Human SMILE-Derived Stromal Lenticule Scaffold for Regenerative Therapy: Review and Perspectives
Abstract
:1. Introduction
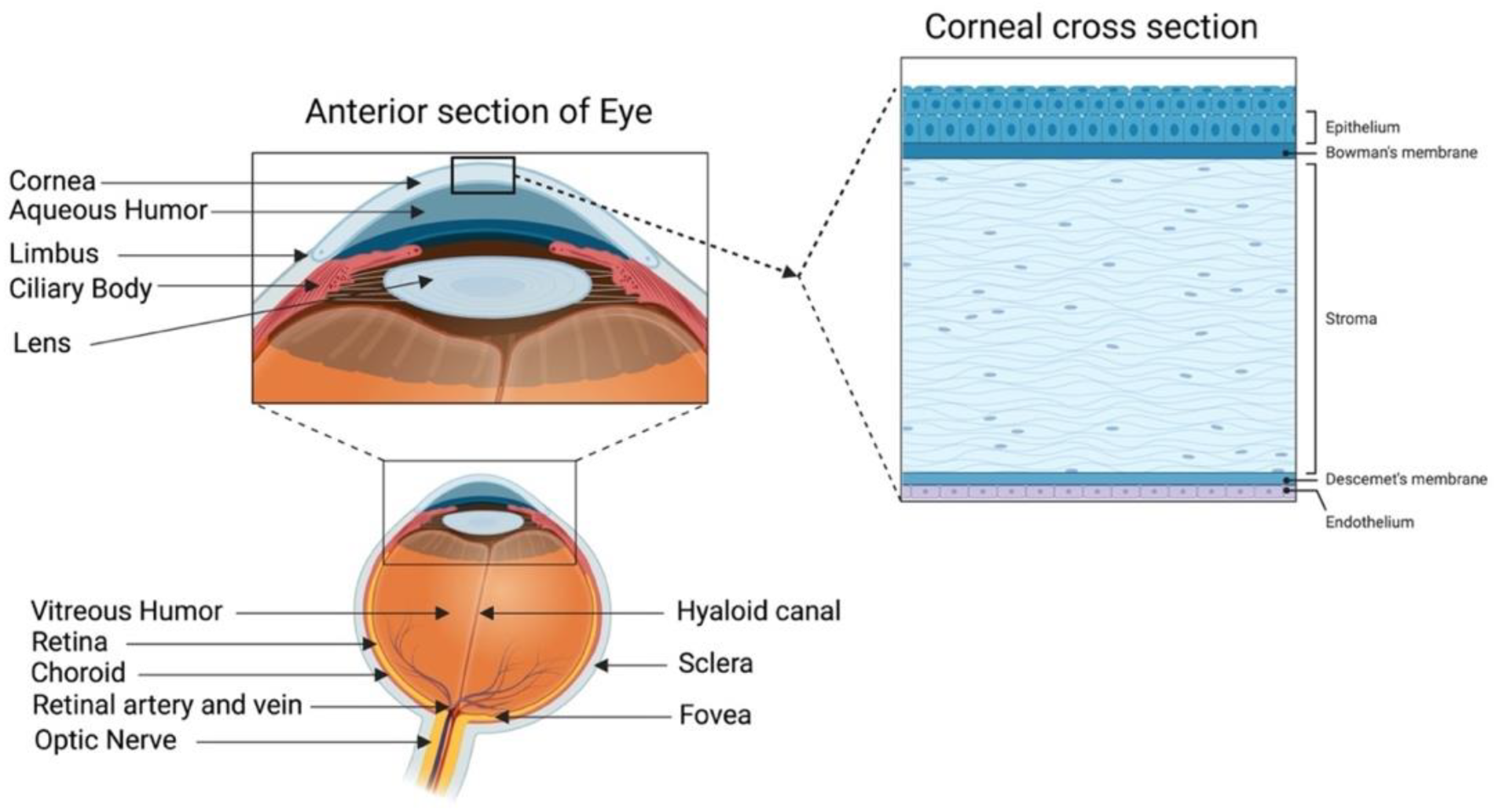
1.1. Human Cornea Anatomy, Composition and Cell Types
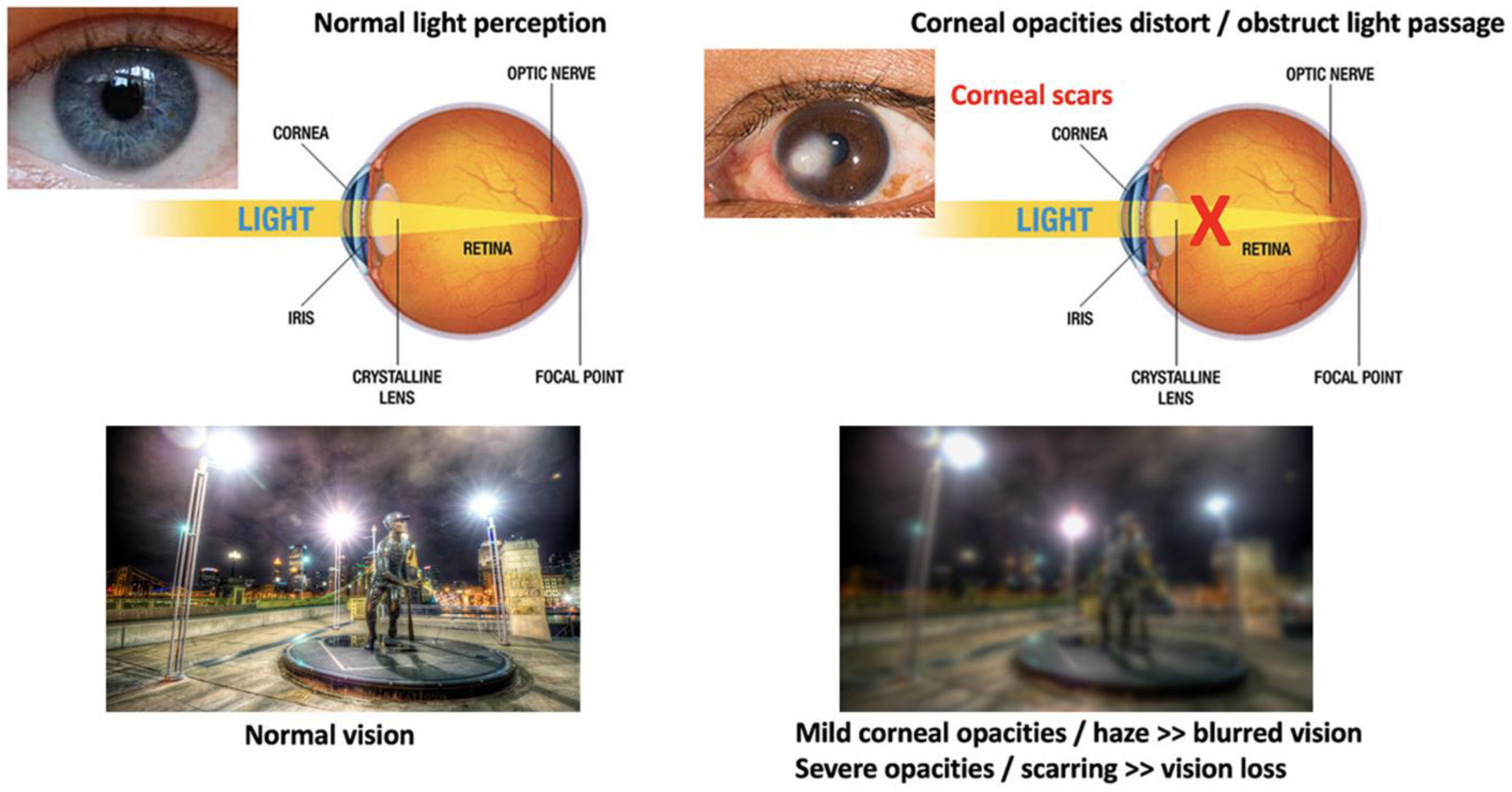
1.2. Corneal Blindness and Conventional Treatments with Tissue Grafting
1.3. Corneal Wound Healing and Scar Development
2. Corneal Regenerative Approach: Cell-Based vs. Scaffold-Based Strategies
2.1. Cell-Based Therapies
2.2. Scaffold-Based Cell Delivery Strategies
Decellularization of ECM Tissues for Scaffold-Based Engineering
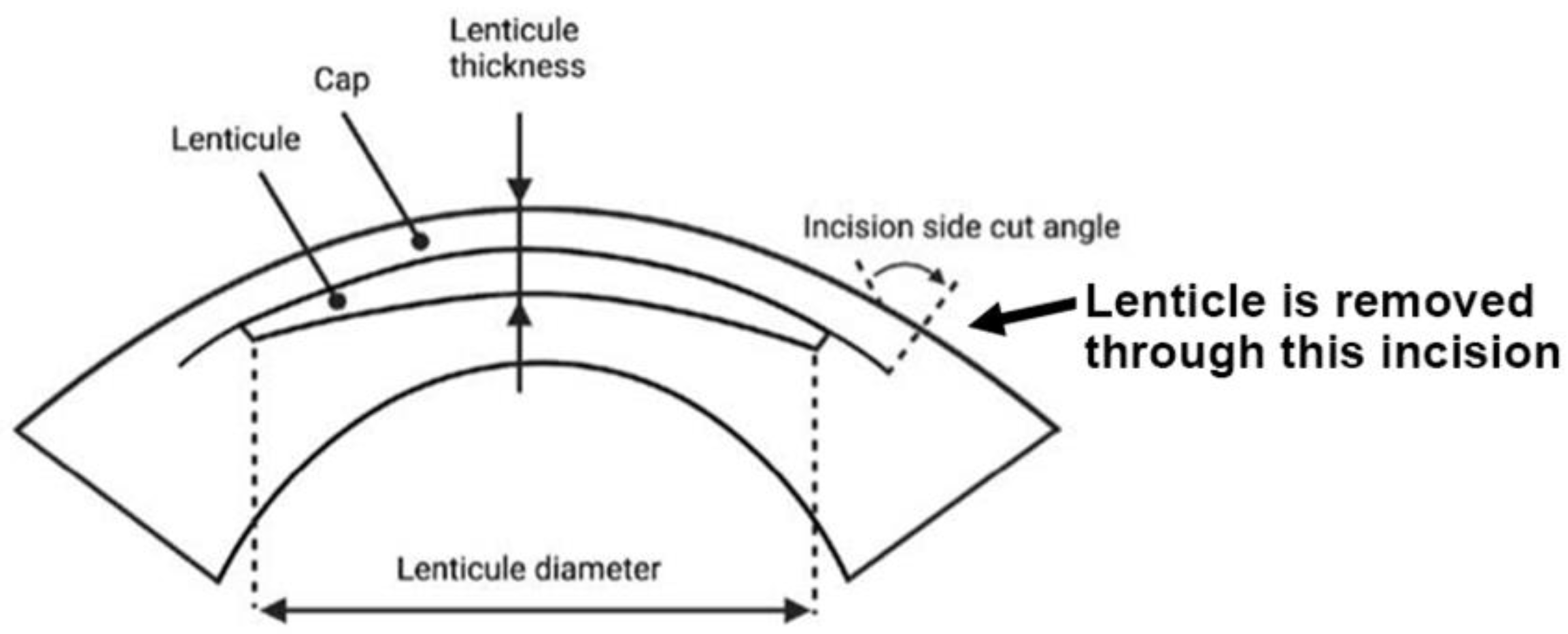
3. Stromal Lenticules from SMILE
3.1. Utilization of SMILE-Derived Stromal Lenticules
| Corneal Conditions | Lenticule Types | Procedure | Study Subjects | Conclusion | References |
|---|---|---|---|---|---|
| Presbyopia | Allogenic corneal inlay prepared from SMILE-derived lenticules | Presbyopic allogenic refractive lenticule (PEARL) inlay | 4 patients with emmetropia and presbyopia | It demonstrated the safety and efficacy of a PEARL corneal inlay for presbyopic correction. | [80,82] |
| Hyperopia | Autologous SMILE-derived lenticules | Lenticule implantation | 5 patients with 1 eye myopic and the other hyperopic | Implanting an autologous SMILE-derived lenticule for hyperopia correction was safe, effective, and stable. | [83] |
| Allogenic SMILE-derived lenticule | Femtosecond laser-assisted keyhole endokeratophakia | A 23-year-old aphakic patient | Treatment corrected hyperopia to 50% of the intended correction. | [75] | |
| Keratoconus | Allogenic SMILE-derived lenticules | Femtosecond laser-assisted stromal lenticule implantation combined with accelerated collagen cross-linking | 6 patients with progressive keratoconus | Combined lenticule implantation and collagen cross-linking is a feasible option to treat low to moderate keratoconus. | [84] |
| Corneal dystrophy | Allogenic SMILE-derived lenticules | Epikeratophakia combined with photo-therapeutic keratectomy | 6 patients with recurrent corneal dystrophy | A feasible treatment with improvement in vision and a good safety profile. | [85] |
| Micro-perforations | Allogenic SMILE-derived lenticule patch graft | Glued lenticule patch graft transplantation | 7 eyes of 7 patients | A safe, feasible, and inexpensive surgical option. | [86] |
3.2. SMILE Lenticule Storage and Customization
3.3. Decellularized SMILE Lenticules in Corneal Bioengineering
3.4. Current Obstacles to the Use of SMILE Lenticules for Clinical Applications
- No standard methods with high reproducibility are available to customize lenticules prior to implantation in patients that require specific settings. Although several studies have shown some degree of modification to have the appropriate thickness for refractive correction or to be mechanically strengthened for ectasia treatment or for the elimination of immune-prone biomolecules for allogenic lenticules by decellularization [68,89,91], standard methods that are widely acceptable to the clinical community are yet to be established.
- Lenticule storage and biobanking systems are still being developed in a few countries, such as Singapore (https://www.straitstimes.com/singapore/health/singapore-launches-first-bank-in-asia-for-eye-surgery-patients-to-freeze-piece-of, accessed on 3 July 2022) [87,95]. A structured regulatory and organizational framework for lenticule processing and banking is important for the successful operation, standardization, and quality assurance of lenticule products and for safe and effective treatments for patients.
4. Applications of ECM Scaffolds from Other Sources in Tissue Engineering
4.1. Recellularization on Stromal Scaffolds and Potential Applications
4.2. Tissue Regeneration with ECM Scaffolds
4.2.1. Cell-Scaffold Interactions Guide Tissue Formation
4.2.2. ECM-Scaffold-Mediated Tissue Regeneration
4.3. ECM Scaffolds in Drug Delivery and Tissue Engineering
4.3.1. Scaffold-Mediated Drug Delivery
4.3.2. Nanomaterials and ECM Scaffolds for Drug Delivery
4.3.3. Nanoparticles Incorporated in ECM Scaffolds
4.4. Growth Factor Binding to ECM Scaffolds and Applications
ECM-Scaffold-Mediated Delivery of Growth Factors
5. Perspective on Translating Existing Knowledge of ECM-Based Scaffold Engineering to the SMILE-Derived Lenticule Scaffold for Potential Therapeutic Applications
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Patel, S.; Alió, J.L.; Pérez-Santonja, J.J. Refractive Index Change in Bovine and Human Corneal Stroma before and after LASIK: A Study of Untreated and Re-treated Corneas Implicating Stromal Hydration. Investig. Ophthalmol. Vis. Sci. 2004, 45, 3523–3530. [Google Scholar] [CrossRef]
- Eghrari, A.O.; Riazuddin, S.A.; Gottsch, J.D. Overview of the Cornea: Structure, Function, and Development. Prog. Mol. Biol. Transl. Sci. 2015, 134, 7–23. [Google Scholar]
- Sridhar, M.S. Anatomy of cornea and ocular surface. Indian J. Ophthalmol. 2018, 66, 190–194. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.E. Bowman’s layer in the cornea—Structure and function and regeneration. Exp. Eye Res. 2020, 195, 108033. [Google Scholar] [CrossRef] [PubMed]
- DelMonte, D.W.; Kim, T. Anatomy and physiology of the cornea. J. Cataract. Refract. Surg. 2011, 37, 588–598. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Anderson, M.C.; Liu, C.Y. The role of corneal stroma: A potential nutritional source for the cornea. J. Nat. Sci. 2017, 3, e428. [Google Scholar]
- Chen, S.; Mienaltowski, M.J.; Birk, D.E. Regulation of corneal stroma extracellular matrix assembly. Exp. Eye Res. 2015, 133, 69–80. [Google Scholar] [CrossRef] [Green Version]
- Kabosova, A.; Azar, D.T.; Bannikov, G.A.; Campbell, K.P.; Durbeej, M.; Ghohestani, R.F.; Jones, J.C.R.; Kenney, M.C.; Koch, M.; Ninomiya, Y.; et al. Compositional Differences between Infant and Adult Human Corneal Basement Membranes. Investig. Ophthalmol. Vis. Sci. 2007, 48, 4989–4999. [Google Scholar] [CrossRef] [Green Version]
- Jacobsen, I.E.; Jensen, O.A.; Prause, J.U. Structure and composition of Bowman’s membrane. Study by frozen resin cracking. Acta Ophthalmol. Cph. 1984, 62, 39–53. [Google Scholar] [CrossRef]
- Bonanno, J.A. Identity and regulation of ion transport mechanisms in the corneal endothelium. Prog. Retin. Eye Res. 2003, 22, 69–94. [Google Scholar] [CrossRef]
- Gain, P.; Jullienne, R.; He, Z.; Aldossary, M.; Acquart, S.; Cognasse, F.; Thuret, G. Global Survey of Corneal Transplantation and Eye Banking. JAMA Ophthalmol. 2016, 134, 167–173. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guérin, L.-P.; Le-Bel, G.; Desjardins, P.; Couture, C.; Gillard, E.; Boisselier, É.; Bazin, R.; Germain, L.; Guérin, S.L. The Human Tissue-Engineered Cornea (hTEC): Recent Progress. Int. J. Mol. Sci. 2021, 22, 1291. [Google Scholar] [CrossRef] [PubMed]
- Price, M.O.; Feng, M.T.; Price, F.W.J. Endothelial Keratoplasty Update 2020. Cornea 2021, 40, 541–547. [Google Scholar] [CrossRef] [PubMed]
- Price, M.O.; Mehta, J.S.; Jurkunas, U.V.; Price, F.W. Corneal endothelial dysfunction: Evolving understanding and treatment options. Prog. Retin. Eye Res. 2021, 82, 100904. [Google Scholar] [CrossRef] [PubMed]
- Feizi, S.; Zare, M. Current approaches for management of postpenetrating keratoplasty astigmatism. J. Ophthalmol. 2011, 2011, 708736. [Google Scholar] [CrossRef] [Green Version]
- Ljubimov, A.V.; Saghizadeh, M. Progress in corneal wound healing. Prog. Retin. Eye Res. 2015, 49, 17–45. [Google Scholar] [CrossRef] [Green Version]
- Yam, G.H.F.; Riau, A.K.; Funderburgh, M.L.; Mehta, J.S.; Jhanji, V. Keratocyte biology. Exp. Eye Res. 2020, 196, 108062. [Google Scholar] [CrossRef]
- Wilson, S.E.; Mohan, R.R.; Mohan, R.R.; Ambrósio, R.; Hong, J.; Lee, J. The Corneal Wound Healing Response: Cytokine-mediated Interaction of the Epithelium, Stroma, and Inflammatory Cells. Prog. Retin. Eye Res. 2001, 20, 625–637. [Google Scholar] [CrossRef]
- Ruan, Y.; Jiang, S.; Musayeva, A.; Pfeiffer, N.; Gericke, A. Corneal Epithelial Stem Cells—Physiology, Pathophysiology and Therapeutic Options. Cells 2021, 10, 2302. [Google Scholar] [CrossRef]
- Saghizadeh, M.; Kramerov, A.A.; Svendsen, C.N.; Ljubimov, A.V. Concise review: Stem cells for corneal wound healing. Stem Cells 2017, 35, 2105–2114. [Google Scholar] [CrossRef] [Green Version]
- Català, P.; Thuret, G.; Skottman, H.; Mehta, J.S.; Parekh, M.; Dhubhghaill, S.N.; Collin, R.W.J.; Nuijts, R.M.M.A.; Ferrari, S.; LaPointe, V.L.S. Approaches for corneal endothelium regenerative medicine. Prog. Retin. Eye Res. 2022, 87, 100987. [Google Scholar] [CrossRef] [PubMed]
- Vercammen, H.; Miron, A.; Oellerich, S.; Melles, G.R.; Dhubhghaill, S.N.; Koppen, C.; van den Bogerd, B. Corneal endothelial wound healing: Understanding the regenerative capacity of the innermost layer of the cornea. Transl. Res. 2022. [Google Scholar] [CrossRef] [PubMed]
- Warejcka, D.J.; Narayan, M.; Twining, S.S. Maspin increases extracellular plasminogen activator activity associated with corneal fibroblasts and myofibroblasts. Exp. Eye Res. 2011, 93, 618–627. [Google Scholar] [CrossRef] [Green Version]
- Nishida, T.; Ueda, A.; Otori, T.; Fujita, H. Long-term storage of endocytosed latex beads in keratocytes in vivo. Cornea 1991, 10, 532–535. [Google Scholar] [CrossRef]
- Funderburgh, J.L.; Mann, M.M.; Funderburgh, M.L. Keratocyte Phenotype Mediates Proteoglycan Structure: A role for fibroblasts in corneal fibrosis. J. Biol. Chem. 2003, 278, 45629–45637. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ma, J.; Zhou, D.; Fan, M.; Wang, H.; Huang, C.; Zhang, Z.; Wu, Y.; Li, W.; Chen, Y.; Liu, Z. Keratocytes Create Stromal Spaces to Promote Corneal Neovascularization Via MMP13 Expression. Investig. Ophthalmol. Vis. Sci. 2014, 55, 6691–6703. [Google Scholar] [CrossRef] [Green Version]
- Nosrati, H.; Alizadeh, Z.; Nosrati, A.; Ashrafi-Dehkordi, K.; Banitalebi-Dehkordi, M.; Sanami, S.; Khodaei, M. Stem cell-based therapeutic strategies for corneal epithelium regeneration. Tissue Cell 2021, 68, 101470. [Google Scholar] [CrossRef]
- Kobayashi, T.; Kan, K.; Nishida, K.; Yamato, M.; Okano, T. Corneal regeneration by transplantation of corneal epithelial cell sheets fabricated with automated cell culture system in rabbit model. Biomaterials 2013, 34, 9010–9017. [Google Scholar] [CrossRef]
- Nosrati, H.; Abpeikar, Z.; Mahmoudian, Z.G.; Zafari, M.; Majidi, J.; Alizadeh, A.; Moradi, L.; Asadpour, S. Corneal epithelium tissue engineering: Recent advances in regeneration and replacement of corneal surface. Regen. Med. 2020, 15, 2029–2044. [Google Scholar] [CrossRef]
- Bandeira, F.; Goh, T.W.; Setiawan, M.; Yam, G.H.; Mehta, J.S. Cellular therapy of corneal epithelial defect by adipose mesenchymal stem cell-derived epithelial progenitors. Stem Cell Res. Therapy 2020, 11, 14. [Google Scholar] [CrossRef] [Green Version]
- Kumar, A.; Yun, H.; Funderburgh, M.L.; Du, Y. Regenerative therapy for the Cornea. Prog. Retin. Eye Res. 2021, 87, 101011. [Google Scholar] [CrossRef]
- Basu, S.; Hertsenberg, A.J.; Funderburgh, M.L.; Burrow, M.K.; Mann, M.M.; Du, Y.; Lathrop, K.L.; Syed-Picard, F.N.; Adams, S.M.; Birk, D.E. Human limbal biopsy–derived stromal stem cells prevent corneal scarring. Sci. Transl. Med. 2014, 6, ra172–ra266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jhanji, V.; Santra, M.; Riau, A.K.; Geary, M.L.; Yang, T.; Rubin, E.; Yusoff, N.Z.B.M.; Dhaliwal, D.K.; Mehta, J.S.; Yam, G.H.-F. Combined therapy using human corneal stromal stem cells and quiescent keratocytes to prevent corneal scarring after injury. Int. J. Mol. Sci. 2022, 23, 6980. [Google Scholar] [CrossRef] [PubMed]
- Kinoshita, S.; Koizumi, N.; Ueno, M.; Okumura, N.; Imai, K.; Tanaka, H.; Yamamoto, Y.; Nakamura, T.; Inatomi, T.; Bush, J. Injection of cultured cells with a ROCK inhibitor for bullous keratopathy. N. Engl. J. Med. 2018, 378, 995–1003. [Google Scholar] [CrossRef] [PubMed]
- Ying, L.Y.; Qiu, W.Y.; Wang, B.H.; Zhou, P.; Zhang, B.; Yao, Y.F. Corneal endothelial regeneration in human eyes using endothelium-free grafts. BMC Ophthalmol. 2022, 22, 32. [Google Scholar] [CrossRef] [PubMed]
- Okumura, N.; Koizumi, N. Regeneration of the corneal endothelium. Curr. Eye Res. 2020, 45, 303–312. [Google Scholar] [CrossRef] [PubMed]
- Mahdavi, S.S.; Abdekhodaie, M.J.; Mashayekhan, S.; Baradaran-Rafii, A.; Djalilian, A.R. Bioengineering Approaches for Corneal Regenerative Medicine. Tissue Eng. Regen. Med. 2020, 17, 567–593. [Google Scholar] [CrossRef]
- El Zarif, M.; Alió, J.L.; Alió del Barrio, J.L.; De Miguel, M.P.; Abdul Jawad, K.; Makdissy, N. Corneal Stromal Regeneration: A Review of Human Clinical Studies in Keratoconus Treatment. Front. Med. 2021, 8, 650724. [Google Scholar] [CrossRef]
- De Miguel, M.P.; Fuentes-Julián, S.; Blázquez-Martínez, A.; Pascual, C.Y.; Aller, M.A.; Arias, J.; Arnalich-Montiel, F. Immunosuppressive properties of mesenchymal stem cells: Advances and applications. Curr. Mol. Med. 2012, 12, 574–591. [Google Scholar] [CrossRef]
- Kao, W.W.Y.; Coulson-Thomas, V.J. Cell Therapy of Corneal Diseases. Cornea 2016, 35 (Suppl. 1), S9–S19. [Google Scholar] [CrossRef] [Green Version]
- De Pieri, A.; Rochev, Y.; Zeugolis, D.I. Scaffold-free cell-based tissue engineering therapies: Advances, shortfalls and forecast. Regen. Med. 2021, 6, 18. [Google Scholar] [CrossRef] [PubMed]
- Rossetti, T.; Nicholls, F.; Modo, M. Intracerebral Cell Implantation: Preparation and Characterization of Cell Suspensions. Cell Transplant. 2016, 25, 645–664. [Google Scholar] [CrossRef] [Green Version]
- Amer, M.H.; Rose, F.R.A.J.; Shakesheff, K.M.; Modo, M.; White, L.J. Translational considerations in injectable cell-based therapeutics for neurological applications: Concepts, progress and challenges. Regen. Med. 2017, 2, 23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Becker, A.; Riet, I.V. Homing and migration of mesenchymal stromal cells: How to improve the efficacy of cell therapy? World J. Stem Cells 2016, 8, 73–87. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, A. Mesenchymal stem cell delivery routes and fate. Int. J. Stem Cells 2008, 1, 1–7. [Google Scholar] [CrossRef]
- García-Gareta, E.; Abduldaiem, Y.; Sawadkar, P.; Kyriakidis, C.; Lali, F.; Greco, K.V. Decellularised scaffolds: Just a framework? Current knowledge and future directions. J. Tissue Eng. 2020, 11, 2041731420942903. [Google Scholar] [CrossRef]
- Li, Y.; Xiao, Y.; Liu, C. The Horizon of Materiobiology: A Perspective on Material-Guided Cell Behaviors and Tissue Engineering. Chem. Rev. 2017, 117, 4376–4421. [Google Scholar] [CrossRef]
- Gu, C.; Feng, J.; Waqas, A.; Deng, Y.; Zhang, Y.; Chen, W.; Long, J.; Huang, S.; Chen, L. Technological Advances of 3D Scaffold-Based Stem Cell/Exosome Therapy in Tissues and Organs. Front. Cell Dev. Biol. 2021, 9, 709204. [Google Scholar] [CrossRef]
- Bourget, J.M.; Guillemette, M.; Veres, T.; Auger, F.A.; Germain, L. Alignment of cells and extracellular matrix within tissue-engineered substitutes. In Advances in Biomaterials Science and Biomedical Applications; IntechOpen: London, UK, 2013; pp. 365–390. [Google Scholar]
- Jester, J.V.; Moller-Pedersen, T.; Huang, J.; Sax, C.M.; Kays, W.T.; Cavangh, H.D.; Petroll, W.M.; Piatigorsky, J. The cellular basis of corneal transparency: Evidence for ‘corneal crystallins’. J. Cell Sci. 1999, 112, 613–622. [Google Scholar] [CrossRef]
- Lewis, G.; Shaw, K.M. Modeling the tensile behavior of human Achilles tendon. Bio-Med. Mater. Eng. 1997, 7, 231–244. [Google Scholar] [CrossRef]
- Lynch, H.A.; Johannessen, W.; Wu, J.P.; Jawa, A.; Elliott, D.M. Effect of fiber orientation and strain rate on the nonlinear uniaxial tensile material properties of tendon. J. Biomech. Eng. 2003, 125, 726–731. [Google Scholar] [CrossRef]
- Jeffery, A.; Blunn, G.; Archer, C.; Bentley, G. Three-dimensional collagen architecture in bovine articular cartilage. J. Bone Jt. Surg. Br. Vol. 1991, 73, 795–801. [Google Scholar] [CrossRef] [PubMed]
- Paine, M.L.; Snead, M.L. Protein interactions during assembly of the enamel organic extracellular matrix. J. Bone Miner. Res. 1997, 12, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Evans, M.J.; Cox, R.A.; Shami, S.G.; Wilson, B.; Plopper, C.G. The role of basal cells in attachment of columnar cells to the basal lamina of the trachea. Am. J. Respir. Cell Mol. Biol. 1989, 1, 463–469. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.; Jin, X. The development of tissue engineering corneal scaffold: Which one the history will choose? Ann. Eye Sci. 2018, 3, 6. [Google Scholar] [CrossRef]
- Mobaraki, M.; Abbasi, R.; Vandchali, S.O.; Ghaffari, M.; Moztarzadeh, F.; Mozafari, M. Corneal Repair and Regeneration: Current Concepts and Future Directions. Front. Bioeng. Biotechnol. 2019, 7, 135. [Google Scholar] [CrossRef] [Green Version]
- Crapo, P.M.; Gilbert, T.W.; Badylak, S.F. An overview of tissue and whole organ decellularization processes. Biomaterials 2011, 32, 3233–3243. [Google Scholar] [CrossRef] [Green Version]
- Wilson, S.L.; Sidney, L.E.; Dunphy, S.E.; Rose, J.B.; Hopkinson, A. Keeping an eye on decellularized corneas: A review of methods, characterization and applications. J. Funct. Biomater. 2013, 4, 114–161. [Google Scholar] [CrossRef] [Green Version]
- Liao, J.; Xu, B.; Zhang, R.; Fan, Y.; Xie, H.; Li, X. Applications of decellularized materials in tissue engineering: Advantages, drawbacks and current improvements, and future perspectives. J. Mater. Chem. B 2020, 8, 10023–10049. [Google Scholar] [CrossRef]
- Unnikrishnan, K.; Thomas, L.V.; Kumar, R.M.R. Advancement of Scaffold-Based 3D Cellular Models in Cancer Tissue Engineering: An Update. Front. Oncol. 2021, 11, 733652. [Google Scholar] [CrossRef]
- Gilpin, A.; Yang, Y. Decellularization Strategies for Regenerative Medicine: From Processing Techniques to Applications. Biomed. Res. Int. 2017, 2017, 9831534. [Google Scholar] [CrossRef] [Green Version]
- Riau, A.K.; Liu, Y.C.; Yam, G.H.; Mehta, J.S. Stromal keratophakia: Corneal inlay implantation. Prog. Retin. Eye Res. 2020, 75, 100780. [Google Scholar] [CrossRef]
- Shafiq, M.A.; Gemeinhart, R.A.; Yue, B.Y.; Djalilian, A.R. Decellularized human cornea for reconstructing the corneal epithelium and anterior stroma. Tissue Eng. Part C Method. 2012, 18, 340–348. [Google Scholar] [CrossRef] [PubMed]
- Shafiq, M.A.; Milani, B.Y.; Djalilian, A.R. In vivo evaluation of a decellularized limbal graft for limbal reconstruction. Int. J. Tissue Eng. 2014, 2014, 754245. [Google Scholar] [CrossRef] [Green Version]
- Choi, J.S.; Williams, J.K.; Greven, M.; Walter, K.A.; Laber, P.W.; Khang, G.; Soker, S. Bioengineering endothelialized neo-corneas using donor-derived corneal endothelial cells and decellularized corneal stroma. Biomaterials 2010, 31, 6738–6745. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Niu, G.; San Choi, J.; Giegengack, M.; Atala, A.; Soker, S. Bioengineered multilayered human corneas from discarded human corneal tissue. Biomed. Mater. 2015, 10, 035012. [Google Scholar] [CrossRef]
- Yam, G.H.-F.; Yusoff, N.Z.B.M.; Goh, T.-W.; Setiawan, M.; Lee, X.-W.; Liu, Y.-C.; Mehta, J.S. Decellularization of human stromal refractive lenticules for corneal tissue engineering. Sci. Rep. 2016, 6, 26339. [Google Scholar] [CrossRef] [Green Version]
- He, Z.; Forest, F.; Bernard, A.; Gauthier, A.-S.; Montard, R.; Peoc’h, M.; Jumelle, C.; Courrier, E.; Perrache, C.; Gain, P. Cutting and decellularization of multiple corneal stromal lamellae for the bioengineering of endothelial grafts. Investig. Ophthalmol. Vis. Sci. 2016, 57, 6639–6651. [Google Scholar] [CrossRef]
- Del Barrio, J.L.A.; El Zarif, M.; Azaar, A.; Makdissy, N.; Khalil, C.; Harb, W.; el Achkar, I.; Jawad, Z.A.; de Miguel, M.P.; Alió, J.L. Corneal stroma enhancement with decellularized stromal laminas with or without stem cell recellularization for advanced keratoconus. Am. J. Ophthalmol. 2018, 186, 47–58. [Google Scholar] [CrossRef]
- Fernández-Pérez, J.; Ahearne, M. Decellularization and recellularization of cornea: Progress towards a donor alternative. Methods 2020, 171, 86–96. [Google Scholar] [CrossRef]
- Liu, Y.C.; Mehta, J.S. Small Incision Lenticule Extraction (SMILE). In Cornea, 4th ed.; Krachmer, J.H., Holland, E.J., Eds.; Elsevier Mosby: Philadelphia, PA, USA, 2015. [Google Scholar]
- Zhang, Y.; Shen, Q.; Jia, Y.; Zhou, D.; Zhou, J. Clinical Outcomes of SMILE and FS-LASIK Used to Treat Myopia: A Meta-analysis. J. Refract. Surg. 2016, 32, 256–265. [Google Scholar] [CrossRef] [Green Version]
- Siedlecki, J.; Luft, N.; Mayer, W.J.; Siedlecki, M.; Kook, D.; Meyer, B.; Bechmann, M.; Wiltfang, R.; Priglinger, S.G.; Dirisamer, M. CIRCLE enhancement after myopic SMILE. J. Refract. Surg. 2018, 34, 304–309. [Google Scholar] [CrossRef]
- Pradhan, K.R.; Reinstein, D.Z.; Carp, G.I.; Archer, T.J.; Gobbe, M.; Gurung, R. Femtosecond laser-assisted keyhole endokeratophakia: Correction of hyperopia by implantation of an allogeneic lenticule obtained by SMILE from a myopic donor. J. Refract. Surg. 2013, 29, 777–782. [Google Scholar] [CrossRef] [PubMed]
- Moshirfar, M.; Shah, T.J.; Masud, M.; Fanning, T.; Linn, S.H.; Ronquillo, Y.; Hoopes, P.C.S. A Modified Small-Incision Lenticule Intrastromal Keratoplasty (sLIKE) for the Correction of High Hyperopia: A Description of a New Surgical Technique and Comparison to Lenticule Intrastromal Keratoplasty (LIKE). Med. Hypothesis Discov. Innov. Ophthalmol. 2018, 7, 48–56. [Google Scholar] [PubMed]
- Doroodgar, F.; Jabbarvand, M.; Niazi, S.; Karimian, F.; Niazi, F.; Sanginabadi, A.; Ghoreishi, M.; Alinia, C.; Hashemi, H.; Alió, J.L. Customized stromal lenticule implantation for keratoconus. J. Refract. Surg. 2020, 36, 786–794. [Google Scholar] [CrossRef] [PubMed]
- Mastropasqua, L.; Nubile, M.; Salgari, N.; Mastropasqua, R. Femtosecond laser–assisted stromal lenticule addition keratoplasty for the treatment of advanced keratoconus: A preliminary study. J. Refract. Surg. 2018, 34, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Zhao, F.; Li, M.; Knorz, M.C.; Zhou, X. Treatment of Corneal Ectasia by Implantation of an Allogenic Corneal Lenticule. J. Refract. Surg. 2018, 34, 347–350. [Google Scholar] [CrossRef]
- Liu, Y.-C.; Teo, E.P.W.; Ang, H.P.; Seah, X.Y.; Lwin, N.C.; Yam, G.H.; Mehta, J.S. Biological corneal inlay for presbyopia derived from small incision lenticule extraction (SMILE). Sci. Rep. 2018, 8, 1831. [Google Scholar] [CrossRef] [Green Version]
- Dana, M.R.; Qian, Y.; Hamrah, P. Twenty-five Year Panorama of Corneal Immunology: Emerging Concepts in the Immunopathogenesis of Microbial Keratitis, Peripheral Ulcerative Keratitis, and Corneal Transplant Rejection. Cornea 2000, 19, 625–643. [Google Scholar] [CrossRef]
- Jacob, S.; Kumar, D.A.; Agarwal, A.; Agarwal, A.; Aravind, R.; Saijimol, A.I. Preliminary Evidence of Successful Near Vision Enhancement With a New Technique: Presbyopic Allogenic Refractive Lenticule (PEARL) Corneal Inlay Using a SMILE Lenticule. J. Refract. Surg. 2017, 33, 224–229. [Google Scholar] [CrossRef] [Green Version]
- Sun, L.; Yao, P.; Li, M.; Shen, Y.; Zhao, J.; Zhou, X. The safety and predictability of implanting autologous lenticule obtained by SMILE for hyperopia. J. Refract. Surg. 2015, 31, 374–379. [Google Scholar] [CrossRef] [PubMed]
- Ganesh, S.; Brar, S. Femtosecond Intrastromal Lenticular Implantation Combined With Accelerated Collagen Cross-Linking for the Treatment of Keratoconus—Initial Clinical Result in 6 Eyes. Cornea 2015, 34, 1331–1339. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Miao, H.; Han, T.; Shen, Y.; Zhao, Y.; Sun, L.; Zhou, X. A Pilot Study of SMILE for Hyperopia: Corneal Morphology and Surface Characteristics of Concave Lenticules in Human Donor Eyes. J. Refract. Surg. 2016, 32, 713–716. [Google Scholar] [CrossRef]
- Bhandari, V.; Ganesh, S.; Brar, S.; Pandey, R. Application of the SMILE-Derived Glued Lenticule Patch Graft in Microperforations and Partial-Thickness Corneal Defects. Cornea 2016, 35, 408–412. [Google Scholar] [CrossRef]
- Liu, Y.C.; Williams, G.P.; George, B.L.; Soh, Y.Q.; Seah, X.Y.; Peh, G.S.L.; Yam, G.H.F.; Mehta, J.S. Corneal lenticule storage before reimplantation. Mol. Vis. 2017, 23, 753–764. [Google Scholar]
- Ganesh, S.; Brar, S.; Rao, P.A. Cryopreservation of extracted corneal lenticules after small incision lenticule extraction for potential use in human subjects. Cornea 2014, 33, 1355–1362. [Google Scholar] [CrossRef] [Green Version]
- Damgaard, I.B.; Riau, A.K.; Liu, Y.C.; Tey, M.L.; Yam, G.H.-F.; Mehta, J.S. Reshaping and Customization of SMILE-Derived Biological Lenticules for Intrastromal Implantation. Investig. Ophthalmol. Vis. Sci. 2018, 59, 2555–2563. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bandeira, F.; Yam, G.H.-F.; Liu, Y.C.; Devarajan, K.; Mehta, J.S. Three-Dimensional Neurite Characterization of Small Incision Lenticule Extraction Derived Lenticules. Investig. Ophthalmol. Vis. Sci. 2019, 60, 4408–4415. [Google Scholar] [CrossRef] [Green Version]
- Yam, G.H.-F.; Bandeira, F.; Liu, Y.C.; Devarajan, K.; Yusoff, N.Z.B.M.; Htoon, H.M.; Mehta, J.S. Effect of corneal stromal lenticule customization on neurite distribution and excitatory property. J. Adv. Res. 2022, 38, 275–284. [Google Scholar] [CrossRef]
- Chen, Y.; Yin, Y.W.; Zhao, Y.; Wu, X.-Y.; Young, K.; Song, W.-T.; Xia, X.; Wen, D. Differentiation of human embryonic stem cells derived mesenchymal stem cells into corneal epithelial cells after being seeded on decellularized SMILE-derived lenticules. Int. J. Ophthalmol. 2019, 12, 717–724. [Google Scholar]
- Qin, S.; Zheng, S.; Qi, B.; Guo, R.; Hou, G. Decellularized Human Stromal Lenticules Combine with Corneal Epithelial-Like Cells: A New Resource for Corneal Tissue Engineering. Stem Cells Int. 2019, 2019, 4252514. [Google Scholar] [CrossRef]
- Yin, Y.; Lu, Y.; Xiang, A.; Fu, Y.; Zhao, Y.; Li, Y.; Hu, T.; Du, K.; Hu, S.; Fu, Q.; et al. Comparison of the optical quality after SMILE and FS-LASIK for high myopia by OQAS and iTrace analyzer: A one-year retrospective study. BMC Ophthalmol. 2021, 21, 292. [Google Scholar] [CrossRef] [PubMed]
- Riau, A.K.; Boey, K.P.; Binte, M.; Yusoff, N.Z.; Goh, T.-W.; Yam, G.H.; Tang, K.F.; Phua, C.S.H.; Chen, H.; Chiew, Y.F.; et al. Experiment-Based Validation of Corneal Lenticule Banking in a Health Authority-Licensed Facility. Tissue Eng. Part A 2022, 28, 69–83. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Chen, J.; Zhang, Z.; Lou, K.; Zhang, Q.; Wang, S.; Ni, J.; Liu, W.; Fan, S.; Lin, X. Current advances in the development of natural meniscus scaffolds: Innovative approaches to decellularization and recellularization. Cell Tissue Res. 2017, 370, 41–52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmed, E.; Saleh, T.; Xu, M. Recellularization of Native Tissue Derived Acellular Scaffolds with Mesenchymal Stem Cells. Cells 2021, 10, 1787. [Google Scholar] [CrossRef] [PubMed]
- Diao, J.-M.; Pang, X.; Qiu, Y.; Miao, Y.; Yu, M.-M.; Fan, T.-J. Construction of a human corneal stromal equivalent with non-transfected human corneal stromal cells and acellular porcine corneal stromata. Exp. Eye Res. 2015, 132, 216–224. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; Gan, Y.; Wang, H.; Xu, Y.; Song, L.; Wang, L.; Ouyang, B.; Zhou, Q. A substance exchanger-based bioreactor culture of pig discs for studying the immature nucleus pulposus. Artif. Organs 2017, 41, E308–E319. [Google Scholar] [CrossRef]
- Gonzalez-Andrades, M.; de la Cruz Cardona, J.; Ionescu, A.M.; Campos, A.; del Mar Perez, M.; Alaminos, M. Generation of bioengineered corneas with decellularized xenografts and human keratocytes. Investig. Ophthalmol. Vis. Sci. 2011, 52, 215–222. [Google Scholar] [CrossRef] [Green Version]
- Pang, K.; Du, L.; Wu, X. A rabbit anterior cornea replacement derived from acellular porcine cornea matrix, epithelial cells and keratocytes. Biomaterials 2010, 31, 7257–7265. [Google Scholar] [CrossRef]
- Kargar-Abarghouei, E.; Vojdani, Z.; Hassanpour, A.; Alaee, S.; Talaei-Khozani, T. Characterization, recellularization, and transplantation of rat decellularized testis scaffold with bone marrow-derived mesenchymal stem cells. Stem Cell Res. Ther. 2018, 9, 324. [Google Scholar] [CrossRef] [Green Version]
- Akbay, E.; Onur, M.A. Investigation of survival and migration potential of differentiated cardiomyocytes transplanted with decellularized heart scaffold. J. Biomed. Mater. Res. Part A 2019, 107, 561–570. [Google Scholar] [CrossRef] [PubMed]
- Folkman, J.; Hochberg, M. Self-regulation of growth in three dimensions. J. Exp. Med. 1973, 138, 745–753. [Google Scholar] [CrossRef] [PubMed]
- Broekelmann, T.J.; Bodmer, N.K.; Mecham, R.P. Identification of the growth factor-binding sequence in the extracellular matrix protein MAGP-1. J. Biol. Chem. 2020, 295, 2687–2697. [Google Scholar] [CrossRef] [PubMed]
- Santra, M.; Sharma, M.; Katoch, D.; Jain, S.; Saikia, U.N.; Dogra, M.R.; Luthra-Guptasarma, M. Induction of posterior vitreous detachment (PVD) by non-enzymatic reagents targeting vitreous collagen liquefaction as well as vitreoretinal adhesion. Sci. Rep. 2020, 10, 8250. [Google Scholar] [CrossRef]
- Schwartz, M.A. Integrin signaling revisited. Trends Cell Biol. 2001, 11, 466–470. [Google Scholar] [CrossRef]
- Hynes, R.O. The extracellular matrix: Not just pretty fibrils. Science 2009, 326, 1216–1219. [Google Scholar] [CrossRef] [Green Version]
- Wang, Z.; Wang, Z.; Lu, W.W.; Zhen, W.; Yang, D.; Peng, S. Novel biomaterial strategies for controlled growth factor delivery for biomedical applications. Asia Mater. 2017, 9, e435. [Google Scholar] [CrossRef]
- Dong, C.; Qiao, F.; Chen, G.; Lv, Y. Demineralized and decellularized bone extracellular matrix-incorporated electrospun nanofibrous scaffold for bone regeneration. J. Mater. Chem. B 2021, 9, 6881–6894. [Google Scholar] [CrossRef]
- Wang, M.; Li, B.; Liu, Y.; Tang, L.; Zhang, Y.; Xie, Q. A Novel Bionic Extracellular Matrix Polymer Scaffold Enhanced by Calcium Silicate for Bone Tissue Engineering. ACS Omega 2021, 6, 35727–35737. [Google Scholar] [CrossRef]
- Tavelli, L.; McGuire, M.K.; Zucchelli, G.; Rasperini, G.; Feinberg, S.E.; Wang, H.L.; Giannobile, W.V. Extracellular matrix-based scaffolding technologies for periodontal and peri-implant soft tissue regeneration. J. Periodontol. 2020, 91, 17–25. [Google Scholar] [CrossRef]
- Lih, E.; Park, W.; Park, K.W.; Chun, S.Y.; Kim, H.; Joung, Y.K.; Kwon, T.G.; Hubbell, J.A.; Han, D.K. A bioinspired scaffold with anti-inflammatory magnesium hydroxide and decellularized extracellular matrix for renal tissue regeneration. ACS Cent. Sci. 2019, 5, 458–467. [Google Scholar] [CrossRef] [PubMed]
- Hussey, G.S.; Cramer, M.C.; Badylak, S.F. Extracellular Matrix Bioscaffolds for Building Gastrointestinal Tissue. Cell. Mol. Gastroenterol. Hepatol. 2017, 5, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.S.; Sun, X.; Lee, J.-H.; Kim, H.-W.; Fu, X.; Leong, K.W. Advanced drug delivery systems and artificial skin grafts for skin wound healing. Adv. Drug Deliv. Rev. 2019, 146, 209–239. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Hoshi, R.; Chen, S.; Yi, J.; Duan, C.; Galiano, R.D.; Zhang, H.F.; Ameer, G.A. Sustained release of stromal cell derived factor-1 from an antioxidant thermoresponsive hydrogel enhances dermal wound healing in diabetes. J. Control. Release 2016, 238, 114–122. [Google Scholar] [CrossRef]
- Xiao, J.; Chen, S.; Yi, J.; Zhang, H.; Ameer, G.A. A Cooperative Copper Metal-Organic Framework-Hydrogel System Improves Wound Healing in Diabetes. Adv. Funct. Mater. 2017, 27, 1604872. [Google Scholar] [CrossRef]
- Monaghan, M.; Browne, S.; Schenke-Layland, K.; Pandit, A. A collagen-based scaffold delivering exogenous microrna-29B to modulate extracellular matrix remodeling. Mol. Ther. 2014, 22, 786–796. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, S.N.; Kim, J.K.; Suh, H. Evaluation of antibiotic-loaded collagen-hyaluronic acid matrix as a skin substitute. Biomaterials 2004, 25, 3689–3698. [Google Scholar] [CrossRef]
- Byun, E.; Lee, H. Enhanced loading efficiency and sustained release of doxorubicin from hyaluronic acid/graphene oxide composite hydrogels by a mussel-inspired catecholamine. J. Nanosci. Nanotechnol. 2014, 14, 7395–7401. [Google Scholar] [CrossRef]
- Heo, R.; Park, J.-S.; Jang, H.J.; Kim, S.-H.; Shin, J.M.; Suh, Y.D.; Jeong, J.H.; Jo, D.-G.; Park, J.H. Hyaluronan nanoparticles bearing γ-secretase inhibitor: In vivo therapeutic effects on rheumatoid arthritis. J. Control. Release 2014, 192, 295–300. [Google Scholar] [CrossRef]
- Dreher, M.R.; Raucher, D.; Balu, N.; Colvin, O.M.; Ludeman, S.M.; Chilkoti, A. Evaluation of an elastin-like polypeptide—Doxorubicin conjugate for cancer therapy. J. Control. Release 2003, 91, 31–43. [Google Scholar] [CrossRef]
- Atefyekta, S.; Pihl, M.; Lindsay, C.; Heilshorn, S.C.; Andersson, M. Antibiofilm elastin-like polypeptide coatings: Functionality, stability, and selectivity. Acta Biomater. 2019, 83, 245–256. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.S.; Choi, S.H.; Yoo, H.S. Coaxial electrospun nanofibers for treatment of diabetic ulcers with binary release of multiple growth factors. J. Mater. Chem. 2011, 21, 5258–5267. [Google Scholar] [CrossRef]
- Lai, H.J.; Kuan, C.H.; Wu, H.C.; Tsai, J.C.; Chen, T.M.; Hsieh, D.J.; Wang, T.-W. Tailored design of electrospun composite nanofibers with staged release of multiple angiogenic growth factors for chronic wound healing. Acta Biomater. 2014, 10, 4156–4166. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Zheng, W.; Zhang, J.; Guan, D.; Yang, Z.; Kong, D.; Zhao, Q. Enzyme-controllable delivery of nitric oxide from a molecular hydrogel. Chem. Comm. 2013, 49, 9173–9175. [Google Scholar] [CrossRef]
- Zhou, J.; Wang, M.; Ying, H.; Su, D.; Zhang, H.; Lu, G.; Chen, J. Extracellular Matrix Component Shelled Nanoparticles as Dual Enzyme-Responsive Drug Delivery Vehicles for Cancer Therapy. ACS Biomater. Sci. Eng. 2018, 4, 2404–2411. [Google Scholar] [CrossRef]
- Monteiro, N.; Martins, A.; Reis, R.L.; Neves, N.M. Nanoparticle-based bioactive agent release systems for bone and cartilage tissue engineering. Regen. Ther. 2015, 1, 109–118. [Google Scholar] [CrossRef] [Green Version]
- Mijanović, O.; Pylaev, T.; Nikitkina, A.; Artyukhova, M.; Branković, A.; Peshkova, M.; Bikmulina, P.; Turk, B.; Bolevich, S.; Avetisov, S.; et al. Tissue Engineering Meets Nanotechnology: Molecular Mechanism Modulations in Cornea Regeneration. Micromachines 2021, 12, 1336. [Google Scholar] [CrossRef]
- Jiang, Y.; Krishnan, N.; Heo, J.; Fang, R.H.; Zhang, L. Nanoparticle-hydrogel superstructures for biomedical applications. J. Control. Release 2020, 324, 505–521. [Google Scholar] [CrossRef]
- Pillay, S.; Pillay, V.; Choonara, Y.E.; Naidoo, D.; Khan, R.A.; du Toit, L.C.; Ndesendo, V.M.K.; Modi, G.; Danckwerts, M.P.; Iyuke, S.E. Design, biometric simulation and optimization of a nano-enabled scaffold device for enhanced delivery of dopamine to the brain. Int. J. Pharm. 2009, 382, 277–290. [Google Scholar] [CrossRef]
- Bhosale, U.V.; Devi, V.K.; Jain, N. Formulation and Optimization of Mucoadhesive Nanodrug Delivery System of Acyclovir. J. Young Pharm. 2011, 3, 275–283. [Google Scholar] [CrossRef] [Green Version]
- Honda, M.; Asai, T.; Oku, N.; Araki, Y.; Tanaka, M.; Ebihara, N. Liposomes and nanotechnology in drug development: Focus on ocular targets. Int. J. Nanomed. 2013, 8, 495. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vichare, R.; Garner, I.; Paulson, R.J.; Tzekov, R.; Sahiner, N.; Panguluri, S.K.; Mohapatra, S.; Mohapatra, S.S.; Ayyala, R.; Sneed, K.B.; et al. Biofabrication of Chitosan-Based Nanomedicines and Its Potential Use for Translational Ophthalmic Applications. Appl. Sci. 2020, 10, 4189. [Google Scholar] [CrossRef]
- Chang, M.C.; Kuo, Y.J.; Hung, K.H.; Peng, C.L.; Chen, K.Y.; Yeh, L.K. Liposomal dexamethasone–moxifloxacin nanoparticle combinations with collagen/gelatin/alginate hydrogel for corneal infection treatment and wound healing. Biomed. Mater. 2020, 15, 055022. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Lian, Y.; Fang, Q.; Liu, L.; Zhang, J.; Li, J. Hyaluronic-acid-modified lipid-polymer hybrid nanoparticles as an efficient ocular delivery platform for moxifloxacin hydrochloride. Int. J. Biol. Macromol. 2018, 116, 1026–1036. [Google Scholar] [CrossRef] [PubMed]
- Gupta, H.; Aqil, M.; Khar, R.K.; Ali, A.; Bhatnagar, A.; Mittal, G. Sparfloxacin-loaded PLGA nanoparticles for sustained ocular drug delivery. Nanomed 2010, 6, 324–333. [Google Scholar] [CrossRef]
- Lieleg, O.; Schmoller, K.; Claessens, M.M.A.E.; Bausch, A.R. Cytoskeletal polymer networks: Viscoelastic properties are determined by the microscopic interaction potential of cross-links. Biophys. J. 2009, 96, 4725–4732. [Google Scholar] [CrossRef] [Green Version]
- Stylianopoulos, T.; Poh, M.Z.; Insin, N.; Bawendi, M.G.; Fukumura, D.; Munn, L.L.; Jain, R.K. Diffusion of particles in the extracellular matrix: The effect of repulsive electrostatic interactions. Biophys. J. 2010, 99, 1342–1349. [Google Scholar] [CrossRef] [Green Version]
- Balakrishnan, S.; Bhat, F.; Raja Singh, P.; Mukherjee, S.; Elumalai, P.; Das, S.; Patra, C.R.; Arunakaran, J. Gold nanoparticle–conjugated quercetin inhibits epithelial–mesenchymal transition, angiogenesis and invasiveness via EGFR/VEGFR-2-mediated pathway in breast cancer. Cell Prolif. 2016, 49, 678–697. [Google Scholar] [CrossRef]
- Smith, S.E.; Snider, C.L.; Gilley, D.R.; Grant, D.N.; Sherman, S.L.; Ulery, B.D.; Grant, D.A.; Grant, S.A. Homogenized porcine extracellular matrix derived injectable tissue construct with gold nanoparticles for musculoskeletal tissue engineering applications. J. Biomater. Nanobiotechnol. 2017, 8, 125. [Google Scholar] [CrossRef] [Green Version]
- Cho, W.-K.; Kang, S.; Choi, H.; Rho, C.R. Topically administered gold nanoparticles inhibit experimental corneal neovascularization in mice. Cornea 2015, 34, 456–459. [Google Scholar] [CrossRef]
- Tandon, A.; Sharma, A.; Rodier, J.T.; Klibanov, A.M.; Rieger, F.G.; Mohan, R.R. BMP7 gene transfer via gold nanoparticles into stroma inhibits corneal fibrosis in vivo. PLoS ONE 2013, 8, e66434. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elkhoury, K.; Russell, C.S.; Sanchez-Gonzalez, L.; Mostafavi, A.; Williams, T.J.; Kahn, C.; Peppas, N.A.; Arab-Tehrany, E.; Tamayol, A. Soft-Nanoparticle functionalization of natural hydrogels for tissue engineering applications. Adv. Healthc. Mater. 2019, 8, 1900506. [Google Scholar] [CrossRef] [PubMed]
- Ahearne, M.; Fernández-Pérez, J.; Masterton, S.; Madden, P.W.; Bhattacharjee, P. Designing scaffolds for corneal regeneration. Adv. Healthc. Mater. 2020, 30, 1908996. [Google Scholar] [CrossRef] [Green Version]
- Cheng, K.; Kisaalita, W.S. Exploring cellular adhesion and differentiation in a micro-/nano-hybrid polymer scaffold. Biotechnol. Prog. 2010, 26, 838–846. [Google Scholar] [CrossRef] [PubMed]
- Somasuntharam, I.; Yehl, K.; Carroll, S.L.; Maxwell, J.T.; Martinez, M.D.; Che, P.L.; Brown, M.E.; Salaita, K.; Davis, M.E. Knockdown of TNF-α by DNAzyme gold nanoparticles as an anti-inflammatory therapy for myocardial infarction. Biomaterials 2016, 83, 12–22. [Google Scholar] [CrossRef] [Green Version]
- Kadner, K.; Dobner, S.; Franz, T.; Bezuidenhout, D.; Sirry, M.S.; Zilla, P.; Davies, N.H. The beneficial effects of deferred delivery on the efficiency of hydrogel therapy post myocardial infarction. Biomaterials 2012, 33, 2060–2066. [Google Scholar] [CrossRef]
- Dong, Y.; Hong, M.; Dai, R.; Wu, H.; Zhu, P. Engineered bioactive nanoparticles incorporated biofunctionalized ECM/silk proteins based cardiac patches combined with MSCs for the repair of myocardial infarction: In vitro and in vivo evaluations. Sci. Total Environ. 2020, 707, 135976. [Google Scholar] [CrossRef] [PubMed]
- Tayalia, P.; Mooney, D.J. Controlled growth factor delivery for tissue engineering. Adv. Mater. 2009, 21, 3269–3285. [Google Scholar] [CrossRef]
- Barrientos, S.; Stojadinovic, O.; Golinko, M.S.; Brem, H.; Tomic-Canic, M. Growth factors and cytokines in wound healing. Wound Repair Regen. 2008, 16, 585–601. [Google Scholar] [CrossRef]
- Yancopoulos, G.D.; Davis, S.; Gale, N.W.; Rudge, J.S.; Wiegand, S.J.; Holash, J. Vascular-specific growth factors and blood vessel formation. Nature 2000, 407, 242–248. [Google Scholar] [CrossRef]
- Martino, M.M.; Briquez, P.S.; Maruyama, K.; Hubbell, J.A. Extracellular matrix-inspired growth factor delivery systems for bone regeneration. Adv. Drug Deliv. Rev. 2015, 94, 41–52. [Google Scholar] [CrossRef] [PubMed]
- Fei, Y.; Gronowicz, G.; MHurley, M. Fibroblast growth factor-2, bone homeostasis and fracture repair. Curr. Pharm. Des. 2013, 19, 3354–3363. [Google Scholar] [CrossRef] [PubMed]
- Hollinger, J.O.; Hart, C.E.; Hirsch, S.N.; Lynch, S.; Friedlaender, G.E. Recombinant human platelet-derived growth factor: Biology and clinical applications. J. Bone Jt. Surg. 2008, 90 (Suppl. 1), 48–54. [Google Scholar] [CrossRef] [PubMed]
- Niu, Y.; Li, Q.; Ding, Y.; Dong, L.; Wang, C. Engineered delivery strategies for enhanced control of growth factor activities in wound healing. Adv. Drug Delivery Rev. 2019, 146, 190–208. [Google Scholar] [CrossRef] [PubMed]
- Edelman, E.R.; Nugent, M.A.; Karnovsky, M.J. Perivascular and intravenous administration of basic fibroblast growth factor: Vascular and solid organ deposition. Proc. Natl. Acad. Sci. USA 1993, 90, 1513–1517. [Google Scholar] [CrossRef] [Green Version]
- Lazarous, D.F.; Shou, M.; Scheinowitz, M.; Hodge, E.; Thirumurti, V.; Kitsiou, A.N.; Stiber, J.A.; Lobo, A.D.; Hunsberger, S.; Guetta, E. Comparative effects of basic fibroblast growth factor and vascular endothelial growth factor on coronary collateral development and the arterial response to injury. Circulation 1996, 94, 1074–1082. [Google Scholar] [CrossRef]
- Carragee, E.J.; Chu, G.; Rohatgi, R.; Hurwitz, E.L.; Weiner, B.K.; Yoon, S.T.; Comer, G.; Kopjar, B. Cancer risk after use of recombinant bone morphogenetic protein-2 for spinal arthrodesis. J. Bone Jt. Surg. Am. 2013, 95, 1537–1545. [Google Scholar] [CrossRef] [Green Version]
- Upton, Z.; Cuttle, L.; Noble, A.; Kempf, M.; Topping, G.; Malda, J.; Xie, Y.; Mill, J.; Harkin, D.G.; Kravchuk, O.; et al. Vitronectin: Growth factor complexes hold potential as a wound therapy approach. J. Investig. Dermatol. 2008, 128, 1535–1544. [Google Scholar] [CrossRef]
- Martino, M.M.; Tortelli, F.; Mochizuki, M.; Traub, S.; Ben-David, D.; Kuhn, G.A.; Müller, R.; Livne, E.; Eming, S.A.; Hubbell, J.A. Engineering the growth factor microenvironment with fibronectin domains to promote wound and bone tissue healing. Sci. Transl. Med. 2011, 3, 100ra89. [Google Scholar] [CrossRef] [Green Version]
- Seif-Naraghi, S.B.; Horn, D.; Schup-Magoffin, P.J.; Christman, K.L. Injectable extracellular matrix derived hydrogel provides a platform for enhanced retention and delivery of a heparin-binding growth factor. Acta Biomater. 2012, 8, 3695–3703. [Google Scholar] [CrossRef] [Green Version]
- Gresham, R.C.H.; Bahney, C.S.; Leach, J.K. Growth factor delivery using extracellular matrix-mimicking substrates for musculoskeletal tissue engineering and repair. Bioact. Mater. 2021, 6, 1945–1956. [Google Scholar] [CrossRef]
- Zhu, J.; Clark, R.A.F. Fibronectin at select sites binds multiple growth factors and enhances their activity: Expansion of the collaborative ECM-GF paradigm. J. Investig. Dermatol. 2014, 134, 895–901. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghosh, K.; Ren, X.-D.; Shu, X.Z.; Prestwich, G.D.; Clark, R.A. Fibronectin functional domains coupled to hyaluronan stimulate adult human dermal fibroblast responses critical for wound healing. Tissue Eng. 2006, 12, 601–613. [Google Scholar] [CrossRef] [PubMed]
- Wilgus, T.A. Growth factor—ECM interactions regulate wound repair. Adv. Wound Care 2012, 1, 249–254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ivaska, J.; Heino, J. Cooperation between Integrins and Growth Factor Receptors in Signaling and Endocytosis. Annu. Rev. Cell Dev. Biolo. 2011, 27, 291–320. [Google Scholar] [CrossRef] [PubMed]
- Macri, L.; Silverstein, D.; Clark, R.A. Growth factor binding to the pericellular matrix and its importance in tissue engineering. Adv. Drug Deliv. Rev. 2007, 59, 1366–1381. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.; Silva, E.A.; Mooney, D.J. Growth factor delivery-based tissue engineering: General approaches and a review of recent developments. J. R. Soc. Interface 2011, 8, 153–170. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Briquez, P.; Hubbell, J.; Martino, M. Extracellular Matrix-Inspired Growth Factor Delivery Systems for Skin Wound Healing. Adv. Wound Care 2015, 4, 150127064149004. [Google Scholar] [CrossRef] [Green Version]
- Oliveira, É.R.; Nie, L.; Podstawczyk, D.; Allahbakhsh, A.; Ratnayake, J.; Brasil, D.L.; Shavandi, A. Advances in growth factor delivery for bone tissue engineering. Int. J. Mol. Sci. 2021, 22, 903. [Google Scholar] [CrossRef]
- Roth, S.P.; Brehm, W.; Groß, C.; Scheibe, P.; Schubert, S.; Burk, J. Transforming Growth Factor Beta 3-Loaded Decellularized Equine Tendon Matrix for Orthopedic Tissue Engineering. Int. J. Mol. Sci. 2019, 20, 5474. [Google Scholar] [CrossRef] [Green Version]
- Swindle, C.S.; Tran, K.T.; Johnson, T.D.; Banerjee, P.; Mayes, A.M.; Griffith, L.; Wells, A. Epidermal growth factor (EGF)-like repeats of human tenascin-C as ligands for EGF receptor. J. Cell Biol. 2001, 154, 459–468. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Somanath, P.R.; Malinin, N.L.; Byzova, T.V. Cooperation between integrin alphavbeta3 and VEGFR2 in angiogenesis. Angiogenesis 2009, 12, 177–185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Masson-Gadais, B.; Houle, F.; Laferrière, J.; Huot, J. Integrin alphavbeta3, requirement for VEGFR2-mediated activation of SAPK2/p38 and for Hsp90-dependent phosphorylation of focal adhesion kinase in endothelial cells activated by VEGF. Cell Stress Chaperones 2003, 8, 37–52. [Google Scholar] [CrossRef]
- Frangogiannis, N. Transforming growth factor-β in tissue fibrosis. J. Exp. Med. 2020, 217, e20190103. [Google Scholar] [CrossRef] [PubMed]
- Zhu, M.; Li, W.; Dong, X.; Yuan, X.; Midgley, A.C.; Chang, H.; Wang, Y.; Wang, H.; Wang, K.; Ma, P.X.; et al. In vivo engineered extracellular matrix scaffolds with instructive niches for oriented tissue regeneration. Nat. Commun. 2019, 10, 4620. [Google Scholar] [CrossRef] [Green Version]
- Angunawela, R.I.; Riau, A.K.; Chaurasia, S.S.; Tan, D.T.; Mehta, J.S. Refractive lenticule re-implantation after myopic ReLEx: A feasibility study of stromal restoration after refractive surgery in a rabbit model. Investig. Ophthalmol. Vis. Sci. 2012, 53, 4975–4985. [Google Scholar] [CrossRef] [Green Version]
- Yu, F.S.; Yin, J.; Xu, K.; Huang, J. Growth factors and corneal epithelial wound healing. Brain Res. Bull. 2010, 81, 229–235. [Google Scholar] [CrossRef] [Green Version]
- Miyagi, H.; Jalilian, I.; Murphy, C.J.; Thomasy, S.M. Modulation of human corneal stromal cell differentiation by hepatocyte growth factor and substratum compliance. Exp. Eye Res. 2018, 176, 235–242. [Google Scholar] [CrossRef]
- Ziaei, M.; Greene, C.; Green, C.R. Wound healing in the eye: Therapeutic prospects. Adv. Drug Delivery Rev. 2018, 126, 162–176. [Google Scholar] [CrossRef]
- Susaimanickam, P.J.; Maddileti, S.; Pulimamidi, V.K.; Boyinpally, S.R.; Naik, R.R.; Naik, M.N.; Reddy, G.B.; Sangwan, V.S.; Mariappan, I. Generating minicorneal organoids from human induced pluripotent stem cells. Development 2017, 144, 2338–2351. [Google Scholar] [CrossRef] [Green Version]
- Zarei-Ghanavati, M.; Liu, C. Aspects of Corneal Transplant Immunology. J. Ophthalmic Vis. Res. 2017, 12, 249–250. [Google Scholar] [CrossRef] [PubMed]
- Raghu, P.K.; Bansal, K.K.; Thakor, P.; Bhavana, V.; Madan, J.; Rosenholm, J.M.; Mehra, N.K. Evolution of nanotechnology in delivering drugs to eyes, skin and wounds via topical route. Pharmaceuticals 2020, 13, 167. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santra, M.; Liu, Y.-C.; Jhanji, V.; Yam, G.H.-F. Human SMILE-Derived Stromal Lenticule Scaffold for Regenerative Therapy: Review and Perspectives. Int. J. Mol. Sci. 2022, 23, 7967. https://doi.org/10.3390/ijms23147967
Santra M, Liu Y-C, Jhanji V, Yam GH-F. Human SMILE-Derived Stromal Lenticule Scaffold for Regenerative Therapy: Review and Perspectives. International Journal of Molecular Sciences. 2022; 23(14):7967. https://doi.org/10.3390/ijms23147967
Chicago/Turabian StyleSantra, Mithun, Yu-Chi Liu, Vishal Jhanji, and Gary Hin-Fai Yam. 2022. "Human SMILE-Derived Stromal Lenticule Scaffold for Regenerative Therapy: Review and Perspectives" International Journal of Molecular Sciences 23, no. 14: 7967. https://doi.org/10.3390/ijms23147967
APA StyleSantra, M., Liu, Y.-C., Jhanji, V., & Yam, G. H.-F. (2022). Human SMILE-Derived Stromal Lenticule Scaffold for Regenerative Therapy: Review and Perspectives. International Journal of Molecular Sciences, 23(14), 7967. https://doi.org/10.3390/ijms23147967







