TP53 Mutation Predicts Worse Survival and Earlier Local Progression in Patients with Hepatocellular Carcinoma Treated with Transarterial Embolization
Abstract
1. Introduction
2. Materials and Methods
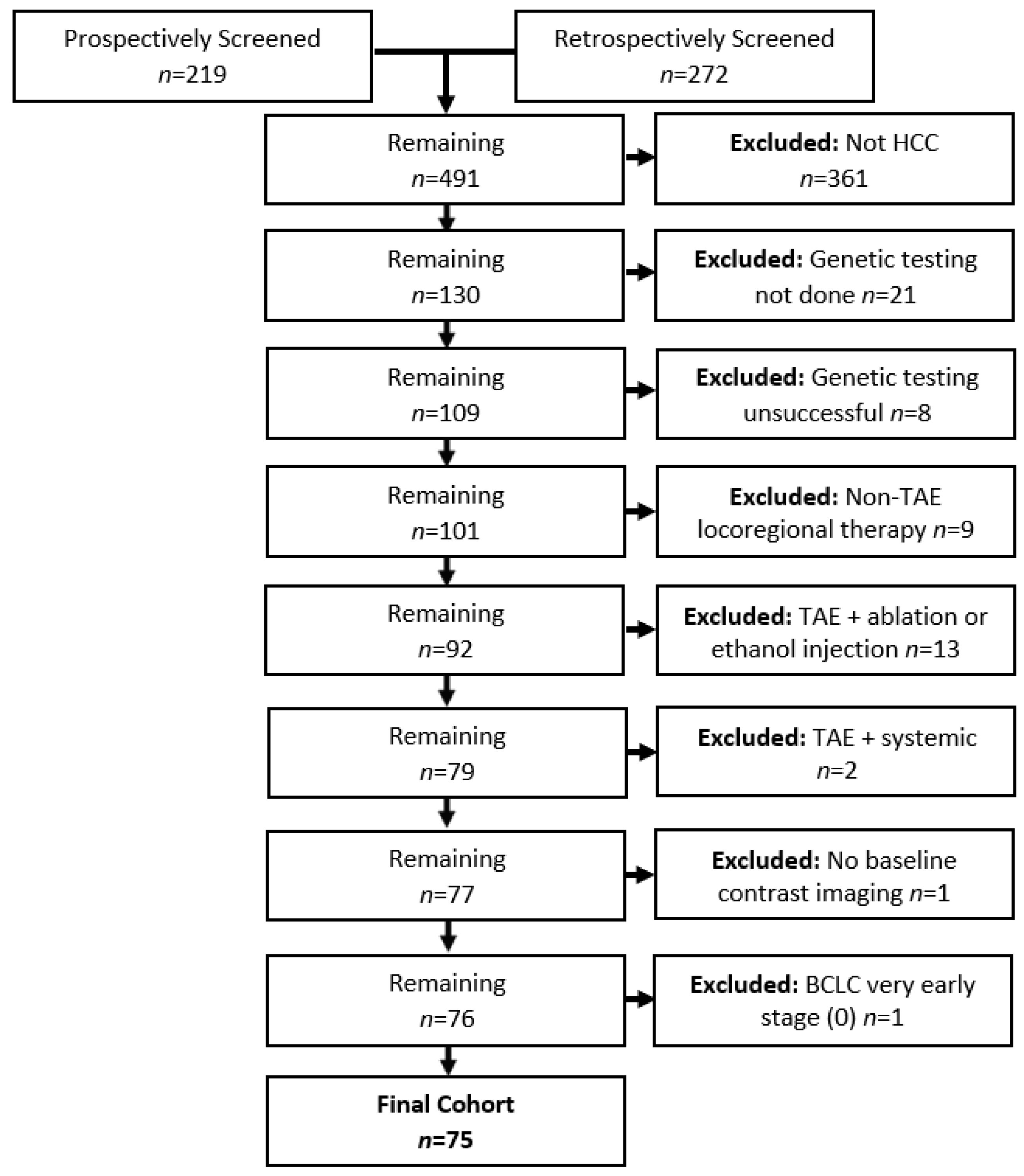
2.1. Patients
2.2. Transarterial Embolization Procedure
2.3. Data Collection
2.4. Genetic Analysis
2.5. Outcome Assessment
2.6. Statistical Analysis
3. Results
3.1. Patient Characteristics
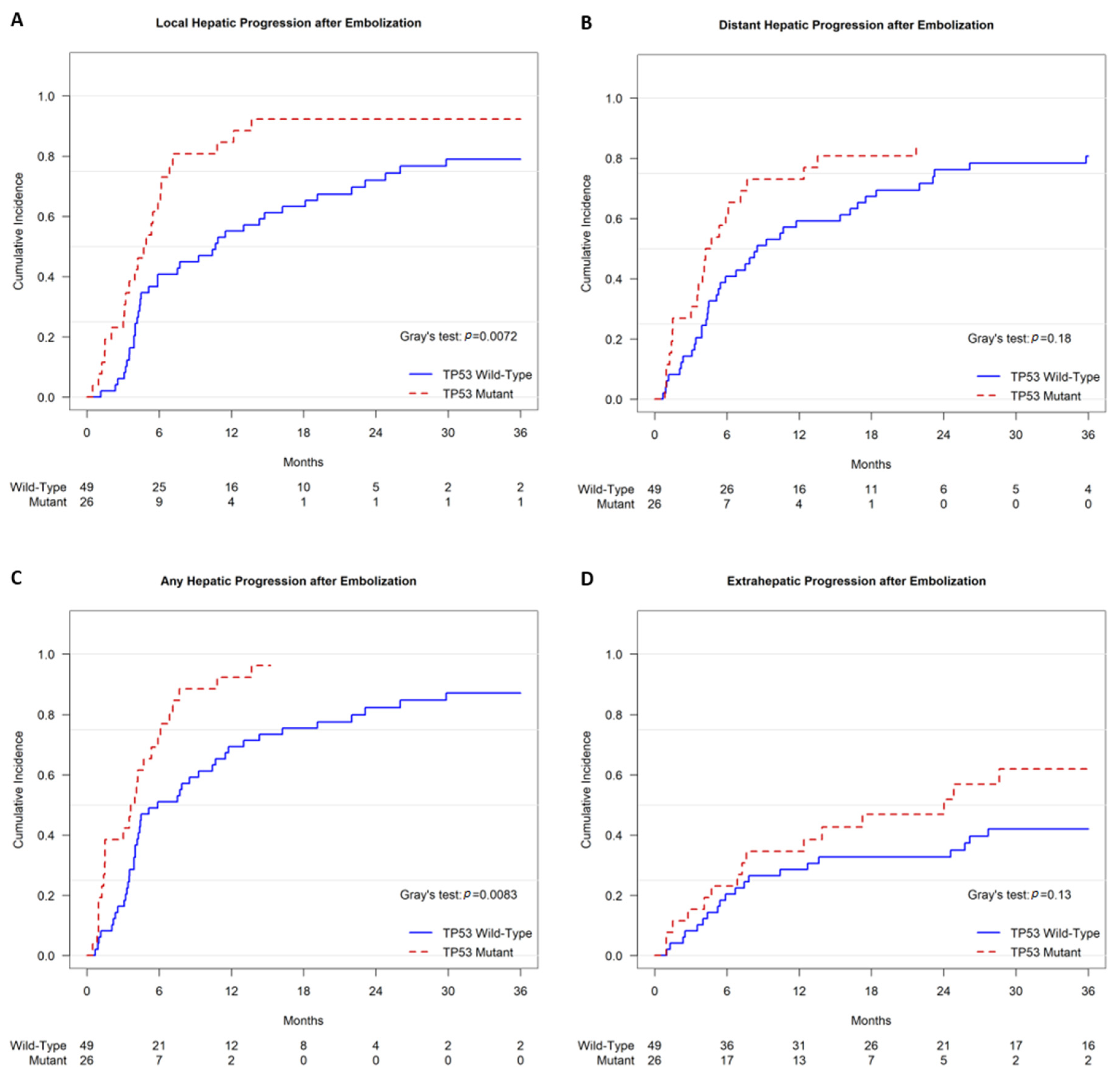
3.2. Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Parkin, D.M.; Pineros, M.; Znaor, A.; Bray, F. Cancer statistics for the year 2020: An overview. Int. J. Cancer 2021, 149, 778–789. [Google Scholar] [CrossRef]
- Kim, E.; Sher, A.; Abboud, G.; Schwartz, M.; Facciuto, M.; Tabrizian, P.; Knesaurek, K.; Fischman, A.; Patel, R.; Nowakowski, S.; et al. Radiation segmentectomy for curative intent of unresectable very early to early stage hepatocellular carcinoma (RASER): A single-centre, single-arm study. Lancet Gastroenterol. Hepatol. 2022, 7, 843–850. [Google Scholar] [CrossRef] [PubMed]
- Reig, M.; Forner, A.; Rimola, J.; Ferrer-Fabrega, J.; Burrel, M.; Garcia-Criado, A.; Kelley, R.K.; Galle, P.R.; Mazzaferro, V.; Salem, R.; et al. BCLC strategy for prognosis prediction and treatment recommendation: The 2022 update. J. Hepatol. 2022, 76, 681–693. [Google Scholar] [CrossRef] [PubMed]
- De la Garza-Ramos, C.; Montazeri, S.A.; Croome, K.P.; LeGout, J.D.; Sella, D.M.; Cleary, S.; Burns, J.; Mathur, A.K.; Overfield, C.J.; Frey, G.T.; et al. Radiation Segmentectomy for the Treatment of Solitary Hepatocellular Carcinoma: Outcomes Compared with Those of Surgical Resection. J. Vasc. Interv. Radiol. 2022, 33, 775–785.e2. [Google Scholar] [CrossRef]
- Belghiti, J.; Kianmanesh, R. Surgical treatment of hepatocellular carcinoma. HPB 2005, 7, 42–49. [Google Scholar] [CrossRef] [PubMed]
- European Association for the Study of the Liver; European Organisation for Research and Treatment of Cancer. EASL-EORTC clinical practice guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2012, 56, 908–943. [Google Scholar] [CrossRef] [PubMed]
- Brown, K.T.; Do, R.K.; Gonen, M.; Covey, A.M.; Getrajdman, G.I.; Sofocleous, C.T.; Jarnagin, W.R.; D‘Angelica, M.I.; Allen, P.J.; Erinjeri, J.P.; et al. Randomized Trial of Hepatic Artery Embolization for Hepatocellular Carcinoma Using Doxorubicin-Eluting Microspheres Compared With Embolization With Microspheres Alone. J. Clin. Oncol. 2016, 34, 2046–2053. [Google Scholar] [CrossRef] [PubMed]
- Roth, G.S.; Benhamou, M.; Teyssier, Y.; Seigneurin, A.; Abousalihac, M.; Sengel, C.; Seror, O.; Ghelfi, J.; Ganne-Carrie, N.; Blaise, L.; et al. Comparison of Trans-Arterial Chemoembolization and Bland Embolization for the Treatment of Hepatocellular Carcinoma: A Propensity Score Analysis. Cancers 2021, 13, 812. [Google Scholar] [CrossRef]
- Marelli, L.; Stigliano, R.; Triantos, C.; Senzolo, M.; Cholongitas, E.; Davies, N.; Tibballs, J.; Meyer, T.; Patch, D.W.; Burroughs, A.K. Transarterial therapy for hepatocellular carcinoma: Which technique is more effective? A systematic review of cohort and randomized studies. Cardiovasc. Interv. Radiol. 2007, 30, 6–25. [Google Scholar] [CrossRef]
- Erinjeri, J.P.; Salhab, H.M.; Covey, A.M.; Getrajdman, G.I.; Brown, K.T. Arterial patency after repeated hepatic artery bland particle embolization. J. Vasc. Interv. Radiol. 2010, 21, 522–526. [Google Scholar] [CrossRef] [PubMed]
- Yarmohammadi, H.; Gonzalez-Aguirre, A.J.; Maybody, M.; Ziv, E.; Boas, F.E.; Erinjeri, J.P.; Sofocleous, C.T.; Solomon, S.B.; Getrajdman, G. Evaluation of the Effect of Operator Experience on Outcome of Hepatic Artery Embolization of Hepatocellular Carcinoma in a Tertiary Cancer Center. Acad. Radiol. 2018, 25, 856–860. [Google Scholar] [CrossRef] [PubMed]
- Ilagan, C.H.; Goldman, D.A.; Gonen, M.; Aveson, V.G.; Babicky, M.; Balachandran, V.P.; Drebin, J.A.; Jarnagin, W.R.; Wei, A.C.; Kingham, T.P.; et al. Recurrence of Hepatocellular Carcinoma After Complete Radiologic Response to Trans-Arterial Embolization: A Retrospective Study on Patterns, Treatments, and Prognoses. Ann. Surg. Oncol. 2022, 29, 6815–6826. [Google Scholar] [CrossRef] [PubMed]
- Ziv, E.; Yarmohammadi, H.; Boas, F.E.; Petre, E.N.; Brown, K.T.; Solomon, S.B.; Solit, D.; Reidy, D.; Erinjeri, J.P. Gene Signature Associated with Upregulation of the Wnt/beta-Catenin Signaling Pathway Predicts Tumor Response to Transarterial Embolization. J. Vasc. Interv. Radiol. 2017, 28, 349–355.e1. [Google Scholar] [CrossRef][Green Version]
- Ziv, E.; Zhang, Y.; Kelly, L.; Nikolovski, I.; Boas, F.E.; Erinjeri, J.P.; Cai, L.; Petre, E.N.; Brody, L.A.; Covey, A.M.; et al. NRF2 Dysregulation in Hepatocellular Carcinoma and Ischemia: A Cohort Study and Laboratory Investigation. Radiology 2020, 297, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Harding, J.J.; Khalil, D.N.; Abou-Alfa, G.K. Biomarkers: What Role Do They Play (If Any) for Diagnosis, Prognosis and Tumor Response Prediction for Hepatocellular Carcinoma? Dig. Dis. Sci. 2019, 64, 918–927. [Google Scholar] [CrossRef] [PubMed]
- Zehir, A.; Benayed, R.; Shah, R.H.; Syed, A.; Middha, S.; Kim, H.R.; Srinivasan, P.; Gao, J.; Chakravarty, D.; Devlin, S.M.; et al. Mutational landscape of metastatic cancer revealed from prospective clinical sequencing of 10,000 patients. Nat. Med. 2017, 23, 703–713. [Google Scholar] [CrossRef] [PubMed]
- Singal, A.G.; Llovet, J.M.; Yarchoan, M.; Mehta, N.; Heimbach, J.K.; Dawson, L.A.; Jou, J.H.; Kulik, L.M.; Agopian, V.G.; Marrero, J.A.; et al. AASLD Practice Guidance on prevention, diagnosis, and treatment of hepatocellular carcinoma. Hepatology 2023, 78, 1922–1965. [Google Scholar] [CrossRef] [PubMed]
- Ally, A.; Balasundaram, M.; Carlsen, R.; Chuah, E.; Clarke, A.; Dhalla, N.; Holt, R.A.; Jones, S.J.; Lee, D.; Ma, Y.; et al. Comprehensive and Integrative Genomic Characterization of Hepatocellular Carcinoma. Cell 2017, 169, 1327–1341.e23. [Google Scholar] [CrossRef] [PubMed]
- Schulze, K.; Imbeaud, S.; Letouze, E.; Alexandrov, L.B.; Calderaro, J.; Rebouissou, S.; Couchy, G.; Meiller, C.; Shinde, J.; Soysouvanh, F.; et al. Exome sequencing of hepatocellular carcinomas identifies new mutational signatures and potential therapeutic targets. Nat. Genet. 2015, 47, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Nault, J.C.; Martin, Y.; Caruso, S.; Hirsch, T.Z.; Bayard, Q.; Calderaro, J.; Charpy, C.; Copie-Bergman, C.; Ziol, M.; Bioulac-Sage, P.; et al. Clinical Impact of Genomic Diversity From Early to Advanced Hepatocellular Carcinoma. Hepatology 2020, 71, 164–182. [Google Scholar] [CrossRef]
- Ahn, S.M.; Jang, S.J.; Shim, J.H.; Kim, D.; Hong, S.M.; Sung, C.O.; Baek, D.; Haq, F.; Ansari, A.A.; Lee, S.Y.; et al. Genomic portrait of resectable hepatocellular carcinomas: Implications of RB1 and FGF19 aberrations for patient stratification. Hepatology 2014, 60, 1972–1982. [Google Scholar] [CrossRef] [PubMed]
- Nault, J.C.; De Reynies, A.; Villanueva, A.; Calderaro, J.; Rebouissou, S.; Couchy, G.; Decaens, T.; Franco, D.; Imbeaud, S.; Rousseau, F.; et al. A hepatocellular carcinoma 5-gene score associated with survival of patients after liver resection. Gastroenterology 2013, 145, 176–187. [Google Scholar] [CrossRef] [PubMed]
- Villanueva, A.; Hoshida, Y.; Battiston, C.; Tovar, V.; Sia, D.; Alsinet, C.; Cornella, H.; Liberzon, A.; Kobayashi, M.; Kumada, H.; et al. Combining clinical, pathology, and gene expression data to predict recurrence of hepatocellular carcinoma. Gastroenterology 2011, 140, 1501–1512.e2. [Google Scholar] [CrossRef] [PubMed]
- Borgheresi, A.; Covey, A.; Yarmohammadi, H.; Boas, F.E.; Ziv, E.; Getrajdman, G.; Erinjeri, J.; Jarnagin, W.; Harding, J.J.; D‘Angelica, M.; et al. Embolization with microspheres alone for hepatocellular carcinoma with portal vein tumor: Analysis of outcome and liver function at disease progression. HPB 2020, 22, 588–594. [Google Scholar] [CrossRef] [PubMed]
- Cheng, D.T.; Mitchell, T.N.; Zehir, A.; Shah, R.H.; Benayed, R.; Syed, A.; Chandramohan, R.; Liu, Z.Y.; Won, H.H.; Scott, S.N.; et al. Memorial Sloan Kettering-Integrated Mutation Profiling of Actionable Cancer Targets (MSK-IMPACT): A Hybridization Capture-Based Next-Generation Sequencing Clinical Assay for Solid Tumor Molecular Oncology. J. Mol. Diagn. 2015, 17, 251–264. [Google Scholar] [CrossRef] [PubMed]
- Baerlocher, M.O.; Nikolic, B.; Sze, D.Y. Adverse Event Classification: Clarification and Validation of the Society of Interventional Radiology Specialty-Specific System. J. Vasc. Interv. Radiol. 2022, 34, S1051-0443. [Google Scholar] [CrossRef] [PubMed]
- Gray, R.J. A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann. Stat. 1988, 16, 1141–1154. [Google Scholar] [CrossRef]
- R-Core-Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021. [Google Scholar]
- Boyault, S.; Rickman, D.S.; de Reynies, A.; Balabaud, C.; Rebouissou, S.; Jeannot, E.; Herault, A.; Saric, J.; Belghiti, J.; Franco, D.; et al. Transcriptome classification of HCC is related to gene alterations and to new therapeutic targets. Hepatology 2007, 45, 42–52. [Google Scholar] [CrossRef] [PubMed]
- Wolfel, G.; Ostheim, E.; Staub, A.; Tumen, D.; Heumann, P.; Schmid, S.; Schlosser, S.; Muller, M.; Gulow, K.; Kunst, C. The p53 Family of Transcription Factors Represses the Alpha- fetoprotein Gene Expression in Hepatocellular Carcinoma. J. Gastrointestin. Liver Dis. 2023, 32, 346–355. [Google Scholar] [CrossRef] [PubMed]
- Peng, S.Y.; Chen, W.J.; Lai, P.L.; Jeng, Y.M.; Sheu, J.C.; Hsu, H.C. High alpha-fetoprotein level correlates with high stage, early recurrence and poor prognosis of hepatocellular carcinoma: Significance of hepatitis virus infection, age, p53 and beta-catenin mutations. Int. J. Cancer 2004, 112, 44–50. [Google Scholar] [CrossRef]
- Xue, M.; Wu, Y.; Fan, W.; Guo, J.; Wei, J.; Wang, H.; Tan, J.; Wang, Y.; Yao, W.; Zhao, Y.; et al. Prognostic Value of TP53 Mutation for Transcatheter Arterial Chemoembolization Failure/Refractoriness in HBV-Related Advanced Hepatocellular Carcinoma. Cancer Res. Treat. 2020, 52, 925–937. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Yim, S.Y.; Jeong, Y.S.; Li, Q.X.; Kang, S.H.; Sohn, B.H.; Kumar, S.V.; Shin, J.H.; Choi, Y.R.; Shim, J.J.; et al. Consensus subtypes of hepatocellular carcinoma associated with clinical outcomes and genomic phenotypes. Hepatology 2022, 76, 1634–1648. [Google Scholar] [CrossRef]
- Kamat, C.D.; Green, D.E.; Warnke, L.; Thorpe, J.E.; Ceriello, A.; Ihnat, M.A. Mutant p53 facilitates pro-angiogenic, hyperproliferative phenotype in response to chronic relative hypoxia. Cancer Lett. 2007, 249, 209–219. [Google Scholar] [CrossRef] [PubMed]
- Ravi, R.; Mookerjee, B.; Bhujwalla, Z.M.; Sutter, C.H.; Artemov, D.; Zeng, Q.; Dillehay, L.E.; Madan, A.; Semenza, G.L.; Bedi, A. Regulation of tumor angiogenesis by p53-induced degradation of hypoxia-inducible factor 1alpha. Genes Dev 2000, 14, 34–44. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Lou, T. Hypoxia inducible factors in hepatocellular carcinoma. Oncotarget 2017, 8, 46691–46703. [Google Scholar] [CrossRef] [PubMed]
- Xia, L.; Mo, P.; Huang, W.; Zhang, L.; Wang, Y.; Zhu, H.; Tian, D.; Liu, J.; Chen, Z.; Zhang, Y.; et al. The TNF-alpha/ROS/HIF-1-induced upregulation of FoxMI expression promotes HCC proliferation and resistance to apoptosis. Carcinogenesis 2012, 33, 2250–2259. [Google Scholar] [CrossRef] [PubMed]
- Meng, M.; Zhong, K.; Jiang, T.; Liu, Z.; Kwan, H.Y.; Su, T. The current understanding on the impact of KRAS on colorectal cancer. Biomed. Pharmacother. 2021, 140, 111717. [Google Scholar] [CrossRef] [PubMed]
- Boerner, T.; Drill, E.; Pak, L.M.; Nguyen, B.; Sigel, C.S.; Doussot, A.; Shin, P.; Goldman, D.A.; Gonen, M.; Allen, P.J.; et al. Genetic Determinants of Outcome in Intrahepatic Cholangiocarcinoma. Hepatology 2021, 74, 1429–1444. [Google Scholar] [CrossRef] [PubMed]
- Zhao, K.; Erinjeri, J.P.; Sotirchos, V.S.; Alexander, E.S.; Moussa, A.M.; Marinelli, B.; Ziv, E.; Sofocleous, C.T.; Abou-Alfa, G.K.; Jarnagin, W.R.; et al. Factors affecting outcomes of Yttrium-90 radioembolization in heavily pretreated patients with intrahepatic cholangiocarcinoma. Abdom. Radiol. 2023, 48, 2434–2442. [Google Scholar] [CrossRef] [PubMed]
- Tanabe, M.; Kanki, A.; Wolfson, T.; Costa, E.A.; Mamidipalli, A.; Ferreira, M.P.; Santillan, C.; Middleton, M.S.; Gamst, A.C.; Kono, Y.; et al. Imaging Outcomes of Liver Imaging Reporting and Data System Version 2014 Category 2, 3, and 4 Observations Detected at CT and MR Imaging. Radiology 2016, 281, 129–139. [Google Scholar] [CrossRef]
- Elmohr, M.; Elsayes, K.M.; Chernyak, V. LI-RADS: Review and updates. Clin. Liver Dis. 2021, 17, 108–112. [Google Scholar] [CrossRef] [PubMed]


| Characteristic | All Patients (n = 75) | TP53 Mutant (n = 26) | TP53 Wild-Type (n = 49) | p-Value |
|---|---|---|---|---|
| Age, Median (IQR), Years | 70.0 (62.0–76.3) | 69.4 (64.5–74.5) | 70.0 (60.7–76.9) | 0.925 |
| Male Gender, No (%) | 63 | 23 (88.5) | 40 (81.6) | 0.526 |
| Ethnicity, No (%) | 0.340 | |||
| White | 57 | 19 (73.1) | 38 (77.6) | |
| Asian | 7 | 2 (7.7) | 5 (10.2) | |
| Black | 5 | 1 (3.8) | 4 (8.2) | |
| Other | 2 | 2 (7.7) | 0 | |
| Unknown | 4 | 2 (7.7) | 2 (4.1) | |
| Other Primary Cancer | 8 (30.8) | 8 (16.3) | 0.134 | |
| Etiology, No (%) | 0.982 | |||
| Hepatitis B | 6 | 3 (11.5) | 3 (6.1) | |
| Hepatitis C | 27 | 8 (30.8) | 19 (38.8) | |
| Steatohepatitis | 12 | 4 (15.4) | 8 (16.3) | |
| Alcohol | 6 | 3 (11.5) | 3 (6.1) | |
| Other | 4 | 1 (3.8) | 3 (6.1) | |
| Multiple | 7 | 3 (11.5) | 4 (8.2) | |
| Unknown | 13 | 4 (15.4) | 9 (18.4) | |
| ECOG PS, No (%) | 0.060 | |||
| 0 | 54 | 15 (57.7) | 39 (79.6) | |
| 1 or 2 | 21 | 11 (42.3) | 10 (20.4) | |
| Prior HCC Treatment, No (%) | 17 | 3 (11.5) | 14 (28.6) | 0.339 |
| Surgery | 12 | 2 (7.7) | 10 (20.4) | |
| Image-guided Locoregional | 6 | 1 (3.8) | 5 (10.2) | |
| Systemic | 2 | 1 (3.8) | 1 (2) | |
| Child–Pugh Class, No (%) | 0.658 | |||
| A (Score 5–6) | 69 | 25 (96.1) | 44 (89.8) | |
| B (Score 7–11) | 6 | 1 (3.8) | 5 (10.2) | |
| ALBI Grade, No (%) | 0.757 | |||
| Grade 1 (Score ≤ −2.60) | 39 | 15 (57.7) | 24 (49) | |
| Grade 2 (−2.60 < Score ≤ −1.39) | 35 | 11 (42.3) | 24 (49) | |
| Grade 3 (−1.39 < Score) | 1 | 0 | 1 (2) | |
| BCLC Stage, No (%) | 0.007 | |||
| A or B | 40 | 8 (30.8) | 32 (65.3) | |
| C | 35 | 18 (69.2) | 17 (34.7) | |
| AFP, Median (IQR), ng/mL | 16.5 (6–296.6) | 18.4 (5.7–685.2) | 15.3 (7.1–166.3) | 0.297 |
| Histologic Grade, No (%) * | 0.011 | |||
| Well or Moderately Differentiated | 59 (78.7) | 16 (61.5) | 43 (87.8) | |
| Poorly Differentiated | 6 (8) | 5 (19.2) | 1 (2) |
| Characteristic | All Patients (n = 75) | TP53 Mutant (n = 26) | TP53 Wild-Type (n = 49) | p-Value |
|---|---|---|---|---|
| Lesion Number, No (%) | 0.811 | |||
| Single | 18 | 5 (19.2) | 13 (26.5) | |
| ≤3 | 40 | 13 (50) | 27 (55.1) | |
| >3 | 35 | 13 (50) | 22 (44.9) | |
| Bilobar Disease | 38 | 15 (57.7) | 23 (46.9) | 0.472 |
| Lesion Diameter, Median (IQR), cm | 5.8 (3.9–8.7) | 7.9 (4.2–9.3) | 5.8 (3.6–6.4) | 0.261 |
| Macrovascular Invasion, No (%) | 15 | 9 (34.6) | 6 (12.2) | 0.018 |
| Extrahepatic Disease, No (%) | 5 | 3 (11.5) | 2 (4.1) | 0.334 |
| Imaging Response at 1 Month Follow-Up | All Patients (n = 75) | TP53 Mutant (n = 26) | TP53 Wild-Type (n = 49) | p-Value |
|---|---|---|---|---|
| Complete Response | 36 | 11 | 25 | 0.628 |
| Partial Response | 34 | 11 | 23 | 0.809 |
| Stable Disease | 0 | 0 | 0 | - |
| Progressive Disease | 5 | 4 | 1 | 0.042 |
| Univariate Cox Analysis | |||
|---|---|---|---|
| HR | 95% CI | p-Value | |
| TP53 Status (Wild-Type vs. Mutant) | 0.55 | 0.32–0.93 | 0.025 |
| AFP (ng/mL) (≤200 vs. >200) | 0.32 | 0.18–0.56 | <0.001 |
| ECOG PS (0 vs. 1 or 2) | 0.46 | 0.26–0.82 | 0.008 |
| BCLC Stage (A or B vs. C) | 0.47 | 0.28–0.81 | 0.004 |
| Lesion Size (≤3 cm vs. >3 cm) | 0.50 | 0.24–1.01 | 0.053 |
| ALBI Grade (1 vs. >1) | 0.94 | 0.57–1.56 | 0.815 |
| Child–Pugh Class (A vs. B) | 0.62 | 0.26–1.45 | 0.266 |
| Tumor Number | |||
| (1 vs. >1) | 0.43 | 0.22–0.84 | 0.013 |
| (≤3 vs. >3) | 0.65 | 0.39–1.08 | 0.093 |
| Tumor Distribution (Unilobar vs. Bilobar) | 0.61 | 0.37–1.02 | 0.057 |
| Baseline Macrovascular Invasion (No vs. Yes) | 0.61 | 0.34–1.12 | 0.111 |
| Histologic Grade (Well or Moderately Differentiated vs. Poorly Differentiated) | 0.76 | 0.32–1.79 | 0.529 |
| Initial mRECIST Response (CR vs. not CR) | 0.54 | 0.33–0.9 | 0.015 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, K.; Karimi, A.; Kelly, L.; Petre, E.; Marinelli, B.; Alexander, E.S.; Sotirchos, V.S.; Erinjeri, J.P.; Covey, A.; Sofocleous, C.T.; et al. TP53 Mutation Predicts Worse Survival and Earlier Local Progression in Patients with Hepatocellular Carcinoma Treated with Transarterial Embolization. Curr. Oncol. 2025, 32, 51. https://doi.org/10.3390/curroncol32010051
Zhao K, Karimi A, Kelly L, Petre E, Marinelli B, Alexander ES, Sotirchos VS, Erinjeri JP, Covey A, Sofocleous CT, et al. TP53 Mutation Predicts Worse Survival and Earlier Local Progression in Patients with Hepatocellular Carcinoma Treated with Transarterial Embolization. Current Oncology. 2025; 32(1):51. https://doi.org/10.3390/curroncol32010051
Chicago/Turabian StyleZhao, Ken, Anita Karimi, Luke Kelly, Elena Petre, Brett Marinelli, Erica S. Alexander, Vlasios S. Sotirchos, Joseph P. Erinjeri, Anne Covey, Constantinos T. Sofocleous, and et al. 2025. "TP53 Mutation Predicts Worse Survival and Earlier Local Progression in Patients with Hepatocellular Carcinoma Treated with Transarterial Embolization" Current Oncology 32, no. 1: 51. https://doi.org/10.3390/curroncol32010051
APA StyleZhao, K., Karimi, A., Kelly, L., Petre, E., Marinelli, B., Alexander, E. S., Sotirchos, V. S., Erinjeri, J. P., Covey, A., Sofocleous, C. T., Harding, J. J., Jarnagin, W., Sigel, C., Vakiani, E., Ziv, E., & Yarmohammadi, H. (2025). TP53 Mutation Predicts Worse Survival and Earlier Local Progression in Patients with Hepatocellular Carcinoma Treated with Transarterial Embolization. Current Oncology, 32(1), 51. https://doi.org/10.3390/curroncol32010051






