Evaluation of the Impact of the Urgent Cancer Care Clinic on Emergency Department Visits, Primary Care Clinician Visits, and Hospitalizations in Winnipeg, Manitoba
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Intervention
2.3. Study Design
2.4. Data Sources and Study Population
2.5. Outcomes
2.6. Statistical Analyses
3. Results
3.1. Characteristics of the Study Cohort
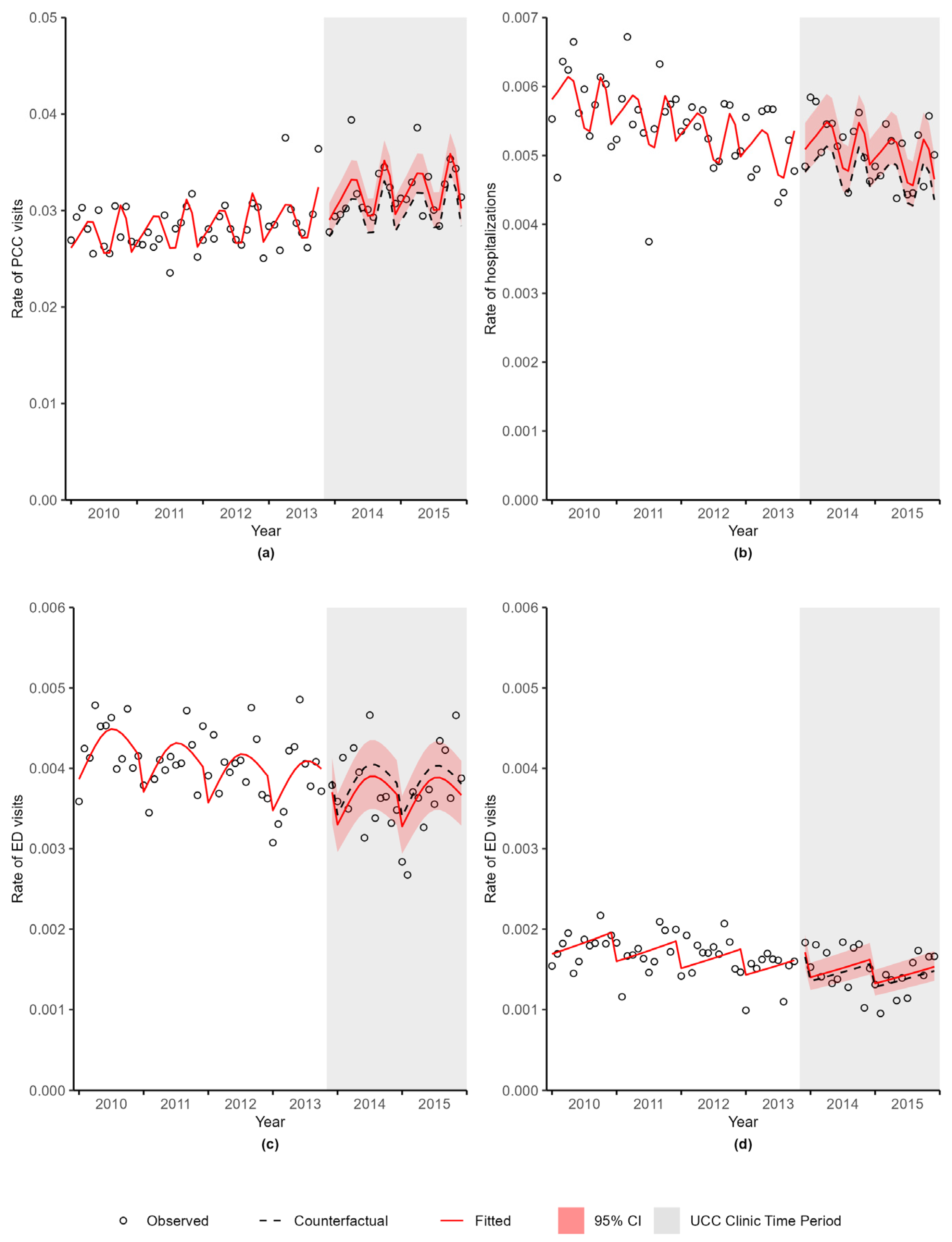
3.2. PCC Visits
3.3. Hospitalizations
3.4. ED Visits
3.5. ED Visit Subgroup Analyses
3.6. Sensitivity Analysis
4. Discussion
4.1. Main Findings
4.2. Comparison with Previous Studies
4.3. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lix, L.; Smith, M.; Pitz, M.; Ahmed, R.; Quon, H.; Griffith, J.; Turner, D.; Hong, S.; Prior, H.; Banerjee, A.; et al. Cancer Data Linkage in Manitoba: Expanding the Infrastructure for Research; Manitoba Centre for Health Policy: Winnipeg, MB, Canada, 2016. [Google Scholar]
- Enright, K.; Grunfeld, E.; Yun, L.; Moineddin, R.; Ghannam, M.; Dent, S.; Eisen, A.; Trudeau, M.; Kaizer, L.; Earle, C.; et al. Population-based assessment of emergency room visits and hospitalizations among women receiving adjuvant chemotherapy for early breast cancer. J. Oncol. Pract. 2015, 11, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Hassett, M.J.; O’Malley, A.J.; Pakes, J.R.; Newhouse, J.P.; Earle, C.C. Frequency and costs of chemotherapy-related serious adverse effects in a population sample of women with breast cancer. J. Natl. Cancer Inst. 2006, 98, 1108–1117. [Google Scholar] [CrossRef]
- Lash, R.S.; Hong, A.S.; Bell, J.F.; Reed, S.C.; Pettit, N. Recognizing the emergency department’s role in oncologic care: A review of the literature on unplanned acute care. Emerg. Cancer Care 2022, 1, 6. [Google Scholar] [CrossRef] [PubMed]
- Shelburne, N.; Simonds, N.I.; Jensen, R.E.; Brown, J. Cancer-related emergency and urgent care: Expanding the research agenda. Emerg. Cancer Care 2022, 1, 4. [Google Scholar] [CrossRef] [PubMed]
- Rivera, D.R.; Gallicchio, L.; Brown, J.; Liu, B.; Kyriacou, D.N.; Shelburne, N. Trends in adult cancer-related emergency department utilization: An analysis of data from the Nationwide Emergency Department Sample. JAMA Oncol. 2017, 3, e172450. [Google Scholar] [CrossRef]
- Hsu, J.; Donnelly, J.P.; Moore, J.X.; Meneses, K.; Williams, G.; Wang, H.E. National characteristics of Emergency Department visits by patients with cancer in the United States. Am. J. Emerg. Med. 2018, 36, 2038–2043. [Google Scholar] [CrossRef]
- VanDyk, A.D.; Harrison, M.B.; Macartney, G.; Ross-White, A.; Stacey, D. Emergency department visits for symptoms experienced by oncology patients: A systematic review. Support. Care Cancer 2012, 20, 1589–1599. [Google Scholar] [CrossRef]
- Lash, R.S.; Bell, J.F.; Reed, S.C.; Poghosyan, H.; Rodgers, J.; Kim, K.K.; Bold, R.J.; Joseph, J.G. A systematic review of emergency department use among cancer patients. Cancer Nurs. 2017, 40, 135–144. [Google Scholar] [CrossRef]
- Caterino, J.M.; Adler, D.; Durham, D.D.; Yeung, S.C.J.; Hudson, M.F.; Bastani, A.; Bernstein, S.L.; Baugh, C.W.; Coyne, C.J.; Grudzen, C.R. Analysis of diagnoses, symptoms, medications, and admissions among patients with cancer presenting to emergency departments. JAMA Netw. Open 2019, 2, e190979. [Google Scholar] [CrossRef]
- Elsayem, A.F.; Merriman, K.W.; Gonzalez, C.E.; Yeung, S.C.J.; Chaftari, P.S.; Reyes-Gibby, C.; Todd, K.H. Presenting symptoms in the emergency department as predictors of intensive care unit admissions and hospital mortality in a comprehensive cancer center. J. Oncol. Pract. 2016, 12, e554–e563. [Google Scholar] [CrossRef]
- Gallaway, M.S.; Idaikkadar, N.; Tai, E.; Momin, B.; Rohan, E.A.; Townsend, J.; Puckett, M.; Stewart, S.L. Emergency department visits among people with cancer: Frequency, symptoms, and characteristics. J. Am. Coll. Emerg. Physicians Open 2021, 2, e12438. [Google Scholar] [CrossRef] [PubMed]
- McKenzie, H.; Hayes, L.; White, K.; Cox, K.; Fethney, J.; Boughton, M.; Dunn, J. Chemotherapy outpatients’ unplanned presentations to hospital: A retrospective study. Support. Care Cancer 2011, 19, 963–969. [Google Scholar] [CrossRef]
- Saxena, A.; Rubens, M.; Ramamoorthy, V.; Tonse, R.; Veledar, E.; McGranaghan, P.; Sundil, S.; Chuong, M.D.; Hall, M.D.; Odia, Y.; et al. Hospitalization rates for complications due to systemic therapy in the United States. Sci. Rep. 2021, 11, 7385. [Google Scholar] [CrossRef]
- Ahn, S.; Lee, Y.S.; Lim, K.S. Emergency department cancer unit and management of oncologic emergencies: Experience in Asan Medical Center. Support. Care Cancer 2012, 20, 2205–2210. [Google Scholar] [CrossRef]
- Mazur, K.A.; McCarthy, K.; Suell, M.N.; Hockenberry, M.J. An outpatient urgent care bay within a pediatric cancer and hematology center. J. Ped. Oncol. Nurs. 2012, 29, 206–210. [Google Scholar] [CrossRef] [PubMed]
- Oatley, M.; Fry, M. A nurse practitioner-led model of care improves access, early assessment and integration of oncology services: An evaluation study. Support. Care Cancer 2020, 28, 5023–5029. [Google Scholar] [CrossRef]
- Xiao, H.; Fahy, R.; Salvaggio, R.; OSullivan, M.; Sokoli, D.; Murray, C.; Majeed, J.; Mao, J.J.; Groeger, J.S. Implementation of symptom care clinic (SCC) for acute symptoms management at outpatient oncology ambulatory centers. J. Clin. Oncol. 2020, 38, 2030. [Google Scholar] [CrossRef]
- Coyle, Y.M.; Miller, A.M.; Paulson, R.S. Model for the cost-efficient delivery of continuous quality cancer care: A hospital and private-practice collaboration. Bayl. Univ. Med. Cent. Proc. 2013, 26, 95–99. [Google Scholar] [CrossRef]
- Hong, A.S.; Froehlich, T.; Clayton Hobbs, S.; Lee, S.J.C.; Halm, E.A. Impact of a cancer urgent care clinic on regional emergency department visits. J. Oncol. Pract. 2019, 15, e501–e509. [Google Scholar] [CrossRef]
- Sivendran, S.; Holliday, R.; De la Torre, K.; Newport, K.B. Impact of a nurse practitioner-staffed, symptom-management clinic on emergency department utilization in a large community oncology cancer institute. J. Clin. Oncol. 2014, 32 (Suppl. 31), 58. [Google Scholar] [CrossRef]
- Gould Rothberg, B.E.; Canavan, M.E.; Mun, S.; Sedghi, T.; Carafeno, T.; Raucci, M.; Dest, V.; Sinanis, N.; Gross, C.P.; Adelson, K.B. Impact of a dedicated cancer urgent care center on acute care utilization. JCO Oncol. Pract. 2022, 18, e129–e136. [Google Scholar] [CrossRef]
- Ruegg, T.A. A nurse practitioner-led urgent care center: Meeting the needs of the patient with cancer. Clin. J. Oncol. Nurs. 2013, 17, e52–e57. [Google Scholar] [CrossRef]
- Meisenberg, B.R.; Graze, L.; Brady-Copertino, C.J. A supportive care clinic for cancer patients embedded within an oncology practice. J. Community Support. Oncol. 2014, 12, 205–208. [Google Scholar] [CrossRef] [PubMed]
- Alfaro, E.; Quinn, M.; Baltic, T.; Acebedo, C.; Israni, M.; Miaskowski, C. Establishment of a cancer acute care clinic within an infusion center. Cancer Care Res. Online 2022, 2, e035. [Google Scholar] [CrossRef]
- Haugstetter, C.; Mason, R.; Sanmugarajah, J.; Hattingh, H.L. Evaluation of a new emergency department avoidance model of care, the Cancer Urgent Assessment Clinic, in response to the COVID-19 pandemic. Emerg. Cancer Care 2022, 1, 11. [Google Scholar] [CrossRef]
- Decker, K.; Lambert, P.; Galloway, K.; Bucher, O.; Pitz, M.; Goldenberg, B.; Singh, H.; Kristjanson, M.; Fatoye, T.; Bow, E.J. Predictors of urgent cancer care clinic and emergency department visits for individuals diagnosed with cancer. Curr. Oncol. 2021, 28, 1773–1789. [Google Scholar] [CrossRef]
- Bernal, J.L.; Cummins, S.; Gasparrini, A. Interrupted time series regression for the evaluation of public health interventions: A tutorial. Int. J. Epidemiol. 2017, 46, 348–355. [Google Scholar] [CrossRef] [PubMed]
- North American Association of Central Cancer Registries. NAACCR—Certification Criteria. Available online: https://www.naaccr.org/certification-criteria/ (accessed on 19 January 2023).
- Roos, L.L.; Mustard, C.A.; Nicol, J.P.; McLerran, D.F.; Malenka, D.J.; Young, T.K.; Cohen, M.M. Registries and administrative data: Organization and accuracy. Med. Care 1993, 31, 201–212. [Google Scholar] [CrossRef]
- Robinson, J.R.; Young, T.K.; Roos, L.L.; Gelskey, D.E. Estimating the burden of disease. Comparing administrative data and self-reports. Med. Care 1997, 35, 932–947. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, G. Generalized Linear Models. 4. A Model for Overdispersed Count Data; Princeton University: Princeton, NJ, USA, 2023; Available online: https://grodri.github.io/glms/r/overdispersion (accessed on 19 January 2023).
- Hartig, F. DHARMa: Residual Diagnostics for Hierarchical (Multi-Level/Mixed) Regression Models; University of Regensberg: Regensberg, Germany, 2022; Available online: https://cran.r-project.org/web/packages/DHARMa/vignettes/DHARMa.html (accessed on 19 January 2023).
- Bhaskaran, K.; Gasparrini, A.; Hajat, S.; Smeeth, L.; Armstrong, B. Time series regression studies in environmental epidemiology. Int. J. Epidemiol. 2013, 42, 1187–1195. [Google Scholar] [CrossRef] [PubMed]
- McFadden, D. Conditional logit analysis of qualitative choice behavior. In Frontiers in Economics; Zarembka, P., Ed.; Academic Press: New York, NY, USA, 1974; pp. 104–142. [Google Scholar]
- Sansone, R.A.; Sansone, L.A. Doctor shopping: A phenomenon of many themes. Innovat. Clin. Neurosci. 2012, 9, 42–46. [Google Scholar]
- Jiang, L.; Lofters, A.; Moineddin, R.; Decker, K.; Groome, P.; Kendell, C.; Krzyzanowska, M.; Li, D.; McBride, M.L.; Mittmann, N.; et al. Primary care physician use across the breast cancer care continuum: CanIMPACT study using Canadian administrative data. Can. Fam. Physician 2016, 62, e589–e598. [Google Scholar] [PubMed]
- Manitoba Health Healthy Living and Seniors; Epidemiology and Surveillance; Public Health Branch; Public Health and Primary Health Care Division. Annual Influenza Report, 2014–2015; Government of Manitoba: Winnipeg, MB, Canada, 2015. [Google Scholar]
- Pedrazzoli, P.; Baldanti, F.; Donatelli, I.; Castrucci, M.R.; Puglisi, F.; Silvestris, N.; Cinieri, S.; Italian Society of Medical Oncology. Vaccination for seasonal influenza in patients with cancer: Recommendations of the Italian Society of Medical Oncology (AIOM). Ann. Oncol. 2014, 25, 1243–1247. [Google Scholar] [CrossRef] [PubMed]
- Goyal, R.K.; Nagar, S.P.; Kabadi, S.M.; Le, H.; Davis, K.L.; Kaye, J.A. Overall survival, adverse events, and economic burden in patients with chronic lymphocytic leukemia receiving systemic therapy: Real world evidence from the medicare population. Cancer Med. 2021, 10, 2690–2702. [Google Scholar] [CrossRef]
- CancerCare Manitoba. Manitoba Cancer System Performance Report—2019; CancerCare Manitoba: Winnipeg, MB, Canada, 2019. [Google Scholar]

| Characteristic | Before UCC Clinic (N = 12,323) | After UCC Clinic (N = 6477) | p-Value |
|---|---|---|---|
| Median age at diagnosis (IQR) | 66 (57–76) | 67 (58–76) | 0.0929 |
| Sex (%) | |||
| Female | 54.3 | 53.1 | |
| Male | 45.7 | 46.9 | 0.1234 |
| Cancer type (%) | |||
| Breast | 18.5 | 16.9 | |
| Digestive | 19.4 | 19.8 | |
| Lung | 12.3 | 13.7 | |
| Genitourinary | 23.7 | 23.6 | |
| Hematologic | 10.3 | 10.4 | |
| Other | 15.8 | 15.6 | 0.0248 |
| Stage at diagnosis (%) | |||
| I | 26.2 | 25.5 | |
| II | 23.2 | 23.3 | |
| III | 17.4 | 17.1 | |
| IV | 21.0 | 21.9 | |
| Unknown or Not Applicable | 12.3 | 12.1 | 0.5551 |
| Systemic therapy within six months of diagnosis (%) | |||
| Yes | 42.7 | 46.3 | |
| No | 57.3 | 53.7 | <0.0001 |
| Radiation therapy within six months of diagnosis (%) | |||
| Yes | 24.7 | 25.9 | |
| No | 75.3 | 74.1 | 0.0883 |
| Surgery within six months of diagnosis (%) | |||
| Yes | 53.9 | 47.9 | |
| No | 46.1 | 52.1 | <0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galloway, K.; Lambert, P.; Bow, E.J.; Czaykowski, P.; Fatoye, T.; Goldenberg, B.; Kristjanson, M.; Singh, H.; Bucher, O.; Decker, K. Evaluation of the Impact of the Urgent Cancer Care Clinic on Emergency Department Visits, Primary Care Clinician Visits, and Hospitalizations in Winnipeg, Manitoba. Curr. Oncol. 2023, 30, 6771-6785. https://doi.org/10.3390/curroncol30070496
Galloway K, Lambert P, Bow EJ, Czaykowski P, Fatoye T, Goldenberg B, Kristjanson M, Singh H, Bucher O, Decker K. Evaluation of the Impact of the Urgent Cancer Care Clinic on Emergency Department Visits, Primary Care Clinician Visits, and Hospitalizations in Winnipeg, Manitoba. Current Oncology. 2023; 30(7):6771-6785. https://doi.org/10.3390/curroncol30070496
Chicago/Turabian StyleGalloway, Katie, Pascal Lambert, Eric J. Bow, Piotr Czaykowski, Tunji Fatoye, Benjamin Goldenberg, Mark Kristjanson, Harminder Singh, Oliver Bucher, and Kathleen Decker. 2023. "Evaluation of the Impact of the Urgent Cancer Care Clinic on Emergency Department Visits, Primary Care Clinician Visits, and Hospitalizations in Winnipeg, Manitoba" Current Oncology 30, no. 7: 6771-6785. https://doi.org/10.3390/curroncol30070496
APA StyleGalloway, K., Lambert, P., Bow, E. J., Czaykowski, P., Fatoye, T., Goldenberg, B., Kristjanson, M., Singh, H., Bucher, O., & Decker, K. (2023). Evaluation of the Impact of the Urgent Cancer Care Clinic on Emergency Department Visits, Primary Care Clinician Visits, and Hospitalizations in Winnipeg, Manitoba. Current Oncology, 30(7), 6771-6785. https://doi.org/10.3390/curroncol30070496





