Root Dilaceration and Dentigerous Cyst—A Cause–Effect Relationship?—“Case-Series Study”
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| DL | root dilaceration |
| DC | dentigerous cyst |
| 3D | three dimensional |
| CBCT | cone-beam computed tomography |
| DAP | dental anomaly pattern |
| ADA | associated dental anomaly |
References
- Tomes, J. A Course of Lectures on Dental Physiology and Surgery. Am. J. Dent. Sci. 1848, 8, 313–350. [Google Scholar] [PubMed]
- BSI 4492; Glossary of Dental Terms. British Standards Institute: London, UK, 1983.
- Shafer, W.G.; Hine, M.K.; Levy, B.M. A Textbook of OralPathology; WB Saunders Co.: Philadelphia, PA, USA, 1983; pp. 308–311. [Google Scholar]
- Tiecke, R.W.; Stuteville, O.H.; Calandra, J.C. Pathologic Physiology of Oral Disease; CV Mosby Co.: St Louis, MI, USA, 1959. [Google Scholar]
- Hamasha, A.A.; Al-Khateeb, T.; Darwazeh, A. Prevalence of dilaceration in Jordanian adults. Int. Endod. J. 2002, 35, 910–912. [Google Scholar] [CrossRef] [PubMed]
- Chohayeb, A.A. Dilaceration of permanent upper lateral incisors: Frequency, direction, and endodontic treatment implications. Oral. Surg. Oral. Med. Oral. Pathol. 1983, 55, 519–520. [Google Scholar] [CrossRef]
- Andreasen, J.O.; Sundström, B.; Ravn, J.J. The effect of traumatic injuries to primary teeth on their permanent successors. I. A clinical and histologic study of 117 injured permanent teeth. Scand. J. Dent. Res. 1971, 79, 219–283. [Google Scholar] [CrossRef] [PubMed]
- Andreasen, J.O.; Flores, M.T. Injuries to Developing Teeth. In Textbook and Color Atlas of Traumatic Injuries to the Teeth; Andreasen, J.O., Andreasen, F.M., Andreasen, L., Eds.; Blackwell Munksgaard: Oxford, UK, 2007; pp. 542–576. [Google Scholar]
- Becker, A. Maxillary central incisors. In The Orthodontic Treatment of Impacted Teeth; Becker, A., Ed.; Wiley-Blackwell: Hoboken, NJ, USA, 2012; pp. 70–109. [Google Scholar]
- Bimstein, E. Root dilaceration and stunting in two unerupted primary incisors. ASDC J. Dent. Child. 1978, 45, 223–225. [Google Scholar] [PubMed]
- Neville, B.W.; Damm, D.D.; Allen, C.M.; Bouquot, J.E. Oral and Maxillofacial Pathology, 2nd ed.; WB Saunders: Philadelphia, PA, USA, 2002; pp. 86–88. [Google Scholar]
- Yeung, K.H.; Cheung, R.C.; Tsang, M.M. Compound odontoma associated with an unerupted and dilacerated maxillary primary central incisor in a young patient. Int. J. Paediatr. Dent. 2003, 13, 208–212. [Google Scholar] [CrossRef]
- Rengaswamy, V. Bilateral dilaceration of maxillary central incisors. Oral. Surg. Oral. Med. Oral. Pathol. 1979, 47, 200. [Google Scholar] [CrossRef]
- Edmondson, H.D.; Crabb, J.J. Dilaceration of both upper central incisor teeth: A case report. J. Dent. 1975, 3, 223–224. [Google Scholar] [CrossRef]
- Lin, L.; Dowden, W.E.; Langeland, K. Bilateral dilaceration. J. Endod. 1982, 8, 85–87. [Google Scholar] [CrossRef]
- Malcić, A.; Jukić, S.; Brzović, V.; Miletić, I.; Pelivan, I.; Anić, I. Prevalence of root dilaceration in adult dental patients in Croatia. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2006, 102, 104–109. [Google Scholar] [CrossRef]
- Seow, W.K.; Perham, S.; Young, W.G.; Daley, T. Dilaceration of a primary maxillary incisor associated with neonatal laryngoscopy. Pediatr. Dent. 1990, 12, 321–324. [Google Scholar] [PubMed]
- Kilpatrick, N.M.; Hardman, P.J.; Welbury, R.R. Dilaceration of a primary tooth. Int. J. Paediatr. Dent. 1991, 1, 151–153. [Google Scholar] [CrossRef] [PubMed]
- Kearns, H.P. Dilacerated incisors and congenitally displaced incisors: Three case reports. Dent. Update 1998, 25, 339–342. [Google Scholar]
- Maragakis, M.G. Crown dilaceration of permanent incisors following trauma to their primary predecessors. J. Clin. Pediatr. Dent. 1995, 20, 49–52. [Google Scholar] [PubMed]
- Chadwick, S.M.; Millett, D. Dilaceration of a permanent mandibular incisor. A case report. Br. J. Orthod. 1995, 22, 279–281. [Google Scholar] [CrossRef] [PubMed]
- Feldman, B.S. Tooth with a 'tail'. A case report of a dilacerated mandibular incisor. Br. J. Orthod. 1984, 11, 42–43. [Google Scholar] [CrossRef] [PubMed]
- Matsuoka, T.; Sobue, S.; Ooshima, T. Crown dilaceration of a first premolar caused by extraction of its deciduous predecessor: A case report. Endod. Dent. Traumatol. 2000, 16, 91–94. [Google Scholar] [CrossRef]
- Asokan, S.; Rayen, R.; Muthu, M.S.; Sivakumar, N. Crown dilaceration of maxillary right permanent central Incisor—A case report. J. Indian Soc. Pedod. Prev. Dent. 2004, 22, 197–200. [Google Scholar]
- Agnihotri, A.; Marwah, N.; Dutta, S. Dilacerated unerupted central incisor: A case report. J. Indian Soc. Pedod. Prev. Dent. 2006, 24, 152–154. [Google Scholar] [CrossRef]
- Prabhakar, A.R.; Reddy, V.V.; Bassappa, N. Duplication and Dilaceration of a Crown with Hypercementosis of the Root Following Trauma: A Case Report. Quintessence Int. 1998, 29, 655–657. [Google Scholar]
- Meadow, D.M.; Needleman, H.L. Dilaceration of the mandibular permanent incisor teeth: Two case reports. Pediatr. Dent. 1981, 3, 276–278. [Google Scholar] [PubMed]
- Yen, H.T.; Diau, M.H.; Tsai, J.W.; Roan, R.T. Dilaceration of a central incisor with iatrogenic root perforation—A case report. Gaoxiong Yi Xue Ke Xue Za Zhi 1991, 7, 386–390. [Google Scholar] [PubMed]
- McNamara, T.G.; McNamara, C.M. Dilaceration of a mandibular incisor: Case report. Singap. Dent. J. 2000, 23, 29–31. [Google Scholar]
- Maia, R.L.; Vieira, A.P. Auto-transplantation of central incisor with root dilaceration. Technical note. Int. J. Oral. Maxillofac. Surg. 2005, 34, 89–91. [Google Scholar] [CrossRef] [PubMed]
- Glenn, F.B.; Stanley, H.R., Jr. Dilaceration of a mandibular permanent incisor. Report of a case. Oral. Surg. Oral. Med. Oral. Pathol. 1960, 13, 1249–1252. [Google Scholar] [CrossRef]
- Ngeow, W.C. An unusual dilacerated root of a second maxillary molar. J. Ir. Dent. Assoc. 1996, 42, 51–52. [Google Scholar]
- Edler, R. Dilaceration of upper central and lateral incisors. A case report. Br. Dent. J. 1973, 135, 331–332. [Google Scholar] [CrossRef]
- Lowe, P.L. Dilaceration caused by direct penetrating injury. Br. Dent. J. 1985, 159, 373–374. [Google Scholar] [CrossRef]
- Thongudomporn, U.; Freer, T.J. Prevalence of dental anomalies in orthodontic patients. Aust. Dent. J. 1998, 43, 395–398. [Google Scholar]
- Eversole, L.R. Clinical Outline of Oral Pathology: Diagnosis and Treatment, 3rd ed.; BC Decker Inc.: Hamilton, ON, Canada, 2002; p. 350. [Google Scholar]
- Jafarzadeh, H.; Abbott, P.V. Dilaceration: Review of an endodontic challenge. J. Endod. 2007, 33, 1025–1030. [Google Scholar] [CrossRef]
- Smith, D.M.; Winter, G.B. Root dilaceration of maxillary incisors. Br. Dent. J. 1981, 150, 125–127. [Google Scholar] [CrossRef] [PubMed]
- McNamara, T.; Woolfe, S.N.; McNamara, C.M. Orthodontic management of a dilacerated maxillary central incisor with an unusual sequela. J. Clin. Orthod. 1998, 32, 293–297. [Google Scholar] [PubMed]
- Walia, P.S.; Rohilla, A.K.; Choudhary, S.; Kaur, R. Review of Dilaceration of Maxillary Central Incisor: A Mutidisciplinary Challenge. Int. J. Clin. Pediatr. Dent. 2016, 9, 90–98. [Google Scholar] [CrossRef] [PubMed]
- Von Gool, A.V. Injury to the permanent tooth germ after trauma to the deciduous predecessor. Oral. Surg. Oral. Med. Oral. Pathol. 1973, 35, 2–12. [Google Scholar] [CrossRef]
- Bassetti, M.A.; Kuttenberger, J.; Novak, J.; Bassetti, R.G. Die follikuläre Zyste: Zwei unterschiedliche Behandlungsmöglichkeiten, präsentiert anhand zweier Fallbeispiele [The dentigerous cyst: Two different treatment options illustrated by two cases]. Swiss. Dent. J. 2019, 129, 193–203. (In German) [Google Scholar] [PubMed]
- Hu, N.N.; Li, Y.Y.; Wang, J.W.; Hou, Z.J.; Yang, X.C. A case report of multiple dentigerous cyst of mandible and review of literature. Shanghai Kou Qiang Yi Xue 2019, 28, 110–112. (In Chinese) [Google Scholar] [PubMed]
- Dhupar, A.; Yadav, S.; Dhupar, V.; Mittal, H.C.; Malik, S.; Rana, P. Bi-maxillary dentigerous cyst in a non-syndromic child—Review of literature with a case presentation. J. Stomatol. Oral. Maxillofac. Surg. 2017, 118, 45–48. [Google Scholar] [CrossRef]
- Daley, T.D.; Wysocki, G.P.; Pringle, G.A. Relative incidence of odontogenic tumors and oral and jaw cysts in a Canadian population. Oral. Surg. Oral. Med. Oral. Pathol. 1994, 77, 276–280. [Google Scholar] [CrossRef]
- Ziccardi, V.B.; Eggleston, T.I.; Schneider, R.E. Using fenestration technique to treat a large dentigerous cyst. J. Am. Dent. Assoc. 1997, 128, 201–205. [Google Scholar] [CrossRef]
- Shetty, R.M.; Dixit, U. Dentigerous Cyst of Inflammatory Origin. Int. J. Clin. Pediatr. Dent. 2010, 3, 195–198. [Google Scholar] [CrossRef]
- Grewal, H.K.; Batra, R. Non Syndromic Bilateral Dentigerous Cysts: A case report. Int. J. Dent. Clin. 2010, 2, 49–51. [Google Scholar]
- Terauchi, M.; Akiya, S.; Kumagai, J.; Ohyama, Y.; Yamaguchi, S. An analysis of dentigerous cysts developed around a mandibular third molar by panoramic radiographs. Dent. J. 2019, 7, 13. [Google Scholar] [CrossRef]
- Zhang, L.L.; Yang, R.; Zhang, L.; Li, W.; MacDonald-Jankowski, D.; Poh, C.F. Dentigerous cyst: A retrospective clinicopathological analysis of 2082 dentigerous cysts in British Columbia, Canada. Int. J. Oral. Maxillofac. Surg. 2010, 39, 878–882. [Google Scholar] [CrossRef] [PubMed]
- Martinelli-Kläy, C.P.; Martinelli, C.R.; Martinelli, C.; Macedo, H.R.; Lombardi, T. Unusual Imaging Features of Dentigerous Cyst: A Case Report. Dent. J. 2019, 7, 76. [Google Scholar] [CrossRef] [PubMed]
- Hyomoto, M.; Kawakami, M.; Inoue, M.; Kirita, T. Clinical conditions for eruption of maxillary canines and mandibular premolars associated with dentigerous cysts. Am. J. Orthod. Dentofacial. Orthop. 2003, 124, 515–520. [Google Scholar] [CrossRef]
- Ghandour, L.; Bahmad, H.F.; Bou-Assi, S. Conservative Treatment of Dentigerous Cyst by Marsupialization in a Young Female Patient: A Case Report and Review of the Literature. Case Rep. Dent. 2018, 2018, 7621363. [Google Scholar] [CrossRef]
- Bansal, S.; Kaur, H.; Bansal, R.N.; Goyal, P. An idiosyncratic post-traumatic tetrad: Compound odontome, dentigerous cyst, impaction, and double-dilaceration. Quintessence Int. 2014, 45, 885–889. [Google Scholar] [CrossRef]
- Tanaka, O.M.; Meira, T.M.; Batista, R.A.C.; Willems, G.; Baggio, G.L.; Couto, S.P.H. Marsupialization of a Large Radicular Cyst with Extensive Maxillary Tooth Displacement: Eight-Year Follow-Up. J. Dent. Child. 2019, 86, 64–68. [Google Scholar]
- Osório, L.B.; Ferrazzo, V.A.; Serpa, G.; Ferrazzo, K.L. Apicotomy as treatment for failure of orthodontic traction. Case Rep. Dent. 2013, 2013, 168232. [Google Scholar] [CrossRef]
- Aoki, N.; Ise, K.; Inoue, A.; Kosugi, Y.; Koyama, C.; Iida, M.; Baba, J.; Iwai, T.; Mitsudo, K. Multidisciplinary approach for treatment of a dentigerous cyst—Marsupialization, orthodontic treatment, and implant placement: A case report. J. Med. Case Rep. 2018, 12, 305. [Google Scholar] [CrossRef]
- Cao, D.; Shao, B.; Izadikhah, I.; Xie, L.; Wu, B.; Li, H.; Yan, B. Root dilaceration in maxillary impacted canines and adjacent teeth: A retrospective analysis of the difference between buccal and palatal impaction. Am. J. Orthod. Dentofacial. Orthop. 2021, 159, 167–174. [Google Scholar] [CrossRef] [PubMed]
- Gorlin, R.J.; Goldman, H.M. Thoma’s Oral Pathology, 6th ed.; Mosby: St Louis, MI, USA, 1970; pp. 104–106. [Google Scholar]
- Kalra, N.; Sushma, K.; Mahapatra, G.K. Changes in developing succedaneous teeth as a consequence of infected deciduous molars. J. Indian Soc. Pedod. Prev. Dent. 2000, 18, 90–94. [Google Scholar]
- Stewart, D.J. Dilacerate unerupted maxillary central incisors. Br. Dent. J. 1978, 145, 229–233. [Google Scholar] [CrossRef] [PubMed]
- Walton, R.E.; Torabinejad, M. Principles and Practice of Endodontics, 3rd ed.; WB Saunders: Philadelphia, PA, USA, 2002; pp. 176–179. [Google Scholar]
- Atwan, S.M.; Turner, D.; Khalid, A. Early intervention to remove mesiodens and avoid orthodontic therapy. Gen. Dent. 2000, 48, 166–169. [Google Scholar] [PubMed]
- Dayi, E.; Gürbüz, G.; Bilge, O.M.; Ciftcioğlu, M.A. Adenomatoid odontogenic tumour (adenoameloblastoma). Case report and review of the literature. Aust. Dent. J. 1997, 42, 315–318. [Google Scholar] [CrossRef] [PubMed]
- Angelos, G.M.; Smith, D.R.; Jorgenson, R.; Sweeney, E.A. Oral complications associated with neonatal oral tracheal intubation: A critical review. Pediatr. Dent. 1989, 11, 133–140. [Google Scholar] [PubMed]
- Proffit, W.R.; Fields, H.W., Jr.; Ackerman, J.L.; Bailey, L.J.; Camilla, T.J.F. Contemporary Orthodontics, 3rd ed.; Mosby: St Louis, MI, USA, 2000; Volume 78, p. 124. [Google Scholar]
- Monsour, F.N.; Adkins, K.F. Responses of periodontal tissues and cementum following transplantation of teeth. J. Oral. Maxillofac. Surg. 1984, 42, 441–446. [Google Scholar] [CrossRef]
- Olaru, M.; Sachelarie, L.; Calin, G. Hard Dental Tissues Regeneration—Approaches and Challenges. Materials 2021, 14, 2558. [Google Scholar] [CrossRef]
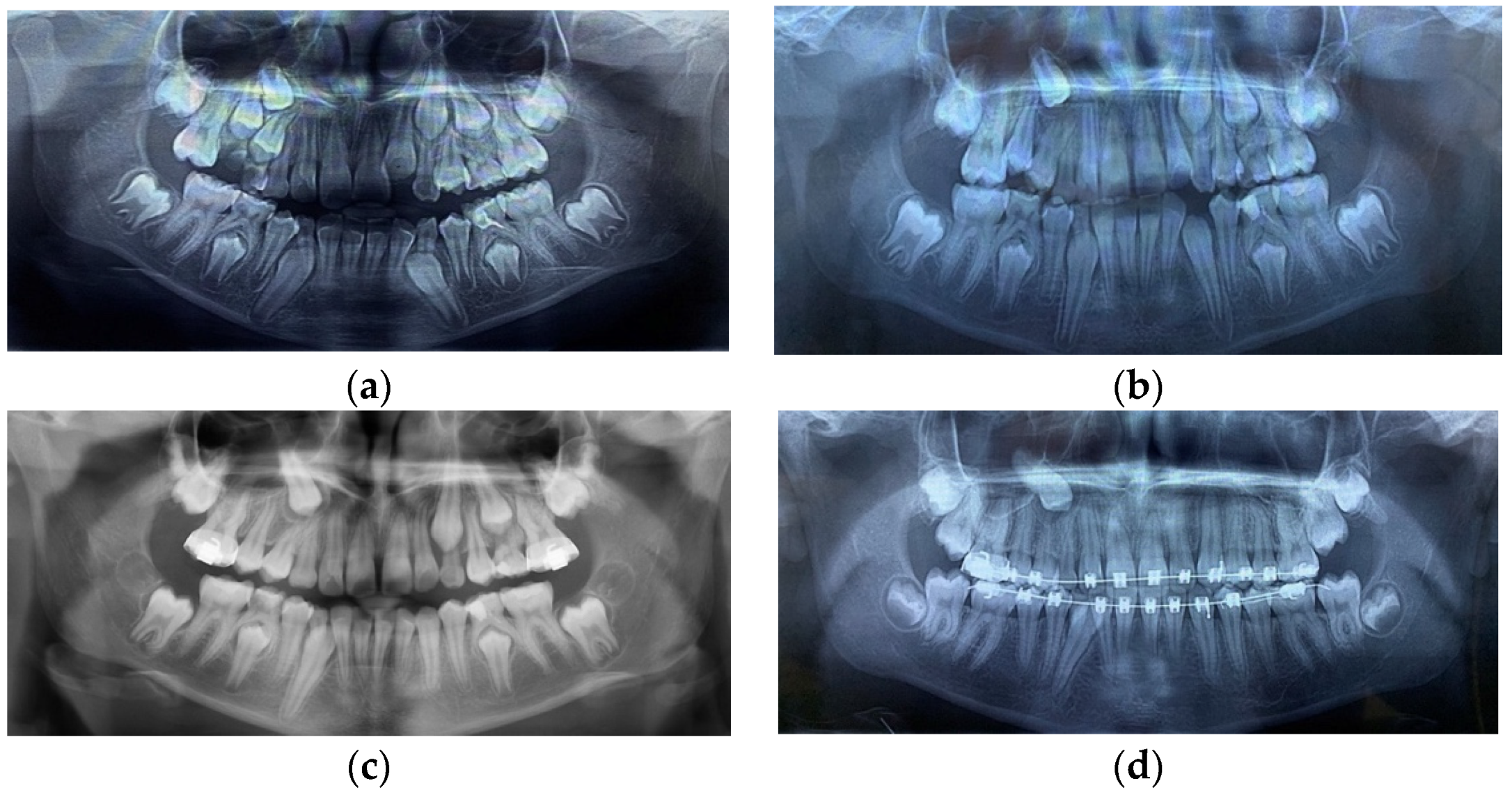
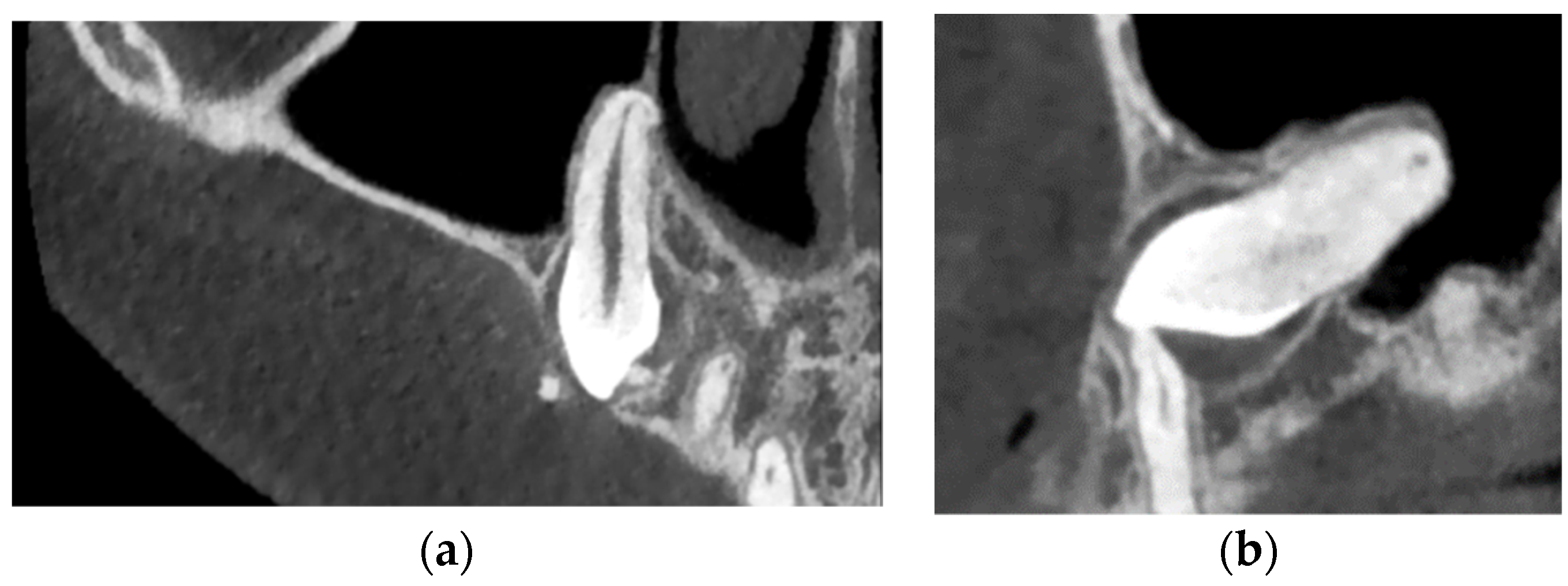
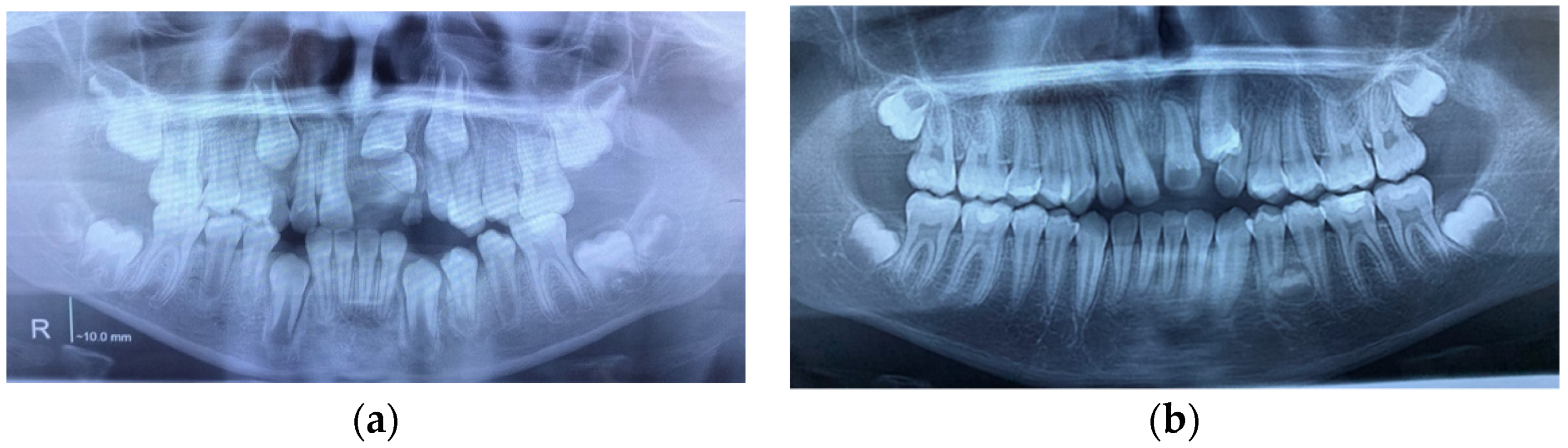
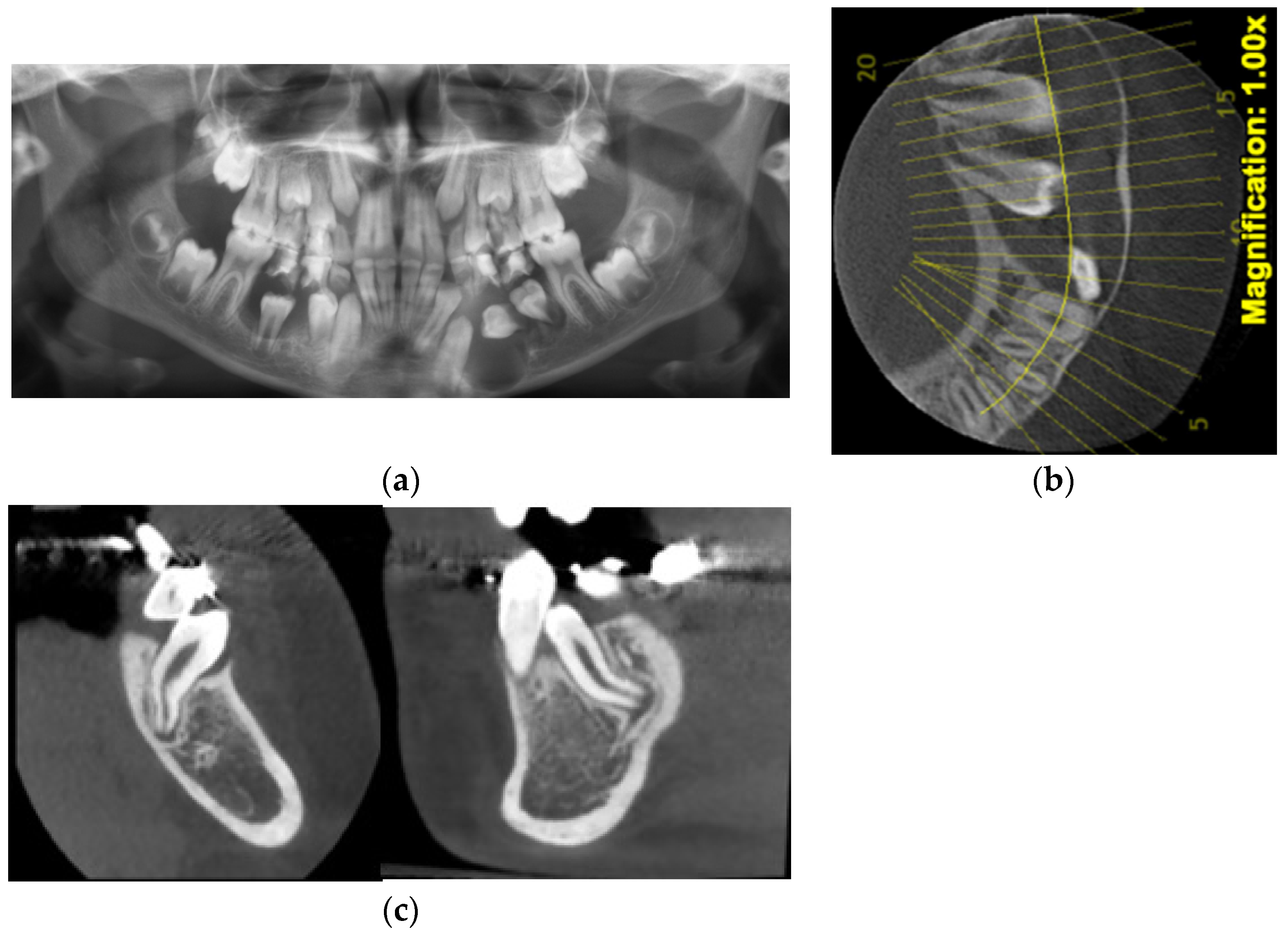
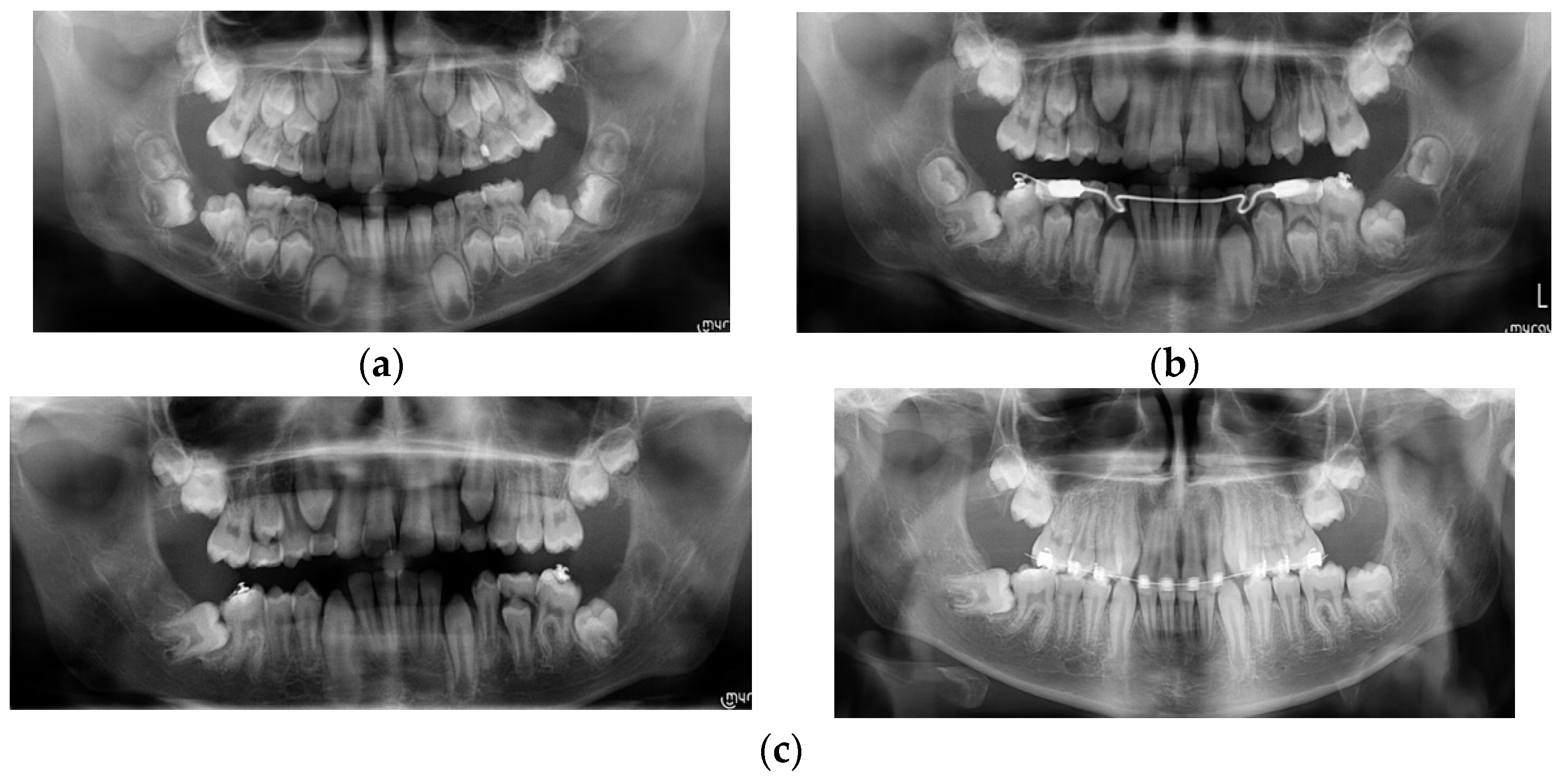
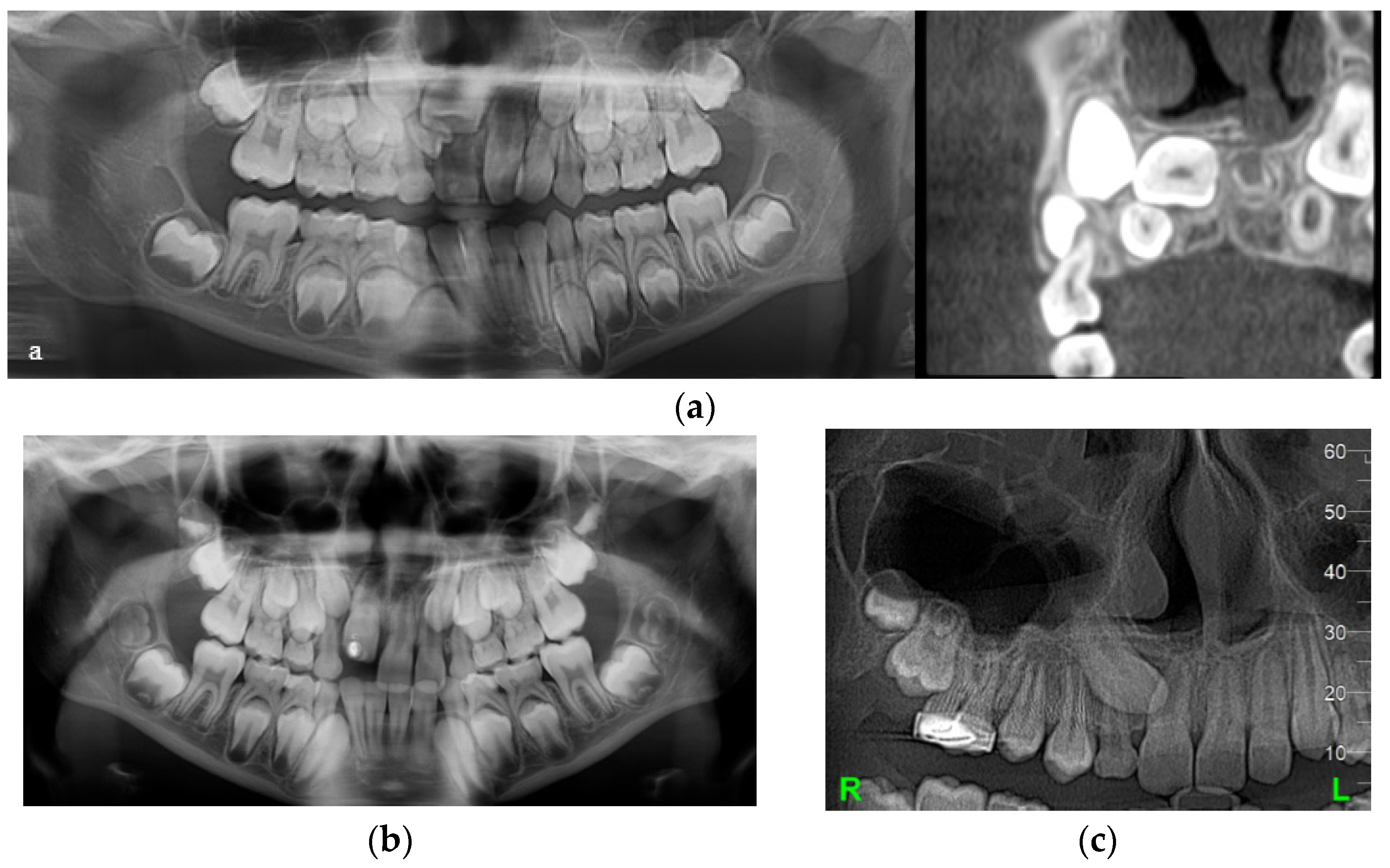
| Case Number | Summary of X-ray Findings |
|---|---|
| Case 1 |
|
| Case 2 |
|
| Case 3 |
|
| Case 4 |
|
| Case 5 |
|
| Case No./Position of DLs or DCs | 1 Right DL | 1 Left DL | 2 | 3 Right DC | 3 Left DC | 4 Right DC | 4 Left DC | 5 Right DL | 5 Left DL |
|---|---|---|---|---|---|---|---|---|---|
| DL | Y | Y | Y | N | Y | Y | Y | Y | Y |
| DC | Y | N | Y | Y | Y | Y | Y | Y | Y 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Enache, A.M.; Feștilă, D.; Boboc, F.; Nagy, E.B.; Ghergie, M.; Dorobanțu, M. Root Dilaceration and Dentigerous Cyst—A Cause–Effect Relationship?—“Case-Series Study”. Appl. Sci. 2022, 12, 9854. https://doi.org/10.3390/app12199854
Enache AM, Feștilă D, Boboc F, Nagy EB, Ghergie M, Dorobanțu M. Root Dilaceration and Dentigerous Cyst—A Cause–Effect Relationship?—“Case-Series Study”. Applied Sciences. 2022; 12(19):9854. https://doi.org/10.3390/app12199854
Chicago/Turabian StyleEnache, Aurelia Magdalena, Dana Feștilă, Florin Boboc, Evelyn Beatrix Nagy, Mircea Ghergie, and Mihai Dorobanțu. 2022. "Root Dilaceration and Dentigerous Cyst—A Cause–Effect Relationship?—“Case-Series Study”" Applied Sciences 12, no. 19: 9854. https://doi.org/10.3390/app12199854
APA StyleEnache, A. M., Feștilă, D., Boboc, F., Nagy, E. B., Ghergie, M., & Dorobanțu, M. (2022). Root Dilaceration and Dentigerous Cyst—A Cause–Effect Relationship?—“Case-Series Study”. Applied Sciences, 12(19), 9854. https://doi.org/10.3390/app12199854







