Abstract
Registered dietitians (RDs) in palliative care help maintain patients’ quality of life by providing personalized nutritional support that alleviates eating-related distress. This study aimed to clarify the role of RDs in palliative care by examining their responsibilities and challenges in caring for cancer patients. A nationwide mailed survey was conducted in 2022, focusing on RDs involved in cancer palliative care. One RD per facility was included from all 501 hospitals accredited by Japan’s Ministry of Health, Labour and Welfare. Multivariate analysis identified factors related to collaboration with palliative care teams and challenges in cancer care. Responses from 325 RDs (63.9%) across 325 hospitals (63.9%) were analyzed. Among RDs who consistently collaborated with the palliative care team (PCT), significant associations (p < 0.05) were found with exclusive engagement in cancer/palliative care, providing nutritional counseling to inpatients, the frequency of ward rounds, and individualized meal provision. Challenges included the following: “I struggled with determining appropriate food choices for patients unable to eat”, and “Metabolic complications like cachexia hindered my ability to provide adequate support”. RDs play a crucial role in providing individualized meals for cancer patients through PCT collaboration and ward rounds. To ensure effective support in challenging situations, RDs must be exclusively engaged in palliative care and receive specialized education.
1. Introduction
Palliative care is a holistic medical approach that addresses the physical symptoms of cancer patients as well as their psychiatric and psychological distress through mental health care [1]. A comprehensive approach to physical, psychosocial, and spiritual issues is necessary at diagnosis, throughout treatment, and in the home setting to ensure that patients and their families receive the highest possible quality of care and recuperation [2].
Common interventions include nutritional support [3]. Malnutrition and cachexia contribute to delayed postoperative recovery, reduced therapeutic efficacy, increased infection risk, prolonged hospitalization, decreased activities of daily living, and diminished quality of life (QOL) [4,5,6,7,8]. Therefore, intervention by registered dietitians (RDs) is important [9,10,11]. A survey of cancer outpatients reported that low QOL and eating-related distress are key factors influencing the decision to seek nutritional counseling [3]. Notably, patients with cancer cachexia and their families express concerns about eating-related distress [12]. They often experience difficulties with food and nutrition and require comprehensive support that addresses psychological aspects such as anxiety and depression [13,14,15]. RDs play a vital role in palliative care, as nutritional support must address both physical needs and psychosocial aspects [9]. Within the healthcare system, RDs are expected to collaborate with palliative care teams (PCTs) and provide nutritional management tailored to patients’ symptoms and preferences [16]. However, the required competencies for RDs in palliative care remain unstandardized, and interdisciplinary collaboration in cancer cachexia management and eating-related distress remains inadequate. We performed a questionnaire survey to explore the responsibilities of RDs in palliative care, the challenges they encounter in patient care, and their role in improving overall patient support.
2. Materials and Methods
2.1. Subjects
Study participants were RDs engaged in cancer palliative care or cancer care who completed a self-administered, anonymous questionnaire survey. In 2022, nationwide questionnaires were mailed to RDs at 509 hospitals that met the criteria for palliative care facilities in Japan and were listed in the institutional directory of the Ministry of Health, Labour and Welfare. One representative RD from each hospital was requested to respond, and completed questionnaires were requested to be returned in a stamped, self-addressed envelope within one month.
2.2. Questionnaire
The demographic data collected included participants’ age, sex, area of practice, years of experience, nature of practice, and prior educational experience related to palliative and end-of-life care. Based on a review of previous studies on palliative care and nutrition, we identified 10 key questions that address the challenges faced by RDs in the care of palliative and terminally ill patients. The questionnaire included the following items:
- ➢
- I struggled with determining appropriate food choices for patients unable to eat.
- ➢
- Metabolic complications, such as cachexia, hindered my ability to provide adequate nutritional support.
- ➢
- I was unable to meet patients’ dietary wishes.
- ➢
- I was concerned that eating might cause severe complications such as vomiting or choking.
- ➢
- The patient refused to eat.
- ➢
- I was consulted on decisions regarding the continuation or discontinuation of tube feeding, gastrostomy, or intravenous nutrition.
- ➢
- Providing psychological support to the patient was challenging.
- ➢
- Differences in opinions among staff members arose due to varying perspectives on patient care.
- ➢
- I felt that my overall knowledge and experience in palliative care were insufficient.
- ➢
- Providing support to patients’ families was challenging.
These items were developed independently based on previous studies [3,9,12,13,14]. Facility-related data included the number of beds, meal management system, availability of individualized meals, and frequency of ward rounds.
2.3. Statistical Analysis
The level of collaboration with the PCT was compared between two groups: (1) RDs who consistently collaborated as team members or maintained continuous involvement with the team (consistently collaborated group [CC group]) and (2) RDs who collaborated with the team on an as-needed basis (collaborated as-needed group [AN group]). Comparisons between the PCT and the CC and AN groups were performed using Fisher’s exact test for nominal variables and the Mann–Whitney U test for ordinal variables. To identify factors associated with collaboration between RDs and PCT, a multivariate analysis was performed using the following independent variables: certification; responsibilities; nutritional counseling responsibilities; ward rounds; provision of meals; level of individualized meal provision; and education in palliative care. In addition, in order to identify the factors influencing the challenging situations encountered by RDs, challenging situations were used as dependent variables for two groups: (1) “often/sometimes” and (2) “not often/never”. Independent variables included years of experience in cancer care; certification as an RD specializing in cancer; exclusively engaged in palliative care or cancer care; meal rounds; fully individualized meals based on patient preferences; level of collaboration with the palliative care team; and pre-graduate education and post-graduate education on palliative care. Multiple logistic regression was used for multivariate analysis. Covariate correlations were assessed to exclude multicollinearity prior to logistic regression analysis. All statistical analyses were performed using SPSS (IBM Corp. Released 2023. IBM SPSS Statistics for Windows, Version 29.0.2.0 Armonk, NY, USA: IBM Corp.). A two-tailed test was applied, and statistical significance was set at p < 0.05.
3. Results
Of the 509 palliative care facilities, responses were received from 329 RDs (response rate of 64.6%). After excluding responses that did not provide consent, 325 facilities (63.9%) and 325 RDs (63.9%) were included in the final analysis. Table 1 shows the characteristics of the RDs. Table 2 describes the characteristics of their respective facilities.

Table 1.
Characteristics of registered dietitians (n = 325).

Table 2.
Characteristics of facilities associated with registered dietitians (n = 325).
Table 3 shows the association between the role of RDs and their collaboration with the PCT. Compared with the AN group (25.8%, n = 84), the CC group (74.2%, n = 241) was significantly more likely to be dedicated to cancer/palliative care (p = 0.003), responsible for nutritional counseling for hospitalized patients (p = 0.005), participate in ward rounds more frequently (p < 0.001), provide individualized meals (p = 0.004), and ensure the availability of completely individualized meals based on patients’ wishes (p = 0.035).

Table 3.
The role of registered dietitians and their collaboration with the palliative care team (n = 325).
Multivariate analysis identified three significant factors influencing consistent collaboration with the PCT: exclusively engaged in palliative care or cancer care (OR = 3.18; 95% CI: 1.27–7.98; p = 0.014); the frequency of ward rounds, with daily (OR = 9.70; 95% CI: 2.23–42.12; p = 0.002) and several times per week (OR = 9.35; 95% CI: 2.19–39.97; p = 0.003) being significant predictors; and the type of meal provision, with the implementation of individualized meals (OR = 3.50; 95% CI: 1.01–12.07; p = 0.048) also being a significant predictor (Table 4).

Table 4.
Multivariate analysis of factors influencing palliative care team collaboration.
Figure 1 shows the challenges encountered by RDs in providing care for palliative patients. More than 90% of RDs reported “often” or “sometimes” experiencing difficulties, including “I struggled with determining appropriate food choices for patients unable to eat”, “Metabolic complications such as cachexia hindered my ability to provide adequate support”, and “I was unable to meet patients’ dietary wishes”.
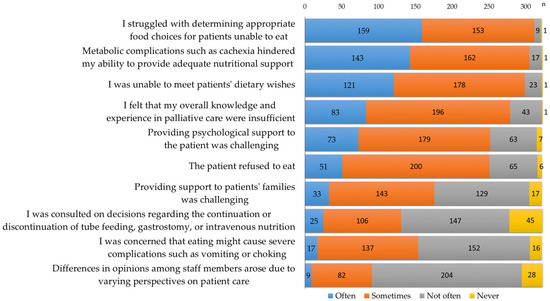
Figure 1.
Challenges encountered by RDs in providing care for palliative patients (n = 325).
To identify the factors influencing these challenges, multivariate analysis was performed using the following independent variables: years of clinical experience, certification as a registered dietitian specializing in cancer (reference: no certification), exclusively engaged in palliative care or cancer care (reference: not exclusively engaged), meal round responsibilities (reference: no meal rounds), fully individualized meals based on patient preferences (reference: no fully individualized meals), level of collaboration with the PCT, pre-graduate education (reference: no pre-graduate education), and post-graduate education (reference: no post-graduate education).
The provision of fully individualized meals was significantly associated with a decrease in the number of challenging situations for RDs, such as “I struggled with determining appropriate food choices for patients unable to eat” (OR = 0.22; 95% CI: 0.05–0.88; p = 0.032) and “Metabolic complications, such as cachexia, hindered my ability to provide adequate nutritional support” (OR = 0.30; 95% CI: 0.11–0.85; p = 0.023). The provision of fully individualized meals based on patient preferences (OR = 0.35; 95% CI: 0.15–0.86; p = 0.022) and pre-graduate education (OR = 0.22; 95% CI: 0.08–0.60; p = 0.003) were significantly associated with fewer challenging situations in which RDs reported, “I was unable to meet patients’ dietary wishes”. Certification as a registered dietitian specializing in cancer (OR = 0.39; 95% CI: 0.18–0.84; p = 0.016) and participation in meal rounds (OR = 0.47; 95% CI: 0.22–0.98; p = 0.044) were significantly associated with fewer challenging situations in which RDs reported, “I felt that my overall knowledge and experience in palliative care were insufficient”. Years of experience in cancer care (OR = 0.95; 95% CI: 0.91–1.00; p = 0.037) and pre-graduate education (OR = 0.46; 95% CI: 0.22–0.99; p = 0.048) were significantly associated with fewer challenging situations in which RDs stated, “The patient refused to eat”. However, post-graduate education was significantly associated with an increase in challenging situations, such as “Providing support to patients’ families was challenging” (OR = 2.01; 95% CI: 1.15–3.52; p = 0.015). Additionally, participation in meal rounds was associated with an increased occurrence of “I was consulted on decisions regarding the continuation or discontinuation of tube feeding, gastrostomy, or intravenous nutrition” (OR = 2.30; 95% CI: 1.40–3.79; p = 0.001) (Table 5).

Table 5.
Multivariate analysis of factors influencing challenging situations for RDs in palliative cancer care.
4. Discussion
4.1. Collaboration with the Palliative Care Team
RDs play a crucial role in providing nutritional support to cancer patients, such as addressing their dietary preferences and eating-related distress, in palliative care settings [17,18]. This study aimed to examine the responsibilities of RDs involved in palliative care, identify the challenges they encounter when working with patients, and explore the interdisciplinary collaboration systems associated with the role of RDs.
A comparison between the CC group and the AN group revealed that the presence of a dedicated RD specializing in palliative cancer care significantly enhances collaboration with the PCT. However, the proportion of dedicated RDs remains low (22%), indicating a need for more specialized RDs to provide tailored support for patients’ dietary preferences and eating-related distress [19,20,21]. Our findings suggest that hospital rounds conducted by RDs, individualized dietary counseling for inpatients, and the provision of fully personalized meals based on patient preferences are all factors associated with stronger collaboration with the PCT [22,23]. These results highlight the importance of RDs actively participating as integral members of the PCT to ensure that meals are customized according to patients’ conditions and preferences [24,25].
4.2. Ward Rounds and Challenges Faced by RDs in Palliative Care
This study underscores the significance of ward rounds as a key skill required for RDs in palliative care. During ward rounds, it is important to monitor food intake and assess various factors such as the patient’s performance status, skeletal muscle mass, levels of anxiety and depression, and degree of fatigue [26]. Incorporating these assessments into nutritional management strategies enables more comprehensive and patient-centered care [27].
RDs frequently encounter difficult situations when dealing with palliative care patients (Figure 1). Many respondents expressed an awareness of their own limitations or were troubled by their inability to provide adequate responses. Our findings suggest that reducing challenging situations for RDs in palliative care may be facilitated by providing pre-graduate training, obtaining specialized certifications in cancer care, and establishing a system that ensures meals are provided in accordance with patients’ preferences. However, participation in meal rounds and post-graduate training were associated with an increase in challenging situations. This may be due to the increased accessibility of dietitians to patients and their families, leading to a greater awareness of the complex roles and responsibilities required in palliative care [28,29]. As the number of RDs assigned to palliative care wards increases and they gain more exposure to the requests and distress of patients and families through ward rounds and nutritional guidance, RDs may experience emotional strain and a loss of confidence [11]. To prevent burnout and foster a sense of professional fulfillment, it is essential to enhance educational opportunities for less experienced and younger RDs [30,31]. Promoting multidisciplinary nutrition support and encouraging a collaborative approach in patient care are crucial steps toward achieving this goal [32,33].
4.3. Need for Specialized Training
Previous studies have reported that various factors, such as years of clinical experience, familiarity with practice guidelines, the implementation of multidimensional patient assessments, and educational background, significantly influence an RD’s role in managing cancer cachexia [11]. Moreover, research on interdisciplinary care practices in cachexia management has reported that effective collaboration alleviates physical symptoms, reduces psychological distress, enhances adherence to treatment, and supports both patients and families in adjusting to and coping with cachexia in addition to the RD’s involvement in providing guideline-based nutritional and exercise therapy [16]. Educating patients and families about cancer cachexia, as well as participating in end-of-life discussions as part of a multidisciplinary team, has been shown to strengthen RD confidence [11,34]. These studies highlight the importance of collaboration with the PCT, comprehensive patient assessments during ward rounds, and active engagement with both patients and their families in implementing comprehensive nutritional support. They are consistent with the recommendations of the present guidelines [5,6,17,18,33]. This study also found that providing psychological support to address eating-related distress is an important responsibility of the RD that requires specialized skills [35,36]. Therefore, it is important to support the training of RDs specializing in palliative care to enhance their ability to contribute effectively to multidisciplinary teams.
4.4. Study Limitations
The response rate for the survey was 63.9%, suggesting that the data likely reflect the perspectives of RDs with a strong awareness of research collaboration and the development of palliative care. Accordingly, the findings may not be fully generalizable to all dietitians involved in palliative care. Nevertheless, given that the typical response rate for anonymous mailed surveys in Japan is approximately 30%, the results of this study may indicate a meaningful trend.
Moreover, as the survey was based on the subjective experiences of RDs in Japan, future studies should incorporate international comparisons and utilize objective indicators to enhance the generalizability and reliability of the findings [37]. It is also important to acknowledge that this study did not evaluate the direct effects of the reported interventions on patients and their families. Future research should aim to assess these outcomes to better understand the potential benefits of such interventions.
Ultimately, cancer patients receiving palliative care will significantly benefit from an enhanced quality of care when RDs are effectively trained in the design and management of multidisciplinary teams [6,14]. Moreover, empowering RDs to actively engage in research on nutritional interventions in cancer care is essential to strengthening their capacity to deliver robust, evidence-based nutritional support [38].
5. Conclusions
Palliative care is a holistic approach that addresses the physical suffering of cancer patients and their psychological and psychosomatic distress. This study investigated the roles and challenges faced by RDs involved in palliative care and identified the key work responsibilities and collaborative systems that contribute to enhanced cancer patient care. The survey results suggest that RDs involved in palliative care must strengthen their collaboration with the PCT, participate in ward rounds, and engage in both pre- and post-graduate education. Furthermore, RDs often face challenging situations in patient care and recognize their own limitations, which can cause distress when they feel unable to provide an adequate response.
Successfully providing individualized meals tailored to patients’ conditions and preferences, as well as addressing eating-related distress, may contribute to a sense of professional fulfillment for RDs and help prevent burnout. It is essential to offer further educational opportunities for less experienced RDs. Establishing a robust collaborative system and fostering education for RDs to practice as integral members of a multidisciplinary PCT are important for improving care quality and supporting the well-being of both patients and healthcare providers.
Author Contributions
Conceptualization, S.K., K.A., N.M. and T.T.; methodology, S.K., K.A., M.M. and T.T.; software, S.K.; validation, A.I. and M.S.; formal analysis, S.K. and K.A.; investigation, S.K., M.M. and T.T.; resources, S.K. and T.T.; data curation, A.I. and M.S; writing—original draft preparation, S.K.; writing—review and editing, K.A., N.M., A.I., M.S. and T.T.; visualization, S.K., A.I., M.S. and M.M.; supervision, K.A. and N.M.; project administration, M.M. and T.T.; funding acquisition, S.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Medical Research Ethics Committee of Institute of Science Tokyo (approval number M2022-106, approval date 1 October 2022).
Informed Consent Statement
This study was performed following the ethical standards outlined in the Helsinki Declaration and the ethical guidelines for medical and health research involving human subjects presented by the Ministry of Health, Labor, and Welfare in Japan. Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Acknowledgments
We appreciate the administrative support provided by Naoko Shirota and Mihoko Nishimura of Tokyo Kasei Gakuin University.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
| RD | Registered dietitian |
| PCT | Palliative care team |
| CC group | Consistently collaborated group |
| AN group | Collaborated as-needed group |
References
- World Health Organization. Available online: https://www.who.int/news-room/fact-sheets/detail/palliative-care (accessed on 5 August 2020).
- Sanders, J.J.; Temin, S.; Ghoshal, A.; Alesi, E.R.; Ali, Z.V.; Chauhan, C.; Cleary, J.F.; Epstein, A.S.; Firn, J.I.; Jones, J.A.; et al. Palliative care for patients with Cancer: ASCO guideline update. J. Clin. Oncol. 2024, 42, 2336–2357. [Google Scholar] [CrossRef] [PubMed]
- Koshimoto, S.; Arimoto, M.; Saitou, K.; Uchibori, M.; Hashizume, A.; Honda, A.; Amano, K.; Nakajima, Y.; Uetake, H.; Matsushima, E. Need and demand for nutritional counselling and their association with quality of life, nutritional status and eating-related distress among patients with cancer receiving outpatient chemotherapy: A cross-sectional study. Support Care Cancer 2019, 27, 3385–3394. [Google Scholar] [CrossRef]
- Arends, J. Malnutrition in cancer patients: Causes, consequences and treatment options. Eur. J. Surg. Oncol. 2024, 50, 107074. [Google Scholar] [CrossRef]
- Arends, J.; Bachmann, P.; Baracos, V.; Barthelemy, N.; Bertz, H.; Bozzetti, F.; Fearon, K.; Hütterer, E.; Isenring, E.; Kaasa, S.; et al. ESPEN guidelines on nutrition in cancer patients. Clin. Nutr. 2017, 36, 11–48. [Google Scholar] [CrossRef]
- Roeland, E.J.; Bohlke, K.; Baracos, V.E.; Bruera, E.; Del Fabbro, E.; Dixon, S.; Fallon, M.; Herrstedt, J.; Lau, H.; Platek, M.; et al. Management of cancer cachexia: ASCO guideline. J. Clin. Oncol. 2020, 38, 2438–2453. [Google Scholar] [CrossRef] [PubMed]
- Grassi, L.; Caruso, R.; Riba, M.B.; Lloyd-Williams, M.; Kissane, D.; Rodin, G.; McFarland, D.; Campos-Ródenas, R.; Zachariae, R.; Santini, D.; et al. Anxiety and depression in adult cancer patients: ESMO Clinical Practice Guideline. ESMO Open 2023, 8, 101155. [Google Scholar] [CrossRef] [PubMed]
- De Feo, G.; Case, A.A.; Crawford, G.B.; Hui, D.; To, J.; Sbrana, A.; Alderman, B.; Mukhopadhyay, S.; Bouleuc, C.; Amano, K.; et al. Multinational Association of Supportive Care in Cancer (MASCC) guidelines: Cannabis for psychological symptoms including insomnia, anxiety, and depression. Support Care Cancer 2023, 31, 176. [Google Scholar] [CrossRef]
- Koshimoto, S.; Yamazaki, T.; Amano, K.; Kako, J.; Arimoto, M.; Saitou, K.; Hashizume, A.; Takeuchi, T.; Matsushima, E. Psychosocial factors and the need for multidisciplinary support in nutrition counselling for cancer chemotherapy patients. Nutrients 2023, 15, 2712. [Google Scholar] [CrossRef]
- Morrison-Koechl, J.; Heckman, G.; Banerjee, A.; Keller, H. Factors associated with dietitian referrals to support long-term care residents advancing towards the end of life. J. Hum. Nutr. Diet. 2024, 37, 673–684. [Google Scholar] [CrossRef]
- Koshimoto, S.; Amano, K.; Mori, N.; Oyamada, S.; Arakawa, S.; Ishiki, H.; Satomi, E.; Morita, T.; Takeuchi, T. Perspectives of registered dietitians and factors associated with their personal accomplishment in the management of cancer cachexia. Support Care Cancer 2023, 31, 124. [Google Scholar] [CrossRef]
- Amano, K.; Morita, T.; Koshimoto, S.; Uno, T.; Katayama, H.; Tatara, R. Eating-related distress in advanced cancer patients with cachexia and family members: A survey in palliative and supportive care settings. Support Care Cancer 2019, 27, 2869–2876. [Google Scholar] [CrossRef] [PubMed]
- Acreman, S. Nutrition in palliative care. Br. J. Community Nurs. 2009, 14, 427–431. [Google Scholar] [CrossRef][Green Version]
- Arends, J. Struggling with nutrition in patients with advanced cancer: Nutrition and nourishment-focusing on metabolism and supportive care. Ann. Oncol. 2018, 39 (Suppl. 2), ii27–ii34. [Google Scholar] [CrossRef] [PubMed]
- Wallin, V.; Mattsson, E.; Omerov, P.; Klarare, A. Caring for patients with eating deficiencies in palliative care-Registered nurses’ experiences: A qualitative study. J. Clin. Nurs. 2022, 31, 3165–3177. [Google Scholar] [CrossRef] [PubMed]
- Amano, K.; Arakawa, S.; Hopkinson, J.B.; Baracos, V.E.; Oyamada, S.; Koshimoto, S.; Mori, N.; Ishiki, H.; Morita, T.; Takeuchi, T.; et al. Factors associated with multimodal care practices for cancer cachexia among registered dietitians. Support Care Cancer 2024, 32, 213. [Google Scholar] [CrossRef]
- Alderman, B.; Allan, L.; Amano, K.; Bouleuc, C.; Davis, M.; Lister-Flynn, S.; Mukhopadhyay, S.; Davies, A. Multinational Association of Supportive Care in Cancer (MASCC) expert opinion/guidance on the use of clinically assisted nutrition in patients with advanced cancer. Support Care Cancer 2022, 30, 2983–2992. [Google Scholar] [CrossRef]
- Muscaritoli, M.; Arends, J.; Bachmann, P.; Baracos, V.; Barthelemy, N.; Bertz, H.; Bozzetti, F.; Hütterer, E.; Isenring, E.; Kaasa, S.; et al. ESPEN practical guideline: Clinical Nutrition in cancer. Clin. Nutr. 2021, 40, 2898–2913. [Google Scholar] [CrossRef]
- Bowers, M.; Higginson, I.J.; Maddocks, M. Patient and Carer Experiences of Cancer Cachexia and Its Management. Curr. Opin. Support. Palliat. Care 2024, 18, 132–137. [Google Scholar] [CrossRef]
- Holdoway, A. Nutrition in Palliative Care: Issues, Perceptions and Opportunities to Improve Care for Patients. Br. J. Nurs. 2022, 31, S20–S27. [Google Scholar] [CrossRef]
- Amano, K.; Koshimoto, S.; Okamura, S.; Sakaguchi, T.; Arakawa, S.; Matsuda, Y.; Tokoro, A.; Takeuchi, T.; Satomi, E.; Wada, T.; et al. Association of Systemic Inflammation with Dietary Intake, Nutrition Impact Symptoms, and Eating-Related Distress Among Patients with Advanced Cancer. Healthcare 2024, 12, 2533. [Google Scholar] [CrossRef]
- Soares, C.H.; Beuren, A.G.; Friedrich, H.J.; Gabrielli, C.P.; Stefani, G.P.; Steemburgo, T. The Importance of Nutrition in Cancer Care: A Narrative Review. Curr. Nutr. Rep. 2024, 13, 950–965. [Google Scholar] [CrossRef]
- Erickson, N.; Sulosari, V.; Sullivan, E.S.; Laviano, A.; van Ginkel-Res, A.; Remijnse, W.; Wesseling, J.; Koepcke, U.; Weber, N.; Huebner, J.; et al. Nutrition Care in Cancer: An Overlooked Part of Patient-Centered Care. Semin. Oncol. Nurs. 2025, 41, 151799. [Google Scholar] [CrossRef]
- Naito, T.; Wakabayashi, H.; Aso, S.; Konishi, M.; Saitoh, M.; Baracos, V.E.; Coats, A.J.; Anker, S.D.; Sherman, L.; Klompenhouwer, T.; et al. The Barriers to Interprofessional Care for Cancer Cachexia among Japanese Healthcare Providers: A Nationwide Survey. J. Cachexia Sarcopenia Muscle 2024, 15, 387–400. [Google Scholar] [CrossRef] [PubMed]
- Pornrattanakavee, P.; Srichan, T.; Seetalarom, K.; Saichaemchan, S.; Oer-Areemitr, N.; Prasongsook, N. Impact of Interprofessional Collaborative Practice in Palliative Care on Outcomes for Advanced Cancer Inpatients in a Resource-Limited Setting. BMC Palliat. Care 2022, 21, 229. [Google Scholar] [CrossRef]
- Hustad, K.S.; Koteng, L.H.; Urrizola, A.; Arends, J.; Bye, A.; Dajani, O.; Deliens, L.; Fallon, M.; Hjermstad, M.J.; Kohlen, M.; et al. Practical Cancer Nutrition, from Guidelines to Clinical Practice: A Digital Solution to Patient-Centred Care. ESMO Open 2025, 10, 104529. [Google Scholar] [CrossRef] [PubMed]
- Källén, E.; Nimström, S.; Rosengren, K. Content and Structure of Ward Rounds Focusing on Interprofessional Collaboration on an Internal Medicine Ward: An Observational Study of Interprofessional Collaboration. J. Interprof. Care 2021, 35, 219–226. [Google Scholar] [CrossRef]
- Schütte, K.; Middelberg-Bisping, K.; Schulz, C. Nutrition and Gastro-Enterological Support in End of Life Care. Best Pract. Res. Clin. Gastroenterol. 2020, 48–49, 101692. [Google Scholar] [CrossRef]
- Cotogni, P.; Stragliotto, S.; Ossola, M.; Collo, A.; Riso, S. The Role of Nutritional Support for Cancer Patients in Palliative Care. Nutrients 2021, 13, 306. [Google Scholar] [CrossRef]
- Chitose, H.; Kuwana, M.; Miura, T.; Inoue, M.; Nagasu, Y.; Shimizu, R.; Hattori, Y.; Uehara, Y.; Kosugi, K.; Matsumoto, Y. A Japanese Nationwide Survey of Nutritional Counseling for Cancer Patients and Risk Factors of Burnout among Registered Dietitians. Palliat. Med. Rep. 2022, 3, 211–219. [Google Scholar] [CrossRef]
- Alhaj, O.A.; Elsahoryi, N.A.; Fekih-Romdhane, F.; Wishah, M.; Sweidan, D.H.; Husain, W.; Achraf, A.; Trabelsi, K.; Hebert, J.R.; Jahrami, H. Prevalence of emotional burnout among dietitians and nutritionists: A systematic review, meta-analysis, meta-regression, and a call for action. BMC Psychol. 2024, 12, 775. [Google Scholar] [CrossRef]
- Crawford, G.B.; Dzierżanowski, T.; Hauser, K.; Larkin, P.; Luque-Blanco, A.I.; Murphy, I.; Puchalski, C.M.; Ripamonti, C.I. Care of the adult cancer patient at the end of life: ESMO Clinical Practice Guidelines. ESMO Open. 2021, 6, 100225. [Google Scholar] [CrossRef] [PubMed]
- Stone, P.; Buckle, P.; Dolan, R.; Feliu, J.; Hui, D.; Laird, B.J.A.; Maltoni, M.; Moine, S.; Morita, T.; Nabal, M.; et al. Prognostic evaluation in patients with advanced cancer in the last months of life: ESMO Clinical Practice Guideline. ESMO Open 2023, 8, 101195. [Google Scholar] [CrossRef] [PubMed]
- Baracos, V.E.; Coats, A.J.; Anker, S.D.; Sherman, L.; Klompenhouwer, T.; International Advisory Board, and Regional Advisory Boards for North America, Europe, and Japan. Identification and Management of Cancer Cachexia in Patients: Assessment of Healthcare Providers’ Knowledge and Practice Gaps. J. Cachexia Sarcopenia Muscle 2022, 13, 2683–2696. [Google Scholar] [CrossRef]
- Miles, A.; Brady, A.; Friary, P.; Sekula, J.; Wallis, C.; Jackson, B. Implementing an Interprofessional Palliative Care Education Program to Speech-Language Therapy and Dietetic Students. J. Interprof. Care 2023, 37, 964–973. [Google Scholar] [CrossRef]
- Tanaka, K.; Nakamura, S.; Narimatsu, H. Nutritional Approach to Cancer Cachexia: A Proposal for Dietitians. Nutrients 2022, 14, 345. [Google Scholar] [CrossRef] [PubMed]
- Öner, Ö.; Ayvat, P.; Gökmen, A.N. Nutritional Therapy in Palliative Care Units: A Bibliometric Analysis. Medicine 2025, 104, e41772. [Google Scholar] [CrossRef]
- Erickson, N.; Sullivan, E.S.; Kalliostra, M.; Laviano, A.; Wesseling, J. Nutrition Care Is an Integral Part of Patient-Centered Medical Care: A European Consensus. Med. Oncol. 2023, 40, 112. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).