Iron Depletion in Systemic and Muscle Compartments Defines a Specific Phenotype of Severe COPD in Female and Male Patients: Implications in Exercise Tolerance
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Exclusion Criteria
2.3. Anthropometric and Lung Function Assessment
2.4. Exercise Capacity and Muscle Function Assessment
2.5. Blood Samples and Muscle Biopsies
2.6. Biological Analyses
2.7. Statistical Analysis
3. Results
3.1. General Clinical Features of the Study Patients
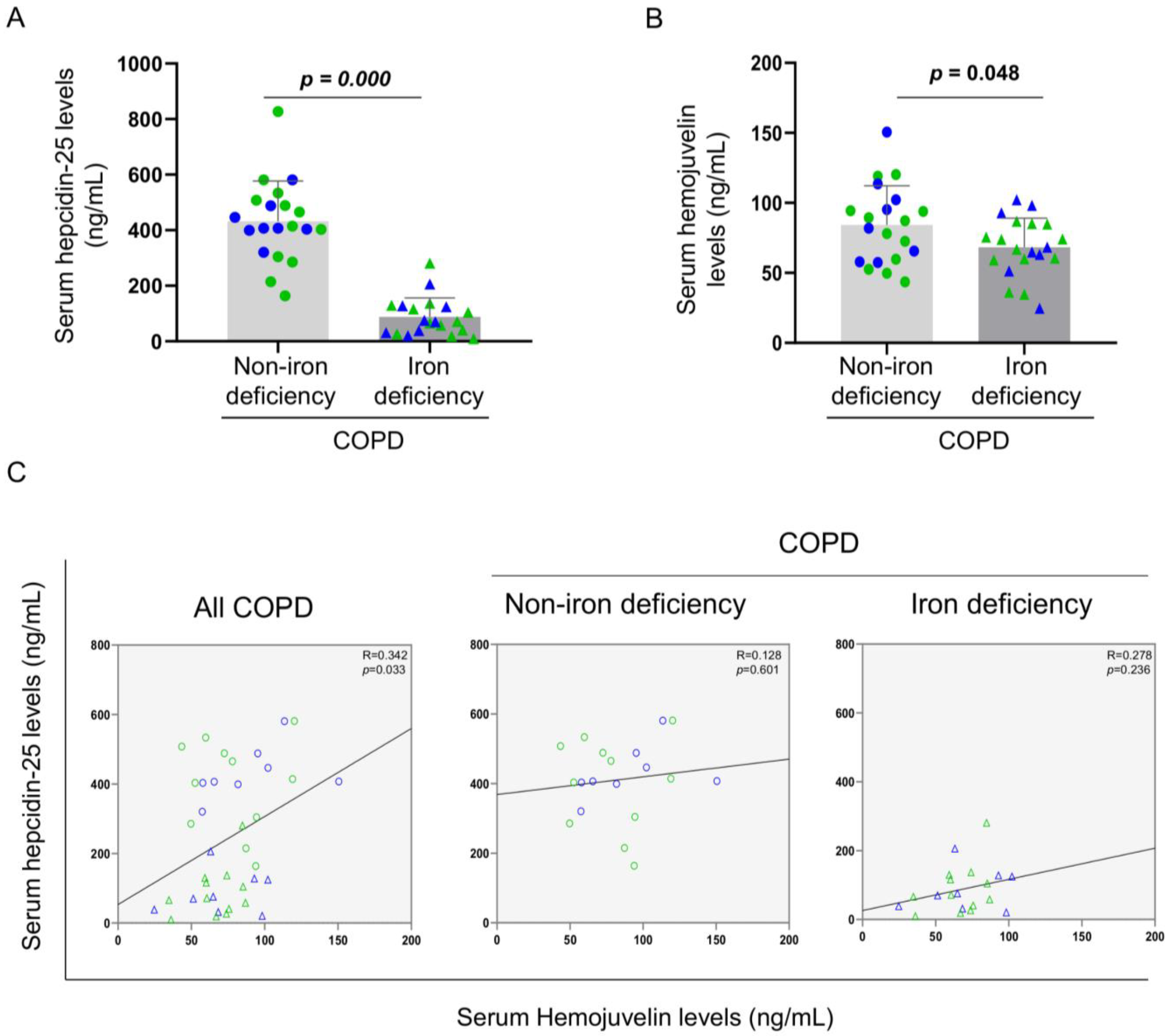
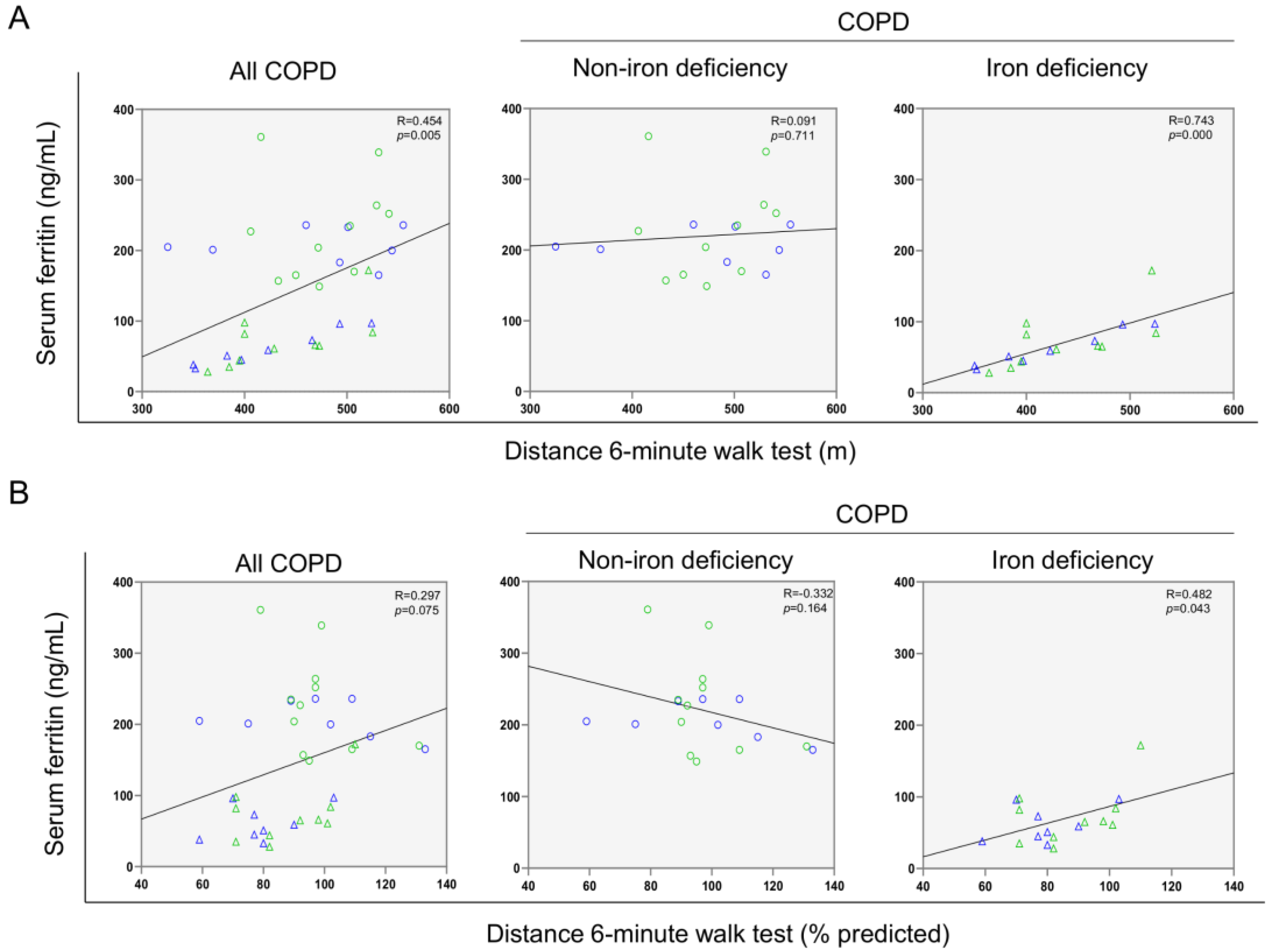
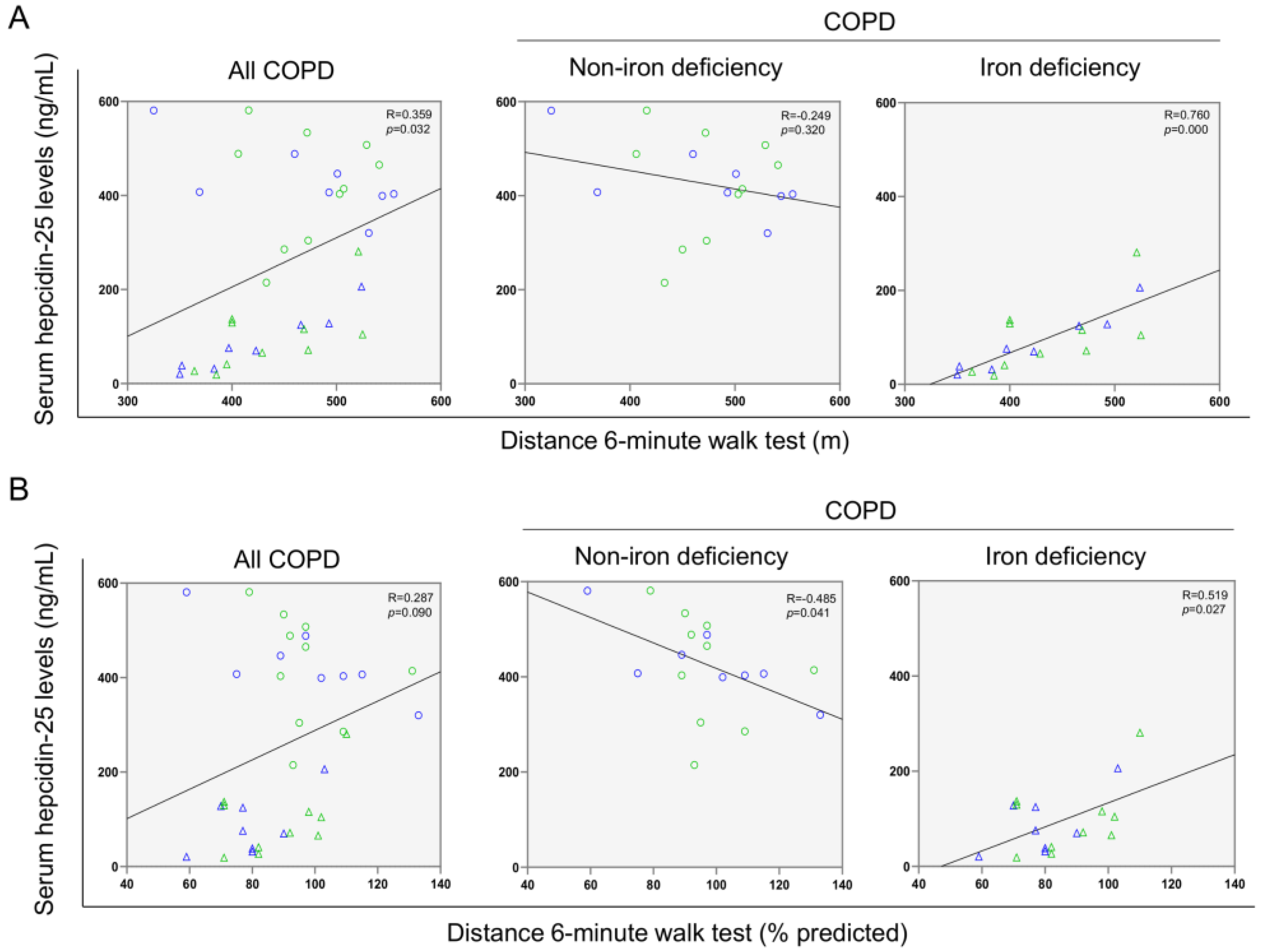
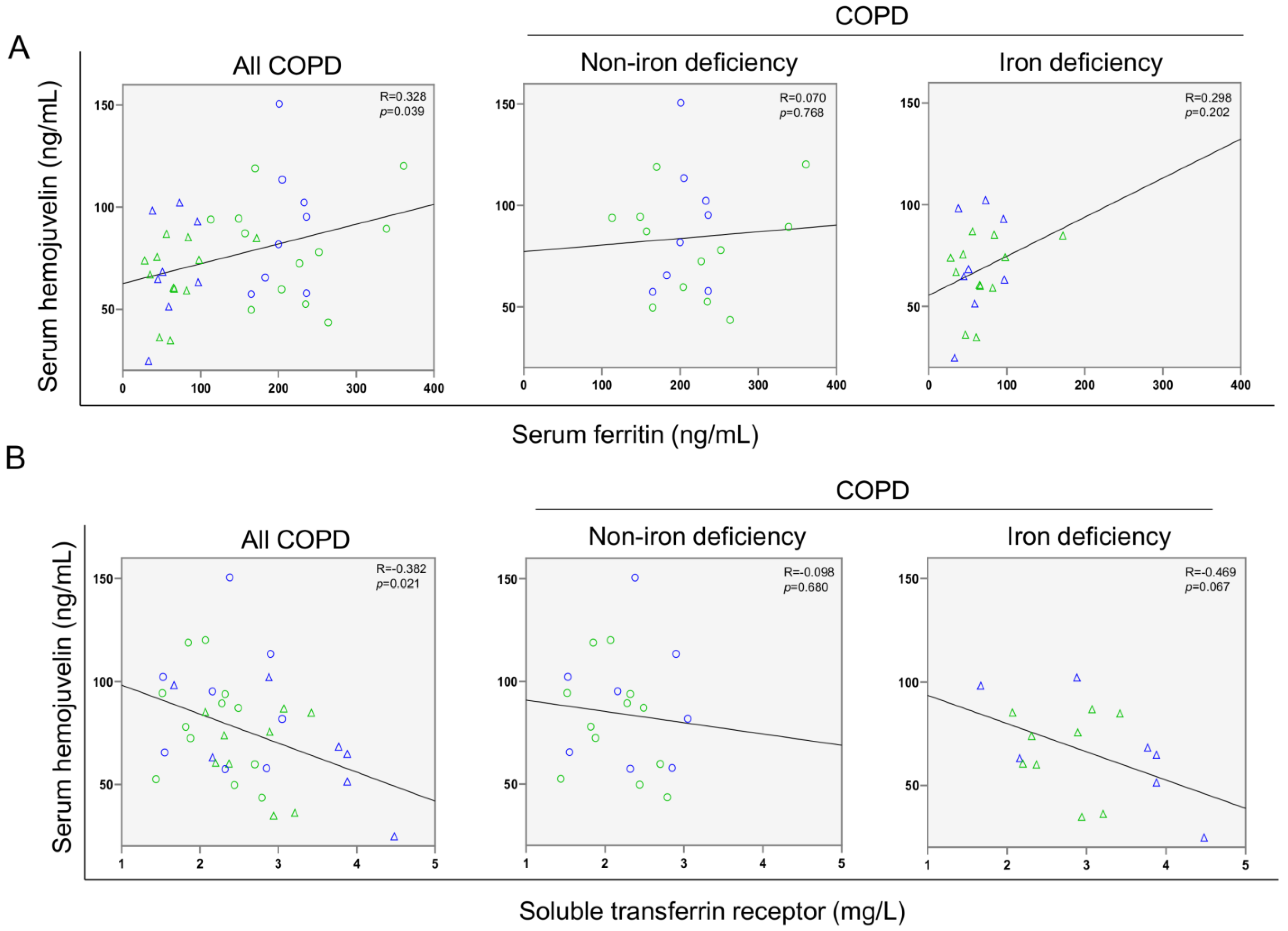
3.2. Associations between Clinical Parameters and Serum Iron Metabolism Markers
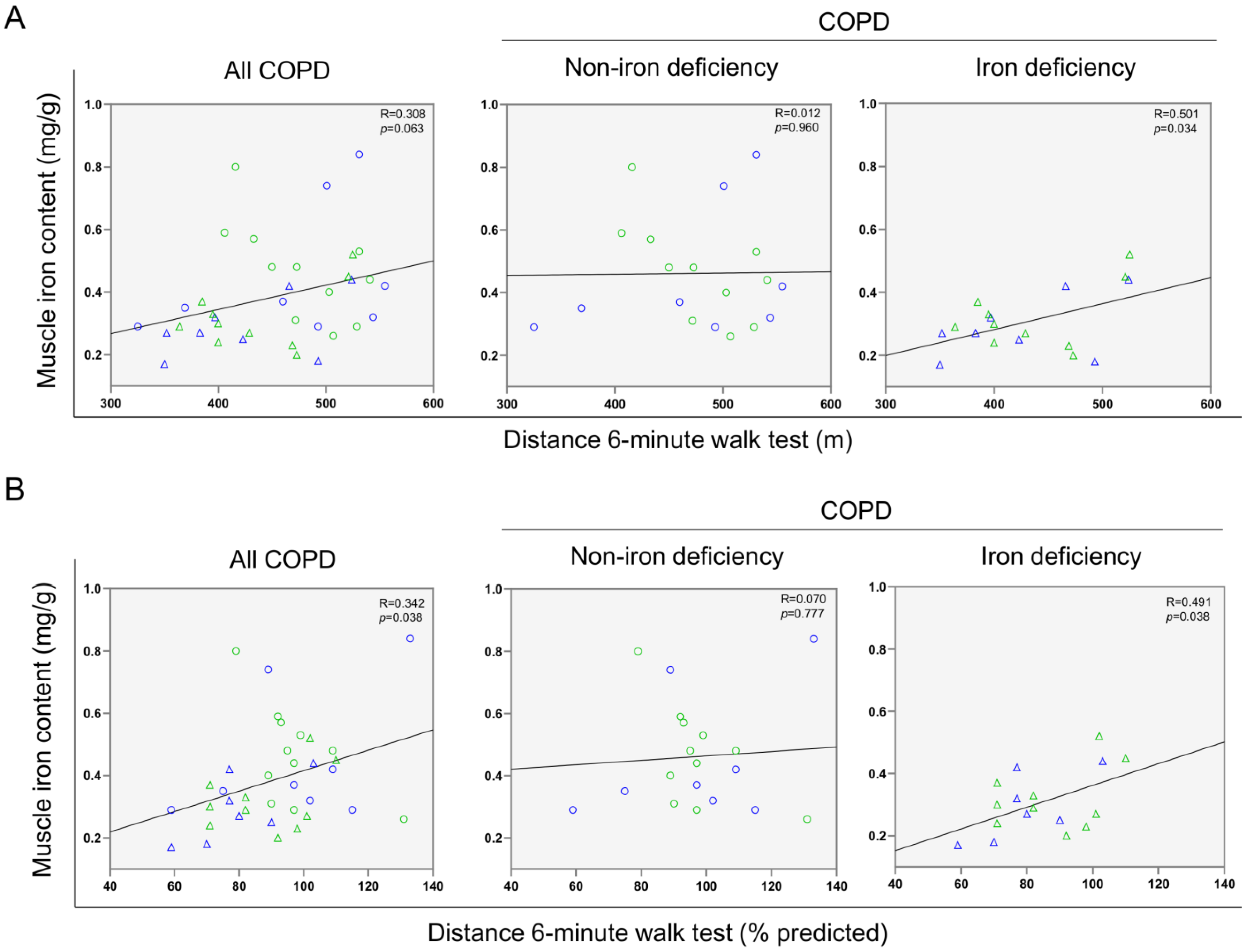
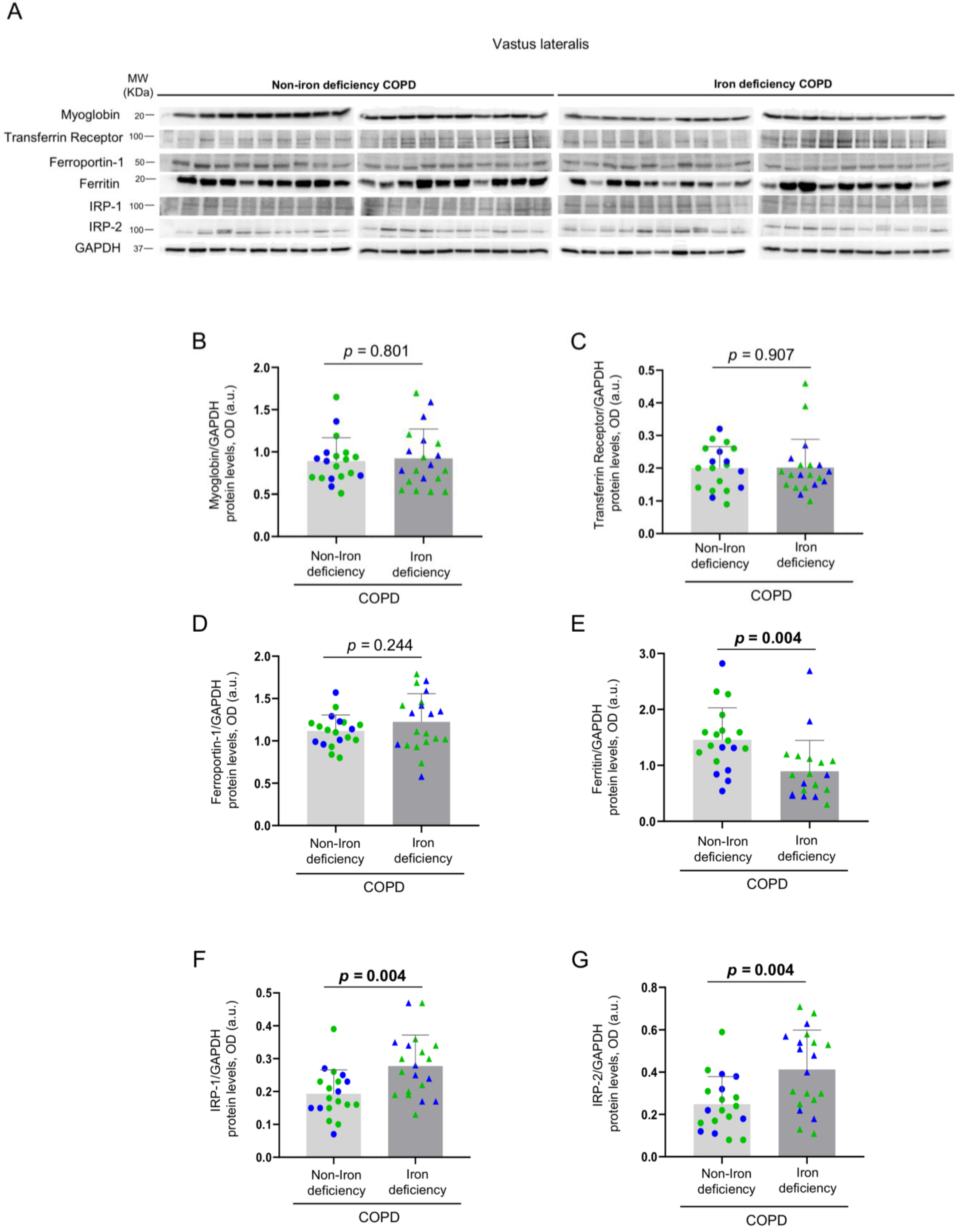
3.3. Iron Metabolism in the Vastus Lateralis
4. Discussion
Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Machado, A.; Marques, A.; Burtin, C. Extra-pulmonary manifestations of COPD and the role of pulmonary rehabilitation: A symptom-centered approach. Expert Rev. Respir. Med. 2020, 15, 131–142. [Google Scholar] [CrossRef]
- Kaluźniak-Szymanowska, A.; Krzymińska-Siemaszko, R.; Deskur-śmielecka, E.; Lewandowicz, M.; Kaczmarek, B.; Wieczorowska-Tobis, K. Malnutrition, Sarcopenia, and Malnutrition-Sarcopenia Syndrome in Older Adults with COPD. Nutrients 2021, 14, 44. [Google Scholar] [CrossRef]
- Cloonan, S.M.; Mumby, S.; Adcock, I.M.; Choi, A.M.K.; Chung, K.F.; Quinlan, G.J. The iron-y of iron overload and iron deficiency in chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2017, 196, 1103–1112. [Google Scholar] [CrossRef]
- Silverberg, D.S.; Mor, R.; Weu, M.T.; Schwartz, D.; Schwartz, I.F.; Chernin, G. Anemia and iron deficiency in COPD patients: Prevalence and the effects of correction of the anemia with erythropoiesis stimulating agents and intravenous iron. BMC Pulm. Med. 2014, 14, 24. [Google Scholar] [CrossRef] [PubMed]
- Nickol, A.H.; Frise, M.C.; Cheng, H.Y.; McGahey, A.; McFadyen, B.M.; Harris-Wright, T.; Bart, N.K.; Curtis, M.K.; Khandwala, S.; O’Neill, D.P.; et al. A cross-sectional study of the prevalence and associations of iron deficiency in a cohort of patients with chronic obstructive pulmonary disease. BMJ Open 2015, 5, e007911. [Google Scholar] [CrossRef]
- Rathi, V.; Ish, P.; Singh, G.; Tiwari, M.; Goel, N.; Gaur, S.N. Iron deficiency in non-anemic chronic obstructive pulmonary disease in a predominantly male population: An ignored entity. Arch. Monaldi Per Le Mal. Del Torace 2020, 90, 38–42. [Google Scholar] [CrossRef]
- Boldt, D.H. New perspectives on iron: An introduction. Am. J. Med. Sci. 1999, 318, 207. [Google Scholar] [CrossRef]
- Winter, W.E.; Bazydlo, L.A.L.; Harris, N.S. The molecular biology of human iron metabolism. Lab. Med. 2014, 45, 92–102. [Google Scholar] [CrossRef]
- Vogt, A.C.S.; Arsiwala, T.; Mohsen, M.; Vogel, M.; Manolova, V.; Bachmann, M.F. On Iron Metabolism and Its Regulation. Int. J. Mol. Sci. 2021, 22, 4591. [Google Scholar] [CrossRef]
- Roemhild, K.; von Maltzahn, F.; Weiskirchen, R.; Knüchel, R.; von Stillfried, S.; Lammers, T. Iron metabolism: Pathophysiology and pharmacology. Trends Pharmacol. Sci. 2021, 42, 640–656. [Google Scholar] [CrossRef]
- Mleczko-Sanecka, K.; Silvestri, L. Cell-type-specific insights into iron regulatory processes. Am. J. Hematol. 2021, 96, 110–127. [Google Scholar] [CrossRef]
- Malyszko, J. Hemojuvelin: The hepcidin story continues. Kidney Blood Press. Res. 2009, 32, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Nemeth, E.; Ganz, T. Hepcidin-Ferroportin Interaction Controls Systemic Iron Homeostasis. Int. J. Mol. Sci. 2021, 22, 6493. [Google Scholar] [CrossRef]
- Mackay, A.; Loza, M.; Branigan, P.; George, S.; Donaldson, G.; Baribaud, F.; Wedzicha, J. Inflammatory serum profiles are consistent across independent exacerbations in COPD patients with a history of frequent exacerbations. Eur. Respir. J. 2015, 46, PA407. [Google Scholar] [CrossRef]
- Tandara, L.; Grubisic, T.Z.; Ivan, G.; Jurisic, Z.; Tandara, M.; Gugo, K.; Mladinov, S.; Salamunic, I. Systemic inflammation up-regulates serum hepcidin in exacerbations and stabile chronic obstructive pulmonary disease. Clin. Biochem. 2015, 48, 1252–1257. [Google Scholar] [CrossRef]
- Wang, C.Y.; Babitt, J.L. Hepcidin Regulation in the Anemia of Inflammation. Curr. Opin. Hematol. 2016, 23, 189. [Google Scholar] [CrossRef] [PubMed]
- Wyart, E.; Hsu, M.Y.; Sartori, R.; Mina, E.; Rausch, V.; Pierobon, E.S.; Mezzanotte, M.; Pezzini, C.; Bindels, L.B.; Lauria, A.; et al. Iron supplementation is sufficient to rescue skeletal muscle mass and function in cancer cachexia. EMBO Rep. 2022, 23, e53746. [Google Scholar] [CrossRef]
- Zhou, D.; Zhang, Y.; Mamtawla, G.; Wan, S.; Gao, X.; Zhang, L.; Li, G.; Wang, X. Iron overload is related to muscle wasting in patients with cachexia of gastric cancer: Using quantitative proteome analysis. Med. Oncol. 2020, 37, 1–11. [Google Scholar] [CrossRef]
- Wilson, A.C.; Kumar, P.L.; Lee, S.; Parker, M.M.; Arora, I.; Morrow, J.D.; Wouters, E.F.M.; Casaburi, R.; Rennard, S.I.; Lomas, D.A.; et al. Heme metabolism genes Downregulated in COPD Cachexia. Respir. Res. 2020, 21, 100. [Google Scholar] [CrossRef]
- Leermakers, P.A.; Schols, A.M.W.J.; Kneppers, A.E.M.; Kelders, M.C.J.M.; de Theije, C.C.; Lainscak, M.; Gosker, H.R. Molecular signalling towards mitochondrial breakdown is enhanced in skeletal muscle of patients with chronic obstructive pulmonary disease (COPD). Sci. Rep. 2018, 8, 15007. [Google Scholar] [CrossRef]
- Pérez-Peiró, M.; Martín-Ontiyuelo, C.; Rodó-Pi, A.; Piccari, L.; Admetlló, M.; Durán, X.; Rodríguez-Chiaradía, D.A.; Barreiro, E. Iron Replacement and Redox Balance in Non-Anemic and Mildly Anemic Iron Deficiency COPD Patients: Insights from a Clinical Trial. Biomedicines 2021, 9, 1191. [Google Scholar] [CrossRef] [PubMed]
- Martín-Ontiyuelo, C.; Rodó-Pin, A.; Sancho-Muñoz, A.; Martinez-Llorens, J.M.; Admetlló, M.; Molina, L.; Gea, J.; Barreiro, E.; Chiaradía, D.A.R. Is iron deficiency modulating physical activity in COPD? Int. J. Chron. Obstruct. Pulmon. Dis. 2019, 14, 211–214. [Google Scholar] [CrossRef]
- Martín-Ontiyuelo, C.; Rodó-Pin, A.; Echeverría-Esnal, D.; Admetlló, M.; Duran-Jordà, X.; Alvarado, M.; Gea, J.; Barreiro, E.; Rodríguez-Chiaradía, D.A. Intravenous Iron Replacement Improves Exercise Tolerance in COPD: A Single-Blind Randomized Trial. Arch. Bronconeumol. 2021, 10, 2903. [Google Scholar] [CrossRef]
- Venkatesan, P. GOLD report: 2022 update. Lancet Respir. Med. 2022, 10, e20. [Google Scholar] [CrossRef]
- Barberan-Garcia, A.; Rodríguez, D.A.; Blanco, I.; Gea, J.; Torralba, Y.; Arbillaga-Etxarri, A.; Barberà, J.A.; Vilarõ, J.; Roca, J.; Orozco-Levi, M. Non-anaemic iron deficiency impairs response to pulmonary rehabilitation in COPD. Respirology 2015, 20, 1089–1095. [Google Scholar] [CrossRef] [PubMed]
- Anker, S.D.; Comin Colet, J.; Filippatos, G.; Willenheimer, R.; Dickstein, K.; Drexler, H.; Lüscher, T.F.; Bart, B.; Banasiak, W.; Niegowska, J.; et al. Ferric Carboxymaltose in Patients with Heart Failure and Iron Deficiency. N. Engl. J. Med. 2009, 361, 2436–2448. [Google Scholar] [CrossRef] [PubMed]
- Sancho-Muñoz, A.; Guitart, M.; Rodríguez, D.A.; Gea, J.; Martínez-Llorens, J.; Barreiro, E. Deficient muscle regeneration potential in sarcopenic COPD patients: Role of satellite cells. J. Cell. Physiol. 2021, 236, 3083–3098. [Google Scholar] [CrossRef]
- Barreiro, E.; Salazar-Degracia, A.; Sancho-Muñoz, A.; Gea, J. Endoplasmic reticulum stress and unfolded protein response profile in quadriceps of sarcopenic patients with respiratory diseases. J. Cell. Physiol. 2019, 234, 11315–11329. [Google Scholar] [CrossRef] [PubMed]
- Puig-Vilanova, E.; Martínez-Llorens, J.; Ausin, P.; Roca, J.; Gea, J.; Barreiro, E. Quadriceps muscle weakness and atrophy are associated with a differential epigenetic profile in advanced COPD. Clin. Sci. 2015, 128, 905–921. [Google Scholar] [CrossRef]
- Roca, J.; Burgos, F.; Barberà, J.A.; Sunyer, J.; Rodriguez-Roisin, R.; Castellsagué, J.; Sanchis, J.; Antóo, J.M.; Casan, P.; Clausen, J.L. Prediction equations for plethysmographic lung volumes. Respir. Med. 1998, 92, 454–460. [Google Scholar] [CrossRef]
- Roca, J.; Burgos, F.; Sunyer, J.; Saez, M.; Chinn, S.; Anto, J.; Rodriguez-Roisin, R.; Quanjer, P.; Nowak, D.; Burney, P. References values for forced spirometry. Group of the European Community Respiratory Health Survey. Eur. Respir. J. 1998, 11, 1354–1362. [Google Scholar] [CrossRef]
- Roca, J.; Vargas, C.; Cano, I.; Selivanov, V.; Barreiro, E.; Maier, D.; Falciani, F.; Wagner, P.; Cascante, M.; Garcia-Aymerich, J.; et al. Chronic Obstructive Pulmonary Disease heterogeneity: Challenges for health risk assessment, stratification and management. J. Transl. Med. 2014, 12, S3. [Google Scholar] [CrossRef]
- Rodriguez, D.A.; Kalko, S.; Puig-Vilanova, E.; Perez-Olabarría, M.; Falciani, F.; Gea, J.; Cascante, M.; Barreiro, E.; Roca, J. Muscle and blood redox status after exercise training in severe COPD patients. Free Radic. Biol. Med. 2012, 52, 88–94. [Google Scholar] [CrossRef]
- Luna-Heredia, E.; Martín-Peña, G.; Ruiz-Galiana, J. Handgrip dynamometry in healthy adults. Clin. Nutr. 2005, 24, 250–258. [Google Scholar] [CrossRef]
- Bui, K.L.; Mathur, S.; Dechman, G.; Maltais, F.; Camp, P.; Saey, D. Fixed Handheld Dynamometry Provides Reliable and Valid Values for Quadriceps Isometric Strength in People With Chronic Obstructive Pulmonary Disease: A Multicenter Study. Phys. Ther. 2019, 99, 1255–1267. [Google Scholar] [CrossRef] [PubMed]
- Seymour, J.M.; Spruit, M.A.; Hopkinson, N.S.; Natanek, S.A.; Man, W.D.C.; Jackson, A.; Gosker, H.R.; Schols, A.M.W.J.; Moxham, J.; Polkey, M.I.; et al. The prevalence of quadriceps weakness in COPD and the relationship with disease severity. Eur. Respir. J. 2010, 36, 81–88. [Google Scholar] [CrossRef]
- Puig-Vilanova, E.; Rodriguez, D.A.; Lloreta, J.; Ausin, P.; Pascual-Guardia, S.; Broquetas, J.; Roca, J.; Gea, J.; Barreiro, E. Oxidative stress, redox signaling pathways, and autophagy in cachectic muscles of male patients with advanced COPD and lung cancer. Free Radic. Biol. Med. 2015, 79, 91–108. [Google Scholar] [CrossRef]
- Firkin, F.; Rush, B. Interpretation of biochemical tests for iron deficiency: Diagnostic difficulties related to limitations of individual tests. Aust. Prescr. 1997, 20, 74–76. [Google Scholar] [CrossRef]
- Cohen-Solal, A.; Leclercq, C.; Deray, G.; Lasocki, S.; Zambrowski, J.J.; Mebazaa, A.; De Groote, P.; Dam, T.; Galinier, M. Iron deficiency: An emerging therapeutic target in heart failure. Heart 2014, 100, 1414–1420. [Google Scholar] [CrossRef]
- Buttarello, M.; Pajola, R.; Novello, E.; Mezzapelle, G.; Plebani, M. Evaluation of the hypochromic erythrocyte and reticulocyte hemoglobin content provided by the Sysmex XE-5000 analyzer in diagnosis of iron deficiency erythropoiesis. Clin. Chem. Lab. Med. 2016, 54, 1939–1945. [Google Scholar] [CrossRef]
- Özdemir, N. Iron deficiency anemia from diagnosis to treatment in children. Turk. Arch. Pediatrics Pediatri Arşivi 2015, 50, 11. [Google Scholar] [CrossRef] [PubMed]
- Enjuanes, C.; Bruguera, J.; Grau, M.; Cladellas, M.; Gonzalez, G.; Meroño, O.; Moliner-Borja, P.; Verdú, J.M.; Farré, N.; Comín-Colet, J. Estado del hierro en la insuficiencia cardiaca crónica: Impacto en síntomas, clase funcional y capacidad de ejercicio submáxima. Rev. Española Cardiol. 2016, 69, 247–255. [Google Scholar] [CrossRef]
- Barandiarán Aizpurua, A.; Sanders-van Wijk, S.; Brunner-La Rocca, H.P.; Henkens, M.T.H.M.; Weerts, J.; Spanjers, M.H.A.; Knackstedt, C.; van Empel, V.P.M. Iron deficiency impacts prognosis but less exercise capacity in heart failure with preserved ejection fraction. ESC Heart Fail. 2021, 8, 1304–1313. [Google Scholar] [CrossRef]
- Cote, C.; Zilberberg, M.D.; Mody, S.H.; Dordelly, L.J.; Celli, B. Haemoglobin level and its clinical impact in a cohort of patients with COPD. Eur. Respir. J. 2007, 29, 923–929. [Google Scholar] [CrossRef]
- Pizzini, A.; Aichner, M.; Sonnweber, T.; Tancevski, I.; Weiss, G.; Löffler-Ragg, J. The Significance of iron deficiency and anemia in a real-life COPD cohort. Int. J. Med. Sci. 2020, 17, 2232. [Google Scholar] [CrossRef] [PubMed]
- Ghio, A.J.; Hilborn, E.D. Indices of iron homeostasis correlate with airway obstruction in an NHANES III cohort. Int. J. Chron. Obstruct. Pulmon. Dis. 2017, 12, 2075. [Google Scholar] [CrossRef]
- Sharma, S.; Nemeth, E.; Chen, Y.H.; Goodnough, J.; Huston, A.; Roodman, G.D.; Ganz, T.; Lichtenstein, A. Involvement of hepcidin in the anemia of multiple myeloma. Clin. Cancer Res. 2008, 14, 3262–3267. [Google Scholar] [CrossRef]
- Joachim, J.H.; Mehta, K.J. Hepcidin in hepatocellular carcinoma. Br. J. Cancer 2022, 127, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Krawiec, P.; Mroczkowska-Juchkiewicz, A.; Pac-Kozuchowska, E. Serum Hepcidin in Children with Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2017, 23, 2165–2171. [Google Scholar] [CrossRef]
- Attia, A.; Mohammed, T.; Abd Al Aziz, U. The relationship between serum hepcidin level and hypoxemia in the COPD patients. Egypt. J. Chest Dis. Tuberc. 2015, 64, 57–61. [Google Scholar] [CrossRef]
- Duru, S.; Bilgin, E.; Ardiç, S. Hepcidin: A useful marker in chronic obstructive pulmonary disease. Ann. Thorac. Med. 2012, 7, 31. [Google Scholar] [CrossRef] [PubMed]
- Wisaksana, R.; De Mast, Q.; Alisjahbana, B.; Jusuf, H.; Sudjana, P.; Indrati, A.R.; Sumantri, R.; Swinkels, D.; Van Crevel, R.; Van Der Ven, A. Inverse Relationship of Serum Hepcidin Levels with CD4 Cell Counts in HIV-Infected Patients Selected from an Indonesian Prospective Cohort Study. PLoS ONE 2013, 8, e79904. [Google Scholar] [CrossRef] [PubMed]
- Gaillard, C.A.; Bock, A.H.; Carrera, F.; Eckardt, K.U.; Van Wyck, D.B.; Bansal, S.S.; Cronin, M.; Meier, Y.; Larroque, S.; Roger, S.D.; et al. Hepcidin Response to Iron Therapy in Patients with Non-Dialysis Dependent CKD: An Analysis of the FIND-CKD Trial. PLoS ONE 2016, 11, e0157063. [Google Scholar] [CrossRef] [PubMed]
- Berglund, S.; Lönnerdal, B.; Westrup, B.; Domellöf, M. Effects of iron supplementation on serum hepcidin and serum erythropoietin in low-birth-weight infants. Am. J. Clin. Nutr. 2011, 94, 1553–1561. [Google Scholar] [CrossRef] [PubMed]
- Lasocki, S.; Lefebvre, T.; Mayeur, C.; Puy, H.; Mebazaa, A.; Gayat, E.; Deye, N.; Fauvaux, C.; Mebazaa, A.; Damoisel, C.; et al. Iron deficiency diagnosed using hepcidin on critical care discharge is an independent risk factor for death and poor quality of life at one year: An observational prospective study on 1161 patients. Crit. Care 2018, 22, 1–8. [Google Scholar] [CrossRef]
- Atkinson, S.H.; Armitage, A.E.; Khandwala, S.; Mwangi, T.W.; Uyoga, S.; Bejon, P.A.; Williams, T.N.; Prentice, A.M.; Drakesmith, H. Combinatorial effects of malaria season, iron deficiency, and inflammation determine plasma hepcidin concentration in African children. Blood 2014, 123, 3221–3229. [Google Scholar] [CrossRef]
- Core, A.B.; Canali, S.; Babitt, J.L. Hemojuvelin and bone morphogenetic protein (BMP) signaling in iron homeostasis. Front. Pharmacol. 2014, 5, 104. [Google Scholar] [CrossRef]
- Shalev, H.; Perez-Avraham, G.; Kapelushnik, J.; Levi, I.; Rabinovich, A.; Swinkels, D.W.; Brasse-Lagnel, C.; Tamary, H. High levels of soluble serum hemojuvelin in patients with congenital dyserythropoietic anemia type I. Eur. J. Haematol. 2013, 90, 31–36. [Google Scholar] [CrossRef]
- Brasse-Lagnel, C.; Poli, M.; Lesueur, C.; Grandchamp, B.; Lavoinne, A.; Beaumont, C.; Bekri, S. Immunoassay for human serum hemojuvelin. Haematologica 2010, 95, 2031–2037. [Google Scholar] [CrossRef]
- Malyszko, J.; Malyszko, J.S.; Levin-Iaina, N.; Koc-Zorawska, E.; Kozminski, P.; Mysliwiec, M. Is hemojuvelin a possible new player in iron metabolism in hemodialysis patients? Int. Urol. Nephrol. 2012, 44, 1805–1811. [Google Scholar] [CrossRef][Green Version]
- Rumjon, A.; Sarafidis, P.; Brincat, S.; Musto, R.; Malyszko, J.; Bansal, S.S.; Macdougall, I.C. Serum hemojuvelin and hepcidin levels in chronic kidney disease. Am. J. Nephrol. 2012, 35, 295–304. [Google Scholar] [CrossRef] [PubMed]
- Constante, M.; Wang, D.; Raymond, V.A.; Bilodeau, M.; Santos, M.M. Repression of repulsive guidance molecule C during inflammation is independent of Hfe and involves tumor necrosis factor-α. Am. J. Pathol. 2007, 170, 497–504. [Google Scholar] [CrossRef] [PubMed]
- Kernan, K.F.; Carcillo, J.A. Hyperferritinemia and inflammation. Int. Immunol. 2017, 29, 401. [Google Scholar] [CrossRef] [PubMed]



| COPD Patients | |||
|---|---|---|---|
| Non-Iron Deficiency | Iron Deficiency | p Value | |
| N = 20 | N = 20 | ||
| Anthropometry | |||
| Age (years) | 68 (8) | 66 (8) | 0.637 |
| Males/Females | 12/8 | 12/8 | 1.000 |
| Body weight (kg) | 60.3 (11.4) | 64.0 (12.7) | 0.291 |
| BMI (kg/m2) | 22.8 (3.5) | 24.1 (4.2) | 0.287 |
| FFMI (kg/m2) | 15.7 (2.2) | 14.9 (2.2) | 0.238 |
| Smoking history | |||
| Active, N (%) | 9 (45) | 12 (60) | 0.525 |
| Ex-smoker, N (%) | 11 (55) | 8 (40) | |
| Packs-year | 52.5 (32.6) | 42.94 (24.8) | 0.327 |
| Lung Function | |||
| FEV1 (L) | 1.19 (0.4) | 1.24 (0.4) | 0.676 |
| FEV1 (% predicted) | 46.7 (16.4) | 44.0 (11.1) | 0.485 |
| FVC (L) | 2.8 (0.5) | 2.7 (0.8) | 0.536 |
| FVC (% predicted) | 84.4 (14.5) | 76.5 (12.0) | 0.071 |
| FEV1/FVC | 44.8 (11.52) | 46.5 (11.1) | 0.626 |
| GOLD classification | |||
| 1, N (%) | 0 (0) | 0 (0) | 0.224 |
| 2, N (%) | 9 (45) | 5 (25) | |
| 3, N (%) | 9 (45) | 12 (60) | |
| 4, N (%) | 2 (10) | 3 (15) | |
| A, N (%) | 11 (55) | 9 (45) | 0.699 |
| B, N (%) | 7 (35) | 9 (45) | |
| C, N (%) | 1 (5) | 1 (5) | |
| D, N (%) | 1 (5) | 1 (5) | |
| COPD Patients | |||
|---|---|---|---|
| Non-Iron Deficiency | Iron Deficiency | p Value | |
| N = 20 | N = 20 | ||
| Six-minute walk test | |||
| Distance (m) | 475.74 (63.29) | 430.50 (64.77) | 0.035 |
| Distance (% predicted) | 97.37 (17.58) | 84.22 (17.14) | 0.019 |
| Upper limb muscle strength | |||
| D-HGS (kg) | 25.83 (7.38) | 28.42 (8.42) | 0.269 |
| D-HGS (% predicted) | 87.52 (18.30) | 93.19 (20.42) | 0.385 |
| ND-HGS (kg) | 23.64 (7.51) | 25.16 (9.03) | 0.648 |
| ND-HGS (% predicted) | 89.26 (23.68) | 89.79 (21.12) | 0.955 |
| Lower limb muscle strength | |||
| D-QMVC (kg) | 22.38 (6.60) | 22.54 (4.19) | 0.332 |
| D-QMVC (% predicted) | 62.70 (21.37) | 62.29 (12.38) | 0.907 |
| ND-QMVC (kg) | 21.29 (5.69) | 21.69 (4.80) | 0.480 |
| ND-QMVC (% predicted) | 60.13 (21.54) | 60.05 (13.97) | 0.953 |
| COPD Patients | |||
|---|---|---|---|
| Non-Iron Deficiency | Iron Deficiency | p Value | |
| N = 20 | N = 20 | ||
| Iron status | |||
| Hemoglobin (g/dL) | 15.2 (1.4) | 15.0 (1.6) | 0.580 |
| Hematocrit (%) | 45.5 (4.7) | 44.8 (4.4) | 0.613 |
| MCV (fL) | 93.7 (3.5) | 91.7 (6.7) | 0.250 |
| MCH (pg) | 31.4 (1.4) | 30.7 (2.8) | 0.311 |
| MCHC (g/dL) | 33.5 (1.3) | 33.4 (1.2) | 0.820 |
| Ferritin (ng/mL) | 214.8 (60.3) | 66.5 (33.0) | 0.000 |
| Transferrin saturation (%) | 31.0 (7.5) | 25.4 (7.2) | 0.024 |
| Transferrin (g/dL) | 236.6 (31.0) | 260.7 (28.9) | 0.012 |
| Soluble transferrin receptor (mg/L) | 2.2 (0.5) | 3.0 (0.8) | 0.002 |
| Serum iron (µg/dL) | 105.8 (26.3) | 94.0 (28.8) | 0.181 |
| Muscle iron content (mg/g) | 0.5 (0.2) | 0.3 (0.1) | 0.002 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pérez-Peiró, M.; Alvarado, M.; Martín-Ontiyuelo, C.; Duran, X.; Rodríguez-Chiaradía, D.A.; Barreiro, E. Iron Depletion in Systemic and Muscle Compartments Defines a Specific Phenotype of Severe COPD in Female and Male Patients: Implications in Exercise Tolerance. Nutrients 2022, 14, 3929. https://doi.org/10.3390/nu14193929
Pérez-Peiró M, Alvarado M, Martín-Ontiyuelo C, Duran X, Rodríguez-Chiaradía DA, Barreiro E. Iron Depletion in Systemic and Muscle Compartments Defines a Specific Phenotype of Severe COPD in Female and Male Patients: Implications in Exercise Tolerance. Nutrients. 2022; 14(19):3929. https://doi.org/10.3390/nu14193929
Chicago/Turabian StylePérez-Peiró, Maria, Mariela Alvarado, Clara Martín-Ontiyuelo, Xavier Duran, Diego A. Rodríguez-Chiaradía, and Esther Barreiro. 2022. "Iron Depletion in Systemic and Muscle Compartments Defines a Specific Phenotype of Severe COPD in Female and Male Patients: Implications in Exercise Tolerance" Nutrients 14, no. 19: 3929. https://doi.org/10.3390/nu14193929
APA StylePérez-Peiró, M., Alvarado, M., Martín-Ontiyuelo, C., Duran, X., Rodríguez-Chiaradía, D. A., & Barreiro, E. (2022). Iron Depletion in Systemic and Muscle Compartments Defines a Specific Phenotype of Severe COPD in Female and Male Patients: Implications in Exercise Tolerance. Nutrients, 14(19), 3929. https://doi.org/10.3390/nu14193929







