Prognostic Factors Associated with Tumor Recurrence and Overall Survival in Soft Tissue Sarcomas of the Extremities in a Colombian Reference Cancer Center
Abstract
1. Introduction
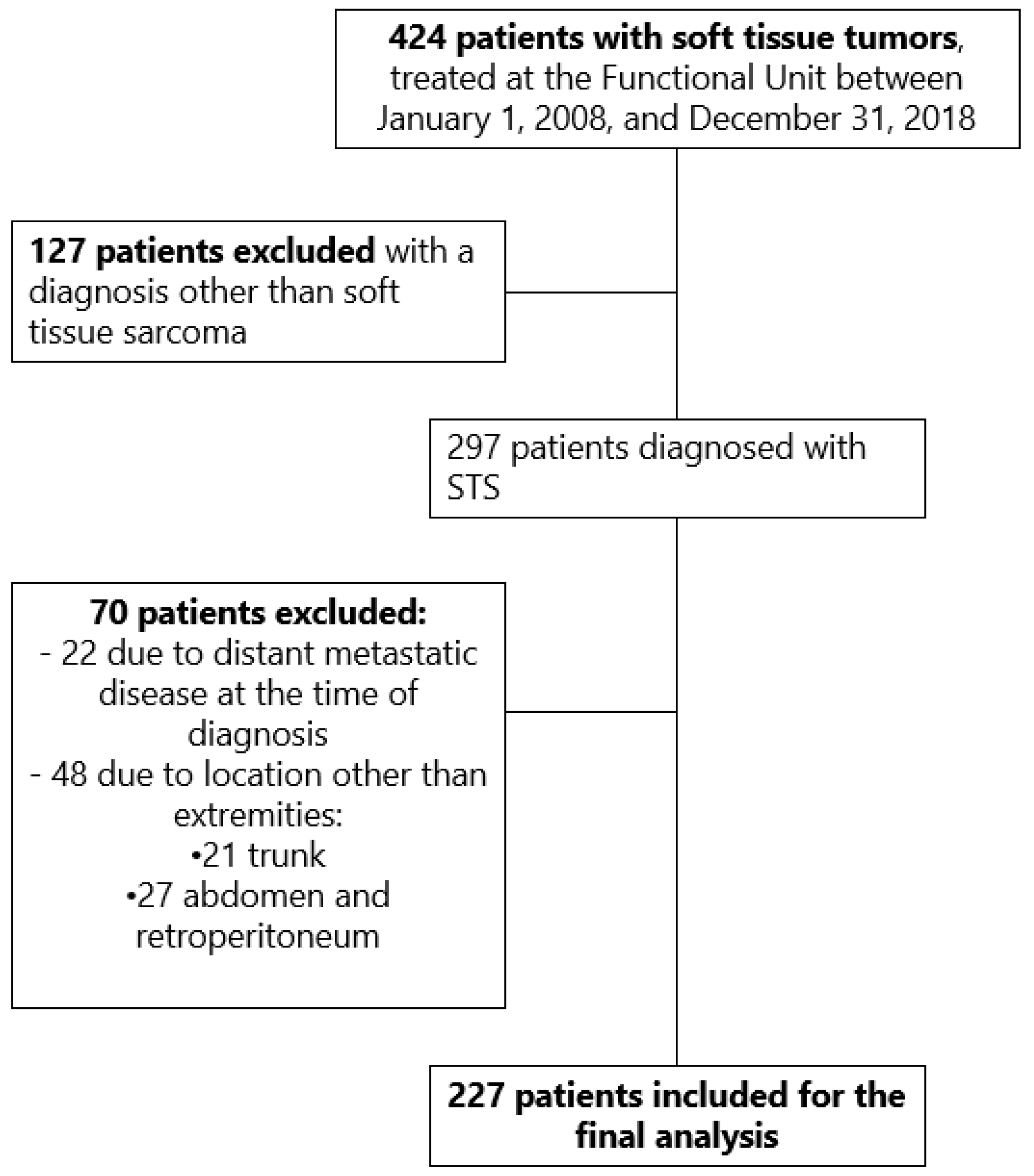
2. Materials and Methods
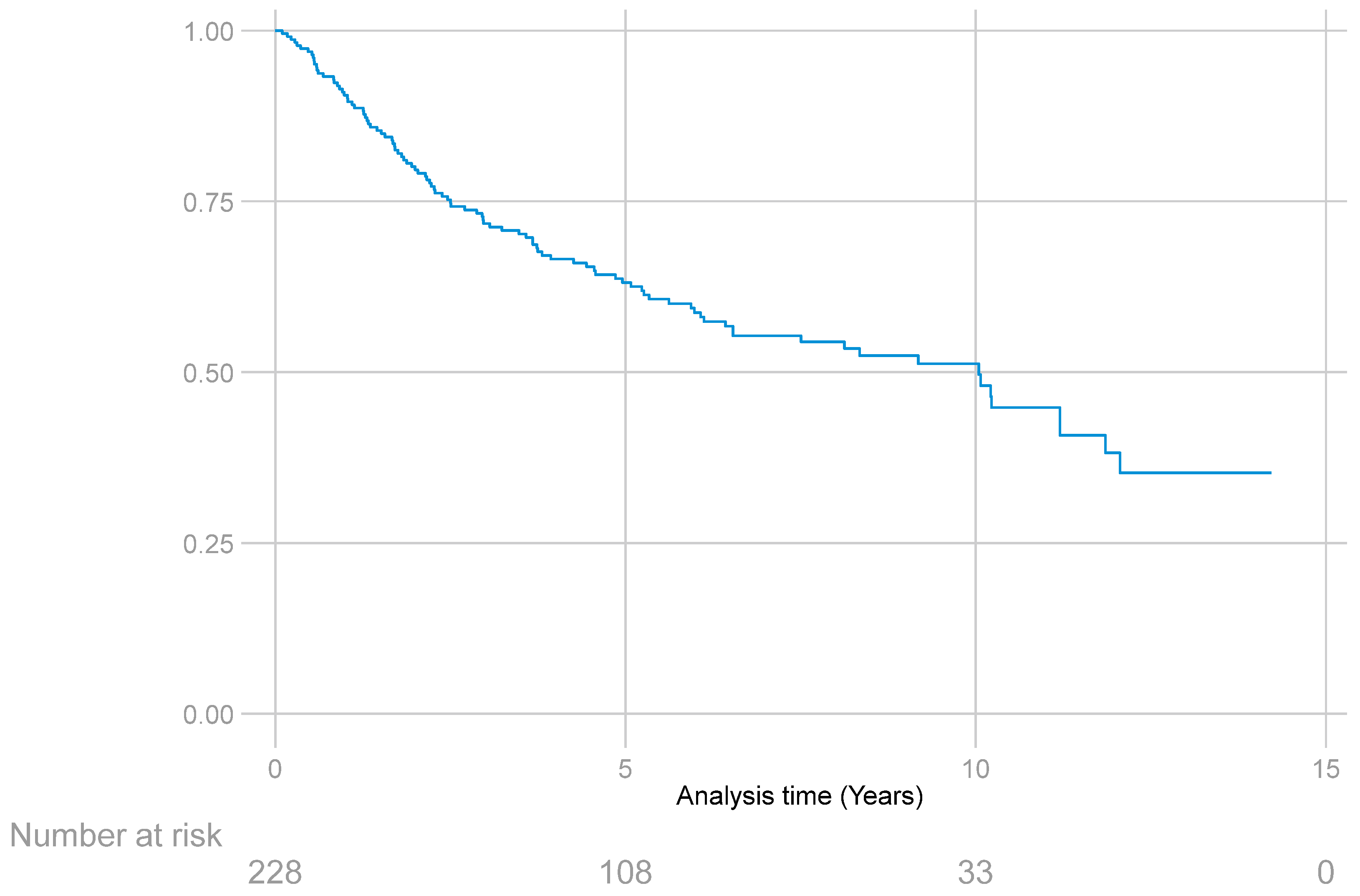
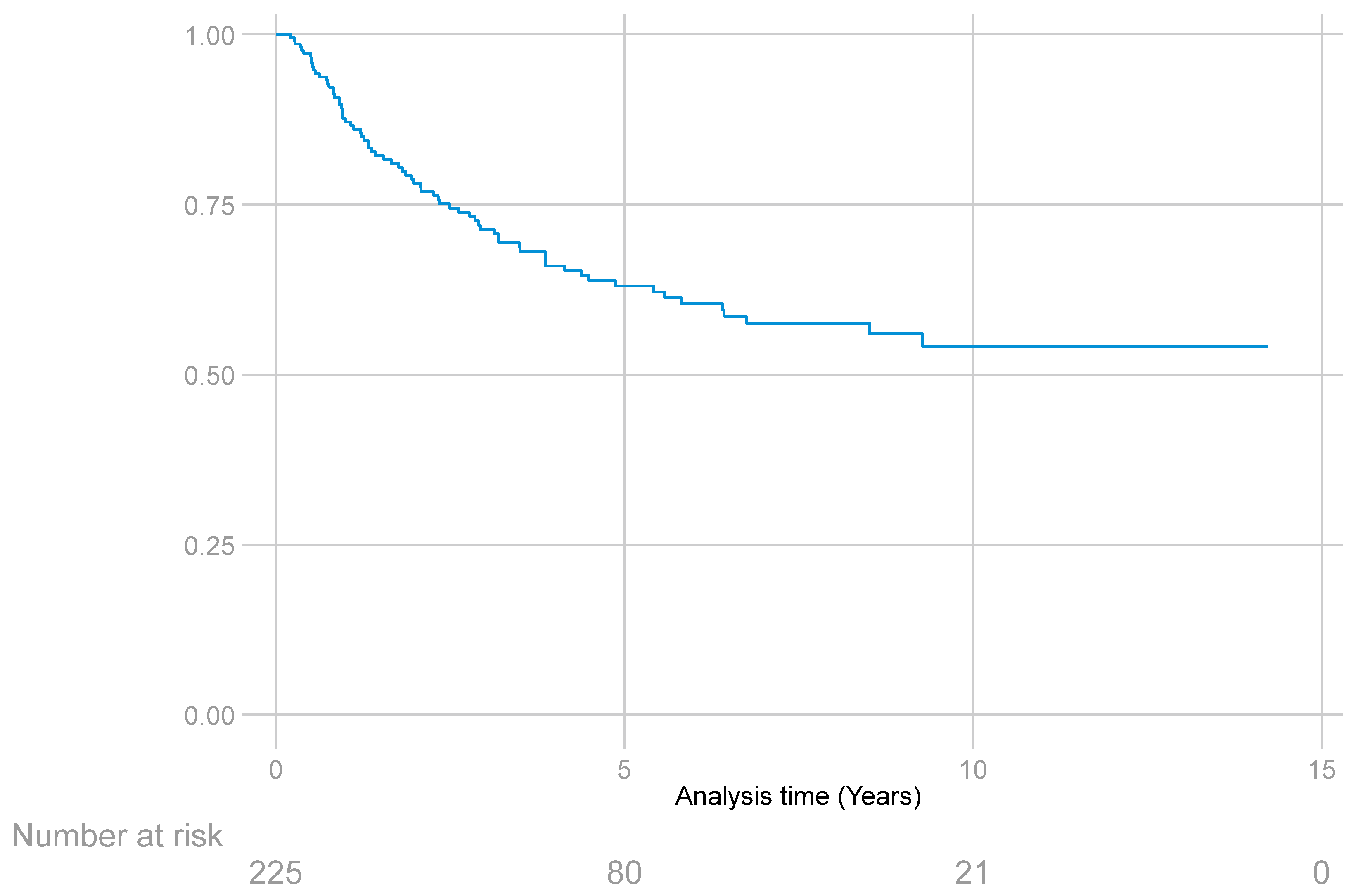
3. Results
Acute and Chronic Complications
4. Discussion
5. Study Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hui, J.Y.C. Epidemiology and Etiology of Sarcomas. Surg. Clin. N. Am. 2016, 96, 901–914. [Google Scholar] [CrossRef] [PubMed]
- American Cancer Society. Cancer Facts & Figures 2020; American Cancer Society: Atlanta, GA, USA, 2020. [Google Scholar]
- Instituto Nacional de Cancerología. Anuario Estadístico 2020; INC: Bogotá, DC, USA, 2020; Volume 18.
- Pisters, P.W.; Weiss, M.; Maki, R. Soft-tissue sarcomas. In Cancer Management: A Multidisciplinary Approach Medical, Surgical, & Radiation Oncology, 4th ed.; UBM Medica LLC: Norwalk, CT, USA, 2011. [Google Scholar]
- Gamboa, A.C.; Gronchi, A.; Cardona, K. Soft-tissue sarcoma in adults: An update on the current state of histiotype-specific management in an era of personalized medicine. CA Cancer J. Clin. 2020, 70, 200–229. [Google Scholar] [CrossRef] [PubMed]
- Keung, E.Z.; Chiang, Y.-J.; Voss, R.K.; Cormier, J.N.; Torres, K.E.; Hunt, K.K.; Feig, B.W.; Roland, C.L. Defining the incidence and clinical significance of lymph node metastasis in soft tissue sarcoma. Eur. J. Surg. Oncol. 2018, 44, 170–177. [Google Scholar] [CrossRef] [PubMed]
- Sbaraglia, M.; Dei Tos, A.P. The pathology of soft tissue sarcomas. Radiol. Medica 2019, 124, 266–281. [Google Scholar] [CrossRef]
- Edge, S.; Byrd, D.; Compton, C.; Fritz, A.; Greene, F.; Trotti, A. The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J. Clin. 2017, 67, 93–99. [Google Scholar] [CrossRef]
- Voss, R.K.; Chiang, Y.-J.; Torres, K.E.; Guadagnolo, B.A.; Mann, G.N.; Feig, B.W.; Cormier, J.N.; Roland, C.L. Adherence to National Comprehensive Cancer Network Guidelines is Associated with Improved Survival for Patients with Stage 2A and Stages 2B and 3 Extremity and Superficial Trunk Soft Tissue Sarcoma. Ann. Surg. Oncol. 2017, 24, 3271–3278. [Google Scholar] [CrossRef]
- Billingsley, K.G.; Lewis, J.J.; Leung, D.H.Y.; Casper, E.S.; Woodruff, J.M.; Brennan, M.F. Multifactorial analysis of the survival of patients with distant metastasis arising from primary extremity sarcoma. Cancer 1999, 85, 389–395. [Google Scholar] [CrossRef]
- Wasif, N.; Smith, C.A.; Tamurian, R.M.; Christensen, S.D.; Monjazeb, A.M.; Martinez, S.R.; Canter, R.J. Influence of physician specialty on treatment recommendations in the multidisciplinary management of soft tissue sarcoma of the extremities. JAMA Surg. 2013, 148, 632–639. [Google Scholar] [CrossRef]
- Rosenberg, S.A.; Tepper, J.; Glatstein, E.; Costa, J.; Baker, A.; Brennam, M.; Demoss, E.V.; Seipp, C.; Sindelar, W.F.; Sugarbaker, P.; et al. The treatment of soft-tissue sarcomas of the extremities: Prospective randomized evaluations of (1) limb-sparing surgery plus radiation therapy compared with amputation and (2) the role of adjuvant chemotherapy. Ann. Surg. 1982, 196, 305–315. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, B.; Davis, A.M.; Turcotte, R.; Bell, R.; Catton, C.; Chabot, P.; Wunder, J.; Kandel, R.; Goddard, K.; Sadura, A.; et al. Preoperative versus postoperative radiotherapy in soft-tissue sarcoma of the limbs: A randomised trial. Lancet 2002, 359, 2235–2241. [Google Scholar] [CrossRef] [PubMed]
- Tierney, J.F.; Mosseri, V.; Stewart, L.A.; Souhami, R.L.; Parmar, M.K. Adjuvant chemotherapy for soft-tissue sarcoma: Review and meta-analysis of the published results of randomised clinical trials. Br. J. Cancer 1995, 72, 469–475. [Google Scholar] [CrossRef] [PubMed]
- Blay, J.-Y.; Honoré, C.; Stoeckle, E.; Meeus, P.; Jafari, M.; Gouin, F.; Anract, P.; Ferron, G.; Rochwerger, A.; Ropars, M.; et al. Surgery in reference centers improves survival of sarcoma patients: A nationwide study. Ann. Oncol. 2019, 30, 1143–1153. [Google Scholar] [CrossRef]
- Demetri, G.D.; Blay, J.Y.; Casali, P.G. Advances and controversies in the management of soft tissue sarcomas. Future Oncol. 2016, 13, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Weskamp, P.; Ufton, D.; Drysch, M.; Wagner, J.M.; Dadras, M.; Lehnhardt, M.; Behr, B.; Wallner, C. Risk Factors for Occurrence and Relapse of Soft Tissue Sarcoma. Cancers 2022, 14, 1273. [Google Scholar] [CrossRef] [PubMed]
- Coindre, J.M.; Trojani, M.; Contesso, G.; David, M.; Rouesse, J.; Bui, N.B.; Bodaert, A.; De Mascarel, I.; De Mascarel, A.; Goussot, J.-F. Reproducibility of a histopathologic grading system for adult soft tissue sarcoma. Cancer 1986, 58, 306–309. [Google Scholar] [CrossRef]
- Brennan, M.F.; Antonescu, C.R.; Moraco, N.; Singer, S. Lessons learned from the study of 10,000 patients with soft tissue sarcoma. Ann. Surg. 2014, 260, 416. [Google Scholar] [CrossRef] [PubMed]
- Torosian, M.H.; Friedrich, M.; Godbold, J.; Hajdu, S.I.; Brennan, M.F. Soft-tissue sarcoma: Initial characteristics and prognostic factors in patients with and without metastatic disease. Semin. Surg. Oncol. 1988, 4, 13–19. [Google Scholar] [CrossRef]
- Li, R.H.; Zhou, Q.; Li, A.B.; Zhang, H.Z.; Lin, Z.Q. A nomogram to predict metastasis of soft tissue sarcoma of the extremities. Medicine 2020, 99, e20165. [Google Scholar] [CrossRef]
- Coindre, J.M.; Terrier, P.; Bui, N.B.; Bonichon, F.; Collin, F.; Le Doussal, V.; Mandard, A.M.; Vilain, O.M.; Jacquemier, J.; Duplay, H.; et al. Prognostic factors in adult patients with locally controlled soft tissue sarcoma. A study of 546 patients from the French Feredarion of Cancer Centers Sarcoma Group. J. Clin. Oncol. 1996, 14, 869–877. [Google Scholar] [CrossRef]
- Gaynor, J.J.; Tan, C.C.; Casper, E.S.; Collin, C.F.; Friedrich, C.; Shiu, M.; Hajdu, I.S.; Brennan, M.F. Refinement of clinicopathologic staging for localized soft tissue sarcoma of the extremity: A study of 423 adults. J. Clin. Oncol. 1992, 10, 1317–1329. [Google Scholar] [CrossRef]
- Pisters, P.W.; Leung, D.H.; Woodruff, J.; Shi, W.; Brennan, M.F. Analysis of prognostic factors in 1,041 patients with localized soft tissue sarcomas of the extremities. J. Clin. Oncol. 1996, 14, 1679–1689. [Google Scholar] [CrossRef] [PubMed]
- Stefanovski, P.; Bidoli, E.; De Paoli, A.; Buonadonna, A.; Boz, G.; Libra, M.; Morassut, S.; Rossi, C.; Carbone, A.; Frustaci, S. Prognostic factors in soft tissue sarcomas: A study of 395 patients. Eur. J. Surg. Oncol. 2002, 28, 153–164. [Google Scholar] [CrossRef] [PubMed]
- Gronchi, A.; Casali, P.; Mariani, L.; Miceli, R.; Fiore, M.; Vullo, S.L.; Bertulli, R.; Collini, P.; Lozza, L.; Olmi, P.; et al. Status of surgical margins and prognosis in adult soft tissue sarcomas of the extremities: A series of patients treated at a single institution. J. Clin. Oncol. 2005, 23, 96–104. [Google Scholar] [CrossRef] [PubMed]
- Stojadinovic, A.; Leung, D.H.Y.; Hoos, A.; Jaques, D.P.; Lewis, J.J.; Brennan, M.F. Analysis of the prognostic significance of microscopic margins in 2,084 localized primary adult soft tissue sarcomas. Ann. Surg. 2002, 235, 424–434. [Google Scholar] [CrossRef]
- Trovik, C.; Bauer, H.; Alvegård, T.; Anderson, H.; Blomqvist, C.; Berlin, O.; Gustafson, P.; Sæter, G.; Wallöe, A. Surgical margins, local recurrence and metastasis in soft tissue sarcomas: 559 Surgically-treated patients from the Scandinavian Sarcoma Group Register. Eur. J. Cancer 2000, 36, 710–716. [Google Scholar] [CrossRef] [PubMed]
- Zagars, G.K.; Ballo, M.T.; Pisters, P.W.T.; Pollock, R.E.; Patel, S.R.; Benjamin, R.S.; Evans, H.L. Prognostic factors for patients with localized soft-tissue sarcoma treated with conservation surgery and radiation therapy: An analysis of 1225 patients. Cancer 2003, 97, 2530–2543. [Google Scholar] [CrossRef]
- Rosenthal, J.; Cardona, K.; Sayyid, S.K.; Perricone, A.J.; Reimer, N.; Monson, D.; Singer, A.D. Nodal metastases of soft tissue sarcomas: Risk factors, imaging findings, and implications. Skelet. Radiol. 2020, 49, 221–229. [Google Scholar] [CrossRef]
- Davis, A.M.; O’Sullivan, B.; Turcotte, R.; Bell, R.; Catton, C.; Chabot, P.; Wunder, J.; Hammond, A.; Benk, V.; Kandel, R.; et al. Late radiation morbidity following randomization to preoperative versus postoperative radiotherapy in extremity soft tissue sarcoma. Radiother. Oncol. 2005, 75, 48–53. [Google Scholar] [CrossRef]
- Gingrich, A.A.; Bateni, S.B.; Monjazeb, A.M.; Darrow, M.A.; Thorpe, S.W.; Kirane, A.R.; Bold, R.J.; Canter, R.J. Neoadjuvant Radiotherapy is Associated with R0 Resection and Improved Survival in Extremity Soft Tissue Sarcoma Patients Undergoing Surgery: An NCDB Analysis Alicia. Ann. Surg. Oncol. 2018, 24, 3252–3263. [Google Scholar] [CrossRef]
- Broecker, J.S.; Ethun, C.G.; Monson, D.K.; Lopez-Aguiar, A.G.; Le, N.; McInnis, M.; Godette, K.; Reimer, N.B.; Oskouei, S.V.; Delman, K.A.; et al. The Oncologic Impact of Postoperative Complications Following Resection of Truncal and Extremity Soft Tissue Sarcomas. Ann. Surg. Oncol. 2017, 24, 3574–3586. [Google Scholar] [CrossRef]
- Schwartz, A.; Rebecca, A.; Smith, A.; Casey, W.; Ashman, J.; Gunderson, L.; Curtis, K.; Chang, Y.-H.H.; Beauchamp, C. Risk factors for significant wound complications following wide resection of extremity soft tissue sarcomas. Clin. Orthop. Relat. Res. 2013, 471, 3612–3617. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Total of Patients (n = 227), n (%) |
|---|---|
| Median age (years) | 53 (18–89) |
| Sex | |
| Men | 117 (51.5) |
| Women | 110 (48.5) |
| Presentation type | |
| Primary without treatment | 142 (62.5) |
| Tumor persistence | 63 (27.8) |
| Tumor recurrence | 22 (9.7) |
| Histologic type | |
| Well-differentiated liposarcoma | 39 (17.2) |
| Undifferentiated pleomorphic sarcoma | 39 (17.2) |
| Myxoid liposarcoma | 33 (14.5) |
| Synovial sarcoma | 25 (11) |
| Myxofibrosarcoma | 21 (9.3) |
| Leiomyosarcoma | 19 (8.4) |
| Malignant neural sheath tumor | 16 (7) |
| Others | 35 (15.4) |
| Histologic grade | |
| I | 67 (29.5) |
| II | 12 (5.3) |
| III | 147 (64.8) |
| No data | 1 (0.4) |
| Tumor size | |
| T1 | 53 (23.3) |
| T2 | 64 (28.1) |
| T3 | 40 (17.7) |
| T4 | 65 (28.7) |
| No data (Initial surgery outside the INC) | 5 (2.2) |
| Clinical stage | |
| IA | 14 (6.2) |
| IB | 43 (18.9) |
| II | 35 (15.4) |
| IIIA | 57 (25.1) |
| IIIB | 66 (29.1) |
| IV (Lymph node involvement) | 3 (1.3) |
| Not applicable (Dermatofibrosarcoma protuberans) | 9 (3.9) |
| Tumor location | |
| Thigh | 108 (47.7) |
| Leg | 39 (17.2) |
| Forearm | 23 (10.1) |
| Gluteus | 16 (7) |
| Foot | 13 (5.7) |
| Arm | 12 (5.3) |
| Shoulder | 10 (4.4) |
| Hand | 6 (2.6) |
| Administered Treatment | Total of Patients (n = 227), n (%) |
|---|---|
| Initial treatment type | |
| Surgical treatment | 170 (74.9) |
| Neoadjuvant RT | 27 (11.9) |
| ILP | 23 (10.1) |
| Neoadjuvant CHT | 7 (3.1) |
| Type of primary tumor surgery | |
| Wide local resection | 130 (57.4) |
| Amputation | 54 (23.8) |
| Widening of margins of previous non-oncological surgery outside the INC | 28 (12.3) |
| Compartmental resection | 9 (3.9) |
| Marginal resection | 6 (2.6) |
| Additional interventions | |
| Sentinel lymph node | 19 (8.3) |
| Lymph node dissection | 18 (7.9) |
| IORT | 14 (6.1) |
| Positive margins in INC pathology | |
| No | 189 (83.3) |
| Yes | 34 (14.9) |
| Planned positive margins | 6 (17.7) |
| Surgery to achieve negative margins | |
| Widening of margins | 11 (4.8) |
| Adjuvant treatment | |
| Adjuvant CHT | 51 (22.4) |
| Adjuvant RT | 85 (37.3) |
| Variable | Overall Survival Hazard Ratio (IC95%) | Recurrence-Free Survival Hazard Ratio (IC95%) | ||
|---|---|---|---|---|
| Age | 1.01 (1–1.02) | p = 0.048 | 0.99 (0.983–1.015) | p = 0.92 |
| Tumor size | 1.01 (0.99–1.04) | p = 0.18 | 1.03 (0.996–1.056) | p = 0.08 |
| Histologic grade | ||||
| I | Ref. | Ref. | ||
| II | 0.69 (0.007–0.67) | p = 0.021 | 1.97 (0.49–7.9) | p = 0.33 |
| III | 0.13 (0.01–1.1) | p = 0.062 | 5.36 (2.29–12.56) | p < 0.001 |
| Type of primary tumor surgery | ||||
| Amputation | Ref. | Ref. | ||
| Compartmental resection | 0.69 (0.2–2.23) | p = 0.56 | 0.68 (0.16–2.83) | p = 0.6 |
| Wide local resection | 0.48 (0.24–0.96) | p = 0.038 | 0.56 (0.26–1.21) | p = 0.14 |
| Marginal resection | 1.81 (0.47–6.9) | p = 0.38 | 2.16 (0.41–11.3) | p = 0.36 |
| Widening of margins of previous non-oncological surgery outside the INC | 0.36 (0.12–1.1) | p = 0.075 | 0.16 (0.045–0.6) | p = 0.006 |
| Positive margins in INC pathology | ||||
| Yes | 1.11 (0.54–2.26) | p = 0.76 | 1.56 (0.75–3.2) | p = 0.23 |
| No | Ref. | Ref. | ||
| Presentation type | ||||
| Primary without treatment | Ref. | Ref. | ||
| Tumor persistence | 0.95 (0.51–1.77) | p = 0.88 | 2.34 (1.25–4.35) | p = 0.007 |
| Tumor recurrence | 0.83 (0.39–1.76) | p = 0.63 | 1.62 (0.74–3.53) | p = 0.21 |
| Initial treatment type | ||||
| Surgical treatment | Ref. | Ref. | ||
| Neoadjuvant CHT | 1.18 (0.43–3.24) | p = 0.73 | 0.68 (0.15–3.03) | p = 0.61 |
| Neoadjuvant RT | 0.7 (0.3–1.65) | p = 0.42 | 0.86 (0.35–2.09) | p = 0.75 |
| ILP | 0.75 (0.36–1.54) | p = 0.44 | 0.62 (0.25–1.52) | p = 0.75 |
| Adjuvant treatment | ||||
| Adjuvant CHT | ||||
| Yes | 0.66 (0.38–1.14) | p = 0.14 | 1.14 (0.3–1.2) | p = 0.15 |
| No | Ref. | Ref. | ||
| Adjuvant RT | ||||
| Yes | 0.7 (0.38–1.27) | p = 0.24 | 0.6 (0.3–1.2) | p = 1.2 |
| No | Ref. | Ref. | ||
| Variable | Local Recurrence Hazard Ratio (IC95%) | Distant Recurrence Hazard Ratio (IC95%) | ||
|---|---|---|---|---|
| Age | 0.99 (0.77–1.02) | p = 0.77 | 0.99 (0.983–1.019) | p = 0.93 |
| Tumor size | 1 (0.95–1.05) | p = 0.89 | 1.03 (1.007–1.067) | p = 0.015 |
| Histologic grade | ||||
| I | Ref. | Ref. | ||
| II | 1.1 (0.11–10.5) | p = 0.92 | 2.21 (0.37–13.08) | p = 0.38 |
| III | 6.09 (2.03–18.2) | p = 0.001 | 4.53 (1.42–14.49) | p = 0.011 |
| Type of primary tumor surgery | ||||
| Amputation | Ref. | Ref. | ||
| Compartmental resection | 3.43 (0.48–24.63) | p = 0.21 | 0.48 (0.086–2.74) | p = 0.41 |
| Wide local resection | 1.69 (0.46–6.1) | p = 0.42 | 0.37 (0.14–0.94) | p = 0.038 |
| Marginal resection | 8.88 (0.75–104.4) | p = 0.08 | 0.78 (0.08–7.52) | p = 0.83 |
| Widening of margins of previous non-oncological surgery outside the INC | 0.51 (0.08–3.06) | p = 0.46 | 0.07 (0.008–0.64) | p = 0.019 |
| Positive margins in INC pathology | ||||
| Yes | 1.74 (0.69–4.34) | 1 (0.37–2.72) | ||
| No | Ref. | p = 0.23 | Ref. | p = 0.98 |
| Presentation type | ||||
| Primary without treatment | Ref. | Ref. | ||
| Tumor persistence | 2.85 (1.23–6.57) | p = 0.014 | 1.49 (0.65–3.41) | p = 0.33 |
| Tumor recurrence | 1.6 (0.5–5.07) | p = 0.42 | 1.42 (0.55–3.64) | p = 0.46 |
| Initial treatment type | ||||
| Surgical treatment | Ref. | Ref. | ||
| Neoadjuvant CHT | 0.81 (0.09–6.84) | p = 0.85 | 1.35 (0.28–6.44) | p = 0.7 |
| Neoadjuvant RT | 0.77 (0.21–2.65) | p = 0.65 | 0.98 (0.32–3.03) | p = 0.98 |
| ILP | 1.02 (0.32–3.24) | p = 0.96 | 0.50 (0.14–1.78) | p = 0.29 |
| Adjuvant treatment | ||||
| Adjuvant CHT | ||||
| Yes | 0.75 (0.33–1.69) | p = 0.49 | 1.25 (0.62–2.54) | p = 0.52 |
| No | Ref. | Ref. | ||
| Adjuvant RT | ||||
| Yes | 0.55 (0.22–1.4) | p = 0.21 | 0.82 (0.33–2.01) | p = 0.66 |
| No | Ref. | Ref. | ||
| Variable | Acute Complications Coefficient (β) (IC95%) | Chronic Complications Odds Ratio (IC95%) | ||
|---|---|---|---|---|
| Age | 0.017 (0.002–0.031) | p = 0.022 | 1 (0.96–1.03) | p = 0.89 |
| Tumor size | 0.036 (0.007–0.065) | p = 0.015 | 0.96 (0.87–1.07) | p = 0.52 |
| Histologic grade | ||||
| I | Ref. | Ref. | ||
| II | 0.19 (0.82–1.22) | p = 0.7 | 1.1 (0.07–15.76) | p = 0.94 |
| III | 0.41 (0.19–1.02) | p = 0.18 | 1.55 (0.3–7.9) | p = 0.59 |
| Type of primary tumor surgery | ||||
| Amputation | Ref. | - | Ref. | |
| Compartmental resection | 1.37 (0.1–2.63) | p = 0.03 | - | |
| Wide local resection | 1.38 (0.43–2.33) | p = 0.004 | 2.49 (0.23–26.46) | p = 0.44 |
| Marginal resection | 1.47 (−0.12–3.06) | p = 0.07 | 7.33 (0.24–219.49) | p = 0.25 |
| Widening of margins of previous non-oncological surgery outside the INC | 1.69 (0.34–3.05) | p = 0.014 | 0.77 (0.027–21.82) | p = 0.88 |
| Positive margins in INC pathology | ||||
| Yes | Ref. | Ref. | ||
| No | −0.07 (−0.754–0.596) | p = 0.81 | 0.62 (0.11–3.37) | p = 0.58 |
| Presentation type | ||||
| Primary without treatment | Ref. | Ref. | ||
| Tumor persistence | −0.24 (−1.01–0.52) | p = 0.53 | 1.53 (0.32–7.25) | p = 0.59 |
| Tumor recurrence | 0.95 (0.32–1.59) | p = 0.003 | 3.35 (0.68–16.33) | p = 0.13 |
| Initial treatment type | ||||
| Surgical treatment | Ref. | Ref. | ||
| Neoadjuvant CHT | −0.14 (−1.63–1.34) | p = 0.84 | 2.31 (0.18–29.12) | p = 0.51 |
| Neoadjuvant RT | 0.16 (−0.05–0.88) | p = 0.65 | 3.53 (0.44–28.42) | p = 0.23 |
| ILP | −0.21 (−1.18–0.76) | p = 0.67 | 2.41 (0.37–15.68) | p = 0.35 |
| Adjuvant treatment | ||||
| Adjuvant CHT | p = 0.45 | |||
| Yes | 0.02 (−0.57–0.62) | p = 0.93 | 0.55 (0.11–2.64) | |
| No | Ref. | Ref. | ||
| Adjuvant RT | p = 0.052 | |||
| Yes | −0.03 (−0.6–0.53) | p = 0.9 | 4.36 (0.98–19.26) | |
| No | Ref. | Ref. | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Díaz Casas, S.E.; Villacrés, J.M.; Lehmann Mosquera, C.; García Mora, M.; Mariño Lozano, I.; Ángel Aristizábal, J.; Suarez Rodríguez, R.; Duarte Torres, C.A.; Sánchez Pedraza, R. Prognostic Factors Associated with Tumor Recurrence and Overall Survival in Soft Tissue Sarcomas of the Extremities in a Colombian Reference Cancer Center. Curr. Oncol. 2024, 31, 1725-1738. https://doi.org/10.3390/curroncol31040131
Díaz Casas SE, Villacrés JM, Lehmann Mosquera C, García Mora M, Mariño Lozano I, Ángel Aristizábal J, Suarez Rodríguez R, Duarte Torres CA, Sánchez Pedraza R. Prognostic Factors Associated with Tumor Recurrence and Overall Survival in Soft Tissue Sarcomas of the Extremities in a Colombian Reference Cancer Center. Current Oncology. 2024; 31(4):1725-1738. https://doi.org/10.3390/curroncol31040131
Chicago/Turabian StyleDíaz Casas, Sandra E., Juanita Martínez Villacrés, Carlos Lehmann Mosquera, Mauricio García Mora, Iván Mariño Lozano, Javier Ángel Aristizábal, Raúl Suarez Rodríguez, Carlos Alfonso Duarte Torres, and Ricardo Sánchez Pedraza. 2024. "Prognostic Factors Associated with Tumor Recurrence and Overall Survival in Soft Tissue Sarcomas of the Extremities in a Colombian Reference Cancer Center" Current Oncology 31, no. 4: 1725-1738. https://doi.org/10.3390/curroncol31040131
APA StyleDíaz Casas, S. E., Villacrés, J. M., Lehmann Mosquera, C., García Mora, M., Mariño Lozano, I., Ángel Aristizábal, J., Suarez Rodríguez, R., Duarte Torres, C. A., & Sánchez Pedraza, R. (2024). Prognostic Factors Associated with Tumor Recurrence and Overall Survival in Soft Tissue Sarcomas of the Extremities in a Colombian Reference Cancer Center. Current Oncology, 31(4), 1725-1738. https://doi.org/10.3390/curroncol31040131





