Abstract
The pathophysiological mechanisms involved in chronic disorders such as complex regional pain syndrome, fibromyalgia, chronic fatigue syndrome, silicone breast implant–related symptoms, and post-COVID syndrome have not been clearly defined. The course of the pain in some of the syndromes, the absence of evident tissue damage, and the predominance of alterations in the autonomic nervous system are shared similarities between them. The production of autoantibodies following a trigger in the syndromes was previously described, for instance, trauma in complex regional pain syndrome, infectious agents in fibromyalgia, chronic fatigue syndrome, and post-COVID syndrome, and the immune stimulation by silicone in women with breast implants. In fact, the autoantibodies produced were shown to be directed against the autonomic nervous system receptors, leading to the amplification of the perception of pain alongside various clinical symptoms seen during the clinical course of the syndromes. Therefore, we viewed autoantibodies targeting the autonomic nervous system resulting in autonomic dysfunction as likely the most comprehensive explanation of the pathophysiology of the disorders mentioned. Based on this, we aimed to introduce a new concept uniting complex regional pain syndrome, fibromyalgia, chronic fatigue syndrome, silicone breast implant–related symptoms, and post-COVID syndrome, namely “autoimmune autonomic dysfunction syndromes”. Due to its etiological, pathophysiological, and clinical implications, the suggested term would be more precise in classifying the syndromes under one title. The new title would doubtlessly facilitate both laboratory and clinical studies aimed to improve diagnosis and make treatment options more directed and precise.
1. Introduction
The interplay between pain processing and the autonomic nervous system has long been described [1]. Defined as unpleasant sensation or emotional experience associated with tissue damage by the international association for the study of pain (IASP) [2], the definition of pain has received various criticisms over the last decades. Among others, the need of regular updating due to the advances in researching pain at both physical and psychological levels [3,4], and the addition of cognitive and social components of pain to the definition [5] have been suggested. While the definition is still controversial [6], the debate and research in the field of pain etiology are far more complicated, especially when it comes to chronic pain without apparent tissue damage or inflammation. For instance, the pathophysiology of chronic pain syndromes such as complex regional pain syndrome, chronic fatigue syndrome, and fibromyalgia remains unestablished. In this regard, Goebel addressed the mechanism of pain as “autoantibody pain”, secondary to the Fc-region binding of autoantibodies found in chronic pain syndromes and thus modifying the release of neurotransmitters resulting in various intensities of pain [7]. The theory of autoantibody pain was later strengthened by Cuhadar et al. [8] in an animal-based experiment. The study included skin incision in mice followed by the administration of pathological autoantibodies (IgG) from patients with complex regional pain syndrome. Mice treated with the IgG showed hypersensitivity to both cold and heat stimulation compared to mice treated with IgG from healthy individuals. Mice with skin incision alone without IgG administration manifested the same findings. Moreover, the symptomatology in women with silicone breast implants has shown various autoimmune features in terms of autoantibody production and clinical presentation. The basis for silicone breast implant illness (BII) was formerly reviewed [9]. A causal association between the systemic reaction to the implants as in autoimmune/autoinflammatory syndrome induced by adjuvants (ASIA), the production of autoantibodies, the resultant symptoms including autonomic dysautonomia and cognitive impairment, and eventually the disappearance of symptoms following the removal of the implants, have all been addressed. Recently, the proposed and yet undefined mechanisms behind the post-COVID or long COVID syndrome, characterized by nonspecific general complaints following clinical recovery from COVID-19, brought to our attention the similarities between post COVID and other syndromes such as chronic fatigue syndrome and fibromyalgia [10]. The suggestion that a combination of biological, psychological, and social factors are involved in post-COVID pathophysiology [11] strengthened our assumption of a common mechanism between the entities. In addition, the presence of functional autoantibodies against G-protein coupled receptors (GPCR) related to the autonomic nervous system in patients with persistent post-COVID symptoms, particularly neurological complaints [12], also supports our hypothesis that autoimmunity is a broad pathophysiological base of the syndromes.
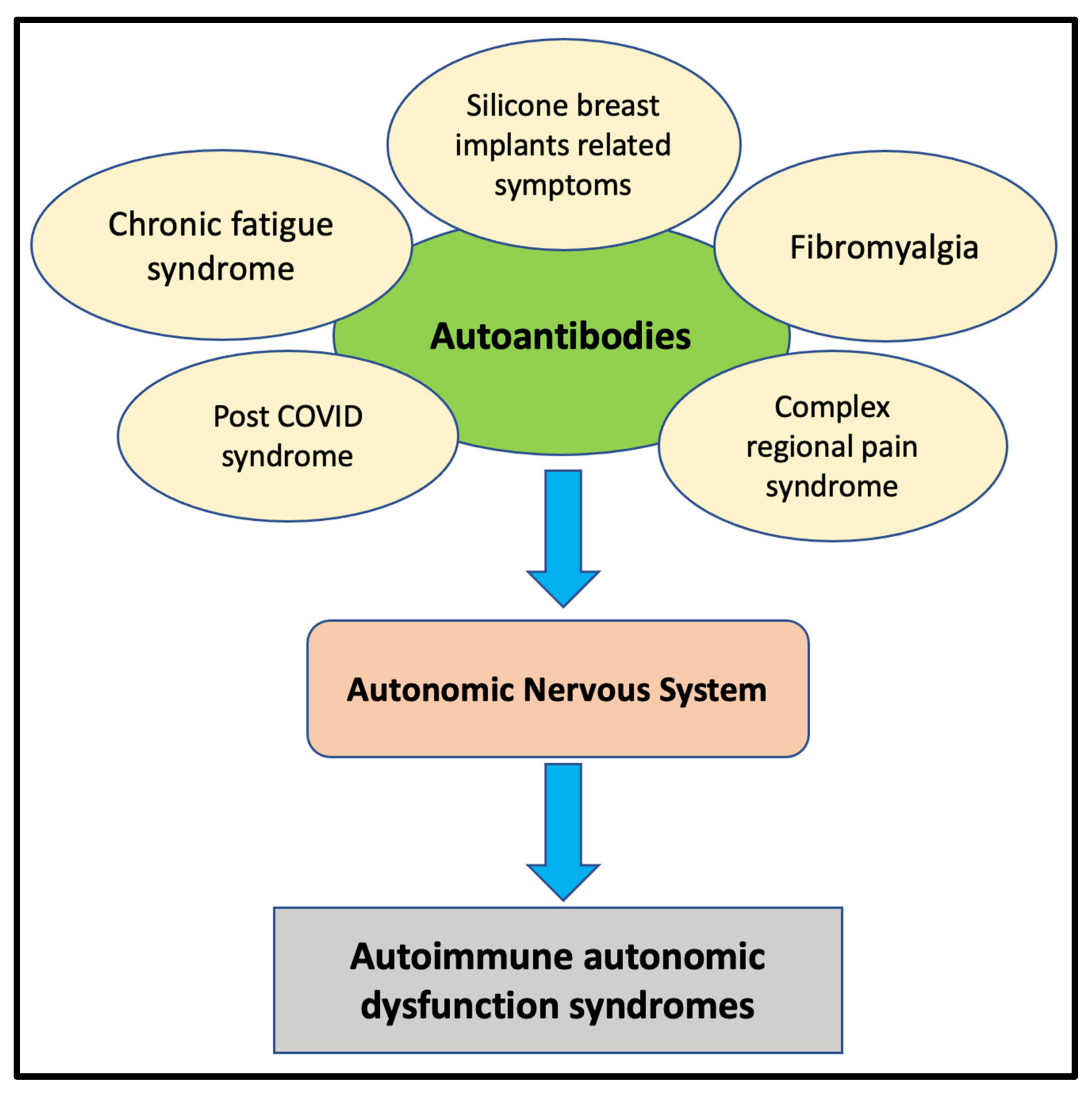
Correspondingly, based on previous studies addressing autoimmune aspects of the syndromes, we introduce in this review a new concept in regard to the pathophysiological mechanism of the aforementioned chronic syndromes, called “autoimmune autonomic dysfunction syndromes” (Figure 1). In our opinion, the concept is wider, taking into consideration the clinical aspects shared by complex regional pain syndrome, chronic fatigue syndrome, fibromyalgia, silicone breast implant–related symptoms, and post-COVID syndrome. Our proposal is grounded and strengthened in the current paper.
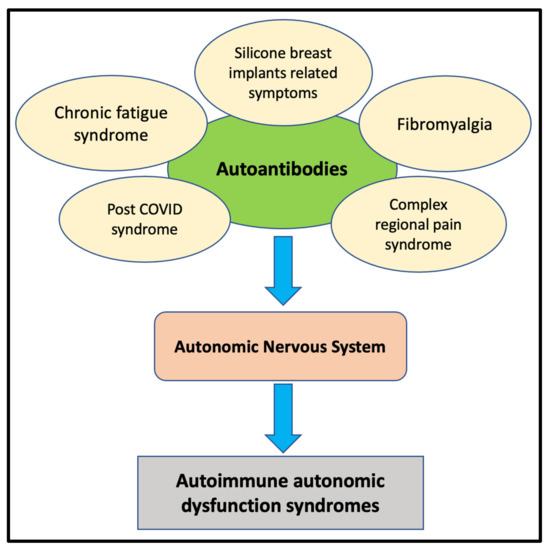
Figure 1.
The presence of autoantibodies directed against the autonomic nervous system receptors and the subsequent clinical presentations of the syndromes.
2. Complex Regional Pain Syndrome (CRPS)
CRPS is a chronic pain disorder of undefined etiology characterized by persistent pain confined to one region of the body, more commonly affecting the lower extremities [13]. In addition to pain, motor, sensory, and autonomic abnormalities are observed [14]. The majority of patients with CRPS have no peripheral nerve injury and are categorized as type I CRPS, whereas a small percentage of patients suffering peripheral nerve injury are referred to as type II CRPS [15].
Due to the unanswered questions regarding the etiology and pathophysiology of the disease, CRPS has been widely investigated in the last decades [16]. For instance, in a systematic review and meta-analysis, Parkitny and colleagues [17] showed a significant increase in serum inflammatory cytokines such as interleukin (IL)-8 and soluble tumor necrosis factor (TNF) in the acute phase of the disease. In turn, in chronic disease, TNF-alpha and bradykinins, among others, were elevated in blisters and cerebrospinal fluid (CSF). In addition, a decrease in substance P, E- and L-selectin was observed. The authors concluded that patients with CRPS show a proinflammatory state manifested by high inflammatory cytokines in the blood, blisters, and CSF, with several differences in the acute and chronic course of the disease. Similar findings supporting a proinflammatory condition were documented by Alexander et al. [18], who demonstrated significantly high CSF levels of IL-1beta, IL-6, and TNF-alpha in patients with CRPS compared to individuals with other pain syndromes as well as healthy subjects.
Furthermore, the role of the autonomic nervous system in the manifestation of CRPS has been widely documented yet not fully established. Birklein and colleagues [19] thoroughly investigated autonomic dysfunction in patients with CRPS in both the acute and chronic stages of the disease. Patients in the study were examined twice, shortly after diagnosis and 2 years afterward. Skin temperature was found warmer in the acute stage and colder in the chronic stage, whereas sweating was increased in both stages; all were statistically significant. More recently, alteration in the autonomic nervous system, particularly the sympathetic one, and its implication in the pathophysiology of CRPS were demonstrated [20]. In fact, the autonomic nervous system was viewed as a target of autoantibodies resulting in CRPS. Autoantibodies against receptors in the autonomic nervous system were found in 40% of patients with CRPS, suggesting an autoimmune nature of the disease [21]. Moreover, functional autoantibodies of IgG directed against beta-2 and muscarinic-2 receptors were detected in the serum of patients with CRPS [22]. The autoantibodies isolated showed pain-like properties. In another study comparing sera from patients with CRPS, rheumatoid arthritis, axial spondyloarthritis, psoriatic arthritis, and healthy individuals, the specificity and sensitivity of P29ING4 autoantibodies were found to be higher in patients with CRPS [23]. As a result, the authors suggested to use the immune complexes of P29ING4 in the diagnostic work-up in patients suspected to suffer from CRPS. Therefore, and unsurprisingly in our view, CRPS was suggested to be an autoimmune disease by Goebel et al. [24]. Due to the correlation between trauma and the appearance of CRPS, the authors proposed a term called “IRAM”, indicating an injury-triggered, regionally restricted, autoantibody-mediated autoimmune disorder with minimally destructive course. Moreover, when skin incisions in mice were treated with IgG isolated from patients with longstanding CRPS, the skin showed prolonged swelling and hyperalgesia in comparison to the control group. In addition, mice treated with IgG from patients with CRPS manifested cellular changes such as microglia and astrocyte activation at the dorsal horn as well as pain regions in the brain [25]. The findings were supported by a recent study by Sahbaie and colleagues [26]. Passive transfer of serum from mice with induced fracture containing autoantibodies against the autonomic nervous system receptors and the role in pain processing were interestingly presented. The authors concluded that targeting the autonomic nervous system might aid in the prevention and treatment of chronic pain following trauma such as CRPS.
3. Fibromyalgia
A generalized and chronic pain is a central component in the definition of fibromyalgia, in addition to fatigue as well as cognitive and sleep disorders [27]. The etiology of fibromyalgia is still unclear; however, the correlation between infectious agents and the development of fibromyalgia is well documented in the medical literature [28,29,30]. In recent years, the central nervous system (CNS) was shown to serve as a key factor in the pathogenesis of fibromyalgia. Abnormalities in pain processing and neurochemical imbalances in the CNS were found to result in central amplification of pain in patients with fibromyalgia [31]. Furthermore, studies on structural and functional brain magnetic resonance imaging (MRI) in patients with fibromyalgia demonstrated several abnormalities in grey matter volume, the pain-modulating system, and the pain matrix [32]. The abnormalities of the CNS, with an emphasis on pain hypersensitivity, were postulated to occur secondary to autoimmune mechanisms. Buskila et al. [33] addressed the association and possible correlation between fibromyalgia and autoimmunity. Patients with fibromyalgia were found to have a variety of autoantibodies, including antinuclear antibody (ANA) as well as antithyroid antibodies. In addition, high incidence of fibromyalgia in patients with autoimmune and rheumatic diseases was illustrated. Furthermore, in an animal-based study, Goebel and colleagues [34] injected mice with IgG isolated from patients with fibromyalgia. Mice treated with IgG from fibromyalgia patients showed an amplified response to mechanical and cold stimulation compared to IgG from healthy people and IgG-depleted fibromyalgia patients. According to the study, the IgG isolated were found to hyperstimulate nociceptive afferents in the dorsal root ganglia responsible for the hypersensitivity to pain stimuli seen in fibromyalgia. Accordingly, we agree with Martinez-Lavin, who addressed fibromyalgia as possibly an autoimmune disease, stressing the importance of further investigations and the need for scientific-based evidence [35].
4. Chronic Fatigue Syndrome
Fatigue is a subjective feeling of tiredness leading to the inability to conduct regular activities [36]. In turn, “chronic fatigue syndrome” (CFS), or myalgic encephalomyelitis (ME), is a clinical condition based on several criteria aimed to better diagnose, investigate, and treat patients suffering from fatigue [37,38]. The history of fatigue and its related nomenclature, starting from “neuromyasthenia”, through “myalgic encephalomyelitis”, and finally “chronic fatigue syndrome”, was described in previous papers [39,40]. While fatigue is the predominant complaint of the syndrome, a chronic and generalized pain is common and often underestimated in patients with CFS [41]. Additionally, cognitive impairment, sleep disorders, as well as orthostatic-related symptoms were documented [39]. Regarding the etiology of CFS, the syndrome cannot be viewed as a disease caused by one factor; rather, CFS is in fact a multifactorial disorder induced by a combination of physiological and psychological causes [42]. Infections and infectious agents were correlated and addressed as a trigger for CFS [43]. Unsurprisingly, since the beginning of the COVID-19 pandemic [44], fatigue has been linked to COVID-19 in diverse manners. For example, fatigue was the most common manifestation of the post-COVID period in patients recovering from SARS-CoV-2 infection [45,46].
Therefore, the correlation and similarities between CFS, fibromyalgia, and post-COVID syndrome are numerous and may share a common mechanism. The involvement and disturbances of the autonomic nervous system in CFS has been described. Freeman and colleagues [47] reported significant alterations in the sympathetic and parasympathetic nervous system functions in 23 patients with CFS compared to healthy controls. During tilt tests conducted in the patients, alterations were recorded in expiratory to inspiratory ratio, systolic and diastolic blood pressure, and heart rate. Moreover, autonomic dysfunction was strongly associated with fatigue in 40 patients with CFS compared to healthy age- and sex-matched controls [48]. In addition, a recent study that enrolled 1226 patients with CFS suffering from cervical muscle-related complaints documented an involvement of the autonomic nervous system [49]. The recovery of patients after treatment with physical therapy was found to be linked to the amelioration of the autonomic nervous system function. The autonomic dysfunction described was found to be related to autoimmune mechanisms. Autoimmune etiology in CFS, including autoantibodies against neurotransmitters and their role in severe metabolic disturbances seen in patients with CFS, were previously reported [50].
5. Silicone Breast Implant (SBI)–Related Symptoms
The correlation between silicone breast implants and autoimmunity in terms of the production of autoantibodies and the clinical presentation is not a new finding. High titers of antinuclear antibodies (ANA) were found in 10 out of 11 symptomatic women with SBIs [51]. The characteristics of isolated ANA resembled autoantibodies found in idiopathic forms of autoimmune diseases. Furthermore, a thorough analysis of 20 autoantibodies in 116 women with SBIs compared to 134 controls was conducted by Bar-Meir et al. [52]. The main symptoms in the group of women with SBIs were fatigue, myalgia, polyarthralgia, and impaired memory. A significantly increased incidence of autoantibodies against 15 of the 20 autoantigens studied was detected in the breast implant group. Around 20% of the breast implant group had four autoantibodies, and 8% had six autoantibodies. In addition, Zandman-Goddard and colleagues [53] reported an increased incidence of autoantibody production in women with SBIs, particularly of anti-SSB/La and anticollagen II types, in both symptomatic and asymptomatic women. However, the authors showed that polyclonality of the autoantibodies was more prominent in the symptomatic group. A correlation between the duration of implants and the appearance of the autoantibodies was also demonstrated.
In regard to the function of the autonomic nervous system in women with SBIs, alterations in the autonomic nervous system and its dysfunction were termed “autoimmune dysautonomia” by Halpert et al. [54]. The authors suggested the name “autoimmune dysautonomia” following the detection of low sera levels of autoantibodies against G protein-coupled receptors (GCPRs) of the autonomic nervous system in 93 women with SBIs. Women enrolled in the study demonstrated a constellation of symptoms, including fatigue, dry mouth and eyes, and cognitive impairment. The results were compared to the levels of autoantibodies in 36 age-matched healthy women without silicone implants, enrolled as controls. A chronic stimulation of the immune system by the silicone implants resulting in autonomic dysautonomia and the subsequent symptoms was concluded by the authors. Since low levels of autoantibodies were detected in women with SBIs compared to controls, another assumption was that these autoantibodies might play an immunomodulatory role in the pathogenesis of the disease rather than a pathogenic role. However, the assumption requires further investigations to be confirmed; the authors are currently working on this hypothesis.
6. Post-COVID Syndrome
Post-COVID and long COVID have been used interchangeably to address a variety of symptoms in the period of time following the clinical recovery from acute SARS-CoV-2 infection [55]. Among others, the symptoms of post-COVID include respiratory, cardiovascular, digestive, and neurological complaints [56,57]. Brain tissues were found to be highly permeable to SARS-CoV-2 in contrast to SARS-CoV, the virus responsible for the SARS outbreak in 2002, shedding light on the neurological presentation of COVID-19 and proposing a possible explanation for the neurological manifestations of post-COVID syndrome [58]. Similarly, immune activation and neuroinflammation as a result of SARS-CoV-2 infection were also reported [59].
In fact, the role the immune system plays in the manifestations and complications of COVID-19 induced by hyperstimulation, hyperferritinemia with its pathological consequences, and the cytokine storm [60,61] cannot be overemphasized. As a result, the strong relation between COVID-19 and autoimmunity in terms of pathophysiology, presentation, complications, and treatment has been described previously [62,63]. Accordingly, the involvement of autoimmune factors in the pathogenesis of post-COVID syndrome was, to a large extent, predicted [64]. For instance, Wang et al. [65] reported a significantly high level of autoantibodies in patients with COVID-19 in comparison to healthy subjects. When injected in mice, the autoantibodies were shown to disturb mice immune function and exacerbate the course of the disease. Moreover, by investigating a total of 31 individuals with post-COVID complaints, mainly neurological ones, Walkut et al. [12] detected autoantibodies against G-protein coupled receptors (GPCR) in all the patients enrolled. The autoantibodies isolated were directed against the autonomic nervous system and showed both positive and negative chronotropic effects, depending on the targeted receptors: beta2-adrenorecptors or muscarinic receptors. Interestingly, nociception-like opioid receptors were targeted by the isolated autoantibodies.
Papers and studies addressing autoimmune mechanisms in the syndromes investigated are summarized in Table 1.

Table 1.
Papers and studies addressing autoimmune mechanisms in the syndromes investigated.
7. Conclusions
We view autoimmunity, in the form of autoimmune autonomic dysfunction as a potential pathophysiological mechanism of complex regional pain syndrome, fibromyalgia, chronic fatigue syndrome, silicone breast implant–related symptoms, and post-COVID syndrome, as revolutionary. As the pathophysiology of the syndromes addressed is unclear, the presence of autoantibodies directed against the autonomic nervous system receptors and the subsequent clinical presentations offer a comprehensive pathophysiological explanation. The term “autoimmune autonomic dysfunction syndromes” could serve as a base for directed research, initially through detailed animal model–based experiments, followed by appropriately designed clinical studies. The results will doubtlessly improve the diagnosis of the syndromes and provide targeted treatment options.
Author Contributions
N.M.: writing—original draft preparation, review, and editing; Y.S.: conceptualization, supervision. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Garland, E.L. Pain processing in the human nervous system: A selective review of nociceptive and biobehavioral pathways. Prim. Care 2012, 39, 561–571. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Merskey, H.E. Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl. 1986, 3, S1–S226. [Google Scholar]
- Aydede, M. Does the IASP definition of pain need updating? Pain Rep. 2019, 4, e777. [Google Scholar] [CrossRef] [PubMed]
- Sluka, K.A.; George, S.Z. A New Definition of Pain: Update and Implications for Physical Therapist Practice and Rehabilitation Science. Phys. Ther. 2021, 101, pzab019. [Google Scholar] [CrossRef]
- Williams, A.C.C.; Craig, K.D. Updating the definition of pain. Pain 2016, 157, 2420–2423. [Google Scholar] [CrossRef]
- Alcock, M.M. Defining pain: Past, present, and future. Pain 2017, 158, 761–762. [Google Scholar] [CrossRef]
- Goebel, A. Autoantibody pain. Autoimmun Rev. 2016, 15, 552–557. [Google Scholar] [CrossRef]
- Cuhadar, U.; Gentry, C.; Vastani, N.; Sensi, S.; Bevan, S.; Goebel, A.; Andersson, D.A. Autoantibodies produce pain in complex regional pain syndrome by sensitizing nociceptors. Pain 2019, 160, 2855–2865. [Google Scholar] [CrossRef]
- Cohen Tervaert, J.W.; Mohazab, N.; Redmond, D.; van Eeden, C.; Osman, M. Breast implant illness: Scientific evidence of its existence. Expert Rev. Clin. Immunol. 2021, 18, 15–29. [Google Scholar] [CrossRef]
- Wong, T.L.; Weitzer, D.J. Long COVID and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)-A Systemic Review and Comparison of Clinical Presentation and Symptomatology. Medicina 2021, 57, 418. [Google Scholar] [CrossRef]
- Sykes, D.L.; Holdsworth, L.; Jawad, N.; Gunasekera, P.; Morice, A.H.; Crooks, M.G. Post-COVID-19 Symptom Burden: What is Long-COVID and How Should We Manage It? Lung 2021, 199, 113–119. [Google Scholar] [CrossRef]
- Wallukat, G.; Hohberger, B.; Wenzel, K.; Furst, J.; Schulze-Rothe, S.; Wallukat, A.; Hönicke, A.-S.; Müller, J. Functional autoantibodies against G-protein coupled receptors in patients with persistent Long-COVID-19 symptoms. J. Transl. Autoimmun. 2021, 4, 100100. [Google Scholar] [CrossRef]
- Bruehl, S. Complex regional pain syndrome. BMJ 2015, 351, h2730. [Google Scholar] [CrossRef] [Green Version]
- Ott, S.; Maihofner, C. Signs and Symptoms in 1043 Patients with Complex Regional Pain Syndrome. J. Pain 2018, 19, 599–611. [Google Scholar] [CrossRef]
- Harden, R.N.; Bruehl, S.; Stanton-Hicks, M.; Wilson, P.R. Proposed new diagnostic criteria for complex regional pain syndrome. Pain Med. 2007, 8, 326–331. [Google Scholar] [CrossRef]
- Birklein, F.; Schlereth, T. Complex regional pain syndrome-significant progress in understanding. Pain 2015, 156 (Suppl. S1), S94–S103. [Google Scholar] [CrossRef]
- Parkitny, L.; McAuley, J.H.; Di Pietro, F.; Stanton, T.R.; O’Connell, N.E.; Marinus, J.; van Hilten, J.J.; Moseley, G.L. Inflammation in complex regional pain syndrome: A systematic review and meta-analysis. Neurology 2013, 80, 106–117. [Google Scholar] [CrossRef] [Green Version]
- Alexander, G.M.; van Rijn, M.A.; van Hilten, J.J.; Perreault, M.J.; Schwartzman, R.J. Changes in cerebrospinal fluid levels of pro-inflammatory cytokines in CRPS. Pain 2005, 116, 213–219. [Google Scholar] [CrossRef]
- Birklein, F.; Riedl, B.; Claus, D.; Neundorfer, B. Pattern of autonomic dysfunction in time course of complex regional pain syndrome. Clin Auton Res. 1998, 8, 79–85. [Google Scholar] [CrossRef]
- Knudsen, L.F.; Terkelsen, A.J.; Drummond, P.D.; Birklein, F. Complex regional pain syndrome: A focus on the autonomic nervous system. Clin. Auton. Res. 2019, 29, 457–467. [Google Scholar] [CrossRef]
- Blaes, F.; Schmitz, K.; Tschernatsch, M.; Kaps, M.; Krasenbrink, I.; Hempelmann, G.; Brau, M.E. Autoimmune etiology of complex regional pain syndrome (M. Sudeck). Neurology 2004, 63, 1734–1736. [Google Scholar] [CrossRef]
- Kohr, D.; Singh, P.; Tschernatsch, M.; Kaps, M.; Pouokam, E.; Diener, M.; Kummer, W.; Birklein, F.; Vincent, A.; Goebel, A.; et al. Autoimmunity against the beta2 adrenergic receptor and muscarinic-2 receptor in complex regional pain syndrome. Pain 2011, 152, 2690–2700. [Google Scholar] [CrossRef]
- Baerlecken, N.T.; Gaulke, R.; Pursche, N.; Witte, T.; Karst, M.; Bernateck, M. Autoantibodies against P29ING4 are associated with complex regional pain syndrome. Immunol. Res. 2019, 67, 461–468. [Google Scholar] [CrossRef] [Green Version]
- Goebel, A.; Blaes, F. Complex regional pain syndrome, prototype of a novel kind of autoimmune disease. Autoimmun Rev. 2013, 12, 682–686. [Google Scholar] [CrossRef]
- Helyes, Z.; Tekus, V.; Szentes, N.; Pohoczky, K.; Botz, B.; Kiss, T.; Kemény, Á.; Környei, Z.; Tóth, K.; Lénárt, N.; et al. Transfer of complex regional pain syndrome to mice via human autoantibodies is mediated by interleukin-1-induced mechanisms. Proc. Natl. Acad. Sci. USA 2019, 116, 13067–13076. [Google Scholar] [CrossRef] [Green Version]
- Sahbaie, P.; Li, W.W.; Guo, T.Z.; Shi, X.Y.; Kingery, W.S.; Clark, J.D. Autonomic Regulation of Nociceptive and Immunologic Changes in a Mouse Model of Complex Regional Pain Syndrome. J. Pain 2021, 23, 472–486. [Google Scholar] [CrossRef]
- Clauw, D.J. Fibromyalgia: A clinical review. JAMA 2014, 311, 1547–1555. [Google Scholar] [CrossRef]
- Wormser, G.P.; Weitzner, E.; McKenna, D.; Nadelman, R.B.; Scavarda, C.; Farber, S.; Prakash, P.; Ash, J.; Nowakowski, J. Long-Term Assessment of Fibromyalgia in Patients with Culture-Confirmed Lyme Disease. Arthritis. Rheumatol. 2015, 67, 837–839. [Google Scholar] [CrossRef]
- Krumina, A.; Chapenko, S.; Kenina, V.; Mihailova, M.; Logina, I.; Rasa, S.; Gintere, S.; Viksna, L.; Svirskis, S.; Murovska, M. The role of HHV-6 and HHV-7 infections in the development of fibromyalgia. J. Neurovirol. 2019, 25, 194–207. [Google Scholar] [CrossRef] [Green Version]
- Pedersen, M.; Asprusten, T.T.; Godang, K.; Leegaard, T.M.; Osnes, L.T.; Skovlund, E.; Tjade, T.; Øie, M.G.; Wyller, V.B.B. Predictors of chronic fatigue in adolescents six months after acute Epstein-Barr virus infection: A prospective cohort study. Brain Behav. Immun. 2019, 75, 94–100. [Google Scholar] [CrossRef]
- Clauw, D.J.; Arnold, L.M.; McCarberg, B.H.; FibroCollaborative. The science of fibromyalgia. Mayo Clin. Proc. 2011, 86, 907–911. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cagnie, B.; Coppieters, I.; Denecker, S.; Six, J.; Danneels, L.; Meeus, M. Central sensitization in fibromyalgia? A systematic review on structural and functional brain MRI. Semin. Arthritis. Rheum. 2014, 44, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Buskila, D.; Sarzi-Puttini, P. Fibromyalgia and autoimmune diseases: The pain behind autoimmunity. Isr. Med. Assoc. J. 2008, 10, 77–78. [Google Scholar] [PubMed]
- Goebel, A.; Krock, E.; Gentry, C.; Israel, M.R.; Jurczak, A.; Urbina, C.M.; Sandor, K.; Vastani, N.; Maurer, M.; Cuhadar, U.; et al. Passive transfer of fibromyalgia symptoms from patients to mice. J. Clin. Invest. 2021, 13, 131. [Google Scholar] [CrossRef]
- Martinez-Lavin, M. Is fibromyalgia an autoimmune illness? Clin. Rheumatol. 2021, 40, 3865–3866. [Google Scholar] [CrossRef]
- Sharpe, M.; Wilks, D. Fatigue. BMJ 2002, 325, 480–483. [Google Scholar] [CrossRef]
- Fukuda, K.; Straus, S.E.; Hickie, I.; Sharpe, M.C.; Dobbins, J.G.; Komaroff, A. The chronic fatigue syndrome: A comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group. Ann. Intern. Med. 1994, 121, 953–959. [Google Scholar] [CrossRef]
- Brurberg, K.G.; Fonhus, M.S.; Larun, L.; Flottorp, S.; Malterud, K. Case definitions for chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME): A systematic review. BMJ Open 2014, 4, e003973. [Google Scholar] [CrossRef]
- Cortes Rivera, M.; Mastronardi, C.; Silva-Aldana, C.T.; Arcos-Burgos, M.; Lidbury, B.A. Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A Comprehensive Review. Diagnostics 2019, 9, 91. [Google Scholar] [CrossRef] [Green Version]
- Sharif, K.; Watad, A.; Bragazzi, N.L.; Lichtbroun, M.; Martini, M.; Perricone, C.; Amital, H.; Shoenfeld, Y. On chronic fatigue syndrome and nosological categories. Clin. Rheumatol. 2018, 37, 1161–1170. [Google Scholar] [CrossRef]
- Meeus, M.; Nijs, J.; Meirleir, K.D. Chronic musculoskeletal pain in patients with the chronic fatigue syndrome: A systematic review. Eur. J. Pain 2007, 11, 377–386. [Google Scholar] [CrossRef]
- Afari, N.; Buchwald, D. Chronic fatigue syndrome: A review. Am. J. Psychiatry 2003, 160, 221–236. [Google Scholar] [CrossRef]
- Rasa, S.; Nora-Krukle, Z.; Henning, N.; Eliassen, E.; Shikova, E.; Harrer, T.; Scheibenbogen, C.; Murovska, M.; Prusty, B.K. Chronic viral infections in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). J. Transl. Med. 2018, 16, 268. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 1 April 2022).
- Kamal, M.; Abo Omirah, M.; Hussein, A.; Saeed, H. Assessment and characterisation of post-COVID-19 manifestations. Int. J. Clin. Pract. 2020, 75, e13746. [Google Scholar] [CrossRef]
- Xiong, Q.; Xu, M.; Li, J.; Liu, Y.; Zhang, J.; Xu, Y.; Dong, W. Clinical sequelae of COVID-19 survivors in Wuhan, China: A single-centre longitudinal study. Clin. Microbiol. Infect. 2021, 27, 89–95. [Google Scholar] [CrossRef]
- Freeman, R.; Komaroff, A.L. Does the chronic fatigue syndrome involve the autonomic nervous system? Am. J. Med. 1997, 102, 357–364. [Google Scholar] [CrossRef]
- Newton, J.L.; Okonkwo, O.; Sutcliffe, K.; Seth, A.; Shin, J.; Jones, D.E. Symptoms of autonomic dysfunction in chronic fatigue syndrome. QJM 2007, 100, 519–526. [Google Scholar] [CrossRef] [Green Version]
- Matsui, T.; Hara, K.; Iwata, M.; Hojo, S.; Shitara, N.; Endo, Y.; Fukuoka, H.; Matsui, M.; Kawaguchi, H. Possible involvement of the autonomic nervous system in cervical muscles of patients with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). BMC Musculoskelet. Disord. 2021, 22, 419. [Google Scholar] [CrossRef]
- Sotzny, F.; Blanco, J.; Capelli, E.; Castro-Marrero, J.; Steiner, S.; Murovska, M.; Scheibenbogen, C. Myalgic Encephalomyelitis/Chronic Fatigue Syndrome—Evidence for an autoimmune disease. Autoimmun. Rev. 2018, 17, 601–609. [Google Scholar] [CrossRef]
- Press, R.I.; Peebles, C.L.; Kumagai, Y.; Ochs, R.L.; Tan, E.M. Antinuclear autoantibodies in women with silicone breast implants. Lancet 1992, 340, 1304–1307. [Google Scholar] [CrossRef]
- Bar-Meir, E.; Teuber, S.S.; Lin, H.C.; Alosacie, I.; Goddard, G.; Terybery, J.; Barka, N.; Shen, B.; Peter, J.; Blank, M.; et al. Multiple autoantibodies in patients with silicone breast implants. J. Autoimmun. 1995, 8, 267–277. [Google Scholar] [CrossRef]
- Zandman-Goddard, G.; Blank, M.; Ehrenfeld, M.; Gilburd, B.; Peter, J.; Shoenfeld, Y. A comparison of autoantibody production in asymptomatic and symptomatic women with silicone breast implants. J. Rheumatol. 1999, 26, 73–77. [Google Scholar]
- Halpert, G.; Watad, A.; Tsur, A.M.; Dotan, A.; Quiros-Lim, H.E.; Heidecke, H.; Gilburd, B.; Haik, J.; Levy, Y.; Blank, M.; et al. Autoimmune dysautonomia in women with silicone breast implants. J. Autoimmun. 2021, 120, 102631. [Google Scholar] [CrossRef]
- Anaya, J.M.; Rojas, M.; Salinas, M.L.; Rodriguez, Y.; Roa, G.; Lozano, M.; Rodríguez-Jiménez, M.; Montoya, N.; Zapata, E.; Monsalve, D.M.; et al. Post-COVID syndrome. A case series and comprehensive review. Autoimmun. Rev. 2021, 20, 102947. [Google Scholar] [CrossRef]
- Salamanna, F.; Veronesi, F.; Martini, L.; Landini, M.P.; Fini, M. Post-COVID-19 Syndrome: The Persistent Symptoms at the Post-viral Stage of the Disease. A Systematic Review of the Current Data. Front. Med. 2021, 8, 653516. [Google Scholar] [CrossRef]
- Oronsky, B.; Larson, C.; Hammond, T.C.; Oronsky, A.; Kesari, S.; Lybeck, M.; Reid, T.R. A Review of Persistent Post-COVID Syndrome (PPCS). Clin. Rev. Allergy Immunol. 2021, 1–9. [Google Scholar] [CrossRef]
- Zhang, B.Z.; Chu, H.; Han, S.; Shuai, H.; Deng, J.; Hu, Y.F.; Gong, H.-R.; Lee, A.C.-Y.; Zou, Z.; Yau, T.; et al. SARS-CoV-2 infects human neural progenitor cells and brain organoids. Cell Res. 2020, 30, 928–931. [Google Scholar] [CrossRef]
- Kempuraj, D.; Selvakumar, G.P.; Ahmed, M.E.; Raikwar, S.P.; Thangavel, R.; Khan, A.; Zaheer, S.A.; Iyer, S.S.; Burton, C.; James, D.; et al. COVID-19, Mast Cells, Cytokine Storm, Psychological Stress, and Neuroinflammation. Neuroscientist 2020, 26, 402–414. [Google Scholar] [CrossRef]
- Mahroum, N.; Alghory, A.; Kiyak, Z.; Alwani, A.; Seida, R.; Alrais, M.; Shoenfeld, Y. Ferritin—From iron, through inflammation and autoimmunity, to COVID-19. J. Autoimmun. 2021, 126, 102778. [Google Scholar] [CrossRef]
- Colafrancesco, S.; Alessandri, C.; Conti, F.; Priori, R. COVID-19 gone bad: A new character in the spectrum of the hyperferritinemic syndrome? Autoimmun. Rev. 2020, 19, 102573. [Google Scholar] [CrossRef]
- Ehrenfeld, M.; Tincani, A.; Andreoli, L.; Cattalini, M.; Greenbaum, A.; Kanduc, D.; Alijotas-Reig, J.; Zinserling, V.; Semenova, N.; Amital, H.; et al. Covid-19 and autoimmunity. Autoimmun. Rev. 2020, 19, 102597. [Google Scholar] [CrossRef] [PubMed]
- Lyons-Weiler, J. Pathogenic priming likely contributes to serious and critical illness and mortality in COVID-19 via autoimmunity. J. Transl. Autoimmun. 2020, 3, 100051. [Google Scholar] [CrossRef] [PubMed]
- Damoiseaux, J.; Dotan, A.; Fritzler, M.J.; Bogdanos, D.P.; Meroni, P.L.; Roggenbuck, D.; Goldman, M.; Landegren, N.; Bastard, P.; Shoenfield, Y.; et al. Autoantibodies and SARS-CoV2 infection: The spectrum from association to clinical implication: Report of the 15th Dresden Symposium on Autoantibodies. Autoimmun. Rev. 2021, 21, 103012. [Google Scholar] [CrossRef] [PubMed]
- Wang, E.Y.; Mao, T.; Klein, J.; Dai, Y.; Huck, J.D.; Jaycox, J.R.; Liu, F.; Zhou, T.; Israelow, B.; Wong, P.; et al. Diverse functional autoantibodies in patients with COVID-19. Nature 2021, 595, 283–288. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).