F.; Vaziri Shahrebabak, E.S.; Mejareh, Z.N.; Khani, S.; Abdollahi, B.; et al. Global Depression in Breast Cancer Patients: Systematic Review and Meta-Analysis. PLoS ONE 2023, 18, e0287372. [Google Scholar] [CrossRef]
- Grusdat, N.P.; Stäuber, A.; Tolkmitt, M.; Schnabel, J.; Schubotz, B.; Wright, P.R.; Schulz, H. Routine Cancer Treatments and Their Impact on Physical Function, Symptoms of Cancer-Related Fatigue, Anxiety, and Depression. Support. Care Cancer 2022, 30, 3733–3744. [Google Scholar] [CrossRef]
- Fleming, B.; Edison, P.; Kenny, L. Cognitive Impairment after Cancer Treatment: Mechanisms, Clinical Characterization, and Management. BMJ 2023, 380, e071726. [Google Scholar] [CrossRef]
- Pospelova, M.; Krasnikova, V.; Fionik, O.; Alekseeva, T.; Samochernykh, K.; Ivanova, N.; Trofimov, N.; Vavilova, T.; Vasilieva, E.; Topuzova, M.; et al. Potential Molecular Biomarkers of Central Nervous System Damage in Breast Cancer Survivors. J. Clin. Med. 2022, 11, 1215. [Google Scholar] [CrossRef] [PubMed]
- Martín, B.R.; Rodríguez, E.J.F.; Galve, M.I.R.; Hernández, J.J.C. Study of Chemotherapy-Induced Cognitive Impairment in Women with Breast Cancer. Int. J. Environ. Res. Public Health 2020, 17, 8896. [Google Scholar] [CrossRef]
- Yi, J.C.; Syrjala, K.L. Anxiety and Depression in Cancer Survivors. Med. Clin. North Am. 2017, 101, 1099–1113. [Google Scholar] [CrossRef] [PubMed]
- Bock, K.; Peltzer, J.; Liu, W.; Colgrove, Y.; Smirnova, I.; Siengsukon, C. Sleep Quality and Lymphedema in Breast Cancer Survivors: A Mixed Method Analysis. J. Cancer Surviv. 2024, 19, 978–992. [Google Scholar] [CrossRef]
- Maass, S.W.M.C.; Roorda, C.; Berendsen, A.J.; Verhaak, P.F.M.; De Bock, G.H. The Prevalence of Long-Term Symptoms of Depression and Anxiety after Breast Cancer Treatment: A Systematic Review. Maturitas 2015, 82, 100–108. [Google Scholar] [CrossRef]
- Lange, M.; Joly, F.; Vardy, J.; Ahles, T.; Dubois, M.; Tron, L.; Winocur, G.; De Ruiter, M.B.; Castel, H. Cancer-Related Cognitive Impairment: An Update on State of the Art, Detection, and Management Strategies in Cancer Survivors. Ann. Oncol. 2019, 30, 1925–1940. [Google Scholar] [CrossRef]
- Rao, V.; Bhushan, R.; Kumari, P.; Cheruku, S.P.; Ravichandiran, V.; Kumar, N. Chemobrain: A Review on Mechanistic Insight, Targets and Treatments. Adv. Cancer Res. 2022, 155, 29–76. [Google Scholar] [CrossRef] [PubMed]
- Was, H.; Borkowska, A.; Bagues, A.; Tu, L.; Liu, J.Y.H.; Lu, Z.; Rudd, J.A.; Nurgali, K.; Abalo, R. Mechanisms of Chemotherapy-Induced Neurotoxicity. Front. Pharmacol. 2022, 13, 750507. [Google Scholar] [CrossRef]
- Nguyen, L.D.; Ehrlich, B.E. Cellular Mechanisms and Treatments for Chemobrain: Insight from Aging and Neurodegenerative Diseases. EMBO Mol. Med. 2020, 12, e12075. [Google Scholar] [CrossRef]
- Daniel, E.; Deng, F.; Patel, S.K.; Sedrak, M.S.; Kim, H.; Razavi, M.; Sun, C.L.; Root, J.C.; Ahles, T.A.; Dale, W.; et al. Brain White Matter Microstructural Changes in Chemotherapy-Treated Older Long-Term Breast Cancer Survivors. Cancer Med. 2023, 13, e6881. [Google Scholar] [CrossRef]
- Nikolaeva, A.; Pospelova, M.; Krasnikova, V.; Makhanova, A.; Tonyan, S.; Krasnopeev, Y.; Kayumova, E.; Vasilieva, E.; Efimtsev, A.; Levchuk, A.; et al. Elevated Levels of Serum Biomarkers Associated with Damage to the CNS Neurons and Endothelial Cells Are Linked with Changes in Brain Connectivity in Breast Cancer Patients with Vestibulo-Atactic Syndrome. Pathophysiology 2023, 30, 260–274. [Google Scholar] [CrossRef] [PubMed]
- Prayuenyong, P.; Kasbekar, A.V.; Hall, D.A.; Hennig, I.; Anand, A.; Baguley, D.M. Imbalance Associated with Cisplatin Chemotherapy in Adult Cancer Survivors: A Clinical Study. Otol. Neurotol. 2021, 42, E730–E734. [Google Scholar] [CrossRef] [PubMed]
- Fleihan, T.; Nader, M.E.; Dickman, J.D. Cisplatin Vestibulotoxicity: A Current Review. Front. Surg. 2024, 11, 1437468. [Google Scholar] [CrossRef]
- MRI Made Easy-Govind B Chavhan-Google Книги. Available online: https://books.google.ru/books?hl=ru&lr=&id=u3BWEwlhlT4C&oi=fnd&pg=PR1&ots=3QXqDZUiW_&sig=NsCTvnPHSscA3ZMnXeYNlSL5mu4&redir_esc=y#v=onepage&q&f=false (accessed on 26 July 2024).
- Nikolaeva, A.; Pospelova, M.; Krasnikova, V.; Makhanova, A.; Tonyan, S.; Efimtsev, A.; Levchuk, A.; Trufanov, G.; Voynov, M.; Sklyarenko, M.; et al. MRI Voxel Morphometry Shows Brain Volume Changes in Breast Cancer Survivors: Implications for Treatment. Pathophysiology 2025, 32, 11. [Google Scholar] [CrossRef]
- Tong, T.; Lu, H.; Zong, J.; Lv, Q.; Chu, X. Chemotherapy-Related Cognitive Impairment in Patients with Breast Cancer Based on MRS and DTI Analysis. Breast Cancer 2020, 27, 893–902. [Google Scholar] [CrossRef]
- Liang, M.Z.; Zhou, J.; Chen, P.; Song, Y.L.; Li, S.H.; Liang, Y.Y.; Hu, G.Y.; Hu, Q.; Sun, Z.; Yu, Y.L.; et al. A Longitudinal Correlational Study of Psychological Resilience, Depression Disorder, and Brain Functional-Structural Hybrid Connectome in Breast Cancer. Depress. Anxiety 2024, 2024, 9294268. [Google Scholar] [CrossRef] [PubMed]
- Reconstruction|DSI Studio Documentation. Available online: https://dsi-studio.labsolver.org/doc/gui_t2.html (accessed on 10 November 2025).
- Metin, M.Ö.; Gökçay, D. Diffusion Tensor Imaging Group Analysis Using Tract Profiling and Directional Statistics. Front. Neurosci. 2021, 15, 625473. [Google Scholar] [CrossRef] [PubMed]
- Carrozzi, A.; Gramegna, L.L.; Sighinolfi, G.; Zoli, M.; Mazzatenta, D.; Testa, C.; Lodi, R.; Tonon, C.; Manners, D.N. Methods of Diffusion MRI Tractography for Localization of the Anterior Optic Pathway: A Systematic Review of Validated Methods. Neuroimage Clin. 2023, 39, 103494. [Google Scholar] [CrossRef]
- Yeh, F.C. DSI Studio: An Integrated Tractography Platform and Fiber Data Hub for Accelerating Brain Research. Nat. Methods 2025, 22, 1617–1619. [Google Scholar] [CrossRef]
- Laurell, A.A.S.; Mak, E.; O’Brien, J.T. A Systematic Review of Diffusion Tensor Imaging and Tractography in Dementia with Lewy Bodies and Parkinson’s Disease Dementia. Neurosci. Biobehav. Rev. 2025, 169, 106007. [Google Scholar] [CrossRef] [PubMed]
- Piper, K.S.; Myhre, K.K.; Jensen, H.E.; Madsen, K.; Mikkelsen, M.K.; Lund, C. Dizziness and Impaired Walking Balance in Aging Patients during Chemotherapy. J. Geriatr. Oncol. 2024, 15, 102059. [Google Scholar] [CrossRef]
- Müller, J.; Ringhof, S.; Vollmer, M.; Jäger, L.B.; Stein, T.; Weiler, M.; Wiskemann, J. Out of Balance—Postural Control in Cancer Patients before and after Neurotoxic Chemotherapy. Gait Posture 2020, 77, 156–163. [Google Scholar] [CrossRef]
- Tofthagen, C.S.; Cheville, A.L.; Loprinzi, C.L. The Physical Consequences of Chemotherapy-Induced Peripheral Neuropathy. Curr. Oncol. Rep. 2020, 22, 50. [Google Scholar] [CrossRef]
- McCrary, J.M.; Goldstein, D.; Trinh, T.; Timmins, H.C.; Li, T.; Menant, J.; Friedlander, M.; Lewis, C.R.; Hertzberg, M.; O’Neill, S.; et al. Balance Deficits and Functional Disability in Cancer Survivors Exposed to Neurotoxic Cancer Treatments. J. Natl. Compr. Cancer Netw. 2019, 17, 949–955. [Google Scholar] [CrossRef] [PubMed]
- Mole, J.P.; Subramanian, L.; Bracht, T.; Morris, H.; Metzler-Baddeley, C.; Linden, D.E.J. Increased Fractional Anisotropy in the Motor Tracts of Parkinson’s Disease Suggests Compensatory Neuroplasticity or Selective Neurodegeneration. Eur. Radiol. 2016, 26, 3327. [Google Scholar] [CrossRef] [PubMed]
- Prayuenyong, P.; Taylor, J.A.; Pearson, S.E.; Gomez, R.; Patel, P.M.; Hall, D.A.; Kasbekar, A.V.; Baguley, D.M. Vestibulotoxicity Associated With Platinum-Based Chemotherapy in Survivors of Cancer: A Scoping Review. Front. Oncol. 2018, 8, 363. [Google Scholar] [CrossRef]
- Prayuenyong, P.; Kasbekar, A.V.; Hall, D.A.; Baguley, D.M. Audiovestibular Clinician Experiences and Opinions about Cisplatin Vestibulotoxicity. Eur. Arch. Otorhinolaryngol. 2020, 277, 3283–3293. [Google Scholar] [CrossRef]
- Prakash, N.; Hageman, N.; Hua, X.; Toga, A.W.; Perlman, S.L.; Salamon, N. Patterns of Fractional Anisotropy Changes in White Matter of Cerebellar Peduncles Distinguish Spinocerebellar Ataxia-1 from Multiple System Atrophy and Other Ataxia Syndromes. Neuroimage 2009, 47, T72–T81. [Google Scholar] [CrossRef] [PubMed]
| Main Group | ||
|---|---|---|
| Abs. | (%) | |
| Madden Mastectomy | 23 | 65.7 |
| Sectoral Mastectomy | 7 | 20.0 |
| Subcutaneous Mastectomy | 5 | 14.3 |
| Mastectomy with Immediate Breast Reconstruction | 12 | 34.3 |
| Side of Intervention: left | 13 | 37.1 |
| Side of Intervention: right | 22 | 62.9 |
| Total | 35 | 100 |
| DTI Parameters | Pulse Sequence |
|---|---|
| Repetition time/TR | 2800.0 ms |
| Echo time/TE | 79.00 ms |
| FoV | 220 mm |
| Slice thickness | 3.0 mm |
| Flip angle | 90° |
| Voxel size x (mm), y (mm) | 1.7 × 1.7 × 3.0 mm |
| Study time | 3:37 |
| Structure | Healthy Volunteers | Main Group | p-Value |
|---|---|---|---|
| Middle cerebellar peduncles | 0.191 ± 0.063 | 0.175 ± 0.053 | 0.046 |
| Cerebellar vermis | 0.125 ± 0.035 | 0.130 ± 0.043 | 0.510 |
| Right cerebellar hemisphere | 0.149 ± 0.045 | 0.127 ± 0.036 | 0.055 |
| Left cerebellar hemisphere | 0.172 ± 0.054 | 0.139 ± 0.039 | 0.024 |
| Right inferior cerebellar peduncle | 0.165 ± 0.056 | 0.171 ± 0.057 | 0.421 |
| Cranial nerve VIII | 0.189 ± 0.078 | 0.188 ± 0.055 | 0.396 |
| Right brainstem–reticular tract | 0.190 ± 0.091 | 0.195 ± 0.048 | 0.784 |
| Structure | Main Group | Healthy Volunteers | p-Value |
|---|---|---|---|
| Middle cerebellar peduncles | 0.257 ± 0.064 | 0.191 ± 0.063 | 0.016 |
| Cerebellar vermis | 0.164 ± 0.038 | 0.125 ± 0.035 | 0.054 |
| Right cerebellar hemisphere | 0.176 ± 0.051 | 0.149 ± 0.045 | 0.095 |
| Left cerebellar hemisphere | 0.169 ± 0.028 | 0.172 ± 0.054 | 0.948 |
| Right inferior cerebellar peduncle | 0.219 ± 0.056 | 0.165 ± 0.056 | 0.152 |
| Cranial nerve VIII | 0.274 ± 0.081 | 0.189 ± 0.078 | 0.013 |
| Right brainstem–reticular tract | 0.274 ± 0.026 | 0.190 ± 0.091 | 0.055 |
| Structure | Main Group, Point 1 | Main Group, Point 2 | p-Value |
|---|---|---|---|
| Middle cerebellar peduncles | 0.175 ± 0.053 | 0.257 ± 0.064 | 0.001 |
| Cerebellar vermis | 0.130 ± 0.043 | 0.164 ± 0.038 | 0.021 |
| Right cerebellar hemisphere | 0.127 ± 0.036 | 0.176 ± 0.051 | 0.001 |
| Left cerebellar hemisphere | 0.139 ± 0.039 | 0.169 ± 0.028 | 0.011 |
| Right inferior cerebellar peduncle | 0.171 ± 0.057 | 0.219 ± 0.056 | 0.009 |
| Cranial nerve VIII | 0.188 ± 0.055 | 0.274 ± 0.081 | 0.001 |
| Right brainstem–reticular tract | 0.195 ± 0.048 | 0.274 ± 0.026 | 0.095 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nikolaeva, A.; Pospelova, M.; Voynov, M.; Krasnikova, V.; Makhanova, A.; Tonyan, S.; Efimtsev, A.; Olga, F.; Levchuk, A.; Trufanov, G.; et al. Diffusion Tensor Tractography Shows White Matter Tract Changes in Breast Cancer Survivors with Balance Impairment. Pathophysiology 2025, 32, 63. https://doi.org/10.3390/pathophysiology32040063
Nikolaeva A, Pospelova M, Voynov M, Krasnikova V, Makhanova A, Tonyan S, Efimtsev A, Olga F, Levchuk A, Trufanov G, et al. Diffusion Tensor Tractography Shows White Matter Tract Changes in Breast Cancer Survivors with Balance Impairment. Pathophysiology. 2025; 32(4):63. https://doi.org/10.3390/pathophysiology32040063
Chicago/Turabian StyleNikolaeva, Alexandra, Maria Pospelova, Mark Voynov, Varvara Krasnikova, Albina Makhanova, Samvel Tonyan, Aleksandr Efimtsev, Fionik Olga, Anatoliy Levchuk, Gennadiy Trufanov, and et al. 2025. "Diffusion Tensor Tractography Shows White Matter Tract Changes in Breast Cancer Survivors with Balance Impairment" Pathophysiology 32, no. 4: 63. https://doi.org/10.3390/pathophysiology32040063
APA StyleNikolaeva, A., Pospelova, M., Voynov, M., Krasnikova, V., Makhanova, A., Tonyan, S., Efimtsev, A., Olga, F., Levchuk, A., Trufanov, G., Samochernykh, K., Alekseeva, T., Combs, S. E., & Shevtsov, M. (2025). Diffusion Tensor Tractography Shows White Matter Tract Changes in Breast Cancer Survivors with Balance Impairment. Pathophysiology, 32(4), 63. https://doi.org/10.3390/pathophysiology32040063










