Urinary Diversion Can Improve the Chance of Implementing New Therapeutic Lines in Patients with Malignant Ureteral Obstruction: A Multicenter Study
Abstract
1. Introduction
2. Materials and Methods
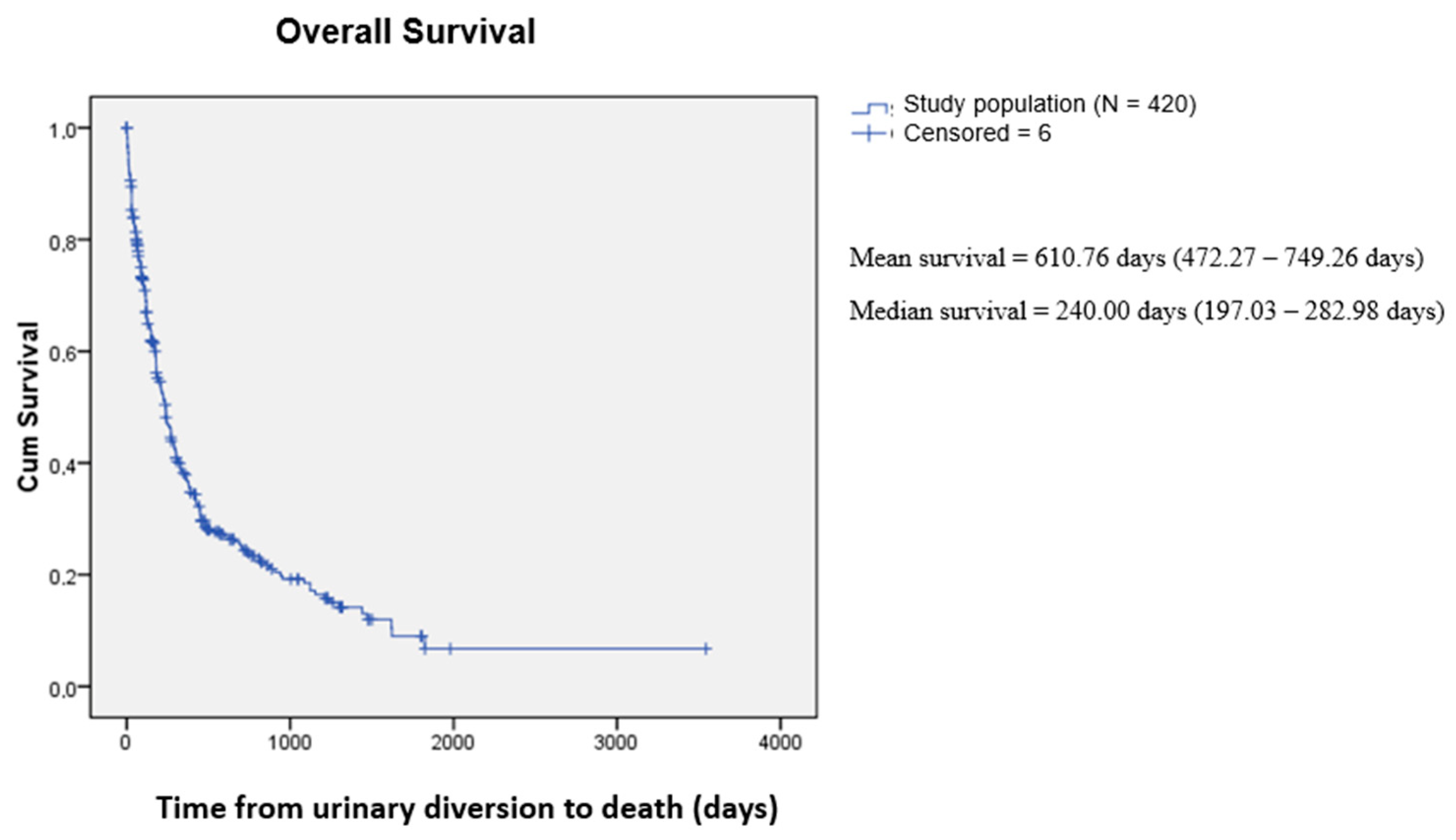
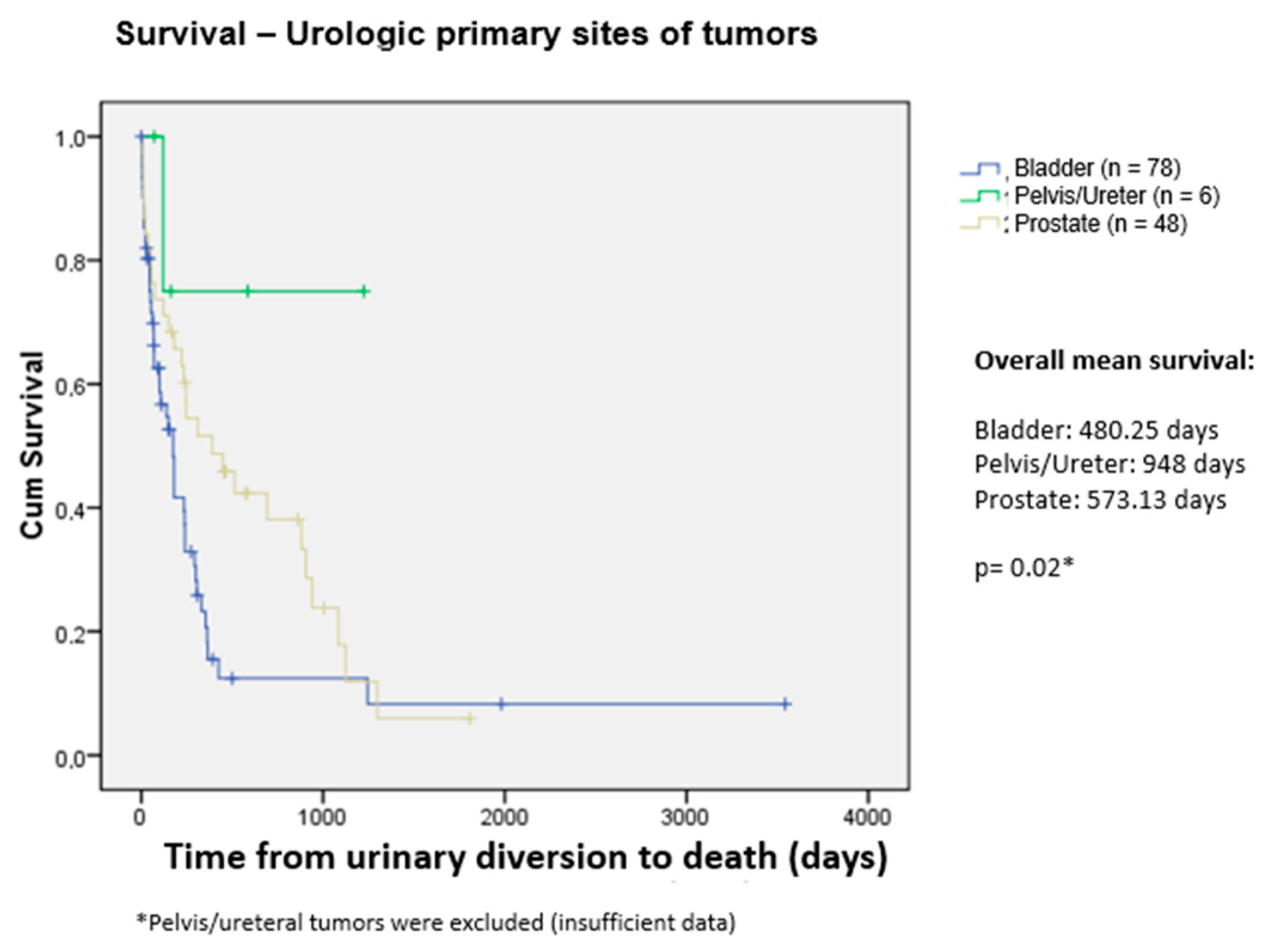
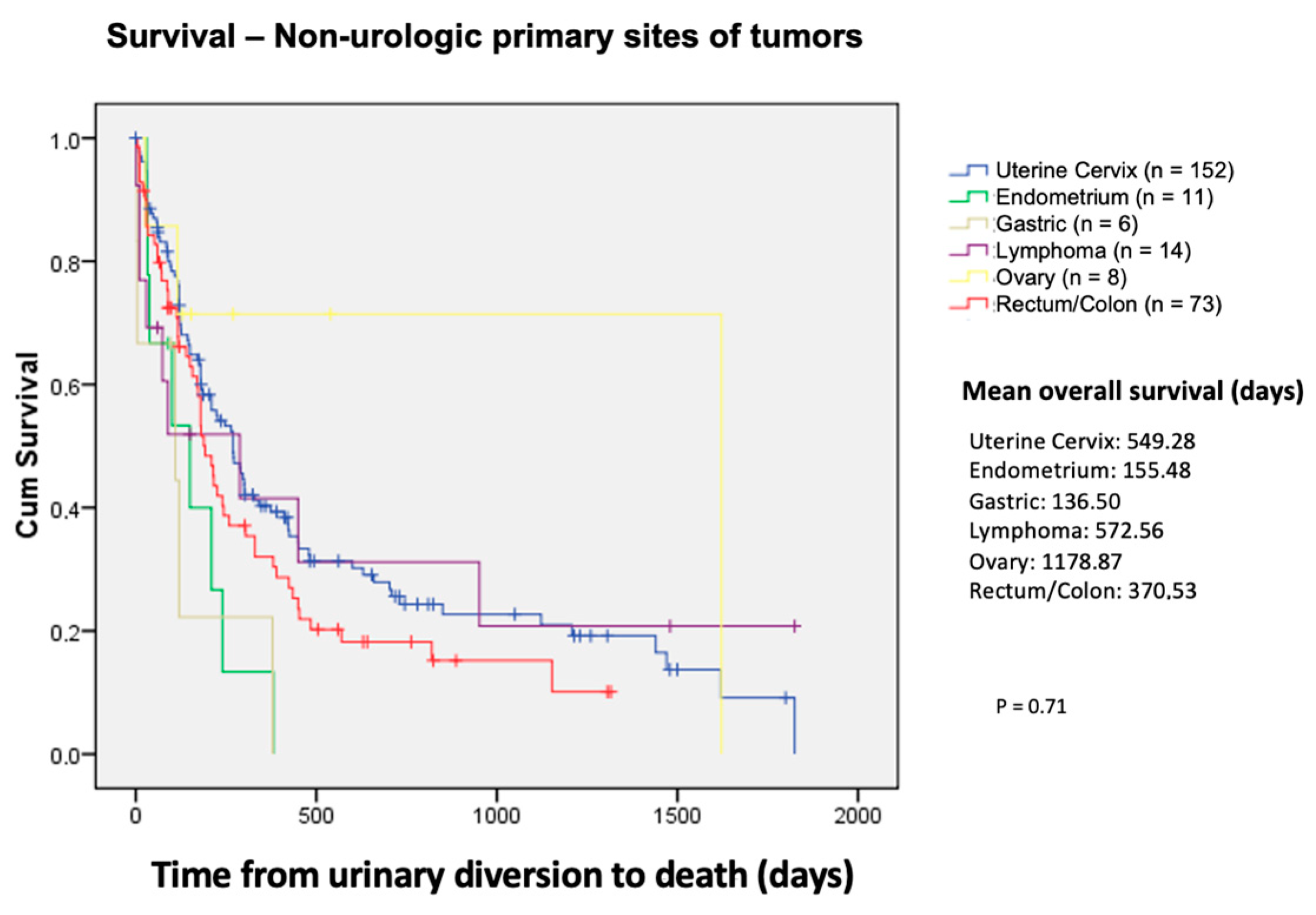
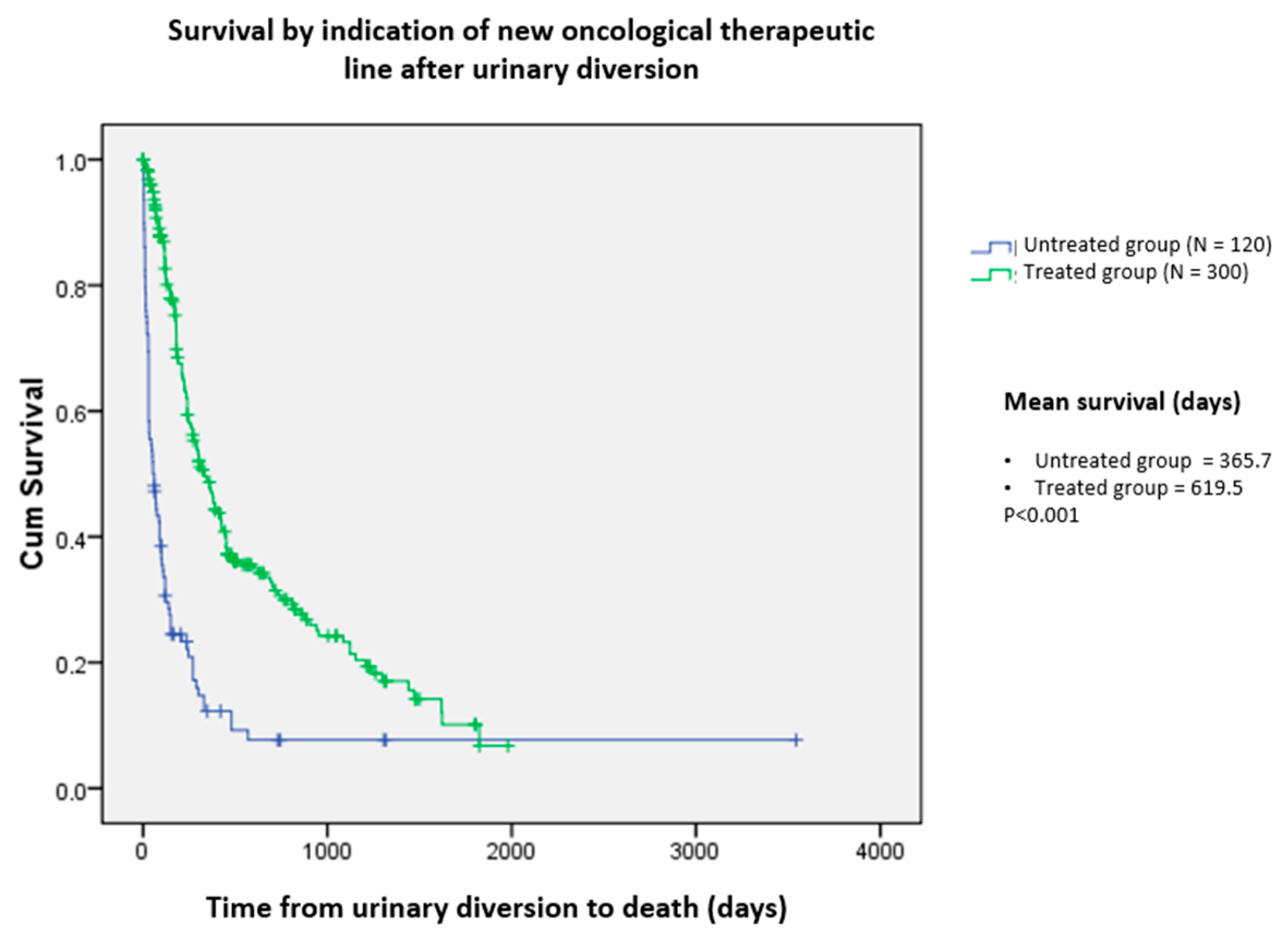
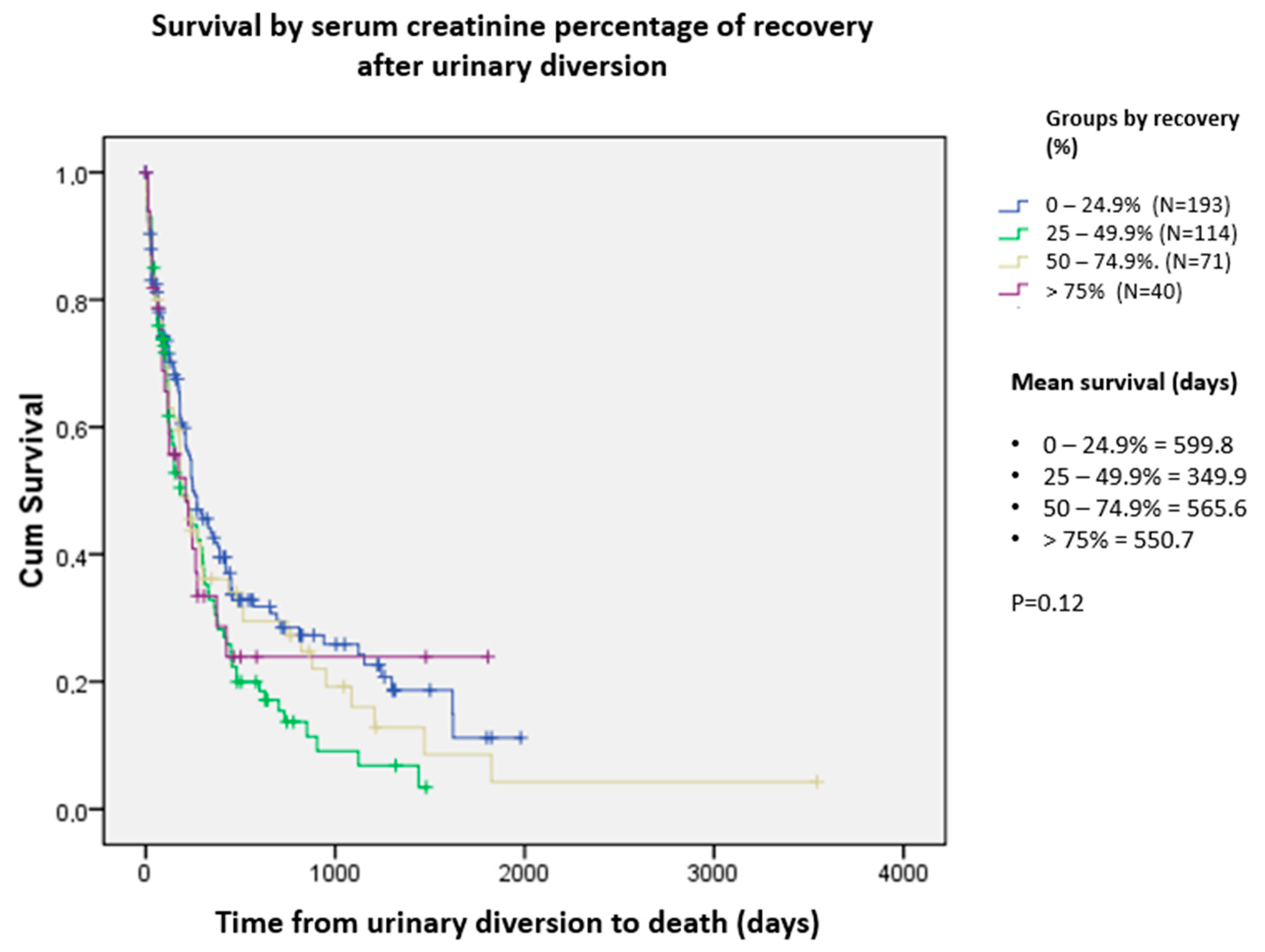
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Meldrum, K.K. Chapter 48-Pathophysiology of Urinary Tract Obstruction. In Campbell-Walsh Urology, 11th ed.; Wein, A.J., Ed.; Elsevier: Amsterdam, The Netherlands, 2016; pp. 1104–1147. [Google Scholar]
- Hsu, L.; Li, H.; Pucheril, D.; Hansen, M.; Littleton, R.; Peabody, J.; Sammon, J. Use of percutaneous nephrostomy and ureteral stenting in management of ureteral obstruction. World J. Nephrol. 2016, 5, 172–181. [Google Scholar] [CrossRef] [PubMed]
- Song, S.H.; Pak, S.; Jeong, I.G.; Kim, K.S.; Park, H.K.; Kim, C.-S.; Ahn, H.; Hong, B. Outcomes of stent-change therapy for bilateral malignancy-related ureteral obstruction. Int. Urol. Nephrol. 2015, 47, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Chitale, S.V.; Scott-Barrett, S.; Ho, E.T.; Burgess, N.A. The management of ureteric obstruction secondary to malignant pelvic disease. Clin. Radiol. 2002, 57, 1118–1121. [Google Scholar] [CrossRef] [PubMed]
- Chung, S.Y.; Stein, R.J.; Landsittel, D.; Davies, B.J.; Cuellar, D.C.; Hrebinko, R.L.; Tarin, T.; Averch, T.D. 15-year expe-rience with the management of extrinsic ureteral obstruction with indwelling ureteral stents. J. Urol. 2004, 172, 592–595. [Google Scholar] [CrossRef]
- Sountoulides, P.; Mykoniatis, I.; Dimasis, N. Palliative management of malignant upper urinary tract obstruction. Hippokratia. 2014, 18, 292–297. [Google Scholar]
- Sountoulides, P.; Pardalidis, N.; Sofikitis, N. Endourologic management of malignant ureteral obstruction: Indications, results, and quality-of-life issues. J. Endourol. 2010, 24, 129–142. [Google Scholar] [CrossRef]
- Fiuk, J.; Bao, Y.; Calleary, J.G.; Schwartz, B.F.; Denstedt, J.D. The use of internal stents in chronic ureteral obstruction. J. Urol. 2015, 193, 1092–1100. [Google Scholar] [CrossRef]
- Izumi, K.; Mizokami, A.; Maeda, Y.; Koh, E.; Namiki, M. Current outcome of patients with ureteral stents for the management of malignant ureteral obstruction. J. Urol. 2011, 185, 556–561. [Google Scholar] [CrossRef]
- Ishioka, J.; Kageyama, Y.; Inoue, M.; Higashi, Y.; Kihara, K. Prognostic model for predicting sur-vival after palliative urinary diversion for ureteral obstruction: Analysis of 140 cases. J. Urol. 2008, 180, 618–621, discussion 21. [Google Scholar] [CrossRef]
- Kouba, E.; Wallen, E.M.; Pruthi, R.S. Management of ureteral obstruction due to advanced ma-lignancy: Optimizing therapeutic and palliative outcomes. J. Urol. 2008, 180, 444–450. [Google Scholar] [CrossRef]
- Lev-Chelouche, D.; Keidar, A.; Rub, R.; Matzkin, H.; Gutman, M. Hydronephrosis associated with colorectal carcinoma: Treatment and outcome. Eur. J. Surg. Oncol. 2001, 27, 482–486. [Google Scholar] [CrossRef] [PubMed]
- Friedlander, J.I.; Duty, B.D.; Okeke, Z.; Smith, A.D. Obstructive uropathy from locally advanced and metastatic prostate cancer: An old problem with new therapies. J. Endourol. 2012, 26, 102–109. [Google Scholar] [CrossRef]
- Ganatra, A.M.; Loughlin, K.R. The management of malignant ureteral obstruction treated with ureteral stents. J. Urol. 2005, 174, 2125–2128. [Google Scholar] [CrossRef] [PubMed]
- Prentice, J.; Amer, T.; Tasleem, A.; Aboumarzouk, O. Malignant ureteric obstruction decom-pression: How much gain for how much pain? A narrative review. J. R. Soc. Med. 2018, 111, 125–135. [Google Scholar] [CrossRef]
- Alawneh, A.; Tuqan, W.; Innabi, A.; Al-Nimer, Y.; Azzouqah, O.; Rimawi, D.; Taqash, A.; Elkhatib, M.; Klepstad, P. Clinical Factors Associated With a Short Survival Time After Percutaneous Nephrostomy for Ureteric Obstruction in Cancer Patients: An Updated Model. J. Pain. Symptom Manag. 2016, 51, 255–261. [Google Scholar] [CrossRef]
- Azuma, T.; Nagase, Y.; Oshi, M. Prognostic marker for patients with malignant ureter obstruction. Clin. Genitourin. Cancer 2013, 11, 353–356. [Google Scholar] [CrossRef] [PubMed]
- Cordeiro, M.D.; Coelho, R.F.; Chade, D.C.; Pessoa, R.R.; Chaib, M.S.; Colombo-Júnior, J.R.; Pontes-Júnior, J.; Guglielmetti, G.B.; Srougi, M. A prognostic model for survival after palliative urinary diversion for malignant ureteric obstruction: A prospective study of 208 patients. BJU Int. 2016, 117, 266–271. [Google Scholar] [CrossRef]
- New, F.; Deverill, S.; Somani, B.K. Role of percutaneous nephrostomy in end of life prostate cancer patients: A systematic review of the literature. Cent. Eur. J. Urol. 2018, 71, 404–409. [Google Scholar]
- Chiou, R.K.; Chang, W.Y.; Horan, J.J. Ureteral obstruction associated with prostate cancer: The outcome after percutaneous nephrostomy. J. Urol. 1990, 143, 957–959. [Google Scholar] [CrossRef]
- Oefelein, M.G. Prognostic significance of obstructive uropathy in advanced prostate cancer. Urology 2004, 63, 1117–1121. [Google Scholar] [CrossRef]
- Lapitan, M.C.; Buckley, B.S. Impact of palliative urinary diversion by percutaneous nephrosto-my drainage and ureteral stenting among patients with advanced cervical cancer and obstructive uropathy: A prospective cohort. J. Obs. Obstet. Gynaecol. Res. 2011, 37, 1061–1070. [Google Scholar] [CrossRef] [PubMed]
- Dienstmann, R.; da Silva Pinto, C.; Pereira, M.T.; Small, I.A.; Ferreira, C.G. Palliative percutaneous nephrostomy in recurrent cervical cancer: A retrospective analysis of 50 consecutive cases. J. Pain. Symptom Manag. 2008, 36, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Noegroho, B.S.; Kurniawan, A.P.; Wijayanti, Z.; Mustafa, A. Factors Affecting Survival Outcome After Percutaneous Nephrostomy as Palliative Urinary Diversion in Obstructive Uropathy due to Advance Cervical Cancer Patients. Asian Pac. J. Cancer Prev. 2021, 22, 1211–1216. [Google Scholar] [CrossRef] [PubMed]
| Variable | Subcategories | N | % |
|---|---|---|---|
| Sex | Female | 250 | 59.52 |
| Male | 170 | 40.48 | |
| Ethnicity | Caucasian | 241 | 57.38 |
| Black | 84 | 20.00 | |
| Brown | 41 | 9.76 | |
| Not reported | 54 | 12.86 | |
| Comorbidities | Arterial Hypertension | 136 | 32.38 |
| Diabetes | 60 | 14.28 | |
| Dyslipidemia | 8 | 1.90 | |
| Obesity | 6 | 1.42 | |
| Smoking | 86 | 20.47 | |
| Others | 84 | 20.00 | |
| Not reported | 40 | 9.55 | |
| Laterality | Right side | 118 | 28.1 |
| Of Obstruction | Left side | 114 | 27.1 |
| Bilateral | 188 | 44.8 | |
| Kidney Units | Right side | 306 | 50.3 |
| Compromised | Left side | 302 | 49.7 |
| Total | 608 | 100.0 | |
| Urinary diversion | Ureteral stent | 423 | 69.6 |
| Procedure by | Nephrostomy | 176 | 28.9 |
| Kidney Unit | Not drained | 9 | 1.5 |
| Complications | Infection | 25 | 71.4 |
| Bleeding | 5 | 14 | |
| Urinary tract perforation | 3 | 8.3 | |
| Nephrectomy | 1 | 2.9 | |
| Vaginal fistula | 1 | 2.9 | |
| Total | 35 | 100.0 |
| Type of Neoplasm | Etiology | No. | % of Total | Relative % |
|---|---|---|---|---|
| Urological | Bladder | 78 | 18.6 | 57.4 |
| Prostate | 48 | 11.4 | 35.3 | |
| Pelvis/Ureter | 6 | 1.4 | 4.4 | |
| Testicle | 2 | 0.5 | 1.5 | |
| Kidney | 1 | 0.2 | 0.7 | |
| Urethra | 1 | 0.2 | 0.7 | |
| Total 1 | 136 | 32.4 | 100 | |
| Non-urological | Uterine cervix | 152 | 36.2 | 53.9 |
| Rectum/Colon | 73 | 17.4 | 25.9 | |
| Lymphoma | 14 | 3.3 | 5.0 | |
| Uterus/Endometrium | 11 | 2.6 | 3.9 | |
| Ovary | 8 | 1.9 | 2.8 | |
| Stomach | 6 | 1.4 | 2.1 | |
| Mama | 5 | 1.2 | 1.8 | |
| Retroperitoneum | 2 | 0.5 | 0.7 | |
| Sarcoma | 2 | 0.5 | 0.7 | |
| Liposarcoma | 2 | 0.5 | 0.7 | |
| Peritoneum | 2 | 0.5 | 0.7 | |
| Neuroendocrine | 2 | 0.5 | 0.7 | |
| Pancreas | 2 | 0.5 | 0.7 | |
| Schwanoma | 2 | 0.5 | 0.7 | |
| Vagina | 1 | 0.2 | 0.4 | |
| Total | 284 | 67.6 | 100 |
| Variable | Pre-Drainage Creatinine (T0) | Post-Drainage Creatinine (T1) | Latest Creatinine (T2) | |
|---|---|---|---|---|
| Sex | Male Female p value | 3.8240 3.1964 0.05 | 2.0085 1.7266 0.05 | 2.9204 2.3805 0.01 |
| Type of neoplasm | Urological | 4.2598 | 2.0178 | 2.8374 |
| Non-urological | 3.0629 | 1.7560 | 2.4849 | |
| p value | 0.001 | 0.08 | 0.12 | |
| Primary site | Bladder | 4.5531 | 2.0051 | 2.9508 |
| Prostate | 4.0006 | 2.1951 | 2.8568 | |
| Cervix | 3.5407 | 1.8625 | 2.4044 | |
| Colorectal | 2.1874 | 1.4985 | 3.0089 | |
| Stage of the disease | Metastatic | 3.3631 | 1.8799 | 2.5827 |
| Locally advanced | 3.4887 | 1.8236 | 2.6062 | |
| p value | 0.71 | 0.71 | 0.91 | |
| Obstruction Laterality | Bilateral | 4.8325 | 2.3992 | 3.1101 |
| Unilateral | 2.3299 | 1.3813 | 2.1789 | |
| p value | <0.001 | <0.001 | <0.001 | |
| Type of procedure | Percutaneous nephrostomy | 5.1368 | 2.2253 | 3.1743 |
| Double J | 3.4109 | 1.8687 | 2.4869 | |
| p value | <0.001 | 0.07 | 0.01 | |
| Patient Current | Alive | 3.2226 | 1.6172 | 1.6567 |
| Status | Dead | 3.5536 | 1.9565 | 3.1382 |
| p value | 0.32 | 0.01 | <0.001 |
| Urological Neoplasms | N | Average (Days) | Standard Deviation | Non-Urological Neoplasms | N | Average (Days) | Standard Deviation |
|---|---|---|---|---|---|---|---|
| Bladder | 45 | 158.58 | 205.750 | Uterine cervix | 96 | 292.00 | 356.236 |
| Prostate | 28 | 367.36 | 400.111 | Rectum/colon | 54 | 209.09 | 212.315 |
| Pelvis/ureter | 1 | 120 | - | Lymphoma | 9 | 211.56 | 316.908 |
| Total | 74 | 237.05 | 308.583 | Uterus/endometrium | 8 | 147.88 | 124.246 |
| Stomach | 5 | 123.20 | 153.521 | ||||
| Ovary | 3 | 588.00 | 896.600 | ||||
| Total | 175 | 255.94 | 320.129 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cartapatti, M.; Machado, R.D.; Mesquita, J.C.; Freua, R.; Cáceres, D.; dos Reis, R.B. Urinary Diversion Can Improve the Chance of Implementing New Therapeutic Lines in Patients with Malignant Ureteral Obstruction: A Multicenter Study. Curr. Oncol. 2024, 31, 7107-7116. https://doi.org/10.3390/curroncol31110523
Cartapatti M, Machado RD, Mesquita JC, Freua R, Cáceres D, dos Reis RB. Urinary Diversion Can Improve the Chance of Implementing New Therapeutic Lines in Patients with Malignant Ureteral Obstruction: A Multicenter Study. Current Oncology. 2024; 31(11):7107-7116. https://doi.org/10.3390/curroncol31110523
Chicago/Turabian StyleCartapatti, Marcelo, Roberto Dias Machado, José Carlos Mesquita, Raphael Freua, Diego Cáceres, and Rodolfo Borges dos Reis. 2024. "Urinary Diversion Can Improve the Chance of Implementing New Therapeutic Lines in Patients with Malignant Ureteral Obstruction: A Multicenter Study" Current Oncology 31, no. 11: 7107-7116. https://doi.org/10.3390/curroncol31110523
APA StyleCartapatti, M., Machado, R. D., Mesquita, J. C., Freua, R., Cáceres, D., & dos Reis, R. B. (2024). Urinary Diversion Can Improve the Chance of Implementing New Therapeutic Lines in Patients with Malignant Ureteral Obstruction: A Multicenter Study. Current Oncology, 31(11), 7107-7116. https://doi.org/10.3390/curroncol31110523





