Nonspecific Signs and/or Symptoms of Cancer: A Retrospective, Observational Analysis from a Secondary Care, US Community Oncology Dataset
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Study Cohort
2.3. Outcomes and Statistical Analysis
3. Results
3.1. Patient Disposition
3.2. Patient Demographics
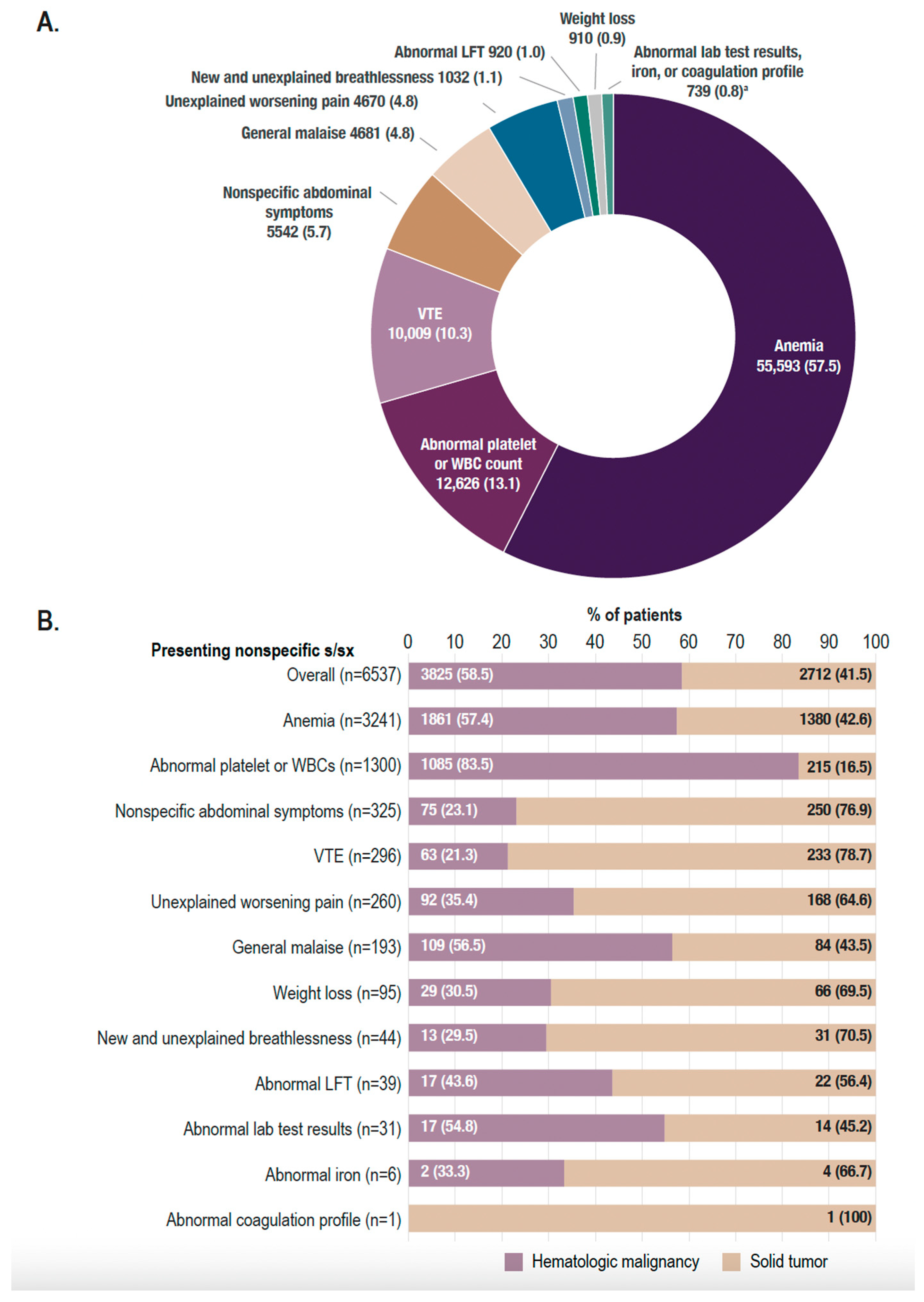
3.3. Clinical Characteristics
3.4. Clinical Outcomes
3.5. Time to Diagnosis in Secondary Care
3.6. Healthcare Resource Utilization
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cancer Statistics-NCI [Internet]. 2020. Available online: https://www.cancer.gov/about-cancer/understanding/statistics (accessed on 7 March 2024).
- Neal, R.D.; Tharmanathan, P.; France, B.; Din, N.U.; Cotton, S.; Fallon-Ferguson, J.; Hamilton, W.; Hendry, A.; Hendry, M.; Lewis, R.; et al. Is increased time to diagnosis and treatment in symptomatic cancer associated with poorer outcomes? Systematic review. Br. J. Cancer 2015, 112, S92–S107. [Google Scholar] [CrossRef]
- World Health Organization. Guide to Cancer Early Diagnosis [Internet]; World Health Organization: Geneva, Switzerland, 2017; Available online: https://www.who.int/publications/i/item/9789241511940 (accessed on 7 March 2024).
- Asymptomatic Multi-Cancer Detection-NCI [Internet]. 2022. Available online: https://www.cancer.gov/research/annual-plan/2024-annual-plan-budget-proposal.pdf (accessed on 7 March 2024).
- Sarma, E.A.; Kobrin, S.C.; Thompson, M.J. A Proposal to Improve the Early Diagnosis of Symptomatic Cancers in the United States. Cancer Prev. Res. 2020, 13, 715–720. [Google Scholar] [CrossRef]
- Koo, M.M.; Hamilton, W.; Walter, F.M.; Rubin, G.P.; Lyratzopoulos, G. Symptom Signatures and Diagnostic Timeliness in Cancer Patients: A Review of Current Evidence. Neoplasia 2018, 20, 165–174. [Google Scholar] [CrossRef]
- Singh, H.; Meyer, A.N.; Thomas, E.J. The frequency of diagnostic errors in outpatient care: Estimations from three large observational studies involving US adult populations. BMJ Qual. Saf. 2014, 23, 727–731. [Google Scholar] [CrossRef]
- Kostopoulou, O.; Delaney, B.C.; Munro, C.W. Diagnostic difficulty and error in primary care—A systematic review. Fam. Pract. 2008, 25, 400–413. [Google Scholar] [CrossRef]
- Pearson, C.; Poirier, V.; Fitzgerald, K.; Rubin, G.; Hamilton, W. Cross-sectional study using primary care and cancer registration data to investigate patients with cancer presenting with non-specific symptoms. BMJ Open 2020, 10, e033008. [Google Scholar] [CrossRef]
- Bosch, X.; Mota Gomes, T.; Montori-Palacin, E.; Moreno, P.; López-Soto, A. Time to Diagnosis and Presenting Symptoms of Patients Diagnosed with Cancer through Emergency and Nonemergency Routes: A Large Retrospective Study from a High-Volume Center. JCO Oncol. Pract. 2024. [Google Scholar]
- Ingeman, M.L.; Christensen, M.B.; Bro, F.; Knudsen, S.T.; Vedsted, P. The Danish cancer pathway for patients with serious non-specific symptoms and signs of cancer–a cross-sectional study of patient characteristics and cancer probability. BMC Cancer 2015, 15, 421. [Google Scholar] [CrossRef]
- Damhus, C.S.; Siersma, V.; Birkmose, A.R.; Dalton, S.O.; Brodersen, J. Use and diagnostic outcomes of cancer patient pathways in Denmark–is the place of initial diagnostic work-up an important factor? BMC Health Serv. Res. 2022, 22, 130. [Google Scholar] [CrossRef]
- Dolly, S.O.; Jones, G.; Allchorne, P.; Wheeler, D.; Ali, S.; Mukadam, Y.; Zheng, S.; Rahman, L.; Sindhar, J.; Moss, C.L.; et al. The effectiveness of the Guy’s Rapid Diagnostic Clinic (RDC) in detecting cancer and serious conditions in vague symptom patients. Br. J. Cancer 2021, 124, 1079–1087. [Google Scholar] [CrossRef]
- American Society of Clinical Oncology. The State of Cancer Care in America, 2017: A Report by the American Society of Clinical Oncology. J. Oncol. Pract. 2017, 13, e353–e394. [Google Scholar] [CrossRef]
- Software: Surveillance Research Program, National Cancer Institute SEER*Stat Software Version 8.4.3. [Internet]. Surveillance, Epidemiology, and end Results SEER*Stat Software. Available online: www.seer.cancer.gov/seerstat (accessed on 23 January 2024).
- Nicholson, B.D.; Thompson, M.J.; Hobbs, F.D.R.; Nguyen, M.; McLellan, J.; Green, B.; Chubak, J.; Oke, J.L. Measured weight loss as a precursor to cancer diagnosis: Retrospective cohort analysis of 43 302 primary care patients. J. Cachexia Sarcopenia Muscle 2022, 13, 2492–2503. [Google Scholar] [CrossRef]
- Jones, R.; Latinovic, R.; Charlton, J.; Gulliford, M.C. Alarm symptoms in early diagnosis of cancer in primary care: Cohort study using General Practice Research Database. BMJ 2007, 334, 1040. [Google Scholar] [CrossRef]
- Jellema, P.; Van der Windt, D.A.; Bruinvels, D.J.; Mallen, C.D.; van Weyenberg, S.J.; Mulder, C.J.; de Vet, H.C. Value of symptoms and additional diagnostic tests for colorectal cancer in primary care: Systematic review and meta-analysis. BMJ 2010, 340, c1269. [Google Scholar] [CrossRef]
- Väyrynen, J.P.; Tuomisto, A.; Väyrynen, S.A.; Klintrup, K.; Karhu, T.; Mäkelä, J.; Herzig, K.H.; Karttunen, T.J.; Mäkinen, M.J. Preoperative anemia in colorectal cancer: Relationships with tumor characteristics, systemic inflammation, and survival. Sci. Rep. 2018, 8, 1126. [Google Scholar] [CrossRef]
- Walter, F.M.; Rubin, G.; Bankhead, C.; Morris, H.C.; Hall, N.; Mills, K.; Dobson, C.; Rintoul, R.C.; Hamilton, W.; Emery, J. Symptoms and other factors associated with time to diagnosis and stage of lung cancer: A prospective cohort study. Br. J. Cancer 2015, 112 (Suppl. S1), S6–S13. [Google Scholar] [CrossRef]
- Howell, D.A.; Smith, A.G.; Jack, A.; Patmore, R.; Macleod, U.; Mironska, E.; Roman, E. Time-to-diagnosis and symptoms of myeloma, lymphomas and leukaemias: A report from the Haematological Malignancy Research Network. BMC Hematol. 2013, 13, 9. [Google Scholar] [CrossRef]
- Nicholson, B.D.; Aveyard, P.; Koshiaris, C.; Perera, R.; Hamilton, W.; Oke, J.; Hobbs, F.R. Combining simple blood tests to identify primary care patients with unexpected weight loss for cancer investigation: Clinical risk score development, internal validation, and net benefit analysis. PLoS Med. 2021, 18, e1003728. [Google Scholar] [CrossRef]
- Hippisley-Cox, J.; Coupland, C. Identifying patients with suspected colorectal cancer in primary care: Derivation and validation of an algorithm. Br. J. Gen. Pract. J. R. Coll. Gen. Pract. 2012, 62, e29–e37. [Google Scholar] [CrossRef]
- Savage, R.; Messenger, M.; Neal, R.D.; Ferguson, R.; Johnston, C.; Lloyd, K.L.; Neal, M.D.; Sansom, N.; Selby, P.; Sharma, N.; et al. Development and validation of multivariable machine learning algorithms to predict risk of cancer in symptomatic patients referred urgently from primary care: A diagnostic accuracy study. BMJ Open 2022, 12, e053590. [Google Scholar] [CrossRef]
- Palmirotta, R.; Lovero, D.; Cafforio, P.; Felici, C.; Mannavola, F.; Pellè, E.; Quaresmini, D.; Tucci, M.; Silvestris, F. Liquid biopsy of cancer: A multimodal diagnostic tool in clinical oncology. Ther. Adv. Med. Oncol. 2018, 10, 1758835918794630. [Google Scholar] [CrossRef]
- Marrugo-Ramírez, J.; Mir, M.; Samitier, J. Blood-Based Cancer Biomarkers in Liquid Biopsy: A Promising Non-Invasive Alternative to Tissue Biopsy. Int. J. Mol. Sci. 2018, 19, 2877. [Google Scholar] [CrossRef] [PubMed]
- Klein, E.A.; Richards, D.; Cohn, A.; Tummala, M.; Lapham, R.; Cosgrove, D.; Chung, G.; Clement, J.; Gao, J.; Hunkapiller, N.; et al. Clinical validation of a targeted methylation-based multi-cancer early detection test using an independent validation set. Ann. Oncol. 2021, 32, 1167–1177. [Google Scholar] [CrossRef]
- Nicholson, B.D.; Oke, J.; Virdee, P.S.; Harris, D.A.; O’Doherty, C.; Park, J.E.; Hamady, Z.; Sehgal, V.; Millar, A.; Medley, L.; et al. Multi-cancer early detection test in symptomatic patients referred for cancer investigation in England and Wales (SYMPLIFY): A large-scale, observational cohort study. Lancet Oncol. 2023, 24, 733–743. [Google Scholar] [CrossRef] [PubMed]

| Inclusion/Exclusion Criteria | Patients Remaining |
|---|---|
| Patients with ≥1 nonspecific signs and/or symptoms from their iKM EHR problem list within The US Oncology Network between 1 January 2016, and 31 December 2020 | 251,704 |
| Above visit is their first visit for nonspecific signs and/or symptoms between 1 January 2016, and 31 December 2020 | 232,559 |
| Patients ≥40 years of age at visit with nonspecific signs and/or symptoms (index date) | 201,163 |
| Patients ≥1 additional vital visit within 12 months after the index visit | 170,874 |
| Exclude patients with a documented diagnosis of any cancer (excluding basal cell carcinoma and squamous cell carcinoma skin cancer) in iKM EHR within 3 years on or prior to the index date | 104,002 |
| Exclude patients with erroneous data | 103,984 |
| Overall (N = 103,984) | Patients with Only 1 Presenting Nonspecific Sign and/or Symptom (n = 96,722) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anemia (n = 55,593) | Abnormal Platelet or WBC Counts (n = 12,626) | VTE (n = 10,009) | Nonspecific Abdominal Symptoms (n = 5542) | General Malaise (n = 4681) | Unexplained Worsening Pain (n = 4670) | New/Unexplained Breathlessness (n = 1032) | Abnormal Liver Function Test (n = 920) | Weight Loss (n = 910) | Abnormal Lab Test Results (n = 537) | Abnormal Iron (n = 149) | Abnormal Coagulation Profile (n = 53) | ||
| Age | |||||||||||||
| Mean (SD) | 64.9 (13.4) | 65.5 (14.0) | 64.7 (12.8) | 62.6 (12.2) | 64.2 (12.0) | 64.9 (12.9) | 64.6 (11.9) | 67.1 (11.8) | 61.8 (11.3) | 69.4 (12.1) | 63.0 (12.0) | 62.5 (12.0) | 61.3 (12.5) |
| ≥65 years, n (%) | 53,875 (51.8) | 30,273 (54.5) | 6364 (50.4) | 4329 (43.3) | 2694 (48.6) | 2339 (50.0) | 2309 (49.4) | 597 (57.8) | 369 (40.1) | 597 (65.6) | 239 (44.5) | 63 (42.3) | 25 (47.2) |
| Sex, n (%) | |||||||||||||
| Female | 67,004 (64.4) | 38,143 (68.6) | 6912 (54.7) | 5176 (51.7) | 3897 (70.3) | 3069 (65.6) | 3051 (65.3) | 652 (63.2) | 522 (56.7) | 495 (54.4) | 334 (62.2) | 99 (66.4) | 31 (58.5) |
| Race, n (%) | |||||||||||||
| White | 67,154 (64.6) | 34,054 (61.3) | 8811 (69.8) | 6419 (64.1) | 3981 (71.8) | 3450 (73.7) | 3281 (70.3) | 769 (74.5) | 654 (71.1) | 595 (65.4) | 363 (67.6) | 91 (61.1) | 36 (67.9) |
| Black | 14,788 (14.2) | 9516 (17.1) | 1016 (8.0) | 1391 (13.9) | 453 (8.2) | 466 (10.0) | 472 (10.1) | 78 (7.6) | 47 (5.1) | 149 (16.4) | 79 (14.7) | 13 (8.7) | 3 (5.7) |
| Asian | 2305 (2.2) | 1238 (2.2) | 344 (2.7) | 77 (0.8) | 143 (2.6) | 63 (1.3) | 123 (2.6) | 37 (3.6) | 47 (5.1) | 14 (1.5) | 17 (3.2) | 11 (7.4) | 2 (3.8) |
| Native American | 297 (0.3) | 146 (0.3) | 39 (0.3) | 11 (0.1) | 33 (0.6) | 18 (0.4) | 18 (0.4) | 3 (0.3) | 2 (0.2) | 0 (0.00) | 1 (0.2) | 0 (0.00) | 0 (0.00) |
| Other | 2350 (2.3) | 1346 (2.4) | 265 (2.1) | 186 (1.9) | 104 (1.9) | 74 (1.6) | 112 (2.4) | 24 (2.3) | 23 (2.5) | 20 (2.2) | 9 (1.7) | 14 (9.4) | 2 (3.8) |
| Not documented | 17,090 (16.4) | 9293 (16.7) | 2151 (17.0) | 1925 (19.2) | 828 (14.9) | 610 (13.0) | 664 (14.2) | 121 (11.7) | 147 (16.0) | 132 (14.5) | 68 (12.7) | 20 (13.4) | 10 (18.9) |
| Practice region, n (%) a | |||||||||||||
| South | 50,115 (48.2) | 29,674 (53.4) | 4801 (38.0) | 4276 (42.7) | 2035 (36.7) | 2828 (60.4) | 1862 (39.9) | 367 (35.6) | 220 (23.9) | 355 (39.0) | 348 (64.8) | 11 (7.4) | 9 (17.0) |
| West | 30,749 (29.6) | 13,368 (24.0) | 4974 (39.4) | 3172 (31.7) | 2311 (41.7) | 988 (21.1) | 2066 (44.2) | 419 (40.6) | 567 (61.6) | 246 (27.0) | 127 (23.7) | 131 (87.9) | 40 (75.5) |
| Midwest | 17,212 (16.6) | 9434 (17.0) | 2005 (15.9) | 1795 (17.9) | 964 (17.4) | 645 (13.8) | 579 (12.4) | 195 (18.9) | 94 (10.2) | 233 (25.6) | 37 (6.9) | 3 (2.0) | 1 (1.9) |
| Northeast | 5908 (5.7) | 3117 (5.6) | 846 (6.7) | 766 (7.7) | 232 (4.2) | 220 (4.7) | 163 (3.5) | 51 (4.9) | 39 (4.2) | 76 (8.4) | 25 (4.7) | 4 (2.7) | 3 (5.7) |
| Smoking status, n (%) | |||||||||||||
| Never | 48,321 (46.5) | 26,725 (48.1) | 5082 (40.3) | 5042 (50.4) | 2590 (46.7) | 2083 (44.5) | 1939 (41.5) | 444 (43.0) | 455 (49.5) | 357 (39.2) | 187 (34.8) | 76 (51.0) | 24 (45.3) |
| Former | 30,323 (29.2) | 16,481 (29.6) | 3567 (28.3) | 2875 (28.7) | 1648 (29.7) | 1226 (26.2) | 1238 (26.5) | 364 (35.3) | 306 (33.3) | 300 (33.0) | 101 (18.8) | 48 (32.2) | 16 (30.2) |
| Current | 8637 (8.3) | 3797 (6.8) | 1754 (13.9) | 699 (7.0) | 471 (8.5) | 365 (7.8) | 467 (10.0) | 74 (7.2) | 71 (7.7) | 165 (18.1) | 45 (8.4) | 17 (11.4) | 6 (11.3) |
| Not documented | 16,703 (16.1) | 8590 (15.5) | 2223 (17.6) | 1393 (13.9) | 833 (15.0) | 1007 (21.5) | 1026 (22.0) | 150 (14.5) | 88 (9.6) | 88 (9.7) | 204 (38.0) | 8 (5.4) | 7 (13.2) |
| BMI (kg/m2) group, n (%) | |||||||||||||
| Obese (BMI ≥ 30) | 42,099 (40.5) | 22,334 (40.2) | 5238 (41.5) | 4988 (49.8) | 1850 (33.4) | 1770 (37.8) | 1838 (39.4) | 384 (37.2) | 341 (37.1) | 113 (12.4) | 230 (42.8) | 47 (31.5) | 29 (54.7) |
| Overweight (BMI = 25–29.9) | 29,549 (28.4) | 15,564 (28.0) | 3690 (29.2) | 2712 (27.1) | 1707 (30.8) | 1449 (31.0) | 1415 (30.3) | 297 (28.8) | 297 (32.3) | 215 (23.6) | 165 (30.7) | 42 (28.2) | 11 (20.8) |
| Normal (BMI = 18.5–24.9) | 23,766 (22.9) | 13,081 (23.5) | 2761 (21.9) | 1293 (12.9) | 1590 (28.7) | 1140 (24.4) | 1096 (23.5) | 262 (25.4) | 220 (23.9) | 442 (48.6) | 107 (19.9) | 45 (30.2) | 10 (18.9) |
| Underweight (BMI < 18.5) | 1469 (1.4) | 777 (1.4) | 149 (1.2) | 50 (0.5) | 124 (2.2) | 70 (1.5) | 63 (1.3) | 16 (1.6) | 12 (1.3) | 70 (7.7) | 5 (0.9) | 3 (2.0) | 0 (0.00) |
| Not Documented | 7101 (6.8) | 3837 (6.9) | 788 (6.2) | 966 (9.7) | 271 (4.9) | 252 (5.4) | 258 (5.5) | 73 (7.1) | 50 (5.4) | 70 (7.7) | 30 (5.6) | 12 (8.1) | 3 (5.7) |
| Months of follow-up | |||||||||||||
| Mean (SD) | 20.0 (17.7) | 19.9 (17.6) | 18.7 (19.0) | 19.8 (17.8) | 22.0 (18.0) | 21.6 (15.6) | 23.2 (17.0) | 22.5 (17.9) | 23.4 (19.8) | 17.2 (16.0) | 19.0 (16.8) | 20.3 (19.0) | 16.6 (20.5) |
| Number of Patients Presenting with Only 1 Nonspecific Sign and/or Symptom | Number of Patients Diagnosed with Cancer | Proportion of Patients Diagnosed with Cancer | |
|---|---|---|---|
| Anemia | 55,593 | 3363 | 6.0% |
| Abnormal platelet or WBC counts | 12,626 | 1329 | 10.5% |
| VTE | 10,009 | 309 | 3.1% |
| Nonspecific abdominal symptoms | 5542 | 337 | 6.1% |
| General malaise | 4681 | 203 | 4.3% |
| Unexplained worsening pain | 4670 | 275 | 5.9% |
| New/unexplained breathlessness | 1032 | 45 | 4.4% |
| Abnormal liver function test | 920 | 40 | 4.3% |
| Weight loss | 910 | 102 | 11.2% |
| Abnormal lab test results | 537 | 33 | 6.1% |
| Abnormal iron | 149 | 6 | 4.0% |
| Abnormal coagulation profile | 53 | 1 | 1.9% |
| Patients Diagnosed with 1 Primary Cancer (n = 6537) | |
|---|---|
| Primary hematologic malignancy, n (%) | 3825 (58.5) |
| Myeloid neoplasm a | 1911 (28.2) |
| Lymphoma | 1147 (16.9) |
| Plasma cell neoplasm | 678 (10) |
| Lymphoid leukemia | 89 (1.3) |
| Primary solid tumor, n (%) | 2712 (41.5) |
| Lower gastrointestinal | 470 (7.2) |
| Genitourinary | 412 (6.3) |
| Respiratory | 395 (6.0) |
| Upper gastrointestinal | 373 (5.7) |
| Breast | 350 (5.4) |
| Other b | 301 (4.6) |
| Gynecologic | 296 (4.5) |
| Melanoma | 66 (1.0) |
| Head and neck | 49 (0.7) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benton, C.B.; He, D.; Todoroff, K.; Coignet, M.V.; Luan, Y.; Wong, J.C.; Kurtzman, K.N.; Zackon, I. Nonspecific Signs and/or Symptoms of Cancer: A Retrospective, Observational Analysis from a Secondary Care, US Community Oncology Dataset. Curr. Oncol. 2024, 31, 3643-3656. https://doi.org/10.3390/curroncol31070268
Benton CB, He D, Todoroff K, Coignet MV, Luan Y, Wong JC, Kurtzman KN, Zackon I. Nonspecific Signs and/or Symptoms of Cancer: A Retrospective, Observational Analysis from a Secondary Care, US Community Oncology Dataset. Current Oncology. 2024; 31(7):3643-3656. https://doi.org/10.3390/curroncol31070268
Chicago/Turabian StyleBenton, Christopher B., Ding He, Karen Todoroff, Marie V. Coignet, Ying Luan, Jason C. Wong, Kathryn N. Kurtzman, and Ira Zackon. 2024. "Nonspecific Signs and/or Symptoms of Cancer: A Retrospective, Observational Analysis from a Secondary Care, US Community Oncology Dataset" Current Oncology 31, no. 7: 3643-3656. https://doi.org/10.3390/curroncol31070268
APA StyleBenton, C. B., He, D., Todoroff, K., Coignet, M. V., Luan, Y., Wong, J. C., Kurtzman, K. N., & Zackon, I. (2024). Nonspecific Signs and/or Symptoms of Cancer: A Retrospective, Observational Analysis from a Secondary Care, US Community Oncology Dataset. Current Oncology, 31(7), 3643-3656. https://doi.org/10.3390/curroncol31070268





