The Role of Registered Dietitians in Cancer Palliative Care: Responsibilities, Challenges, and Interdisciplinary Collaboration—A Cross-Sectional Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Questionnaire
- ➢
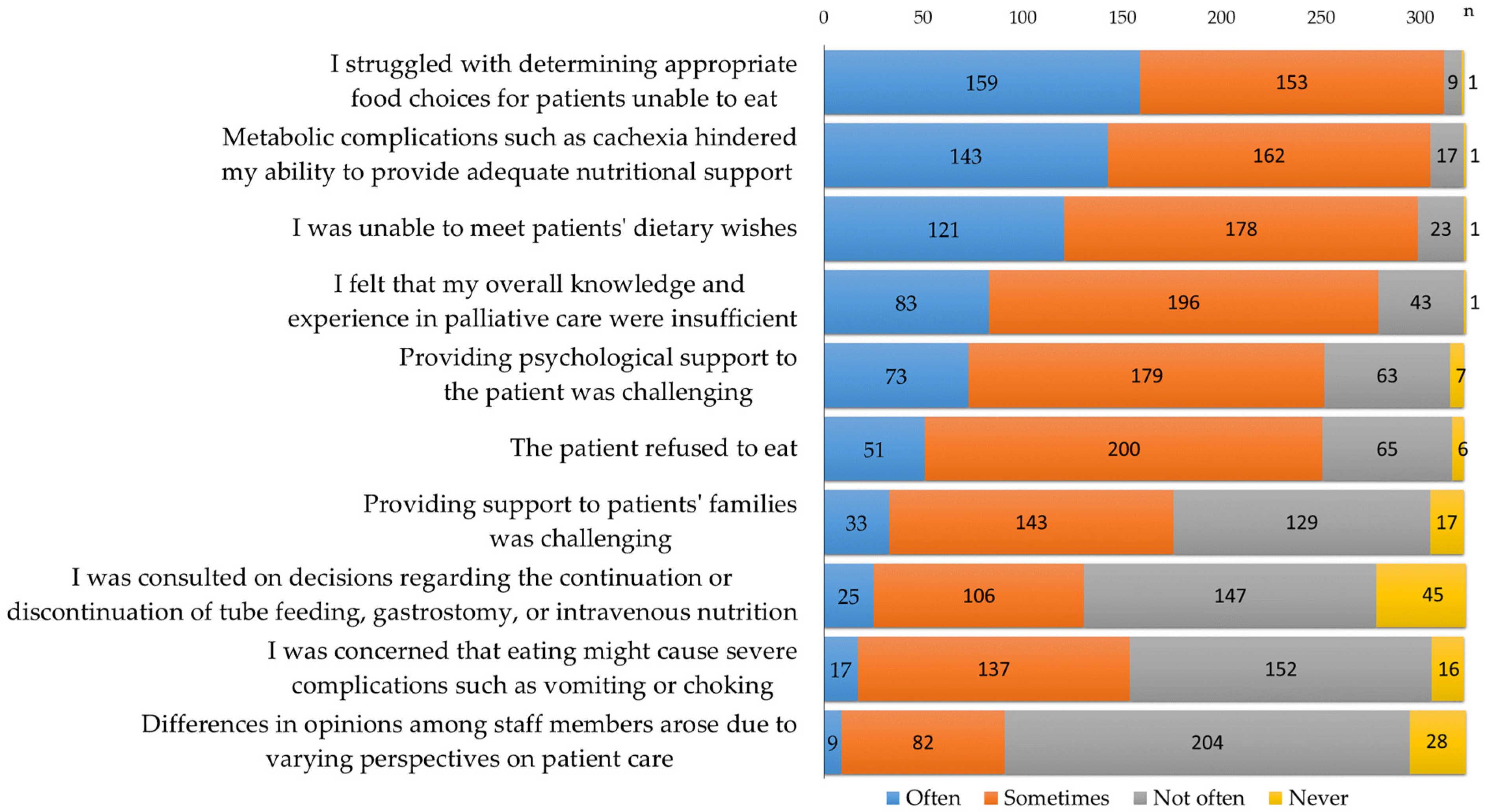
- I struggled with determining appropriate food choices for patients unable to eat.
- ➢
- Metabolic complications, such as cachexia, hindered my ability to provide adequate nutritional support.
- ➢
- I was unable to meet patients’ dietary wishes.
- ➢
- I was concerned that eating might cause severe complications such as vomiting or choking.
- ➢
- The patient refused to eat.
- ➢
- I was consulted on decisions regarding the continuation or discontinuation of tube feeding, gastrostomy, or intravenous nutrition.
- ➢
- Providing psychological support to the patient was challenging.
- ➢
- Differences in opinions among staff members arose due to varying perspectives on patient care.
- ➢
- I felt that my overall knowledge and experience in palliative care were insufficient.
- ➢
- Providing support to patients’ families was challenging.
2.3. Statistical Analysis
3. Results
4. Discussion
4.1. Collaboration with the Palliative Care Team
4.2. Ward Rounds and Challenges Faced by RDs in Palliative Care
4.3. Need for Specialized Training
4.4. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| RD | Registered dietitian |
| PCT | Palliative care team |
| CC group | Consistently collaborated group |
| AN group | Collaborated as-needed group |
References
- World Health Organization. Available online: https://www.who.int/news-room/fact-sheets/detail/palliative-care (accessed on 5 August 2020).
- Sanders, J.J.; Temin, S.; Ghoshal, A.; Alesi, E.R.; Ali, Z.V.; Chauhan, C.; Cleary, J.F.; Epstein, A.S.; Firn, J.I.; Jones, J.A.; et al. Palliative care for patients with Cancer: ASCO guideline update. J. Clin. Oncol. 2024, 42, 2336–2357. [Google Scholar] [CrossRef] [PubMed]
- Koshimoto, S.; Arimoto, M.; Saitou, K.; Uchibori, M.; Hashizume, A.; Honda, A.; Amano, K.; Nakajima, Y.; Uetake, H.; Matsushima, E. Need and demand for nutritional counselling and their association with quality of life, nutritional status and eating-related distress among patients with cancer receiving outpatient chemotherapy: A cross-sectional study. Support Care Cancer 2019, 27, 3385–3394. [Google Scholar] [CrossRef]
- Arends, J. Malnutrition in cancer patients: Causes, consequences and treatment options. Eur. J. Surg. Oncol. 2024, 50, 107074. [Google Scholar] [CrossRef]
- Arends, J.; Bachmann, P.; Baracos, V.; Barthelemy, N.; Bertz, H.; Bozzetti, F.; Fearon, K.; Hütterer, E.; Isenring, E.; Kaasa, S.; et al. ESPEN guidelines on nutrition in cancer patients. Clin. Nutr. 2017, 36, 11–48. [Google Scholar] [CrossRef]
- Roeland, E.J.; Bohlke, K.; Baracos, V.E.; Bruera, E.; Del Fabbro, E.; Dixon, S.; Fallon, M.; Herrstedt, J.; Lau, H.; Platek, M.; et al. Management of cancer cachexia: ASCO guideline. J. Clin. Oncol. 2020, 38, 2438–2453. [Google Scholar] [CrossRef] [PubMed]
- Grassi, L.; Caruso, R.; Riba, M.B.; Lloyd-Williams, M.; Kissane, D.; Rodin, G.; McFarland, D.; Campos-Ródenas, R.; Zachariae, R.; Santini, D.; et al. Anxiety and depression in adult cancer patients: ESMO Clinical Practice Guideline. ESMO Open 2023, 8, 101155. [Google Scholar] [CrossRef] [PubMed]
- De Feo, G.; Case, A.A.; Crawford, G.B.; Hui, D.; To, J.; Sbrana, A.; Alderman, B.; Mukhopadhyay, S.; Bouleuc, C.; Amano, K.; et al. Multinational Association of Supportive Care in Cancer (MASCC) guidelines: Cannabis for psychological symptoms including insomnia, anxiety, and depression. Support Care Cancer 2023, 31, 176. [Google Scholar] [CrossRef]
- Koshimoto, S.; Yamazaki, T.; Amano, K.; Kako, J.; Arimoto, M.; Saitou, K.; Hashizume, A.; Takeuchi, T.; Matsushima, E. Psychosocial factors and the need for multidisciplinary support in nutrition counselling for cancer chemotherapy patients. Nutrients 2023, 15, 2712. [Google Scholar] [CrossRef]
- Morrison-Koechl, J.; Heckman, G.; Banerjee, A.; Keller, H. Factors associated with dietitian referrals to support long-term care residents advancing towards the end of life. J. Hum. Nutr. Diet. 2024, 37, 673–684. [Google Scholar] [CrossRef]
- Koshimoto, S.; Amano, K.; Mori, N.; Oyamada, S.; Arakawa, S.; Ishiki, H.; Satomi, E.; Morita, T.; Takeuchi, T. Perspectives of registered dietitians and factors associated with their personal accomplishment in the management of cancer cachexia. Support Care Cancer 2023, 31, 124. [Google Scholar] [CrossRef]
- Amano, K.; Morita, T.; Koshimoto, S.; Uno, T.; Katayama, H.; Tatara, R. Eating-related distress in advanced cancer patients with cachexia and family members: A survey in palliative and supportive care settings. Support Care Cancer 2019, 27, 2869–2876. [Google Scholar] [CrossRef] [PubMed]
- Acreman, S. Nutrition in palliative care. Br. J. Community Nurs. 2009, 14, 427–431. [Google Scholar] [CrossRef][Green Version]
- Arends, J. Struggling with nutrition in patients with advanced cancer: Nutrition and nourishment-focusing on metabolism and supportive care. Ann. Oncol. 2018, 39 (Suppl. 2), ii27–ii34. [Google Scholar] [CrossRef] [PubMed]
- Wallin, V.; Mattsson, E.; Omerov, P.; Klarare, A. Caring for patients with eating deficiencies in palliative care-Registered nurses’ experiences: A qualitative study. J. Clin. Nurs. 2022, 31, 3165–3177. [Google Scholar] [CrossRef] [PubMed]
- Amano, K.; Arakawa, S.; Hopkinson, J.B.; Baracos, V.E.; Oyamada, S.; Koshimoto, S.; Mori, N.; Ishiki, H.; Morita, T.; Takeuchi, T.; et al. Factors associated with multimodal care practices for cancer cachexia among registered dietitians. Support Care Cancer 2024, 32, 213. [Google Scholar] [CrossRef]
- Alderman, B.; Allan, L.; Amano, K.; Bouleuc, C.; Davis, M.; Lister-Flynn, S.; Mukhopadhyay, S.; Davies, A. Multinational Association of Supportive Care in Cancer (MASCC) expert opinion/guidance on the use of clinically assisted nutrition in patients with advanced cancer. Support Care Cancer 2022, 30, 2983–2992. [Google Scholar] [CrossRef]
- Muscaritoli, M.; Arends, J.; Bachmann, P.; Baracos, V.; Barthelemy, N.; Bertz, H.; Bozzetti, F.; Hütterer, E.; Isenring, E.; Kaasa, S.; et al. ESPEN practical guideline: Clinical Nutrition in cancer. Clin. Nutr. 2021, 40, 2898–2913. [Google Scholar] [CrossRef]
- Bowers, M.; Higginson, I.J.; Maddocks, M. Patient and Carer Experiences of Cancer Cachexia and Its Management. Curr. Opin. Support. Palliat. Care 2024, 18, 132–137. [Google Scholar] [CrossRef]
- Holdoway, A. Nutrition in Palliative Care: Issues, Perceptions and Opportunities to Improve Care for Patients. Br. J. Nurs. 2022, 31, S20–S27. [Google Scholar] [CrossRef]
- Amano, K.; Koshimoto, S.; Okamura, S.; Sakaguchi, T.; Arakawa, S.; Matsuda, Y.; Tokoro, A.; Takeuchi, T.; Satomi, E.; Wada, T.; et al. Association of Systemic Inflammation with Dietary Intake, Nutrition Impact Symptoms, and Eating-Related Distress Among Patients with Advanced Cancer. Healthcare 2024, 12, 2533. [Google Scholar] [CrossRef]
- Soares, C.H.; Beuren, A.G.; Friedrich, H.J.; Gabrielli, C.P.; Stefani, G.P.; Steemburgo, T. The Importance of Nutrition in Cancer Care: A Narrative Review. Curr. Nutr. Rep. 2024, 13, 950–965. [Google Scholar] [CrossRef]
- Erickson, N.; Sulosari, V.; Sullivan, E.S.; Laviano, A.; van Ginkel-Res, A.; Remijnse, W.; Wesseling, J.; Koepcke, U.; Weber, N.; Huebner, J.; et al. Nutrition Care in Cancer: An Overlooked Part of Patient-Centered Care. Semin. Oncol. Nurs. 2025, 41, 151799. [Google Scholar] [CrossRef]
- Naito, T.; Wakabayashi, H.; Aso, S.; Konishi, M.; Saitoh, M.; Baracos, V.E.; Coats, A.J.; Anker, S.D.; Sherman, L.; Klompenhouwer, T.; et al. The Barriers to Interprofessional Care for Cancer Cachexia among Japanese Healthcare Providers: A Nationwide Survey. J. Cachexia Sarcopenia Muscle 2024, 15, 387–400. [Google Scholar] [CrossRef] [PubMed]
- Pornrattanakavee, P.; Srichan, T.; Seetalarom, K.; Saichaemchan, S.; Oer-Areemitr, N.; Prasongsook, N. Impact of Interprofessional Collaborative Practice in Palliative Care on Outcomes for Advanced Cancer Inpatients in a Resource-Limited Setting. BMC Palliat. Care 2022, 21, 229. [Google Scholar] [CrossRef]
- Hustad, K.S.; Koteng, L.H.; Urrizola, A.; Arends, J.; Bye, A.; Dajani, O.; Deliens, L.; Fallon, M.; Hjermstad, M.J.; Kohlen, M.; et al. Practical Cancer Nutrition, from Guidelines to Clinical Practice: A Digital Solution to Patient-Centred Care. ESMO Open 2025, 10, 104529. [Google Scholar] [CrossRef] [PubMed]
- Källén, E.; Nimström, S.; Rosengren, K. Content and Structure of Ward Rounds Focusing on Interprofessional Collaboration on an Internal Medicine Ward: An Observational Study of Interprofessional Collaboration. J. Interprof. Care 2021, 35, 219–226. [Google Scholar] [CrossRef]
- Schütte, K.; Middelberg-Bisping, K.; Schulz, C. Nutrition and Gastro-Enterological Support in End of Life Care. Best Pract. Res. Clin. Gastroenterol. 2020, 48–49, 101692. [Google Scholar] [CrossRef]
- Cotogni, P.; Stragliotto, S.; Ossola, M.; Collo, A.; Riso, S. The Role of Nutritional Support for Cancer Patients in Palliative Care. Nutrients 2021, 13, 306. [Google Scholar] [CrossRef]
- Chitose, H.; Kuwana, M.; Miura, T.; Inoue, M.; Nagasu, Y.; Shimizu, R.; Hattori, Y.; Uehara, Y.; Kosugi, K.; Matsumoto, Y. A Japanese Nationwide Survey of Nutritional Counseling for Cancer Patients and Risk Factors of Burnout among Registered Dietitians. Palliat. Med. Rep. 2022, 3, 211–219. [Google Scholar] [CrossRef]
- Alhaj, O.A.; Elsahoryi, N.A.; Fekih-Romdhane, F.; Wishah, M.; Sweidan, D.H.; Husain, W.; Achraf, A.; Trabelsi, K.; Hebert, J.R.; Jahrami, H. Prevalence of emotional burnout among dietitians and nutritionists: A systematic review, meta-analysis, meta-regression, and a call for action. BMC Psychol. 2024, 12, 775. [Google Scholar] [CrossRef]
- Crawford, G.B.; Dzierżanowski, T.; Hauser, K.; Larkin, P.; Luque-Blanco, A.I.; Murphy, I.; Puchalski, C.M.; Ripamonti, C.I. Care of the adult cancer patient at the end of life: ESMO Clinical Practice Guidelines. ESMO Open. 2021, 6, 100225. [Google Scholar] [CrossRef] [PubMed]
- Stone, P.; Buckle, P.; Dolan, R.; Feliu, J.; Hui, D.; Laird, B.J.A.; Maltoni, M.; Moine, S.; Morita, T.; Nabal, M.; et al. Prognostic evaluation in patients with advanced cancer in the last months of life: ESMO Clinical Practice Guideline. ESMO Open 2023, 8, 101195. [Google Scholar] [CrossRef] [PubMed]
- Baracos, V.E.; Coats, A.J.; Anker, S.D.; Sherman, L.; Klompenhouwer, T.; International Advisory Board, and Regional Advisory Boards for North America, Europe, and Japan. Identification and Management of Cancer Cachexia in Patients: Assessment of Healthcare Providers’ Knowledge and Practice Gaps. J. Cachexia Sarcopenia Muscle 2022, 13, 2683–2696. [Google Scholar] [CrossRef]
- Miles, A.; Brady, A.; Friary, P.; Sekula, J.; Wallis, C.; Jackson, B. Implementing an Interprofessional Palliative Care Education Program to Speech-Language Therapy and Dietetic Students. J. Interprof. Care 2023, 37, 964–973. [Google Scholar] [CrossRef]
- Tanaka, K.; Nakamura, S.; Narimatsu, H. Nutritional Approach to Cancer Cachexia: A Proposal for Dietitians. Nutrients 2022, 14, 345. [Google Scholar] [CrossRef] [PubMed]
- Öner, Ö.; Ayvat, P.; Gökmen, A.N. Nutritional Therapy in Palliative Care Units: A Bibliometric Analysis. Medicine 2025, 104, e41772. [Google Scholar] [CrossRef]
- Erickson, N.; Sullivan, E.S.; Kalliostra, M.; Laviano, A.; Wesseling, J. Nutrition Care Is an Integral Part of Patient-Centered Medical Care: A European Consensus. Med. Oncol. 2023, 40, 112. [Google Scholar] [CrossRef]
| Characteristics | n (%) |
|---|---|
| Age | |
| 20–29 years old | 27 (8.3) |
| 30–39 years old | 99 (30.5) |
| 40–49 years old | 124 (38.2) |
| 50–59 years old | 66 (20.3) |
| 60 years old or over | 8 (2.5) |
| Sex | |
| Male | 28 (8.6) |
| Female | 276 (84.9) |
| Area of Practice | |
| Exclusively engaged in palliative care | 60 (18.5) |
| Exclusively engaged in cancer care | 11 (3.4) |
| Concurrently in another area | 254 (78.2) |
| Years of Experience in Cancer Care | |
| 0–5 years | 108 (33.2) |
| 6–10 years | 107 (32.9) |
| 11–15 years | 49 (15.1) |
| 16–20 years | 36 (11.1) |
| 21 years or more | 11 (3.4) |
| Certifications | |
| Certification as a registered dietitian specializing in pathophysiology | 172 (52.9) |
| Certification as a registered dietitian specializing in cancer | 139 (42.8) |
| Duties | |
| Nutritional management | 309 (95.1) |
| Nutritional counseling | 308 (94.8) |
| Conferences | 290 (89.2) |
| Meal rounds | 185 (56.9) |
| Menu planning | 89 (27.4) |
| Cooking | 9 (2.8) |
| Catering and serving | 15 (4.6) |
| Ingredient management | 21 (6.5) |
| Nutritional Counseling Responsibilities | |
| Nutritional counseling for palliative care inpatients | 229 (70.5) |
| Nutritional counseling for palliative care outpatients | 144 (44.3) |
| Number of Ward Rounds | |
| Daily | 129 (39.7) |
| Several times a week | 157 (48.3) |
| Several times a month | 24 (7.4) |
| Occasionally in a year | 11 (3.4) |
| Academic Society Memberships | |
| Japan Society of Metabolism and Clinical Nutrition | 252 (77.5) |
| Japanese Society for Parenteral and Enteral Nutrition Therapy | 185 (56.9) |
| The Japanese Society of Nutrition and Dietetics | 18 (5.5) |
| Japanese Society for Palliative Medicine | 14 (4.3) |
| The Japanese Society of Clinical Nutrition | 13 (4.0) |
| Japanese Society on Nutrition Care and Management | 7 (2.2) |
| Japanese Association of Supportive Care in Cancer | 3 (0.9) |
| Japan Society of Clinical Oncology | 1 (0.3) |
| Japan Psycho-Oncology Society | 0 (0.0) |
| Education in Palliative Care | |
| Pre-graduate education | 48 (14.8) |
| Post-graduate education | 238 (73.2) |
| Characteristics | n (%) |
|---|---|
| Meal Provision System | |
| Directly operated by hospital | 61 (18.8) |
| Outside contractors | 188 (57.8) |
| Partially outsourced to outside contractors | 72 (22.2) |
| Number of Beds in Palliative Care Units | |
| 0 beds (= Palliative care provided in general wards) | 170 (52.3) |
| 1–9 beds | 28 (8.6) |
| 10–19 beds | 40 (12.3) |
| 20–29 beds | 63 (19.4) |
| ≥30 beds | 10 (3.1) |
| Type of Meal Provision | |
| Individualized meals | 179 (55.1) |
| Palliative care meals | 79 (24.3) |
| Standard therapeutic meals | 67 (20.6) |
| Level of Individualized Meal Provision | |
| Fully individualized meals based on patient preferences | 61 (18.8) |
| Partially individualized meals | 237 (72.9) |
| No individualized meals | 21 (6.5) |
| Level of Collaboration with the Palliative Care Team | |
| Consistently collaborated | 241 (74.2) |
| Collaborated as needed | 84 (25.8) |
| Level of Collaboration with the Nutrition Support Team | |
| Consistently collaborated | 52 (16.0) |
| Collaborated as needed | 273 (84.0) |
| Variable | Consistently Collaborated (CC) Group (n = 241) | Collaborated As-Needed (AN) Group (n = 84) | p-Value |
|---|---|---|---|
| n (%) | n (%) | ||
| Certification | |||
| Certification as a registered dietitian specializing in pathophysiology | 129 (53.5) | 43 (51.2) | 0.800 |
| Certification as a registered dietitian specializing in cancer | 108 (44.8) | 31 (36.9) | 0.249 |
| Responsibilities | |||
| Exclusively engaged in palliative or cancer care | 62 (25.7) | (10.7) | 0.003 * |
| Concurrently in other departments | 179 (74.3) | 75 (89.3) | |
| Nutritional Counseling Responsibilities | |||
| For palliative care inpatients | 180 (74.7) | (58.3) | 0.005 |
| For palliative care outpatients | 114 (47.3) | 30 (35.7) | 0.066 |
| Duties | |||
| Meal rounds | 138 (57.3) | 47 (56.0) | 0.222 |
| Ward Rounds | |||
| Daily | 102 (42.3) | 27 (32.1) | <0.001 * |
| Several times a week | 122 (50.6) | 35 (41.7) | |
| Several times a month | 11 (4.6) | 13 (15.5) | |
| Several times a year | 3 (1.2) | 8 (9.5) | |
| Provision of Meals | |||
| Individualized meals | 146 (60.6) | 33 (39.3) | 0.004 * |
| Palliative care meals | 48 (19.9) | 31 (36.9) | |
| Standard therapeutic meals | 47 (19.5) | 20 (23.8) | |
| Level of Individualized Meal Provision | |||
| Fully individualized meals based on patient preferences | 50 (20.7) | 11 (13.1) | 0.035 * |
| Partially individualized meals | 174 (72.2) | 63 (75.0) | |
| No individualized meals | 12 (5.0) | 9 (10.7) | |
| Education in Palliative Care | |||
| Pre-graduate education | 37 (15.4) | 11 (13.1) | 0.241 |
| Post-graduate education | 181 (75.1) | 57 (67.9) | 0.167 |
| Independent Variable | Odds Ratio (95% CI) | p-Value |
|---|---|---|
| Years of experience in cancer care | 1.03 (0.98–1.09) | 0.269 |
| Certification as a registered dietitian specializing in cancer | 1.13 (0.59–2.19) | 0.713 |
| Exclusively engaged in palliative care or cancer care | 3.18 (1.27–7.98) | 0.014 * |
| Ward rounds (reference: occasionally in a year) | ||
| Several times a month | 2.32 (0.46–11.83) | 0.310 |
| Several times per week | 9.35 (2.19–39.97) | 0.003 * |
| Daily | 9.70 (2.23–42.12) | 0.002 * |
| Type of meal provision (reference: standard therapeutic meals) | ||
| Palliative care meals | 1.68 (0.60–4.70) | 0.322 |
| Individualized meals | 3.50 (1.01–12.07) | 0.048 * |
| Dependent Variable | Independent Variable | Odds Ratio (95% CI) | p-Value |
|---|---|---|---|
| I struggled with determining appropriate food choices for patients unable to eat. | Years of experience in cancer care | 1.04 (0.92–1.16) | 0.555 |
| Certification as a registered dietitian specializing in cancer | 0.30 (0.06–1.53) | 0.148 | |
| Exclusively engaged in palliative care or cancer care | 2.71 (0.32–22.96) | 0.361 | |
| Meal rounds | 0.41 (0.08–2.19) | 0.299 | |
| Fully individualized meals based on patient preferences | 0.22 (0.05–0.88) | 0.032 * | |
| Level of collaboration with the palliative care team | 0.32 (0.04–2.54) | 0.279 | |
| Pre-graduate education | 1.03 (0.11–9.26) | 0.982 | |
| Post-graduate education | 0.44 (0.05–3.92) | 0.462 | |
| Metabolic complications, such as cachexia, hindered my ability to provide adequate nutritional support. | Years of experience in cancer care | 0.97 (0.89–1.05) | 0.466 |
| Certification as a registered dietitian specializing in cancer | 1.90 (0.55–6.60) | 0.310 | |
| Exclusively engaged in palliative care or cancer care | 3.88 (0.48–31.3) | 0.203 | |
| Meal rounds | 1.69 (0.59–4.82) | 0.327 | |
| Fully individualized meals based on patient preferences | 0.30 (0.11–0.85) | 0.023 * | |
| Level of collaboration with the palliative care team | 1.87 (0.61–5.69) | 0.274 | |
| Pre-graduate education | 0.75 (0.19–2.91) | 0.674 | |
| Post-graduate education | 1.28 (0.40–4.06) | 0.681 | |
| I was unable to meet patients’ dietary wishes. | Years of experience in cancer care | 0.96 (0.89–1.04) | 0.322 |
| Certification as a registered dietitian specializing in cancer | 2.05 (0.67–6.23) | 0.207 | |
| Exclusively engaged in palliative care or cancer care | 0.58 (0.20–1.67) | 0.313 | |
| Meal rounds | 0.55 (0.20–1.50) | 0.240 | |
| Fully individualized meals based on patient preferences | 0.35 (0.15–0.86) | 0.022 * | |
| Level of collaboration with the palliative care team | 0.90 (0.27–2.98) | 0.862 | |
| Pre-graduate education | 0.22 (0.08–0.60) | 0.003 * | |
| Post-graduate education | 0.86 (0.28–2.65) | 0.786 | |
| I felt that my overall knowledge and experience in palliative care were insufficient. | Years of experience in cancer care | 0.96 (0.90–1.01) | 0.095 |
| Certification as a registered dietitian specializing in cancer | 0.39 (0.18–0.84) | 0.016 * | |
| Exclusively engaged in palliative care or cancer care | 0.74 (0.32–1.71) | 0.481 | |
| Meal rounds | 0.47 (0.22–0.98) | 0.044 * | |
| Fully individualized meals based on patient preferences | 0.59 (0.29–1.19) | 0.140 | |
| Level of collaboration with the palliative care team | 1.15 (0.50–2.65) | 0.740 | |
| Pre-graduate education | 1.61 (0.51–5.08) | 0.421 | |
| Post-graduate education | 0.79 (0.32–1.96) | 0.604 | |
| Providing psychological support to the patient was challenging. | Years of experience in cancer care | 0.98 (0.93–1.02) | 0.308 |
| Certification as a registered dietitian specializing in cancer | 1.54 (0.80–2.97) | 0.195 | |
| Exclusively engaged in palliative care or cancer care | 1.03 (0.50–2.14) | 0.932 | |
| Meal rounds | 1.14 (0.65–2.01) | 0.645 | |
| Fully individualized meals based on patient preferences | 1.15 (0.65–2.02) | 0.634 | |
| Level of collaboration with the palliative care team | 1.30 (0.70–2.43) | 0.409 | |
| Pre-graduate education | 1.21 (0.52–2.80) | 0.663 | |
| Post-graduate education | 1.60 (0.86–2.98) | 0.137 | |
| The patient refused to eat. | Years of experience in cancer care | 0.95 (0.91–1.00) | 0.037 * |
| Certification as a registered dietitian specializing in cancer | 0.85 (0.44–1.64) | 0.632 | |
| Exclusively engaged in palliative care or cancer care | 1.12 (0.52–2.37) | 0.778 | |
| Meal rounds | 0.83 (0.46–1.50) | 0.535 | |
| Fully individualized meals based on patient preferences | 0.82 (0.46–1.46) | 0.496 | |
| Level of collaboration with the palliative care team | 1.03 (0.52–2.02) | 0.932 | |
| Pre-graduate education | 0.46 (0.22–0.99) | 0.048 * | |
| Post-graduate education | 1.83 (0.95–3.51) | 0.071 | |
| Providing support to patients’ families was challenging. | Years of experience in cancer care | 1.00 (0.96–1.04) | 0.992 |
| Certification as a registered dietitian specializing in cancer | 1.18 (0.68–2.03) | 0.556 | |
| Exclusively engaged in palliative care or cancer care | 1.56 (0.84–2.90) | 0.161 | |
| Meal rounds | 1.36 (0.84–2.20) | 0.214 | |
| Fully individualized meals based on patient preferences | 0.67 (0.41–1.10) | 0.111 | |
| Level of collaboration with the palliative care team | 1.27 (0.73–2.21) | 0.399 | |
| Pre-graduate education | 1.31 (0.65–2.62) | 0.446 | |
| Post-graduate education | 2.01 (1.15–3.52) | 0.015 * | |
| I was consulted on decisions regarding the continuation or discontinuation of tube feeding, gastrostomy, or intravenous nutrition. | Years of experience in cancer care | 1.01 (0.97–1.06) | 0.604 |
| Certification as a registered dietitian specializing in cancer | 1.05 (0.61–1.82) | 0.862 | |
| Exclusively engaged in palliative care or cancer care | 0.89 (0.48–1.66) | 0.723 | |
| Meal rounds | 2.30 (1.40–3.79) | 0.001 * | |
| Fully individualized meals based on patient preferences | 1.34 (0.82–2.20) | 0.244 | |
| Level of collaboration with the palliative care team | 0.84 (0.47–1.47) | 0.533 | |
| Pre-graduate education | 1.02 (0.51–2.05) | 0.949 | |
| Post-graduate education | 1.61 (0.90–2.89) | 0.110 | |
| I was concerned that eating might cause severe complications such as vomiting or choking. | Years of experience in cancer care | 1.00 (0.96–1.05) | 0.928 |
| Certification as a registered dietitian specializing in cancer | 0.94 (0.55–1.59) | 0.805 | |
| Exclusively engaged in palliative care or cancer care | 0.94 (0.52–1.70) | 0.832 | |
| Meal rounds | 1.03 (0.64–1.66) | 0.897 | |
| Fully individualized meals based on patient preferences | 1.02 (0.64–1.65) | 0.925 | |
| Level of collaboration with the palliative care team | 1.21 (0.70–2.10) | 0.485 | |
| Pre-graduate education | 0.99 (0.51–1.94) | 0.978 | |
| Post-graduate education | 1.61 (0.93–2.81) | 0.090 | |
| Differences in opinions among staff members arose due to varying perspectives on patient care. | Years of experience in cancer care | 1.03 (0.98–1.08) | 0.219 |
| Certification as a registered dietitian specializing in cancer | 1.14 (0.64–2.05) | 0.656 | |
| Exclusively engaged in palliative care or cancer care | 1.79 (0.96–3.35) | 0.068 | |
| Meal rounds | 1.06 (0.62–1.80) | 0.828 | |
| Fully individualized meals based on patient preferences | 0.90 (0.53–1.54) | 0.701 | |
| Level of collaboration with the palliative care team | 1.33 (0.70–2.52) | 0.379 | |
| Pre-graduate education | 0.87 (0.40–1.90) | 0.724 | |
| Post-graduate education | 0.85 (0.46–1.57) | 0.596 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koshimoto, S.; Amano, K.; Mori, N.; Imai, A.; Sasaki, M.; Miyajima, M.; Takeuchi, T. The Role of Registered Dietitians in Cancer Palliative Care: Responsibilities, Challenges, and Interdisciplinary Collaboration—A Cross-Sectional Survey. Curr. Oncol. 2025, 32, 275. https://doi.org/10.3390/curroncol32050275
Koshimoto S, Amano K, Mori N, Imai A, Sasaki M, Miyajima M, Takeuchi T. The Role of Registered Dietitians in Cancer Palliative Care: Responsibilities, Challenges, and Interdisciplinary Collaboration—A Cross-Sectional Survey. Current Oncology. 2025; 32(5):275. https://doi.org/10.3390/curroncol32050275
Chicago/Turabian StyleKoshimoto, Saori, Koji Amano, Naoharu Mori, Atsuko Imai, Manami Sasaki, Miho Miyajima, and Takashi Takeuchi. 2025. "The Role of Registered Dietitians in Cancer Palliative Care: Responsibilities, Challenges, and Interdisciplinary Collaboration—A Cross-Sectional Survey" Current Oncology 32, no. 5: 275. https://doi.org/10.3390/curroncol32050275
APA StyleKoshimoto, S., Amano, K., Mori, N., Imai, A., Sasaki, M., Miyajima, M., & Takeuchi, T. (2025). The Role of Registered Dietitians in Cancer Palliative Care: Responsibilities, Challenges, and Interdisciplinary Collaboration—A Cross-Sectional Survey. Current Oncology, 32(5), 275. https://doi.org/10.3390/curroncol32050275





