Surface Roughness and Color Stability of 3D-Printed Denture Base Materials after Simulated Brushing and Thermocycling
Abstract
:1. Introduction
2. Material and Methods
2.1. Specimen Preparation
2.2. Baseline Surface Roughness and Color Coordinate Measurements
2.3. Simulated Brushing and Thermocycling
2.4. Statistical Analysis
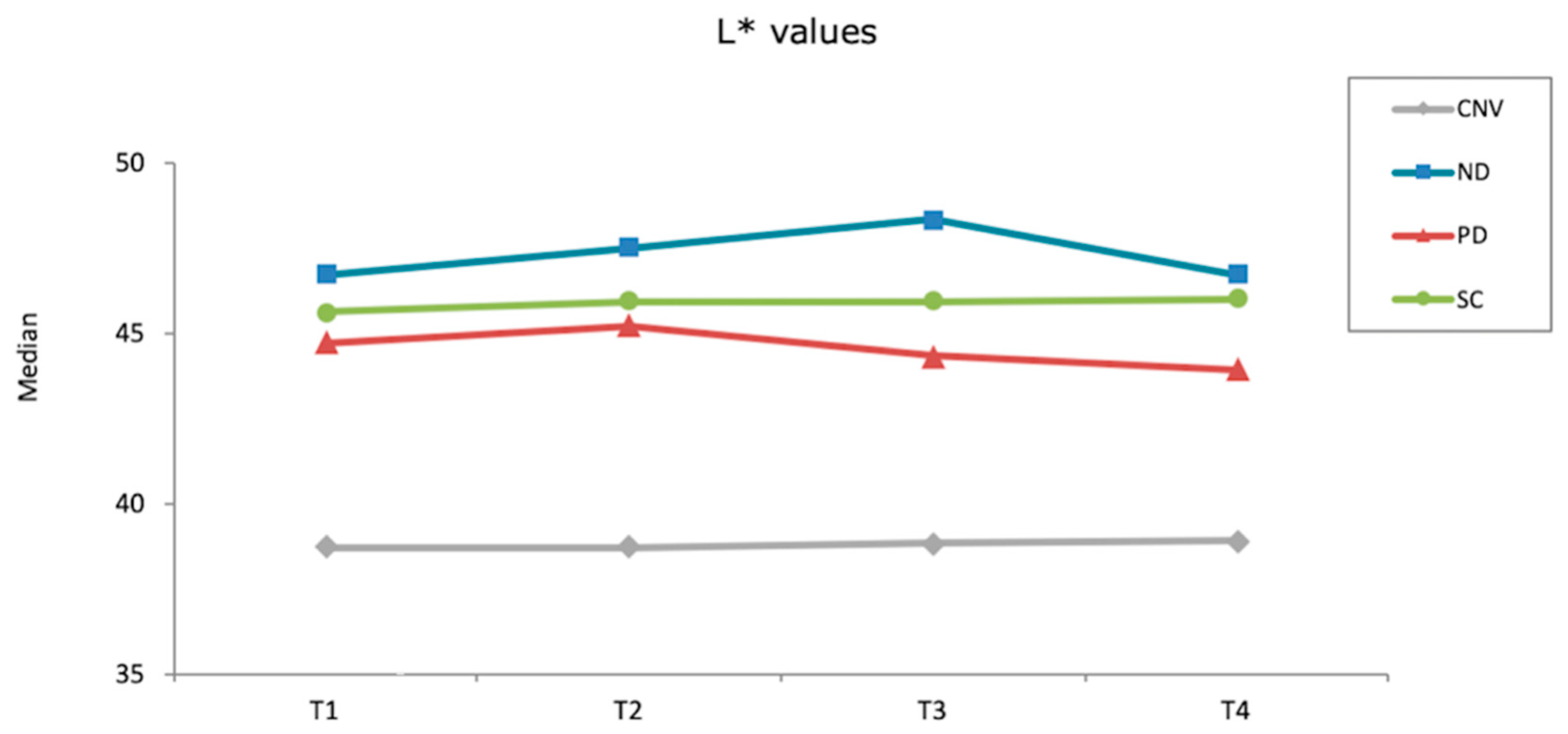
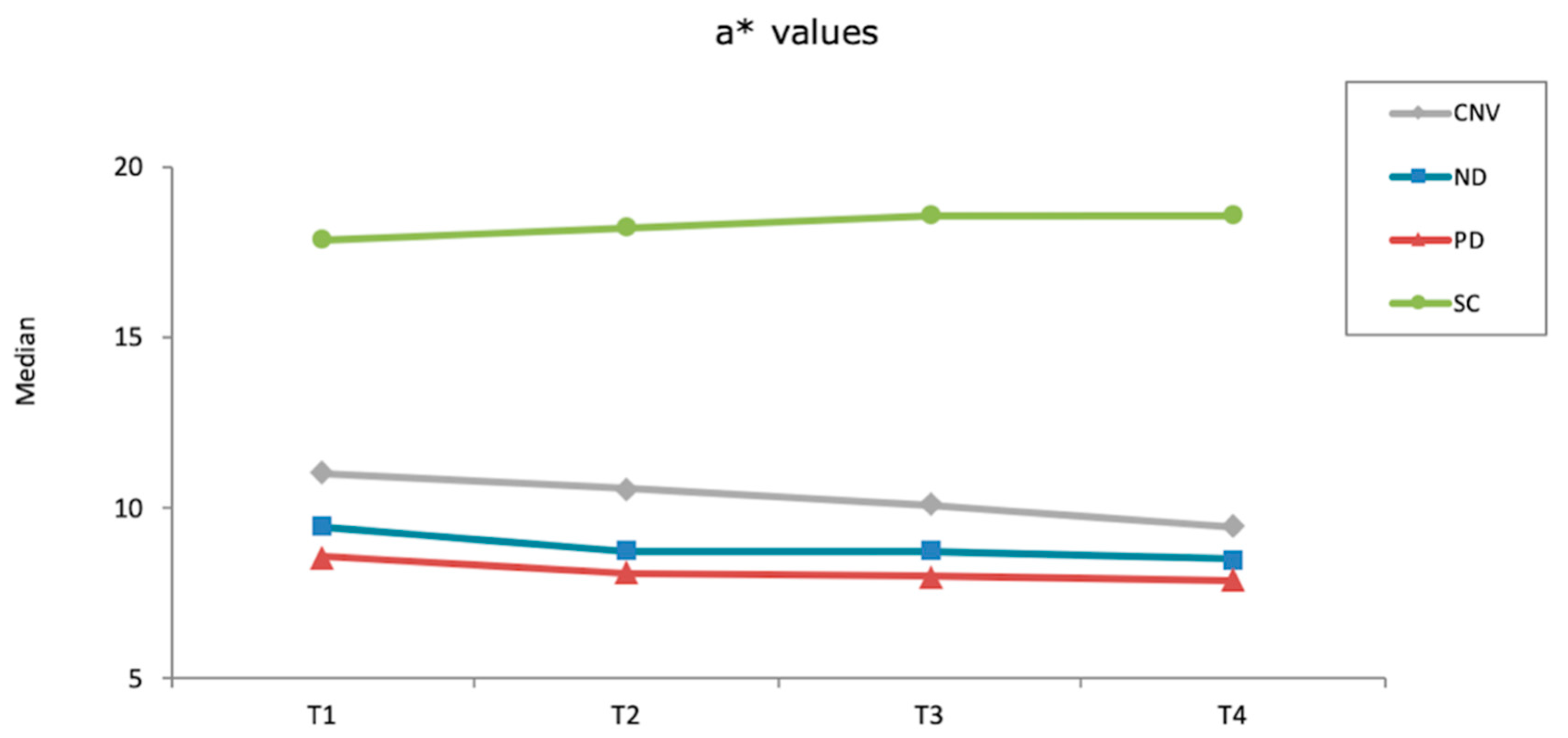
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Al-Dwairi, Z.; Al Haj Ebrahim, A.A.; Baba, N.Z. A comparison of the surface and mechanical properties of 3D printable denture-base resin material and conventional polymethylmethacrylate (PMMA). J. Prosthodont. 2022. [Google Scholar] [CrossRef]
- Alp, G.; Johnston, W.M.; Yilmaz, B. Optical properties and surface roughness of prepolymerized poly(methyl methacrylate) denture base materials. J. Prosthet. Dent. 2019, 121, 347–352. [Google Scholar] [CrossRef]
- Al-Dwairi, Z.N.; Tahboub, K.Y.; Baba, N.Z.; Goodacre, C.J.; Özcan, M. A comparison of the surface properties of CAD/CAM and conventional polymethylmethacrylate (PMMA). J. Prosthodont. 2019, 28, 452–457. [Google Scholar] [CrossRef]
- Gruber, S.; Kamnoedboon, P.; Özcan, M.; Srinivasan, M. CAD/CAM Complete denture resins: An ın vitro evaluation of color stability. J. Prosthodont. 2021, 30, 430–439. [Google Scholar] [CrossRef]
- Atalay, S.; Çakmak, G.; Fonseca, M.; Schimmel, M.; Yilmaz, B. Effect of thermocycling on the surface properties of CAD-CAM denture base materials after different surface treatments. J. Mech. Behav. Biomed. Mater. 2021, 121, 104646. [Google Scholar] [CrossRef]
- Neshandar Asli, H.; Rahimabadi, S.; Babaee Hemmati, Y.; Falahchai, M. Effect of different surface treatments on surface roughness and flexural strength of repaired 3D-printed denture base: An in vitro study. J. Prosthet. Dent. 2021, 126, 595.e1–595.e8. [Google Scholar] [CrossRef]
- Alfouzan, A.F.; Alotiabi, H.M.; Labban, N.; Al-Otaibi, H.N.; Al Taweel, S.M.; AlShehri, H.A. Color stability of 3D-printed denture resins: Effect of aging, mechanical brushing and immersion in staining medium. J. Adv. Prosthodont. 2021, 13, 160–171. [Google Scholar] [CrossRef]
- Chang, Y.H.; Lee, C.Y.; Hsu, M.S.; Du, J.K.; Chen, K.K.; Wu, J.H. Effect of toothbrush/dentifrice abrasion on weight variation, surface roughness, surface morphology and hardness of conventional and CAD/CAM denture base materials. Dent. Mater. J. 2021, 40, 220–227. [Google Scholar] [CrossRef]
- Sorgini, D.B.; da Silva-Lovato, C.H.; Muglia, V.A.; de Souza, R.F.; de Arruda, C.N.; Paranhos Hde, F. Adverse effects on PMMA caused by mechanical and combined methods of denture cleansing. Braz. Dent. J. 2015, 26, 292–296. [Google Scholar] [CrossRef]
- Pisani, M.X.; Bruhn, J.P.; Paranhos, H.F.; Silva-Lovato, C.H.; de Souza, R.F.; Panzeri, H. Evaluation of the abrasiveness of dentifrices for complete dentures. J. Prosthodont. 2010, 19, 369–373. [Google Scholar] [CrossRef]
- de Freitas Pontes, K.M.; de Holanda, J.C.; Fonteles, C.S.; Pontes Cde, B.; Lovato da Silva, C.H.; Paranhos Hde, F. Effect of toothbrushes and denture brushes on heat-polymerized acrylic resins. Gen. Dent. 2016, 64, 49–53. [Google Scholar]
- Shinawi, L.A. Effect of denture cleaning on abrasion resistance and surface topography of polymerized CAD CAM acrylic resin denture base. Electron. Physician. 2017, 9, 4281–4288. [Google Scholar] [CrossRef]
- Sorgini, D.B.; Silva-Lovato, C.H.; de Souza, R.F.; Davi, L.R.; Paranhos Hde, F. Abrasiveness of conventional and specific denture-cleansing dentifrices. Braz. Dent. J. 2012, 23, 154–159. [Google Scholar] [CrossRef]
- Alfouzan, A.F.; Alotiabi, H.M.; Labban, N.; Al-Otaibi, H.N.; Al Taweel, S.M.; AlShehri, H.A. Effect of aging and mechanical brushing on surface roughness of 3D printed denture resins: A profilometer and scanning electron microscopy analysis. Technol. Health Care 2022, 30, 161–173. [Google Scholar] [CrossRef]
- Gungor, H.; Gundogdu, M.; Yesil Duymus, Z. Investigation of the effect of different polishing techniques on the surface roughness of denture base and repair materials. J. Prosthet. Dent. 2014, 112, 1271–1277. [Google Scholar] [CrossRef]
- Bollen, C.M.; Papaioanno, W.; Van Eldere, J.; Schepers, E.; Quirynen, M.; van Steenberghe, D. The influence of abutment surface roughness on plaque accumulation and peri-implant mucositis. Clin. Oral Implants Res. 1996, 7, 201–211. [Google Scholar] [CrossRef]
- Nam, N.E.; Shin, S.H.; Lim, J.H.; Shim, J.S.; Kim, J.E. Effects of artificial tooth brushing and hydrothermal aging on the mechanical properties and color stability of dental 3D printed and CAD/CAM materials. Materials 2021, 14, 6270. [Google Scholar] [CrossRef]
- Dayan, C.; Guven, M.C.; Gencel, B.; Bural, C. A Comparison of the color stability of conventional and CAD/CAM polymethyl methacrylate denture base materials. Acta Stomatol. Croat. 2019, 53, 158–167. [Google Scholar]
- Ren, J.; Lin, H.; Huang, Q.; Zheng, G. Determining color difference thresholds in denture base acrylic resin. J. Prosthet. Dent. 2015, 114, 702–708. [Google Scholar]
- Sagsoz, N.P.; Yanıkoglu, N.; Ulu, H.; Bayındır, F. Color changes of polyamid and polymetyhl methacrylate denture base materials. Open J. Stomatol. 2014, 4, 489–496. [Google Scholar] [CrossRef]
- Gad, M.M.; Fouda, S.M.; Abualsaud, R.; Alshahrani, F.A.; Al-Thobity, A.M.; Khan, S.Q.; Akhtar, S.; Ateeq, I.S.; Helal, M.A.; Al-Harbi, F.A. Strength and surface properties of a 3D-printed denture base polymer. J. Prosthodont. 2022, 31, 412–418. [Google Scholar] [CrossRef]
- Arslan, M.; Murat, S.; Alp, G.; Zaimoglu, A. Evaluation of flexural strength and surface properties of prepolymerized CAD/CAM PMMA-based polymers used for digital 3D complete dentures. Int. J. Comput. Dent. 2018, 21, 31–40. [Google Scholar]
- Ayaz, E.A.; Bağış, B.; Turgut, S. Effects of thermal cycling on surface roughness, hardness and flexural strength of polymethylmethacrylate and polyamide denture base resins. J. Appl. Biomater. Funct. Mater. 2015, 13, e280–e286. [Google Scholar] [CrossRef]
- Di Fiore, A.; Meneghello, R.; Brun, P.; Rosso, S.; Gattazzo, A.; Stellini, E.; Yilmaz, B. Comparison of the flexural and surface properties of milled, 3D-printed, and heat polymerized PMMA resins for denture bases: An in vitro study. J. Prosthodont. Res. 2022, 66, 502–508. [Google Scholar] [CrossRef]
- Srinivasan, M.; Kalberer, N.; Kamnoedboon, P.; Mekki, M.; Durual, S.; Özcan, M.; Müller, F. CAD-CAM complete denture resins: An evaluation of biocompatibility, mechanical properties, and surface characteristics. J. Dent. 2021, 114, 103785. [Google Scholar] [CrossRef]
- Çakmak, G.; Donmez, M.B.; Akay, C.; Atalay, S.; de Paula, M.S.; Schimmel, M.; Yilmaz, B. Effect of simulated brushing and disinfection on the surface roughness and color stability of CAD-CAM denture base materials. J. Mech. Behav. Biomed. Mater. 2022, 134, 105390. [Google Scholar] [CrossRef]
- ISO-4287; Geometrical Product Specifications (GPS)—Surface Texture: Profile Method—Terms, Definitions and Surface Texture Parameters. International Organization for Standardization: Geneva, Switzerland, 1997. Available online: https://www.iso.org/standard/10132.html (accessed on 12 August 2022).
- Sahin, O.; Koroglu, A.; Dede, D.; Yilmaz, B. Effect of surface sealant agents on the surface roughness and color stability of denture base materials. J. Prosthet. Dent. 2016, 116, 610–616. [Google Scholar] [CrossRef]
- Flury, S.; Diebold, E.; Peutzfeldt, A.; Lussi, A. Effect of artificial toothbrushing and water storage on the surface roughness and micromechanical properties of tooth-colored CAD-CAM materials. J. Prosthet. Dent. 2017, 117, 767–774. [Google Scholar] [CrossRef]
- Goldstein, G.R.; Lerner, T. The effect of toothbrushing on a hybrid composite resin. J. Prosthet. Dent. 1991, 66, 498–500. [Google Scholar] [CrossRef]
- Turssi, C.P.; Hara, A.T.; de Magalhães, C.S.; Serra, M.C.; Rodrigues, A.L., Jr. Influence of storage regime prior to abrasion on surface topography of restorative materials. J. Biomed. Mater. Res. B Appl. Biomater. 2003, 65, 227–232. [Google Scholar] [CrossRef]
- Viana Í, E.L.; Weiss, G.S.; Sakae, L.O.; Niemeyer, S.H.; Borges, A.B.; Scaramucci, T. Activated charcoal toothpastes do not increase erosive tooth wear. J. Dent. 2021, 109, 103677. [Google Scholar] [CrossRef]
- Sulaiman, T.A.; Camino, R.N.; Cook, R.; Delgado, A.J.; Roulet, J.F.; Clark, W.A. Time-lasting ceramic stains and glaze: A toothbrush simulation study. J. Esthet. Restor. Dent. 2020, 32, 581–585. [Google Scholar] [CrossRef]
- Acar, O.; Yilmaz, B.; Altintas, S.H.; Chandrasekaran, I.; Johnston, W.M. Color stainability of CAD/CAM and nanocomposite resin materials. J. Prosthet. Dent. 2016, 115, 71–75. [Google Scholar] [CrossRef]
- Lee, Y.K. Comparison of CIELAB DeltaE(*) and CIEDE2000 color-differences after polymerization and thermocycling of resin composites. Dent. Mater. 2005, 21, 678–682. [Google Scholar] [CrossRef]
- Haynes, W. Bonferroni Correction. In Encyclopedia of Systems Biology; Dubitzky, W., Wolkenhauer, O., Cho, K.-H., Yokota, H., Eds.; Springer: New York, NY, USA, 2013; p. 154. [Google Scholar]
- Gale, M.S.; Darvell, B.W. Thermal cycling procedures for laboratory testing of dental restorations. J. Dent. 1999, 27, 89–99. [Google Scholar] [CrossRef]
- Lira, A.F.; Consani, R.L.; Mesquita, M.F.; Nóbilo, M.A.; Henriques, G.E. Effect of toothbrushing, chemical disinfection and thermocycling procedures on the surface microroughness of denture base acrylic resins. Gerodontology 2012, 29, e891–e897. [Google Scholar] [CrossRef]
- The NextDent Website. Available online: https://store.avadent.com/wp-content/uploads/2018/11/SDS_NextDent-Denture-3D_V2.0_20180122_EN.pdf (accessed on 25 May 2022).
- The Saremco Website. Available online: https://www.saremco.ch/wp-content/uploads/2020/09/MSDS-Denturetec-en_07-2020.pdf (accessed on 25 May 2022).

| Material | Type | Abbreviation | Manufacturer |
|---|---|---|---|
| NextDent Denture 3D+ | 3D-printed resin | ND | NextDent B.V., Soesterberg, The Netherlands |
| Denturetec | 3D-printed resin | SC | Saremco Dental AG, Rebstein, Switzerland |
| Polident d.o.o | Prepolymerized PMMA disk | PD | Polident, Volčja Draga, Slovenia |
| Promolux | Heat-polymerized acrylic resin | CNV | Merz Dental GmbH, Lütjenburg, Germany |
| Material | Before Polish | After Polish | After First Brushing Cycle | After Thermocycling | After Second Brushing Cycle |
|---|---|---|---|---|---|
| ND | 7.95 d (7.46–8.50) | 0.13 b (0.13–0.14) | 0.16 b (0.15–0.18) | 0.15 b (0.14–0.16) | 0.14 ab (0.14–0.17) |
| SC | 4.18 c (3.57–4.83) | 0.05 a (0.04–0.06) | 0.07 ab (0.06–0.11) | 0.06 a (0.05–0.06) | 0.06 a (0.05–0.09) |
| PD | 0.24 a (0.23–0.31) | 0.14 b (0.08–0.22) | 0.08 a (0.08–0.1) | 0.10 b (0.09–0.13) | 0.10 a (0.08–0.12) |
| CNV | 1.05 b (0.69–2.81) | 0.11 b (0.10–0.40) | 0.12 a (0.10–0.14) | 0.13 b (0.11–0.17) | 0.20 b (0.15–0.22) |
| Time Interval | ||||
|---|---|---|---|---|
| Material | After Polish- after First Brushing Cycle | After First Brushing Cycle- after Thermocycling | After Thermocycling- after Second Brushing Cycle | After Polish- after Second Brushing Cycle |
| ND | 1.36 Aa (1.13–1.59) | 2.10 Ab (1.83–2.43) | 1.38 Ab (1.10–1.96) | 2.83 Ac (2.57–2.93) |
| SC | 0.57 Aa (0.28–0.87) | 0.51 Aa (0.38–1.06) | 0.38 Aa (0.17–0.47) | 0.69 Aa (0.61–0.77) |
| PD | 0.71 Aa (0.56–2.07) | 0.83 Aa (0.45–1.71) | 0.55 Aa (0.45–0.66) | 0.90 Aa (0.77–1.38) |
| CNV | 0.70 Aa (0.52–1.05) | 0.68 Aa (0.52–0.78) | 0.62 Aa (0.45–0.81) | 1.62 Ab (1.28–1.91) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Çakmak, G.; Molinero-Mourelle, P.; De Paula, M.S.; Akay, C.; Cuellar, A.R.; Donmez, M.B.; Yilmaz, B. Surface Roughness and Color Stability of 3D-Printed Denture Base Materials after Simulated Brushing and Thermocycling. Materials 2022, 15, 6441. https://doi.org/10.3390/ma15186441
Çakmak G, Molinero-Mourelle P, De Paula MS, Akay C, Cuellar AR, Donmez MB, Yilmaz B. Surface Roughness and Color Stability of 3D-Printed Denture Base Materials after Simulated Brushing and Thermocycling. Materials. 2022; 15(18):6441. https://doi.org/10.3390/ma15186441
Chicago/Turabian StyleÇakmak, Gülce, Pedro Molinero-Mourelle, Marcella Silva De Paula, Canan Akay, Alfonso Rodriguez Cuellar, Mustafa Borga Donmez, and Burak Yilmaz. 2022. "Surface Roughness and Color Stability of 3D-Printed Denture Base Materials after Simulated Brushing and Thermocycling" Materials 15, no. 18: 6441. https://doi.org/10.3390/ma15186441
APA StyleÇakmak, G., Molinero-Mourelle, P., De Paula, M. S., Akay, C., Cuellar, A. R., Donmez, M. B., & Yilmaz, B. (2022). Surface Roughness and Color Stability of 3D-Printed Denture Base Materials after Simulated Brushing and Thermocycling. Materials, 15(18), 6441. https://doi.org/10.3390/ma15186441








