A Comprehensive Review and Insights into the New Entity of Differentiated High-Grade Thyroid Carcinoma
Abstract
1. Introduction
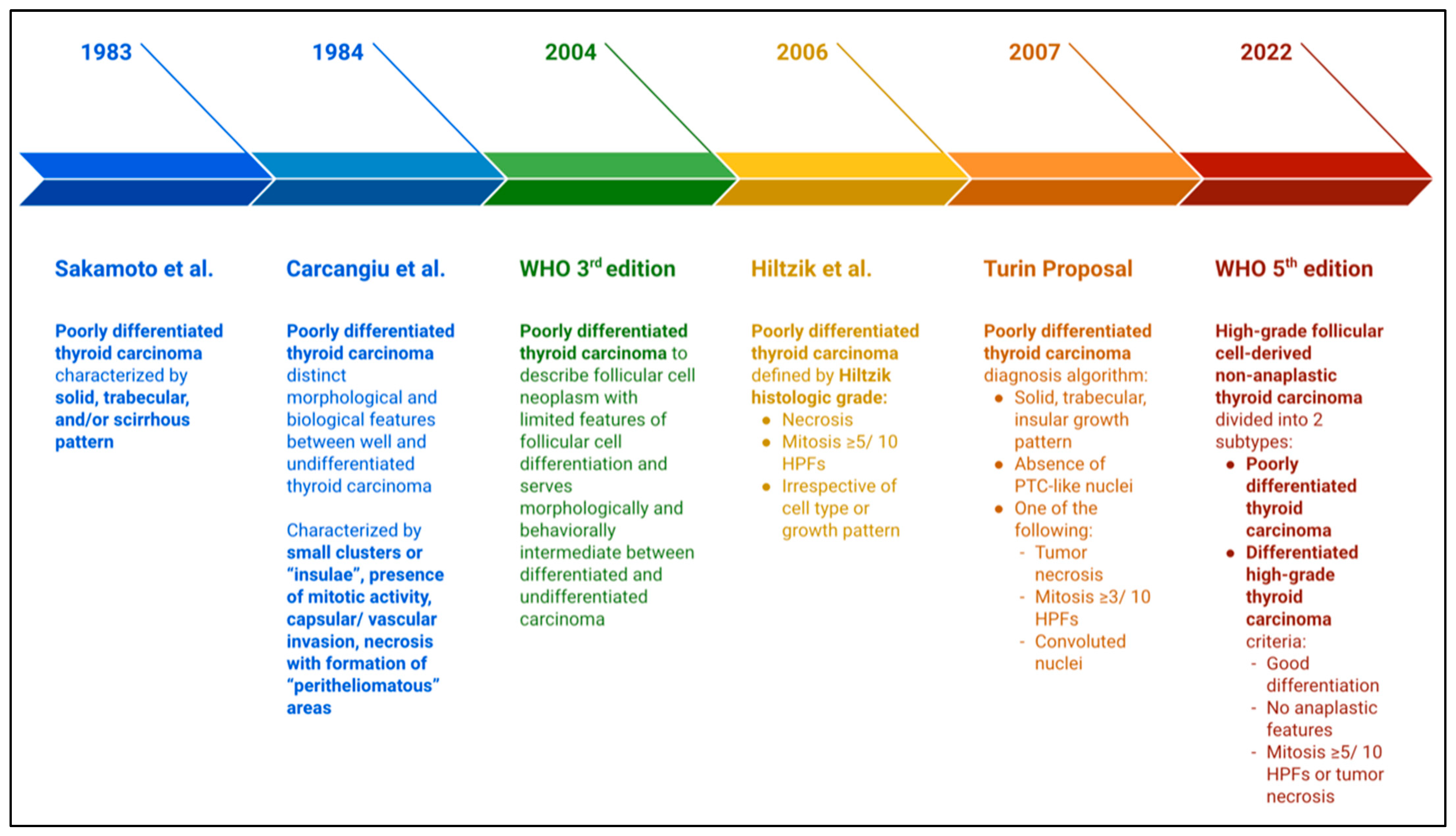
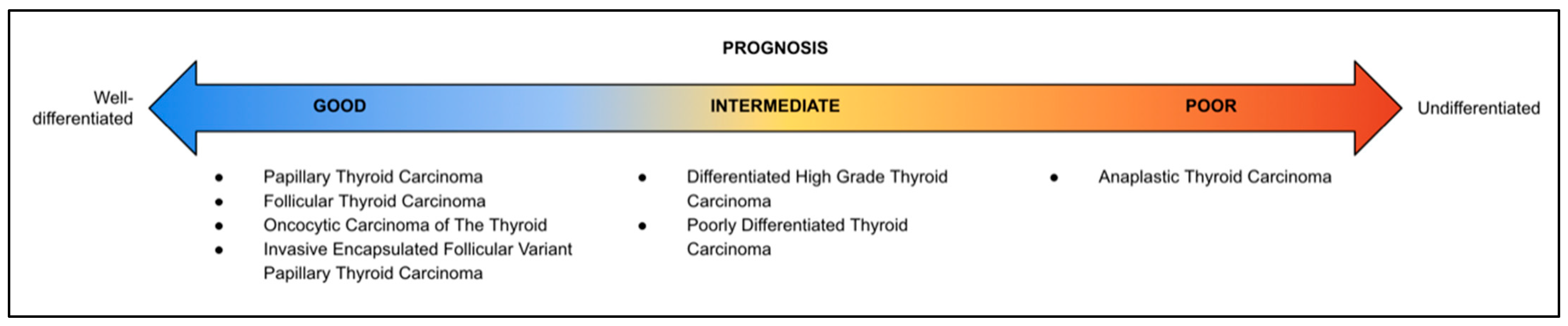
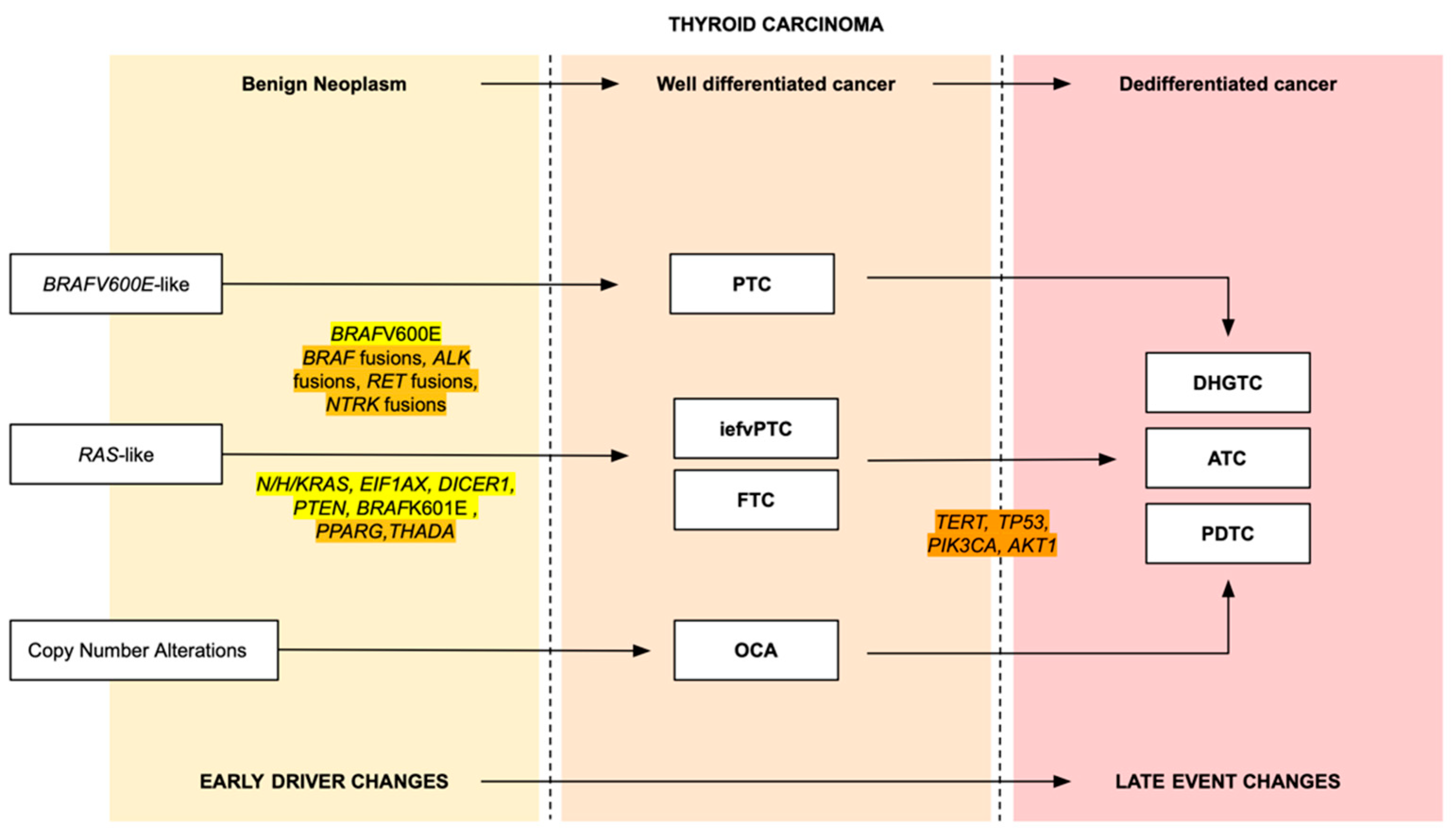
2. The New Classification of Malignant Thyroid Carcinoma
3. Diagnosis
3.1. Macroscopic Features
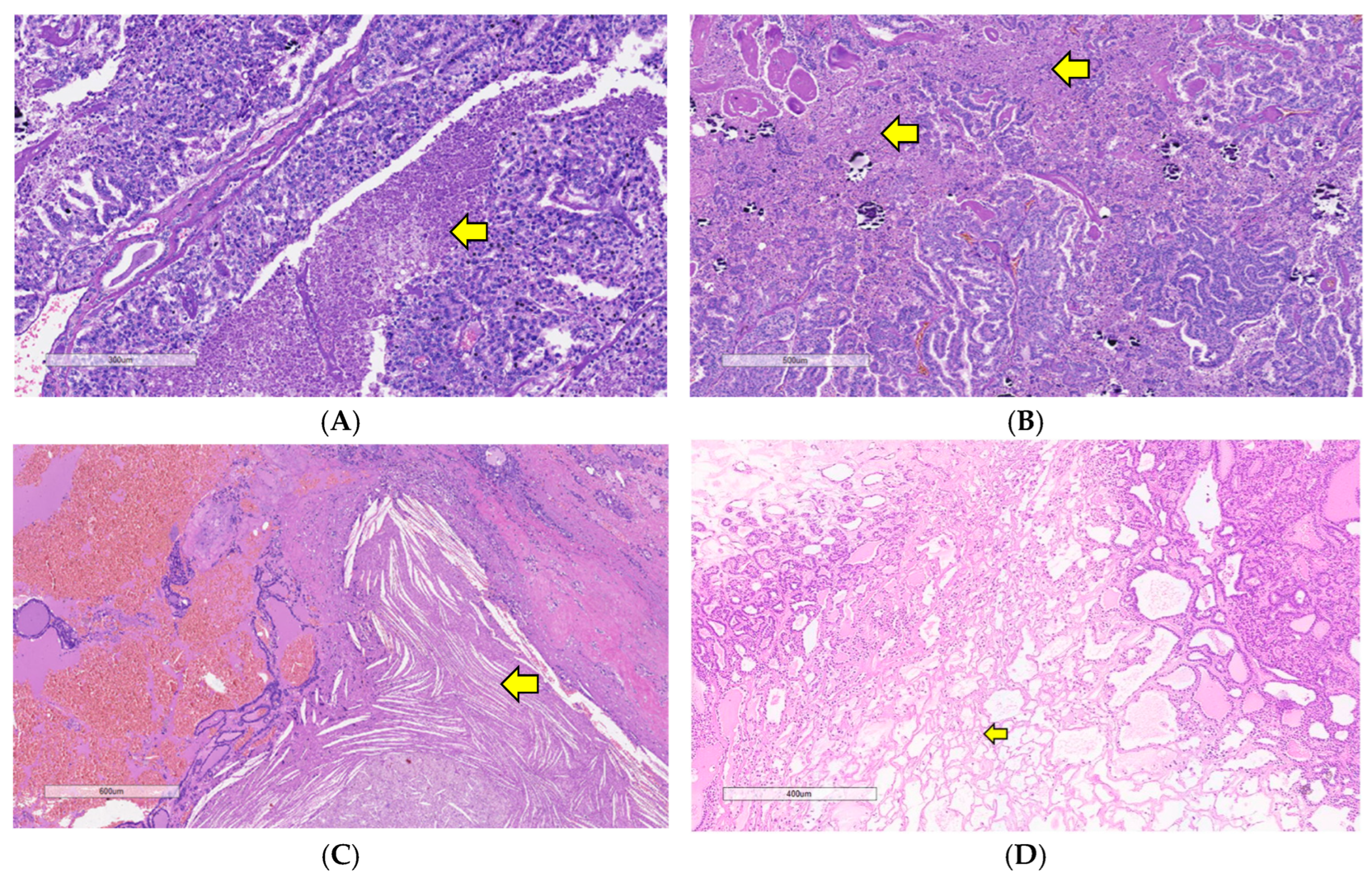
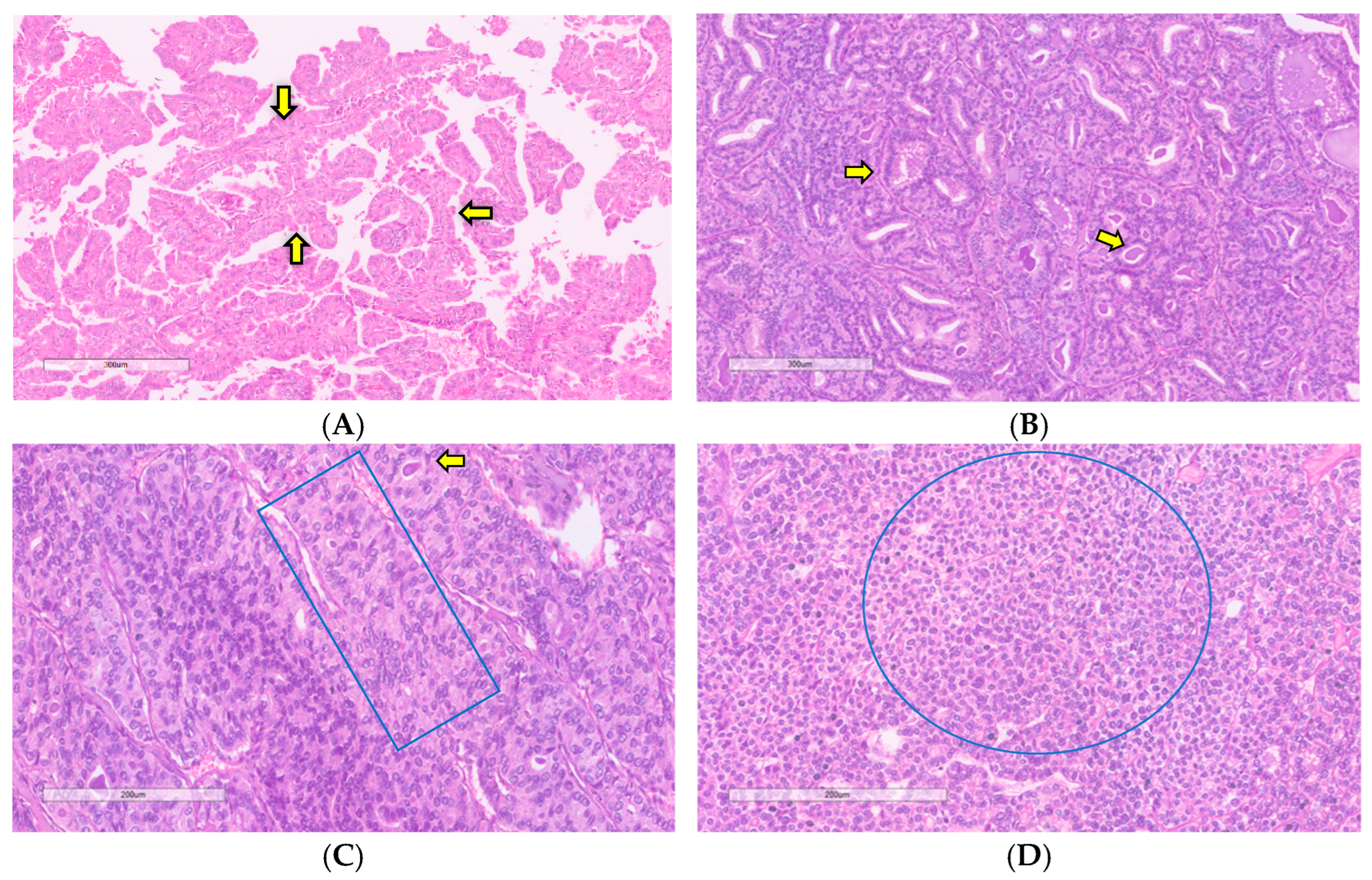
3.2. Microscopic Features
3.2.1. Necrosis
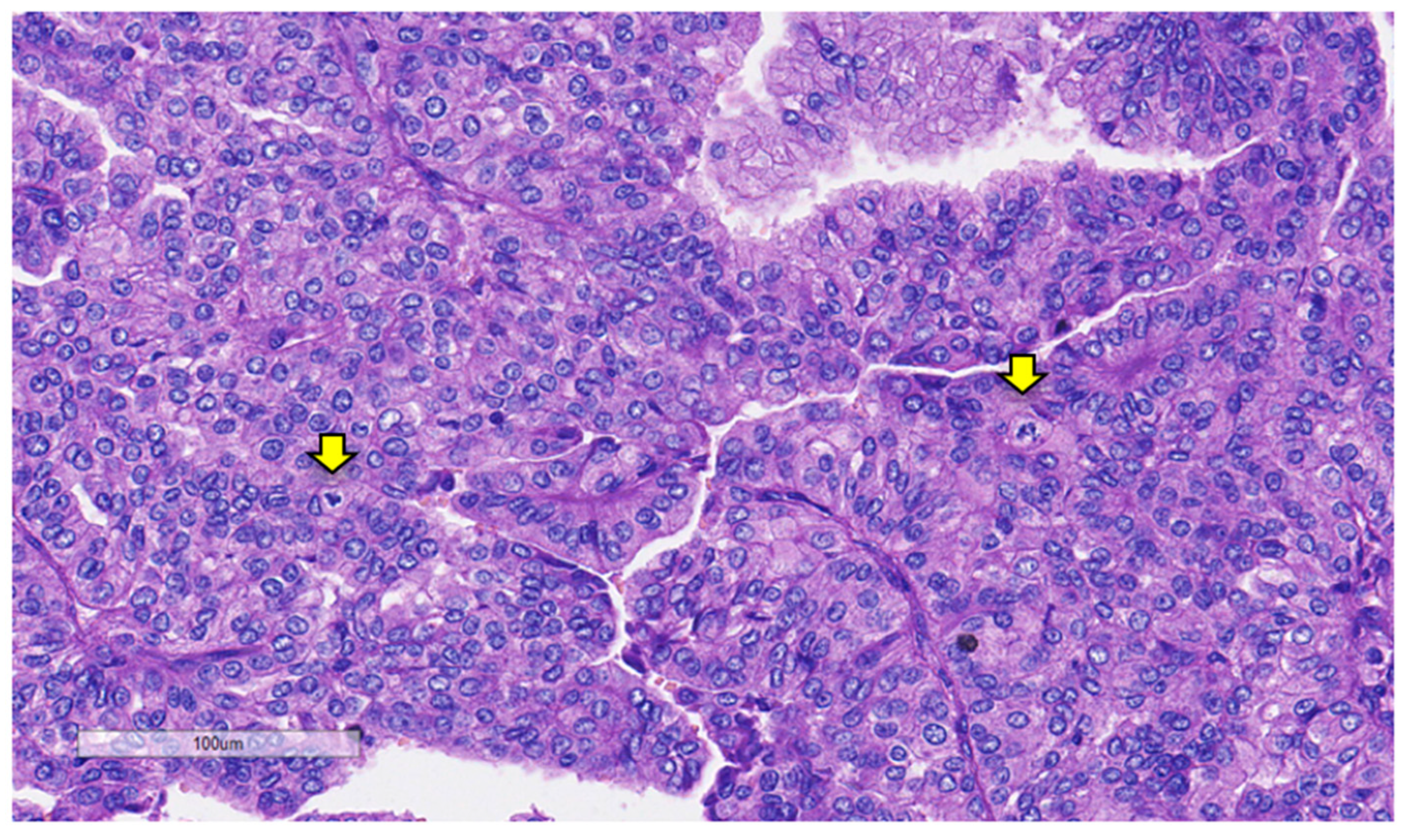
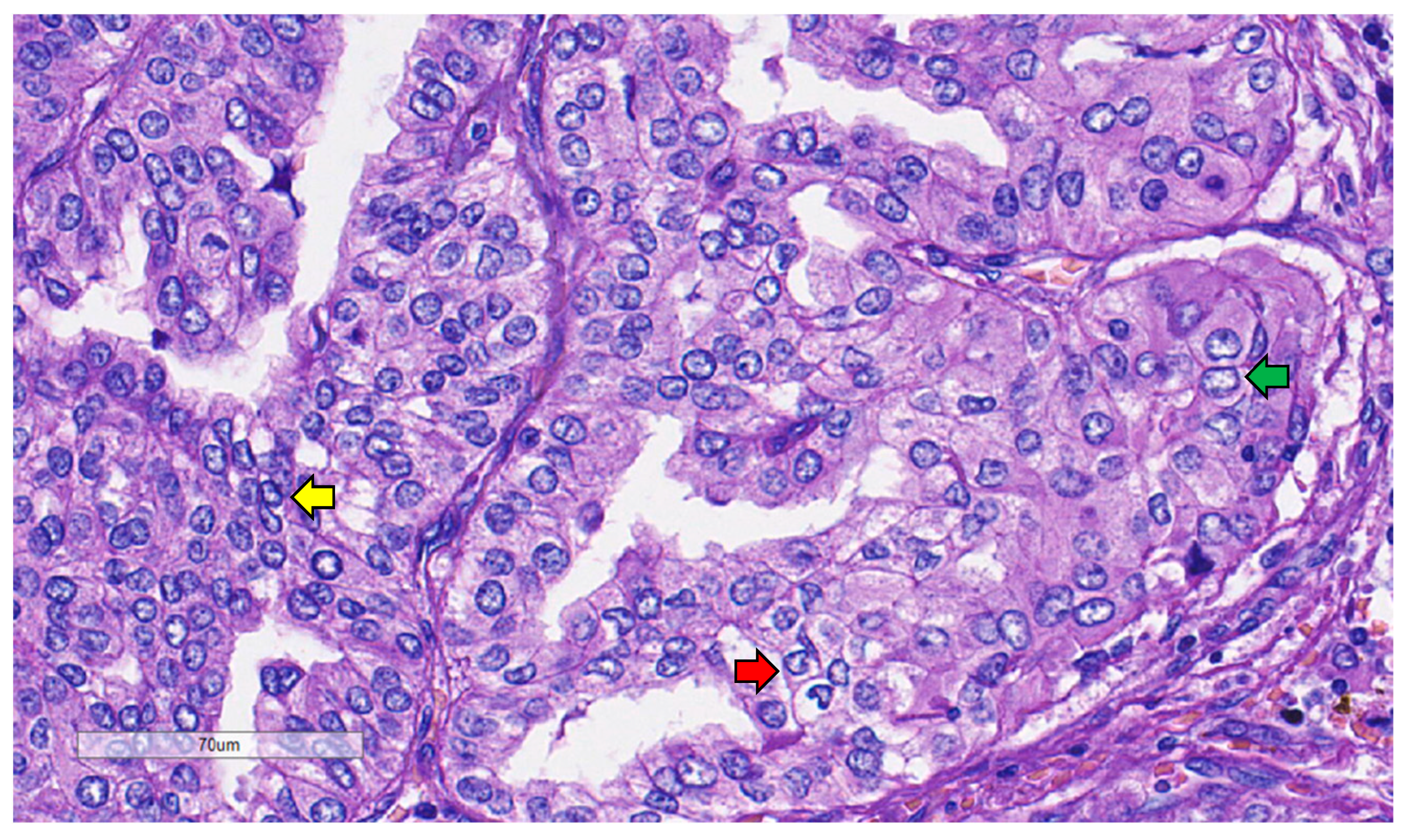
3.2.2. Mitosis
3.2.3. Growth Pattern
3.2.4. Nuclear Features
3.2.5. Role of Ki-67
3.2.6. Cytology
4. Clinical Features
5. Molecular Properties of Differentiated High-Grade Thyroid Carcinoma
6. Treatment and Management
7. Prognosis
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Tallini, G.; Lam, A.K.; Kondo, T.; Piana, S.; Asa, S.L.; Barletta, J. High-grade follicular cell-derived non-anaplastic thyroid carcinoma. In WHO Classification of Tumours Editorial Board. Endocrine and Neuroendocrine Tumours [Internet], 5th ed.; WHO Classification of Tumours Series; International Agency for Research on Cancer: Lyon, France, 2022; Volume 10, Available online: https://tumourclassification.iarc.who.int/chapters/53 (accessed on 9 November 2023).
- Baloch, Z.W.; Asa, S.L.; Barletta, J.A.; Ghossein, R.A.; Juhlin, C.C.; Jung, C.K.; LiVolsi, V.A.; Papotti, M.G.; Sobrinho-Simões, M.; Tallini, G.; et al. Overview of the 2022 WHO classification of thyroid neoplasms. Endocr. Pathol. 2022, 33, 27–63. [Google Scholar] [CrossRef] [PubMed]
- Juhlin, C.C.; Mete, O.; Baloch, Z.W. The 2022 WHO classification of thyroid tumors: Novel concepts in nomenclature and grading. Endocr. Relat. Cancer 2022, 30, e220293. [Google Scholar]
- Volante, M.; Collini, P.; Nikiforov, Y.E.; Sakamoto, A.; Kakudo, K.; Katoh, R.; Lloyd, R.V.; LiVolsi, V.A.; Papotti, M.; Sobrinho-Simoes, M.; et al. Poorly differentiated thyroid carcinoma: The Turin proposal for the use of uniform diagnostic criteria and an algorithmic diagnostic approach. Am. J. Surg. Pathol. 2007, 31, 1256–1264. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, A.; Kasai, N.; Sugano, H. Poorly differentiated carcinoma of the thyroid. A clinicopathologic entity for a high-risk group of papillary and follicular carcinomas. Cancer 1983, 52, 1849–1855. [Google Scholar] [CrossRef] [PubMed]
- Carcangiu, M.L.; Zampi, G.; Rosai, J. Poorly differentiated (“insular”) thyroid carcinoma. A reinterpretation of Langhans’ “wuchernde Struma”. Am. J. Surg. Pathol. 1984, 8, 655–668. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, R.V.; Osamura, R.Y.; Kloppel, G.; Rosai, J. WHO Classification of Tumours of Endocrine Organs, 4th ed.; International Agency for Research on Cancer (IARC): Lyon, France, 2017; pp. 65–91. [Google Scholar]
- Hiltzik, D.; Carlson, D.L.; Tuttle, R.M.; Chuai, S.; Ishill, N.; Shaha, A.; Shah, J.P.; Singh, B.; Ghossein, R.A. Poorly differentiated thyroid carcinomas defined on the basis of mitosis and necrosis: A clinicopathologic study of 58 patients. Cancer 2006, 106, 1286–1295. [Google Scholar] [CrossRef] [PubMed]
- Gnemmi, V.; Renaud, F.; Do Cao, C.; Salleron, J.; Lion, G.; Wemeau, J.L.; Copin, M.C.; Carnaille, B.; Leteurtre, E.; Pattou, F.; et al. Poorly differentiated thyroid carcinomas: Application of the Turin proposal provides prognostic results similar to those from the assessment of high-grade features. Histopathology 2014, 64, 263–273. [Google Scholar] [CrossRef] [PubMed]
- Skansing, D.B.; Londero, S.C.; Asschenfeldt, P.; Larsen, S.R.; Godballe, C. Nonanaplastic follicular cell-derived thyroid carcinoma: Mitosis and necrosis in long-term follow-up. Eur. Arch. Otorhinolaryngol. 2017, 274, 2541–2548. [Google Scholar] [CrossRef]
- Volante, M.; Bussolati, G.; Papotti, M. The story of poorly differentiated thyroid carcinoma: From Langhans’ description to the Turin proposal via Juan Rosai. Semin. Diagn. Pathol. 2016, 33, 277–283. [Google Scholar] [CrossRef]
- Wong, K.S.; Dong, F.; Telatar, M.; Lorch, J.H.; Alexander, E.K.; Marqusee, E.; Cho, N.L.; Nehs, M.A.; Doherty, G.M.; Afkhami, M.; et al. Papillary thyroid carcinoma with high-grade features versus poorly differentiated thyroid carcinoma: An analysis of clinicopathologic and molecular features and outcome. Thyroid 2021, 31, 933–940. [Google Scholar] [CrossRef]
- Jung, C.K.; Bychkov, A.; Kakudo, K. Update from the 2022 World Health Organization classification of thyroid tumors: A standardized diagnostic approach. Endocrinol. Metab. 2022, 37, 703–718. [Google Scholar] [CrossRef] [PubMed]
- Cracolici, V. No longer well-differentiated: Diagnostic criteria and clinical importance of poorly differentiated/high-grade thyroid carcinoma. Surg. Pathol. Clin. 2023, 16, 45–56. [Google Scholar] [CrossRef] [PubMed]
- Xu, B.; Ghossein, R. Poorly differentiated thyroid carcinoma. Semin. Diagn. Pathol. 2020, 37, 243–247. [Google Scholar] [CrossRef] [PubMed]
- Thompson, L.D.R. High grade differentiated follicular cell-derived thyroid carcinoma versus poorly differentiated thyroid carcinoma: A clinicopathologic analysis of 41 cases. Endocr. Pathol. 2023, 34, 234–246. [Google Scholar] [CrossRef] [PubMed]
- Poma, A.M.; Macerola, E.; Ghossein, R.A.; Tallini, G.; Basolo, F. Prevalence of differentiated high-grade thyroid carcinoma among well-differentiated tumors: A systematic review and meta-analysis. Thyroid 2024, 34, 314–323. [Google Scholar] [CrossRef] [PubMed]
- Pizzimenti, C.; Fiorentino, V.; Ieni, A.; Martini, M.; Tuccari, G.; Lentini, M.; Fadda, G. Aggressive variants of follicular cell-derived thyroid carcinoma: An overview. Endocrine 2022, 78, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Kakudo, K.; Wakasa, T.; Ohta, Y.; Yane, K.; Ito, Y.; Yamashita, H. Prognostic classification of thyroid follicular cell tumors using Ki-67 labeling index: Risk stratification of thyroid follicular cell carcinomas. Endocr. J. 2015, 62, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Basolo, F.; Macerola, E.; Poma, A.M.; Torregrossa, L. The 5th edition of WHO classification of tumors of endocrine organs: Changes in the diagnosis of follicular-derived thyroid carcinoma. Endocrine 2023, 80, 470–476. [Google Scholar] [CrossRef] [PubMed]
- Tondi Resta, I.; Gubbiotti, M.A.; Montone, K.T.; Livolsi, V.A.; Baloch, Z.W. Differentiated high grade thyroid carcinomas: Diagnostic consideration and clinical features. Hum. Pathol. 2024, 144, 53–60. [Google Scholar] [CrossRef]
- Alvarez Moreno, J.C.; Muthukumarana, P.; Qiu, S. NRAS gene mutation in differentiated high-grade thyroid carcinoma with multiphenotypic metastatic pattern: A case report. Cureus 2022, 14, e32177. [Google Scholar] [CrossRef]
- Walczyk, A.; Kopczyński, J.; Gąsior-Perczak, D.; Pałyga, I.; Kowalik, A.; Chrapek, M.; Hejnold, M.; Góźdź, S.; Kowalska, A. Histopathology and immunohistochemistry as prognostic factors for poorly differentiated thyroid cancer in a series of Polish patients. PLoS ONE 2020, 15, e0229264. [Google Scholar] [CrossRef] [PubMed]
- Xu, B.; Ibrahimpasic, T.; Wang, L.; Sabra, M.M.; Migliacci, J.C.; Tuttle, R.M.; Ganly, I.; Ghossein, R. Clinicopathologic features of fatal non-anaplastic follicular cell-derived thyroid carcinomas. Thyroid 2016, 26, 1588–1597. [Google Scholar] [CrossRef] [PubMed]
- Jeong, S.I.; Kim, W.; Yu, H.W.; Choi, J.Y.; Ahn, C.H.; Moon, J.H.; Choi, S.I.; Cha, W.; Jeong, W.J.; Park, S.Y.; et al. Incidence and clinicopathological features of differentiated high-grade thyroid carcinomas: An institutional experience. Endocr. Pathol. 2023, 34, 287–297. [Google Scholar] [CrossRef] [PubMed]
- Alzumaili, B.; Xu, B.; Spanheimer, P.M.; Tuttle, R.M.; Sherman, E.; Katabi, N.; Dogan, S.; Ganly, I.; Untch, B.R.; Ghossein, R.A. Grading of medullary thyroid carcinoma on the basis of tumor necrosis and high mitotic rate is an independent predictor of poor outcome. Mod. Pathol. 2020, 33, 1690–1701. [Google Scholar] [CrossRef] [PubMed]
- Samaratunga, H.; Egevad, L.; Delahunt, B. Not all tumour necrosis is granular necrosis. Pathology 2023, 55, 903–904. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.F.; Ahmed, S.; Bhuta, S.; Sercarz, J.A. Infarction of papillary thyroid carcinoma after fine-needle aspiration: Case series and review of literature. JAMA Otolaryngol. Head. Neck Surg. 2014, 140, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Rivera, M.; Ricarte-Filho, J.; Patel, S.; Tuttle, M.; Shaha, A.; Shah, J.P.; Fagin, J.A.; Ghossein, R.A. Encapsulated thyroid tumors of follicular cell origin with high grade features (high mitotic rate/tumor necrosis): A clinicopathologic and molecular study. Hum. Pathol. 2010, 41, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Seethala, R.R.; Baloch, Z.W.; Barletta, J.A.; Khanafshar, E.; Mete, O.; Sadow, P.M.; LiVolsi, V.A.; Nikiforov, Y.E.; Tallini, G.; Thompson, L.D. Noninvasive follicular thyroid neoplasm with papillary-like nuclear features: A review for pathologists. Mod. Pathol. 2018, 31, 39–55. [Google Scholar] [CrossRef] [PubMed]
- Ghossein, R.; Barletta, J.A.; Bullock, M.; Johnson, S.J.; Kakudo, K.; Lam, A.K.; Moonim, M.T.; Poller, D.N.; Tallini, G.; Tuttle, R.M.; et al. Data set for reporting carcinoma of the thyroid: Recommendations from the International Collaboration on Cancer Reporting. Hum. Pathol. 2021, 110, 62–72. [Google Scholar] [CrossRef]
- Volante, M.; Landolfi, S.; Chiusa, L.; Palestini, N.; Motta, M.; Codegone, A.; Torchio, B.; Papotti, M.G. Poorly differentiated carcinomas of the thyroid with trabecular, insular, and solid patterns: A clinicopathologic study of 183 patients. Cancer 2004, 100, 950–957. [Google Scholar] [CrossRef]
- Kakudo, K.; Bychkov, A.; Bai, Y.; Li, Y.; Liu, Z.; Jung, C.K. The new 4th edition World Health Organization classification for thyroid tumors, Asian perspectives. Pathol. Int. 2018, 68, 641–664. [Google Scholar] [CrossRef] [PubMed]
- Asioli, S.; Erickson, L.A.; Righi, A.; Jin, L.; Volante, M.; Jenkins, S.; Papotti, M.; Bussolati, G.; Lloyd, R.V. Poorly differentiated carcinoma of the thyroid: Validation of the Turin proposal and analysis of IMP3 expression. Mod. Pathol. 2010, 23, 1269–1278. [Google Scholar] [CrossRef] [PubMed]
- Cornetta, A.J.; Burchard, A.E.; Pribitkin, E.A.; O’Reilly, R.C.; Palazzo, J.P.; Keane, W.M. Insular carcinoma of the thyroid. Ear Nose Throat J. 2003, 82, 384–389. [Google Scholar] [CrossRef] [PubMed]
- Bongiovanni, M.; Sadow, P.M.; Faquin, W.C. Poorly differentiated thyroid carcinoma: A cytologic-histologic review. Adv. Anat. Pathol. 2009, 16, 283–289. [Google Scholar] [CrossRef] [PubMed]
- LiVolsi, V.A. Papillary thyroid carcinoma: An update. Mod. Pathol. 2011, 24 (Suppl. S2), S1–S9. [Google Scholar] [CrossRef] [PubMed]
- Crescenzi, A.; Baloch, Z. Immunohistochemistry in the pathologic diagnosis and management of thyroid neoplasms. Front. Endocrinol. 2023, 14, 1198099. [Google Scholar] [CrossRef] [PubMed]
- Hellgren, L.S.; Stenman, A.; Paulsson, J.O.; Höög, A.; Larsson, C.; Zedenius, J.; Juhlin, C.C. Prognostic utility of the Ki-67 labeling index in follicular thyroid tumors: A 20-year experience from a tertiary thyroid center. Endocr. Pathol. 2022, 33, 231–242. [Google Scholar] [CrossRef] [PubMed]
- La Rosa, S. Diagnostic, prognostic, and predictive role of Ki67 proliferative index in neuroendocrine and endocrine neoplasms: Past, present, and future. Endocr. Pathol. 2023, 34, 79–97. [Google Scholar] [CrossRef]
- Tang, J.; Gui, C.; Qiu, S.; Wang, M. The clinicopathological significance of Ki67 in papillary thyroid carcinoma: A suitable indicator? World J. Surg. Oncol. 2018, 16, 100. [Google Scholar] [CrossRef]
- Cochand-Priollet, B.; Maleki, Z. Cytology and histology of thyroid nodules: Exploring novel insights in the molecular era for enhanced patient management. Curr. Oncol. 2023, 30, 7753–7772. [Google Scholar] [CrossRef]
- Kakudo, K.; Liu, Z.; Jung, C.K.; Hirokawa, M. High-grade follicular-derived carcinoma in FNA cytology. In Thyroid FNA Cytology, 3rd ed.; Bychkov, A., Lai, C.R., Eds.; Springer Nature Singapore: Singapore, 2023; pp. 391–395. [Google Scholar]
- Wong, K.S.; Barletta, J.A. The new endocrine WHO classification: What does this mean for thyroid cytology? Cancer Cytopathol. 2022, 130, 658–662. [Google Scholar] [CrossRef] [PubMed]
- Rossi, E.D.; Baloch, Z. The impact of the 2022 WHO classification of thyroid neoplasms on everyday practice of cytopathology. Endocr. Pathol. 2023, 34, 23–33. [Google Scholar] [CrossRef] [PubMed]
- Cracolici, V.; Cipriani, N.A. High-grade non-anaplastic thyroid carcinomas of follicular cell origin: A review of poorly differentiated and high-grade differentiated carcinomas. Endocr. Pathol. 2023, 34, 34–47. [Google Scholar] [CrossRef] [PubMed]
- Chernock, R.D.; Rivera, B.; Borrelli, N.; Hill, D.A.; Fahiminiya, S.; Shah, T.; Chong, A.; Aqil, B.; Mehrad, M.; Giordano, T.J.; et al. Poorly differentiated thyroid carcinoma of childhood and adolescence: A distinct entity characterized by DICER1 mutations. Mod. Pathol. 2020, 33, 1264–1274. [Google Scholar] [CrossRef] [PubMed]
- Badulescu, C.I.; Piciu, D.; Apostu, D.; Badan, M.; Piciu, A. Follicular thyroid carcinoma-clinical and diagnostic findings in a 20-year follow up study. Acta Endocrinol. 2020, 16, 170. [Google Scholar] [CrossRef] [PubMed]
- Marcy, P.Y.; Thariat, J.; Bozec, A.; Poissonnet, G.; Benisvy, D.; Dassonville, O. Venous obstruction of thyroid malignancy origin: The Antoine Lacassagne Institute experience. World J. Surg. Oncol. 2009, 7, 40. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, K.; Hirokawa, M.; Yabuta, T.; Fukushima, M.; Kihara, M.; Higashiyama, T.; Tomoda, C.; Takamura, Y.; Ito, Y.; Miya, A.; et al. Tumor thrombus of thyroid malignancies in veins: Importance of detection by ultrasonography. Thyroid 2011, 21, 527–531. [Google Scholar] [CrossRef] [PubMed]
- Hartl, D.M.; Zafereo, M.E.; Kowalski, L.P.; Randolph, G.W.; Olsen, K.D.; Fernandez-Alvarez, V.; Nixon, I.J.; Shaha, A.R.; Angelos, P.; Shah, J.P.; et al. Occlusion of the internal jugular vein in differentiated thyroid carcinoma: Causes and diagnosis. Eur. J. Surg. Oncol. 2021, 47, 1552–1557. [Google Scholar] [CrossRef] [PubMed]
- Marcy, P.Y.; Thariat, J.; Chevenet, C.; Lacout, A. Jugular vein invasion diagnosis and prognosis in thyroid carcinomas. Pol. J. Radiol. 2016, 81, 268–269. [Google Scholar] [CrossRef]
- Morvan, J.B.; Boudin, L.; Metivier, D.; Delarbre, D.; Bouquillon, E.; Thariat, J.; Pascaud, D.; Marcy, P.Y. Internal jugular vein tumor thrombus: A tricky question for the thyroid surgeon. Curr. Oncol. 2022, 29, 9235–9241. [Google Scholar] [CrossRef]
- Jafari, F.; Akerdi, A.T.; Fard, H.A.; Karajizadeh, M.; Paydar, S. Intraluminal extension of papillary thyroid carcinoma into the Internal Jugular Vein; a case report. BMC Endocr. Disord. 2024, 24, 49. [Google Scholar] [CrossRef] [PubMed]
- Nikiforov, Y.E. Thyroid carcinoma: Molecular pathways and therapeutic targets. Mod. Pathol. 2008, 21 (Suppl. S2), S37–S43. [Google Scholar] [CrossRef] [PubMed]
- Xu, B.; Ghossein, R.A. Advances in thyroid pathology: High grade follicular cell-derived thyroid carcinoma and anaplastic thyroid carcinoma. Adv. Anat. Pathol. 2023, 30, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Dettmer, M.S.; Schmitt, A.; Komminoth, P.; Perren, A. Poorly differentiated thyroid carcinoma: An underdiagnosed entity. Pathologe 2020, 41 (Suppl. S1), 1–8. [Google Scholar] [CrossRef] [PubMed]
- Dell’Aquila, M.; Fiorentino, V.; Martini, M.; Capodimonti, S.; Cenci, T.; Lombardi, C.P.; Raffaelli, M.; Pontecorvi, A.; Fadda, G.; Pantanowitz, L.; et al. How limited molecular testing can also offer diagnostic and prognostic evaluation of thyroid nodules processed with liquid-based cytology: Role of TERT promoter and BRAF V600E mutation analysis. Cancer Cytopathol. 2021, 129, 819–829. [Google Scholar] [CrossRef] [PubMed]
- Tong, J.; Ruan, M.; Jin, Y.; Fu, H.; Cheng, L.; Luo, Q.; Liu, Z.; Lv, Z.; Chen, L. Poorly differentiated thyroid carcinoma: A clinician’s perspective. Eur. Thyroid J. 2022, 11, e220021. [Google Scholar] [CrossRef] [PubMed]
- Bellini, M.I.; Biffoni, M.; Patrone, R.; Borcea, M.C.; Costanzo, M.L.; Garritano, T.; Melcarne, R.; Menditto, R.; Metere, A.; Scorziello, C.; et al. Poorly differentiated thyroid carcinoma: Single centre experience and review of the literature. J. Clin. Med. 2021, 10, 5258. [Google Scholar] [CrossRef] [PubMed]
- Ibrahimpasic, T.; Ghossein, R.; Carlson, D.L.; Chernichenko, N.; Nixon, I.; Palmer, F.L.; Lee, N.Y.; Shaha, A.R.; Patel, S.G.; Tuttle, R.M.; et al. Poorly differentiated thyroid carcinoma presenting with gross extrathyroidal extension: 1986–2009 Memorial Sloan-Kettering Cancer Center experience. Thyroid 2013, 23, 997–1002. [Google Scholar] [CrossRef] [PubMed]
- Ibrahimpasic, T.; Ghossein, R.; Shah, J.P.; Ganly, I. Poorly differentiated carcinoma of the thyroid gland: Current status and future prospects. Thyroid 2019, 29, 311–321. [Google Scholar] [CrossRef]
- Xu, B.; David, J.; Dogan, S.; Landa, I.; Katabi, N.; Saliba, M.; Khimraj, A.; Sherman, E.J.; Tuttle, R.M.; Tallini, G.; et al. Primary high-grade non-anaplastic thyroid carcinoma: A retrospective study of 364 cases. Histopathology 2022, 80, 322–337. [Google Scholar] [CrossRef]
- Wong, K.S.; Lorch, J.H.; Alexander, E.K.; Marqusee, E.; Cho, N.L.; Nehs, M.A.; Doherty, G.M.; Barletta, J.A. Prognostic significance of extent of invasion in poorly differentiated thyroid carcinoma. Thyroid 2019, 29, 1255–1261. [Google Scholar] [CrossRef] [PubMed]

| Criteria | PDTC | DHGTC |
|---|---|---|
| Growth Pattern | Solid/insular/trabecular | Papillary/follicular/solid |
| Invasion | Yes | Yes |
| Papillary nuclear features | No | Yes/no |
| High-grade features | Mitotic count ≥ 3/2 mm2 or tumor necrosis or convoluted nuclei | Mitotic count ≥ 5/2 mm2 or tumor necrosis |
| Well-differentiated carcinoma component | No or retention of some | Yes (PTC/FTC/OCA) |
| Anaplastic features | No | No |
| First Author, Year | Jeong S.I. et al., 2023 [25] | Tondi Resta I. et al., 2024 [21] | Thompson et al., 2023 [16] |
|---|---|---|---|
| Study type | Cohort | Cohort | Cohort |
| Country | Republic of Korea | USA | USA |
| Collection time | May 2019–December 2021 | 2012–2022 | January 2010–December 2021 |
| Number of cases | 14 | 32 | 17 |
| Cytology (TBSRTC) | N/A | Yes | N/A |
| I | 1 | ||
| II | 0 | ||
| III | 5 | ||
| IV | 10 | ||
| V | 2 | ||
| VI | 14 | ||
| Necrosis | |||
| Present | 11 | 21 | 17 |
| Absent | 3 | 11 | 0 |
| Mitosis (mean/2 mm2) | 3.14 | 3.2 | 6.1 |
| Invasion | |||
| Lymphatic | 12 | 21 | 8 |
| Vascular | 3 | 6 | 14 |
| PNI | 1 | ||
| None | 8 | ||
| ETE | |||
| Yes | 8 | 17 | 4 |
| No | 6 | 15 | 13 |
| Ki 67 labeling (median) | N/A | 3.50% | 8.30% |
| Metastases | |||
| Regional | 4 | ||
| Nodes | 12 | 10 | 2 |
| Organ/distant | 2 | 5 | 4 |
| Last follow-up status | No evidence of disease (12) Alive with disease (2) | Alive without dx (24) | No evidence of disease (11) |
| Alive with dx (1) | Alive, with metastatic disease (2) | ||
| Died from dx (1) | Dead, with no evidence of disease (1) | ||
| Died from other causes (1) | Dead, with metastatic disease (3) | ||
| Lost to follow-up (5) | |||
| Number of deaths | 0 | 1 | 4 |
| Treatment | N/A | RAI (18) | Surgery only (4) |
| RAI + other chemotherapy (2) | RAI (11) | ||
| RAI + XRT (1) | External beam radiation (3) | ||
| Chemotherapy (1) | Chemotherapy (4) | ||
| Chemotherapy + XRT (1) | |||
| No additional therapy (4) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harahap, A.S.; Roren, R.S.; Imtiyaz, S. A Comprehensive Review and Insights into the New Entity of Differentiated High-Grade Thyroid Carcinoma. Curr. Oncol. 2024, 31, 3311-3328. https://doi.org/10.3390/curroncol31060252
Harahap AS, Roren RS, Imtiyaz S. A Comprehensive Review and Insights into the New Entity of Differentiated High-Grade Thyroid Carcinoma. Current Oncology. 2024; 31(6):3311-3328. https://doi.org/10.3390/curroncol31060252
Chicago/Turabian StyleHarahap, Agnes Stephanie, Regina Stefani Roren, and Shofiyya Imtiyaz. 2024. "A Comprehensive Review and Insights into the New Entity of Differentiated High-Grade Thyroid Carcinoma" Current Oncology 31, no. 6: 3311-3328. https://doi.org/10.3390/curroncol31060252
APA StyleHarahap, A. S., Roren, R. S., & Imtiyaz, S. (2024). A Comprehensive Review and Insights into the New Entity of Differentiated High-Grade Thyroid Carcinoma. Current Oncology, 31(6), 3311-3328. https://doi.org/10.3390/curroncol31060252





