The Incidence and Prevalence of Primary Central Nervous System (CNS) Tumours in Canada (2010–2017), and the Survival of Patients Diagnosed with CNS Tumours (2008–2017)
Abstract
1. Introduction
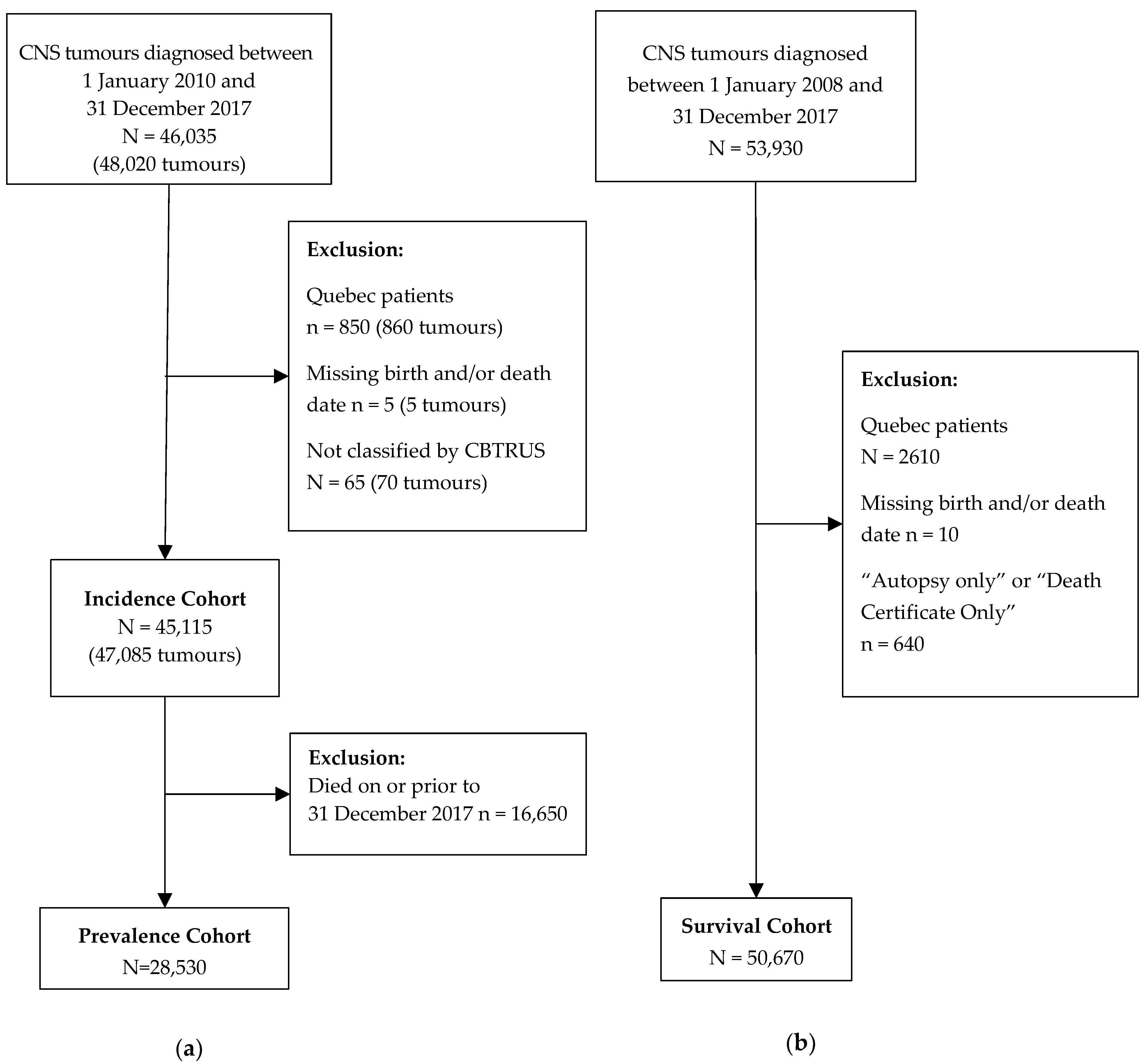
2. Methods
2.1. Data Sources
2.2. Tumour Classification
2.3. Study Population
2.4. Data Analysis
2.5. Multiple Primaries
2.6. Disclosure Rules and Rounding
3. Results
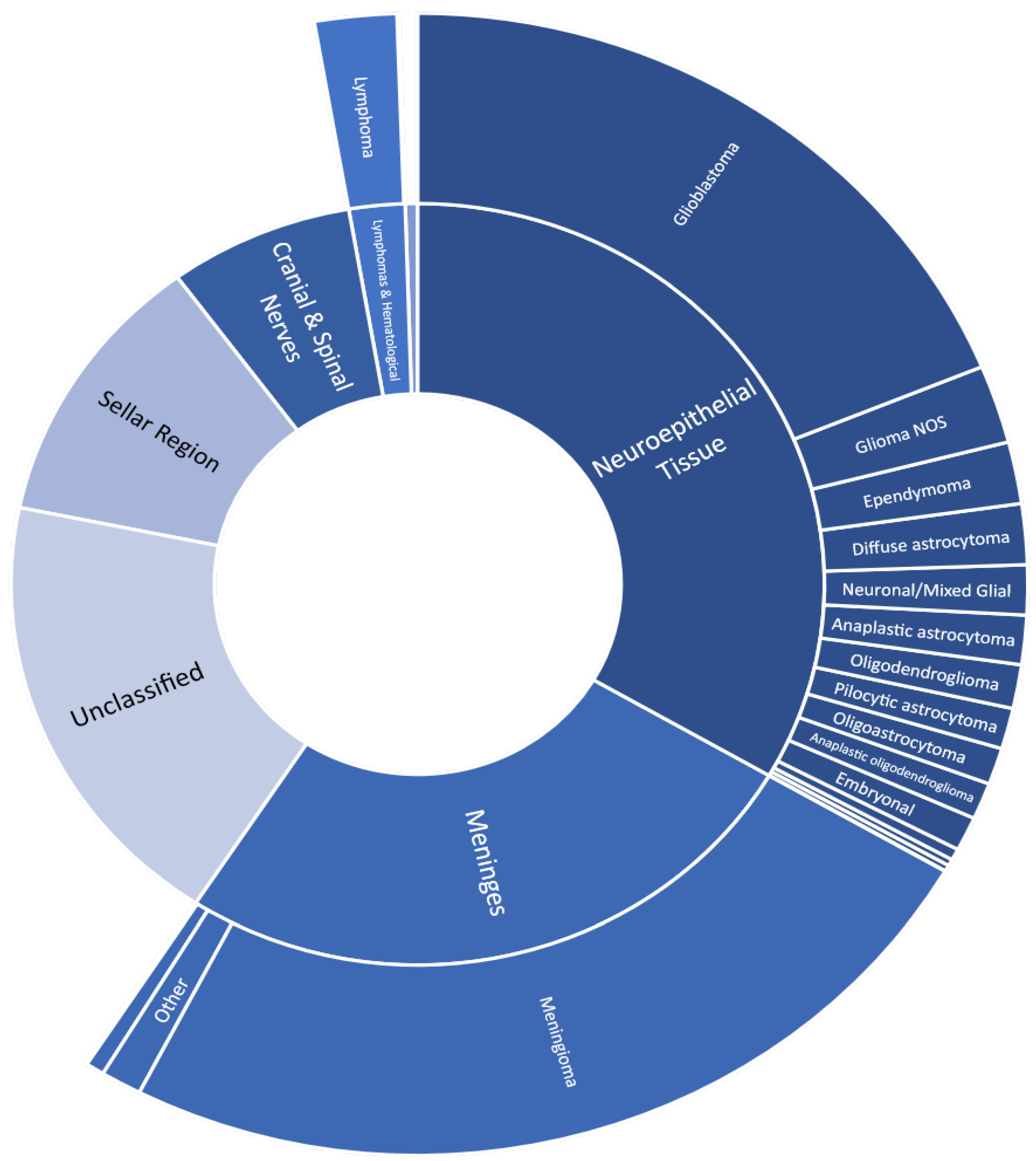
3.1. Incidence
3.1.1. Incidence Stratified by Sex
3.1.2. Incidence Stratified by Age
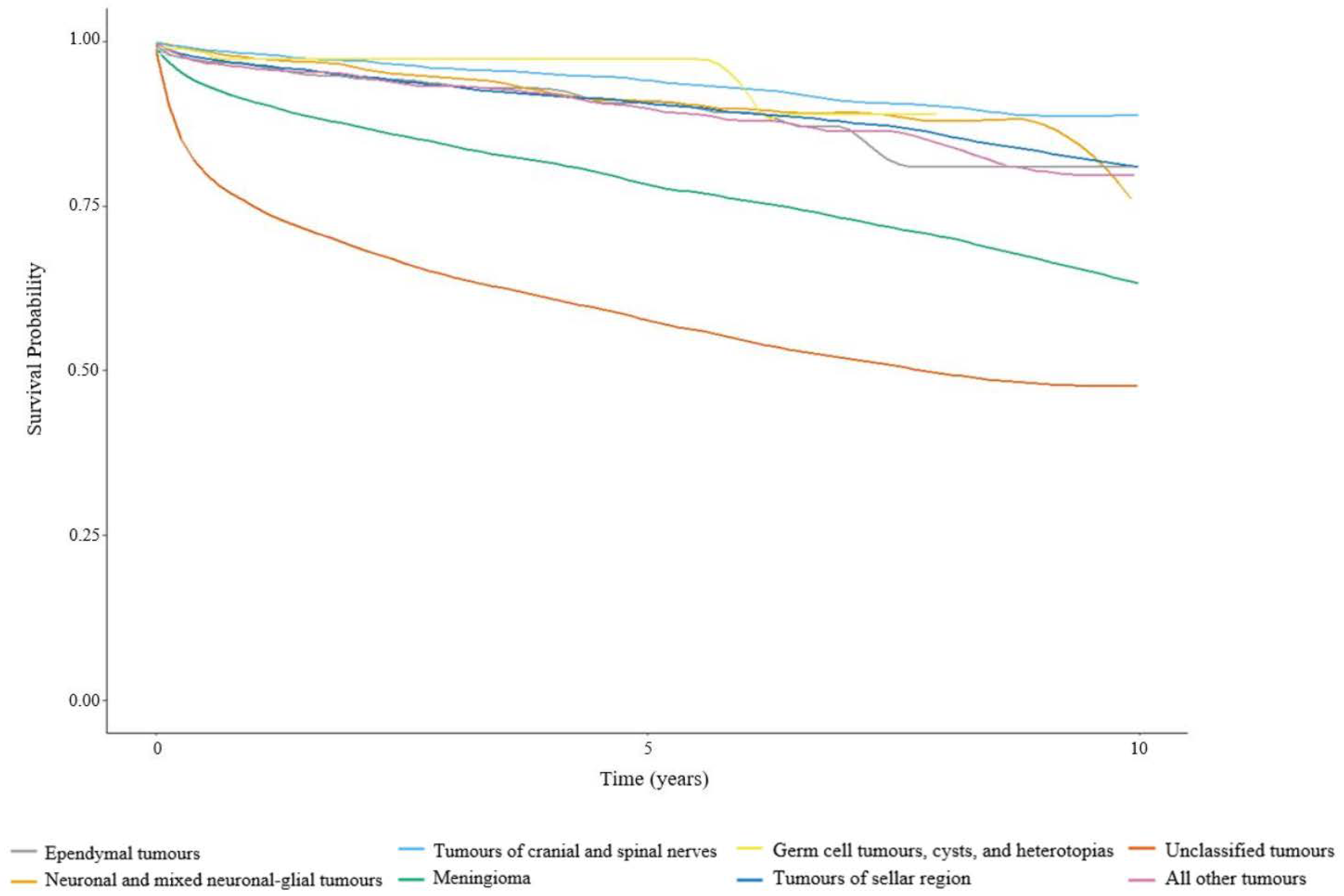
3.2. Survival
3.2.1. Survival Stratified by Age for Malignant Tumours
3.2.2. Survival Stratified by Age for Non-Malignant Tumours
3.3. Prevalence Stratified by Age and Tumour Behaviour
3.4. Unclassified Tumours
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- National Cancer Institute: Surveillance, Epidemiology and End Results Program. The 2007 Multiple Primary and Histology Coding Rules. Available online: https://seer.cancer.gov/tools/mphrules/2007_mphrules_manual_08242012.pdf (accessed on 19 December 2022).
- National Cancer Institute: Surveillance, Epidemiology and End Results Program. Solid Tumour Rules. Available online: https://seer.cancer.gov/tools/solidtumor/2023/STM_Combined.pdf (accessed on 19 December 2022).
- Eckstrand, A.C. CNS Tumours: Exploring Barriers to Registration and Feasibility of Extracting Molecular Characteristics. Master’s Thesis, University of Alberta, Edmonton, AB, Canada, 2018. [Google Scholar]
- Ellison, L.F. Progress in Net Cancer Survival in Canada over 20 Years. Health Rep. 2018, 29, 10–18. [Google Scholar] [PubMed]
- Davis, F.; Nagamuthu, C.; Ross, J.; Megyesi, J. Current Status of Brain Tumor Surveillance in Canada and Why It Matters. J. Registry. Manag. 2015, 42, 139–145. [Google Scholar] [PubMed]
- Canadian Cancer Statistics Advisory Committee in collaboration with the Canadian Cancer Society, Statistics Canada and the Public Health Agency of Canada. Canadian Cancer Statistics 2021. Available online: https://cdn.cancer.ca/-/media/files/research/cancer-statistics/2021-statistics/2021-pdf-en-final.pdf (accessed on 19 December 2022).
- Walker, E.V.; Zakaria, D.; Yuan, Y.; Yasmin, F.; Shaw, A.; Davis, F.G. Brain Tumour Registry of Canada (BTRC): Incidence (2013–2017) and Mortality (2014–2018) Report. Available online: https://braintumourregistry.ca/wp-content/uploads/2021/05/FINAL-Incidence-and-Mortality-Report-2021-logo-word-removed.pdf (accessed on 19 December 2022).
- Walker, E.V.; Liu, J.; Davis, F.G.; Climans, S.; Yuan, Y. Brain Tumour Registry of Canada (BTRC): Survival Report 2010–2017. Available online: https://braintumourregistry.ca/wp-content/uploads/2022/06/Brain-Tumour-Registry-of-Canada-Final-Survival-and-Prevalence-Report-June-2022.pdf (accessed on 19 December 2022).
- Journals No. 110—February 14, 2007 (39-1)—House of Commons of Canada. Available online: https://www.ourcommons.ca/DocumentViewer/en/39-1/house/sitting-110/journals#DOC--2699530 (accessed on 19 December 2022).
- Walker, E.V.; Davis, F.G.; Yasmin, F.; Smith, T.R.; Yuan, Y. Incidence and survival of primary central nervous system tumors diagnosed in 4 Canadian provinces from 2010 to 2015. Neuro-Oncol. Pract. 2022, 10, 203–213. [Google Scholar] [CrossRef] [PubMed]
- Government of Canada, S.C. Canadian Cancer Registry (CCR). Available online: https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=3207&Item_Id=1633&lang=en (accessed on 19 December 2022).
- International Association of Cancer Registries. International Classification of Diseases for Oncology, Third Edition (ICDO-3). Available online: http://www.iacr.com.fr/index.php?option=com_content&view=category&layout=blog&id=100&Itemid=577 (accessed on 19 December 2022).
- Louis, D.N.; Ohgaki, H.; Wiestler, O.D.; Cavenee, W.K. (Eds.) WHO Classification of Tumours of the Central Nervous System, 4th ed; International Agency for Research on Cancer: Lyon, France, 2007; Volume 1, ISBN 978-92-832-2430-3.
- Forjaz, G.; Barnholtz-Sloan, J.S.; Kruchko, C.; Siegel, R.; Negoita, S.; Ostrom, Q.T.; Dickie, L.; Ruhl, J.; Van Dyke, A.; Patil, N.; et al. An Updated Histology Recode for the Analysis of Primary Malignant and Nonmalignant Brain and Other Central Nervous System Tumors in the Surveillance, Epidemiology, and End Results Program. Neuro-Oncol. Adv. 2020, 3, vdaa175. [Google Scholar] [CrossRef] [PubMed]
- Nagamine, C.M.L.; de Goulart, B.N.G.; Ziegelmann, P.K. Net Survival in Survival Analyses for Patients with Cancer: A Scoping Review. Cancers 2022, 14, 3304. [Google Scholar] [CrossRef] [PubMed]
- Perme, M.P.; Stare, J.; Estève, J. On Estimation in Relative Survival. Biometrics 2012, 68, 113–120. [Google Scholar] [CrossRef] [PubMed]
- National Cancer Institute: Surveillance, Epidemiology and End Results Program. Hematopoietic Project. Available online: https://seer.cancer.gov/tools/heme/ (accessed on 19 December 2022).
- Ostrom, Q.T.; Patil, N.; Cioffi, G.; Waite, K.; Kruchko, C.; Barnholtz-Sloan, J.S. CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2013–2017. Neuro. Oncol. 2020, 22, iv1–iv96. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Y.; Amjad, S.; Eckstrand, A.; Sevick, R.; Scott, J.; Devji, S.; Bertrand, C.; King, M.; Brunka, V.; Maplethorpe, E.; et al. On Capturing Radiological Diagnoses of Brain Tumours To Provide Complete Population Data in Cancer Registries in Canada. J. Registry. Manag. 2018, 45, 167–172. [Google Scholar] [PubMed]
- Patel, A.P.; Fisher, J.L.; Nichols, E.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; Abraha, H.N.; Agius, D.; Alahdab, F.; Alam, T.; et al. Global, Regional, and National Burden of Brain and Other CNS Cancer, 1990–2016: A Systematic Analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 376–393. [Google Scholar] [CrossRef] [PubMed]
- Natukka, T.; Raitanen, J.; Haapasalo, H.; Auvinen, A. Incidence Trends of Adult Malignant Brain Tumors in Finland, 1990–2016. Acta Oncologica. 2019, 58, 990–996. [Google Scholar] [CrossRef] [PubMed]
- Visser, O.; Ardanaz, E.; Botta, L.; Sant, M.; Tavilla, A.; Minicozzi, P.; Hackl, M.; Zielonke, N.; Oberaigner, W.; Van Eycken, E.; et al. Survival of Adults with Primary Malignant Brain Tumours in Europe; Results of the EUROCARE-5 Study. Eur. J. Cancer 2015, 51, 2231–2241. [Google Scholar] [CrossRef] [PubMed]
- Brodbelt, A.; Greenberg, D.; Winters, T.; Williams, M.; Vernon, S.; Collins, V.P. Glioblastoma in England: 2007–2011. Eur. J. Cancer 2015, 51, 533–542. [Google Scholar] [CrossRef] [PubMed]
- Hoogendijk, R.; Van der Lugt, J.; Hoving, E.; Kremer, L.; Visser, O.; Wesseling, P.; van Vuurden, D.; Karim-Kos, H. The fifth edition of the World Health Organization Classification of Tumors of the Central Nervous System: Implications for cancer registries. Neuro. Oncol. 2022, 24, 1811–1814. [Google Scholar] [CrossRef] [PubMed]


| Total | Male | Female | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Histology Group b (Major/Specific) | % M e | ASIR | 95% CI | % M e | ASIR | 95% CI | % M e | ASIR | 95% CI | |||
| Tumours of neuroepithelial tissue | 1967 | 92.9 | 7.18 | 7.06–7.29 | 1137 | 93.1 | 8.56 | 8.38–8.74 | 830 | 92.7 | 5.90 | 5.76–6.04 |
| Pilocytic astrocytoma | 68 | 100.0 | 0.25 | 0.23–0.27 | 34 | 100.0 | 0.25 | 0.22–0.28 | 33 | 100.0 | 0.25 | 0.22–0.28 |
| Diffuse astrocytoma | 101 | 100.0 | 0.37 | 0.34–0.40 | 59 | 100.0 | 0.45 | 0.41–0.49 | 41 | 100.0 | 0.30 | 0.27–0.33 |
| Anaplastic astrocytoma | 82 | 100.0 | 0.30 | 0.28–0.32 | 44 | 100.0 | 0.33 | 0.29–0.36 | 38 | 100.0 | 0.28 | 0.25–0.31 |
| Unique astrocytoma variants | 19 | 70.4 | 0.07 | 0.06–0.08 | 12 | 68.9 | 0.09 | 0.07–0.11 | 8 | 73.0 | 0.05 | 0.04–0.07 |
| Glioblastoma | 1106 | 100.0 | 4.01 | 3.93–4.09 | 651 | 100.0 | 4.95 | 4.81–5.08 | 455 | 100.0 | 3.16 | 3.06–3.26 |
| Oligodendroglioma | 73 | 100.0 | 0.27 | 0.25–0.29 | 42 | 100.0 | 0.32 | 0.28–0.35 | 31 | 100.0 | 0.22 | 0.19–0.25 |
| Anaplastic oligodendroglioma | 61 | 100.0 | 0.23 | 0.21–0.25 | 36 | 100.0 | 0.27 | 0.24–0.30 | 26 | 100.0 | 0.19 | 0.16–0.21 |
| Oligoastrocytic tumours | 61 | 100.0 | 0.23 | 0.21–0.25 | 35 | 100.0 | 0.26 | 0.23–0.29 | 27 | 100.0 | 0.20 | 0.17–0.22 |
| Ependymal tumours | 103 | 58.7 | 0.38 | 0.35–0.40 | 59 | 57.1 | 0.44 | 0.40–0.48 | 43 | 60.6 | 0.32 | 0.28–0.35 |
| Glioma malignant, NOS c | 130 | 100.0 | 0.48 | 0.45–0.51 | 70 | 100.0 | 0.53 | 0.49–0.58 | 61 | 100.0 | 0.43 | 0.39–0.47 |
| Choroid plexus tumours | 11 | 10.9 | 0.04 | 0.03–0.05 | 5 | 11.1 | 0.04 | 0.03–0.05 | 6 | 10.8 | 0.05 | 0.03–0.06 |
| Neuronal & mixed neuronal-glial tumours | 83 | 17.4 | 0.31 | 0.29–0.33 | 49 | 18.5 | 0.36 | 0.32–0.39 | 35 | 15.8 | 0.26 | 0.23–0.29 |
| Tumours of the pineal region | 10 | 67.3 | 0.04 | 0.03–0.05 | 5 | 64.3 | 0.04 | 0.03–0.05 | 5 | 70.8 | 0.04 | 0.03–0.05 |
| Embryonal tumours | 57 | 97.7 | 0.21 | 0.19–0.23 | 35 | 98.4 | 0.25 | 0.22–0.28 | 22 | 96.6 | 0.16 | 0.14–0.19 |
| Other neuroepithelial tumours d | 1 | 80.0 | 0.01 | 0.00–0.01 | 1 * | 66.7 | - | - | 1 * | - | - | - |
| Tumours of cranial & spinal nerves | 433 | 0.9 | 1.59 | 1.54–1.65 | 213 | 0.8 | 1.60 | 1.52–1.67 | 220 | 1.0 | 1.59 | 1.52–1.67 |
| Tumours of meninges | 1518 | 3.0 | 5.54 | 5.44–5.64 | 483 | 4.7 | 3.72 | 3.61–3.84 | 1036 | 2.3 | 7.25 | 7.09–7.41 |
| Meningioma | 1422 | 2.1 | 5.18 | 5.09–5.28 | 433 | 3.0 | 3.35 | 3.24–3.47 | 989 | 1.7 | 6.91 | 6.76–7.06 |
| Mesenchymal tumours | 29 | 35.5 | 0.11 | 0.09–0.12 | 14 | 42.5 | 0.10 | 0.08–0.12 | 16 | 29.1 | 0.11 | 0.09–0.13 |
| Primary melanocytic lesions | 4 | 63.6 | 0.01 | 0.01–0.02 | 2 | 66.7 | 0.01 | 0.01–0.02 | 1 | 60.0 | 0.01 | 0.01–0.02 |
| Other neoplasms related to the meninges | 64 | 3.7 | 0.23 | 0.21–0.26 | 34 | 4.3 | 0.25 | 0.22–0.29 | 29 | 3.1 | 0.22 | 0.19–0.25 |
| Lymphomas & hematopoietic neoplasms | 130 | 99.8 | 0.47 | 0.44–0.50 | 73 | 100.0 | 0.55 | 0.51–0.60 | 58 | 99.6 | 0.40 | 0.36–0.43 |
| Lymphoma | 128 | 100.0 | 0.46 | 0.43–0.49 | 71 | 100.0 | 0.54 | 0.50–0.59 | 56 | 100.0 | 0.39 | 0.35–0.42 |
| Other hematopoietic neoplasms | 3 | 92.9 | 0.01 | 0.01–0.02 | 2 | 100.0 | 0.01 | 0.01–0.02 | 2 | 90.0 | 0.01 | 0.01–0.02 |
| Germ cell tumours, cysts, & heterotopias | 29 | 62.7 | 0.11 | 0.09–0.12 | 21 | 71.4 | 0.15 | 0.13–0.18 | 8 | 41.3 | 0.06 | 0.04–0.07 |
| Tumours of sellar region | 689 | 0.4 | 2.53 | 2.46–2.59 | 353 | 0.6 | 2.67 | 2.57–2.77 | 336 | 0.3 | 2.43 | 2.34–2.52 |
| Unclassified tumours | 1121 | - | 4.07 | 3.98–4.15 | 484 | - | 3.86 | 3.74–3.99 | 637 | - | 4.25 | 4.14–4.37 |
| Total | 5886 | 35.7 | 21.48 | 21.28–21.67 | 2762 | 43.7 | 21.11 | 20.83–21.39 | 3124 | 28.8 | 21.87 | 21.60–22.15 |
| Age Group (Years) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 to 14 | 15 to 39 | 40 to 64 | 65+ | |||||||||||||
| Histology Group b (Major/Specific) | % M e | ASIR | 95% CI | % M e | ASIR | 95% CI | % M e | ASIR | 95% CI | % M e | ASIR | 95% CI | ||||
| Tumours of neuroepithelial tissue | 166 | 85.2 | 3.70 | 3.50–3.91 | 310 | 81.9 | 3.40 | 3.26–3.53 | 809 | 96.3 | 8.48 | 8.27–8.69 | 682 | 96.3 | 16.74 | 16.30–17.20 |
| Pilocytic astrocytoma | 38 | 100.0 | 0.84 | 0.75–0.94 | 20 | 100.0 | 0.23 | 0.19–0.26 | 8 | 100.0 | 0.09 | 0.07–0.11 | 1 | 100.0 | 0.03 | 0.02–0.06 |
| Diffuse astrocytoma | 9 | 100.0 | 0.19 | 0.15–0.24 | 30 | 100.0 | 0.33 | 0.29–0.37 | 41 | 100.0 | 0.43 | 0.38–0.48 | 21 | 100.0 | 0.52 | 0.45–0.61 |
| Anaplastic astrocytoma | 3 | 100.0 | 0.06 | 0.04–0.09 | 25 | 100.0 | 0.28 | 0.24–0.32 | 34 | 100.0 | 0.35 | 0.31–0.40 | 21 | 100.0 | 0.50 | 0.43–0.58 |
| Unique astrocytoma variants | 4 | 40.0 | 0.09 | 0.06–0.13 | 8 | 62.5 | 0.08 | 0.06–0.11 | 4 | 94.7 | 0.05 | 0.04–0.07 | 3 | 94.7 | 0.08 | 0.05–0.12 |
| Glioblastoma | 8 | 100.0 | 0.18 | 0.14–0.23 | 53 | 100.0 | 0.58 | 0.52–0.64 | 506 | 100.0 | 5.28 | 5.12–5.45 | 539 | 100.0 | 13.25 | 12.85–13.65 |
| Oligodendroglioma d | 29 * | - | - | - | 29 * | 100.0 | 0.31 | 0.27–0.36 | 38 | 100.0 | 0.40 | 0.36–0.45 | 6 | 100.0 | 0.13 | 0.10–0.18 |
| Anaplastic oligodendroglioma d | 15 * | - | - | - | 15 * | 100.0 | 0.16 | 0.14–0.20 | 36 | 100.0 | 0.38 | 0.34–0.43 | 10 | 100.0 | 0.24 | 0.19–0.30 |
| Oligoastrocytic tumours | 1 | - | 0.01 | 0.00–0.03 | 22 | 100.0 | 0.24 | 0.20–0.27 | 31 | 100.0 | 0.33 | 0.29–0.37 | 8 | 100.0 | 0.20 | 0.16–0.26 |
| Ependymal tumours | 16 | 90.5 | 0.36 | 0.30–0.43 | 28 | 58.4 | 0.30 | 0.26–0.34 | 42 | 50.5 | 0.44 | 0.40–0.49 | 17 | 50.5 | 0.41 | 0.34–0.49 |
| Glioma malignant, NOS c | 26 | 100.0 | 0.59 | 0.51–0.67 | 26 | 100.0 | 0.28 | 0.24–0.32 | 34 | 100.0 | 0.36 | 0.32–0.41 | 44 | 100.0 | 1.09 | 0.98–1.21 |
| Choroid plexus tumours | 5 | 19.4 | 0.11 | 0.08–0.15 | 2 | 7.7 | 0.02 | 0.01–0.03 | 3 | - | 0.03 | 0.02–0.05 | 1 | - | 0.02 | 0.01–0.05 |
| Neuronal & mixed neuronal-glial tumours | 16 | 3.4 | 0.37 | 0.31–0.43 | 38 | 7.9 | 0.42 | 0.37–0.47 | 21 | 41.7 | 0.23 | 0.19–0.26 | 8 | 41.7 | 0.19 | 0.14–0.24 |
| Tumours of the pineal region | 3 | 100.0 | 0.06 | 0.04–0.09 | 3 | 71.4 | 0.03 | 0.02–0.04 | 4 | 45.8 | 0.04 | 0.03–0.06 | 1 | 45.8 | 0.03 | 0.01–0.05 |
| Embryonal tumours | 36 | 99.0 | 0.82 | 0.73–0.92 | 13 | 97.1 | 0.14 | 0.11–0.17 | 6 | 92.1 | 0.06 | 0.04–0.08 | 2 | 92.1 | 0.04 | 0.02–0.07 |
| Other neuroepithelial tumours d | 1 * | 66.7 | - | - | 1 * | . | - | - | 1 * | - | - | - | 1 * | - | - | - |
| Tumours of cranial & spinal nerves | 8 | 5.9 | 0.18 | 0.14–0.23 | 88 | 1.6 | 0.96 | 0.89–1.03 | 237 | 0.6 | 2.50 | 2.39–2.62 | 99 | 0.6 | 2.43 | 2.26–2.60 |
| Tumours of meninges | 6 | 48.6 | 0.13 | 0.10–0.18 | 126 | 3.7 | 1.37 | 1.28–1.46 | 724 | 2.7 | 7.61 | 7.41–7.80 | 663 | 2.7 | 16.32 | 15.88–16.77 |
| Meningioma | 3 | 12.5 | 0.06 | 0.04–0.09 | 103 | 2.1 | 1.11 | 1.04–1.19 | 675 | 2.1 | 7.09 | 6.90–7.28 | 642 | 2.1 | 15.81 | 15.38–16.25 |
| Mesenchymal tumours | 2 | 83.3 | 0.04 | 0.02–0.07 | 4 | 47.6 | 0.05 | 0.03–0.06 | 16 | 29.3 | 0.17 | 0.14–0.20 | 8 | 29.3 | 0.17 | 0.13–0.22 |
| Primary melanocytic lesions d | 1 | 100.0 | 0.02 | 0.01–0.04 | 1 | 40.0 | 0.01 | 0.00–0.02 | 2 * | 58.3 | 0.02 | 0.01–0.03 | 2 * | 58.3 | - | - |
| Other neoplasms related to the meninges | 1 | 25.0 | 0.02 | 0.01–0.04 | 18 | 1.0 | 0.20 | 0.17–0.23 | 31 | 4.5 | 0.33 | 0.29–0.37 | 14 | 4.5 | 0.33 | 0.27–0.40 |
| Lymphomas & hematopoietic neoplasms | 1 | 100.0 | 0.02 | 0.01–0.04 | 7 | 100.0 | 0.08 | 0.06–0.10 | 49 | 99.8 | 0.52 | 0.47–0.57 | 73 | 99.8 | 1.78 | 1.64–1.93 |
| Lymphoma | 1 | 100.0 | 0.01 | 0.00–0.03 | 6 | 100.0 | 0.07 | 0.05–0.09 | 48 | 100.0 | 0.51 | 0.46–0.56 | 71 | 100.0 | 1.76 | 1.62–1.91 |
| Other hematopoietic neoplasms d | 1 * | - | - | - | 1 * | - | - | - | 1 | 91.7 | 0.01 | 0.01–0.02 | 1 | 91.7 | 0.02 | 0.01–0.04 |
| Germ cell tumours, cysts, & heterotopias | 12 | 72.7 | 0.26 | 0.21–0.32 | 13 | 68.3 | 0.15 | 0.12–0.18 | 3 | 14.3 | 0.03 | 0.02–0.05 | 1 | 14.3 | 0.02 | 0.01–0.04 |
| Tumours of sellar region | 13 | 3.4 | 0.27 | 0.22–0.33 | 153 | 0.2 | 1.67 | 1.58–1.77 | 327 | 0.4 | 3.44 | 3.31–3.58 | 198 | 0.4 | 4.84 | 4.60–5.09 |
| Unclassified tumours | 33 | - | 0.73 | 0.65–0.83 | 126 | - | 1.38 | 1.29–1.47 | 314 | - | 3.30 | 3.17–3.43 | 648 | - | 16.02 | 15.59–16.46 |
| Total | 237 | 67.1 | 5.30 | 5.06–5.54 | 823 | 34.2 | 9.00 | 8.78–9.22 | 2464 | 34.4 | 25.88 | 25.52–26.25 | 2363 | 34.4 | 58.16 | 57.33–58.99 |
| Age Group (Years) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 to 14 | 15 to 39 | 40 to 64 | 65+ | |||||||||
| Histology Group a (Major/Specific) | MST d | 5-Year SR e | 95% CI | MST d | 5-Year SR e | 95% CI | MST d | 5-Year SR e | 95% CI | MST d | 5-Year SR e | 95% CI |
| Tumours of neuroepithelial tissue | >120 | 72.4 | 69.9–75.0 | >120 | 67.6 | 65.5–69.8 | 15.8 | 21.1 | 20.0–22.2 | 4.9 | 3.7 | 3.2–4.3 |
| Pilocytic astrocytoma c | >120 | 98.9 | 97.9–100.0 | >120 | 93.2 | 89.5–97.0 | >120 | 88.0 | 80.3–96.4 | - | - | - |
| Diffuse astrocytoma | >120 | 72.7 | 63.5–83.3 | >120 | 74.4 | 68.7–80.6 | 27.9 | 33.1 | 28.3–38.7 | 4.9 | 3.8 | 1.9–7.8 |
| Anaplastic astrocytoma | 11.0 | 25.7 | 12.6–52.3 | 81.7 | 63.3 | 56.4–71.1 | 18.6 | 23.0 | 17.9–29.7 | 5.1 | 3.2 | 0.6–16.0 |
| Unique astrocytoma variants | >120 | 63.0 | 44.4–89.3 | >120 | 67.4 | 53.7–84.8 | 14.3 | 22.7 | 11.7–43.7 | 3.9 | 16.1 | 6.9–37.8 |
| Glioblastoma | 11.3 | 14.3 | 7.0–28.9 | 25.3 | 25.7 | 21.2–31.1 | 12.2 | 5.9 | 5.1–6.7 | 4.8 | 1.3 | 0.9–1.8 |
| Oligodendroglioma c | - | - | - | >120 | 88.5 | 84.0–93.4 | >120 | 75.8 | 71.0–80.9 | 14.1 | 30.5 | 19.2–48.4 |
| Anaplastic oligodendroglioma c | - | - | - | >120 | 73.1 | 65.0–82.2 | 64.5 | 52.2 | 46.3–58.8 | 11.2 | 14.8 | 8.7–25.2 |
| Oligoastrocytic tumours c | - | - | - | >120 | 76.3 | 70.7–82.4 | 51.1 | 44.8 | 39.4–51.0 | 9.1 | 7.6 | 3.4–17.0 |
| Ependymal tumours | >120 | 79.2 | 71.7–87.3 | >120 | 87.5 | 81.5–94.1 | >120 | 81.2 | 75.1–87.9 | 108.9 | 56.9 | 46.5–69.7 |
| Glioma malignant, NOS b | >120 | 59.1 | 53.1–65.8 | >120 | 71.7 | 65.8–78.0 | 29.3 | 35.3 | 29.8–41.7 | 3.2 | 6.3 | 4.2–9.4 |
| Choroid plexus tumours c | - | - | - | - | - | - | - | - | - | - | - | - |
| Neuronal & mixed neuronal-glial tumours c | - | - | - | >120 | 86.0 | 72.3–100.0 | >120 | 57.0 | 45.6–71.2 | 20.7 | 31.8 | 18.0–56.1 |
| Tumours of the pineal region c | 44.5 | 48.4 | 30.3–77.2 | - | - | - | - | - | - | - | - | - |
| Embryonal tumours c | >120 | 68.0 | 62.8–73.5 | >120 | 65.6 | 56.9–75.6 | 68.7 | 57.3 | 42.7–76.7 | - | - | - |
| Other neuroepithelial tumours c | - | - | - | - | - | - | - | - | - | - | - | - |
| Tumours of cranial & spinal nerves c | - | - | - | - | - | - | - | - | - | - | - | - |
| Tumours of meninges | 44.6 | 41.3 | 25.5–66.9 | >120 | 67.9 | 56.4–81.8 | 81.4 | 51.8 | 44.0–61.0 | 34.7 | 41.8 | 33.7–51.8 |
| Meningioma c | - | - | - | >120 | 69.9 | 53.4–91.4 | >120 | 55.3 | 45.3–67.5 | 35.2 | 40.3 | 31.3–52.0 |
| Mesenchymal tumours c | - | - | - | >120 | 70.4 | 52.7–93.9 | >120 | 51.4 | 37.3–70.7 | 28.5 | 44.1 | 25–77.8 |
| Primary melanocytic lesions c | - | - | - | - | - | - | - | - | - | - | - | - |
| Other neoplasms related to the meninges c | - | - | - | - | - | - | 64.6 | 52.1 | 32.3–84.2 | - | - | - |
| Lymphomas & hematopoietic neoplasms c | - | - | - | >120 | 57.2 | 45.5–71.9 | 46.3 | 44.4 | 39.4–50.0 | 5.1 | 16.1 | 13.0–19.8 |
| Lymphoma c | - | - | - | >120 | 58.2 | 46.3–73.2 | 46.3 | 44.4 | 39.3–50.1 | 5.1 | 16.1 | 13.1–19.9 |
| Other hematopoietic neoplasms c | - | - | - | - | - | - | - | - | - | - | - | - |
| Germ cell tumours, cysts, & heterotopias c | >120 | 88.7 | 82.0–96.0 | >120 | 90.2 | 83.9–96.9 | - | - | - | - | - | - |
| Tumours of sellar region c | - | - | - | - | - | - | - | - | - | - | - | - |
| Unclassified tumours | >120 | 76.8 | 64.5–91.4 | >120 | 73.6 | 65.0–83.3 | 37.5 | 47.9 | 42.7–53.8 | 1.9 | 6.4 | 5.1–8.1 |
| Total | >120 | 72.9 | 70.5–75.3 | >120 | 68.4 | 66.5–70.4 | 16.6 | 24.3 | 23.3–25.4 | 4.4 | 5.9 | 5.4–6.6 |
| Age Group (Years) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 to 14 | 15 to 39 | 40 to 64 | 65+ | |||||||||
| Histology Group a (Major/Specific) | MST d | 5-Year SR e | 95% CI | MST d | 5-Year SR e | 95% CI | MST d | 5-Year SR e | 95% CI | MST d | 5-Year SR e | 95% CI |
| Tumours of neuroepithelial tissue | >120 | 96.6 | 93.9–99.3 | >120 | 95.1 | 92.7–97.5 | >120 | 89.8 | 85.9–93.8 | >120 | 71.4 | 61.3–83.2 |
| Pilocytic astrocytoma | ||||||||||||
| Diffuse astrocytoma | ||||||||||||
| Anaplastic astrocytoma | ||||||||||||
| Unique astrocytoma variants c | >120 | 95.0 | 85.9–100.0 | >120 | 100 | 100.0–100.0 | - | - | - | - | - | - |
| Glioblastoma | ||||||||||||
| Oligodendroglioma | ||||||||||||
| Anaplastic oligodendroglioma | ||||||||||||
| Oligoastrocytic tumours | ||||||||||||
| Ependymal tumours c | - | - | - | >120 | 95.8 | 91.1–100.0 | >120 | 93.2 | 88.8–97.7 | >120 | 75.6 | 64.6–88.5 |
| Glioma malignant, NOS b | ||||||||||||
| Choroid plexus tumours c | >120 | 100 | 100.0–100.0 | - | - | - | >120 | 96.3 | 89.4–100.0 | - | - | |
| Neuronal & mixed neuronal-glial tumours | >120 | 96.8 | 93.7–99.9 | >120 | 94.3 | 91.3–97.4 | 113.2 | 82.3 | 74.2–91.2 | 75.5 | 57.1 | 36.9–88.5 |
| Tumours of the pineal region | - | - | - | - | - | - | - | - | - | - | - | - |
| Embryonal tumours | - | - | - | - | - | - | - | - | - | - | - | - |
| Other neuroepithelial tumours | - | - | - | - | - | - | - | - | - | - | - | - |
| Tumours of cranial & spinal nerves | >120 | 100 | 100.0–100.0 | >120 | 98.5 | 97.4–99.7 | >120 | 96.9 | 95.9–97.8 | >120 | 83.2 | 80.2–86.3 |
| Tumours of meninges | >120 | 100 | 100.0–100.0 | >120 | 97.1 | 95.8–98.3 | >120 | 90.8 | 89.9–91.7 | 92.6 | 62.1 | 60.6–63.7 |
| Meningioma | >120 | 100 | 100.0–100.0 | >120 | 97.5 | 96.3–98.8 | >120 | 90.9 | 90.0–91.8 | 90.8 | 61.7 | 60.1–63.3 |
| Mesenchymal tumours c | - | - | - | - | - | - | >120 | 89.4 | 82.1–97.4 | 98.4 | 74.3 | 60.8–90.7 |
| Primary melanocytic lesions c | - | - | - | - | - | - | - | - | - | - | - | - |
| Other neoplasms related to the meninges c | - | - | - | >120 | 96.2 | 92.4–100.0 | >120 | 90.3 | 85.8–95.0 | >120 | 81.4 | 73.2–90.6 |
| Lymphomas & hematopoietic neoplasms | - | - | - | - | - | - | - | - | - | - | - | - |
| Lymphoma | ||||||||||||
| Other hematopoietic neoplasms | - | - | - | - | - | - | - | - | - | - | - | - |
| Germ cell tumours, cysts, & heterotopias c | >120 | 95.7 | 87.7–100.0 | >120 | 100.0 | 100.0–100.0 | >120 | 94.7 | 85.2–100.0 | - | - | - |
| Tumours of sellar region | >120 | 93.7 | 88.4–99.3 | >120 | 98.8 | 98.1–99.5 | >120 | 94.7 | 93.7–95.7 | >120 | 76.0 | 73.5–78.5 |
| Unclassified tumours | >120 | 95.6 | 92.8–98.6 | >120 | 93.3 | 91.4–95.2 | >120 | 73.8 | 71.7–75.9 | 31.0 | 37.4 | 35.6–39.4 |
| Total | >120 | 96.3 | 94.7–97.9 | >120 | 96.9 | 96.3–97.5 | >120 | 89.8 | 89.2–90.4 | 82.6 | 57.9 | 56.9–59.0 |
| Age Group (Years) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 to 14 | 15 to 39 | 40 to 64 | 65+ | |||||||||
| Histology Group a (Major/Specific) | N | PP | 95% CI | N | PP | 95% CI | N | PP | 95% CI | N | PP | 95% CI |
| Tumours of neuroepithelial tissue | 650 | 14.1 | 13.0–15.2 | 1355 | 14.3 | 13.5–15.1 | 2065 | 21.4 | 20.5–22.4 | 765 | 16.3 | 15.2–17.5 |
| Pilocytic astrocytoma | 215 | 4.7 | 4.1–5.3 | 225 | 2.4 | 2.1–2.7 | 70 | 0.7 | 0.6–0.9 | 5 | 0.1 | 0.03–0.3 |
| Diffuse astrocytoma | 35 | 0.8 | 0.5–1.1 | 175 | 1.8 | 1.6–2.1 | 170 | 1.8 | 1.5–2.1 | 30 | 0.6 | 0.4–0.9 |
| Anaplastic astrocytoma | 5 | 0.1 | 0.04–0.3 | 105 | 1.1 | 0.9–1.3 | 125 | 1.3 | 1.1–1.5 | 35 | 0.8 | 0.5–1.0 |
| Unique astrocytoma variants b | 35 * | - | - | 35 * | 0.3 | 0.2–0.5 | 10 | 0.1 | 0.05–0.2 | 5 | 0.1 | 0.03–0.3 |
| Glioblastoma | 15 | 0.3 | 0.2–0.5 | 145 | 1.5 | 1.3–1.8 | 780 | 8.1 | 7.5–8.7 | 470 | 10.0 | 9.1–11.0 |
| Oligodendroglioma b | 155 * | - | - | 155 * | 1.6 | 1.4–1.9 | 250 | 2.6 | 2.3–2.9 | 30 | 0.6 | 0.4–0.9 |
| Anaplastic oligodendroglioma | 0 | - | - | 60 | 0.6 | 0.5–0.8 | 170 | 1.8 | 1.5–2.1 | 30 | 0.6 | 0.4–0.9 |
| Oligoastrocytic tumours b | 95 * | - | - | 95 * | 1.0 | 0.8–1.2 | 135 | 1.4 | 1.2–1.7 | 20 | 0.4 | 0.3–0.7 |
| Ependymal tumours | 80 | 1.7 | 1.4–2.2 | 80 | 0.8 | 0.7–1.1 | 135 | 1.4 | 1.2–1.7 | 60 | 1.3 | 1.0–1.7 |
| Glioma malignant, NOS b | 100 | 2.2 | 1.8–2.6 | 130 | 1.4 | 1.1–1.6 | 140 | 1.5 | 1.2–1.7 | 50 | 1.1 | 0.8–1.4 |
| Choroid plexus tumours | 5 | 0.1 | 0.04–0.3 | 0 | - | - | 0 | - | - | 0 | - | - |
| Neuronal & mixed neuronal-glial tumours c | 25 * | - | - | 25 * | 0.2 | 0.1–0.3 | 35 | 0.4 | 0.3–0.5 | 20 | 0.4 | 0.3–0.7 |
| Tumours of the pineal region c | 10 | 0.2 | 0.1–0.4 | 15 | 0.2 | 0.09–0.3 | 10 * | 0.1 | 0.05–0.2 | 10 * | - | - |
| Embryonal tumours c | 175 | 3.8 | 3.3–4.4 | 105 | 1.1 | 0.9–1.3 | 25 * | 0.3 | 0.2–0.4 | 25 * | - | - |
| Other neuroepithelial tumours d | 10 ** | - | - | 10 ** | - | - | 10 ** | - | - | 10 ** | - | - |
| Tumours of cranial & spinal nerves | 0 | - | - | 10 | 0.05 | 0.02–0.1 | 5 | 0.05 | 0.02–0.1 | 5 | 0.1 | 0.03–0.3 |
| Tumours of meninges | 5 | 0.1 | 0.04–0.3 | 20 | 0.2 | 0.1–0.3 | 65 | 0.7 | 0.5–0.9 | 55 | 1.2 | 0.9–1.5 |
| Meningioma c | 10 * | - | - | 10 * | 0.1 | 0.05–0.2 | 40 | 0.4 | 0.3–0.6 | 45 | 1.0 | 0.7–1.3 |
| Mesenchymal tumours c | 10 * | - | - | 10 * | 0.1 | 0.05–0.2 | 20 | 0.2 | 0.1–0.3 | 5 | 0.1 | 0.03–0.3 |
| Primary melanocytic lesions d | 10 ** | - | - | 10 ** | - | - | 10 ** | - | - | 10 ** | - | - |
| Other neoplasms related to the meninges c | 10 * | - | - | 10 * | - | - | 10 * | 0.05 | 0.02–0.1 | 10 * | - | - |
| Lymphomas & hematopoietic neoplasmsc | 30 * | - | - | 30 * | 0.3 | 0.2–0.5 | 155 | 1.6 | 1.4–1.9 | 175 | 3.7 | 3.2–4.3 |
| Lymphoma c | 25 * | - | - | 25 * | 0.3 | 0.2–0.4 | 150 | 1.6 | 1.3–1.8 | 175 | 3.7 | 3.2–4.3 |
| Other hematopoietic neoplasms c | 10 * | - | - | 10 * | - | - | 10 * | - | - | 10 * | - | - |
| Germ cell tumours, cysts, & heterotopias | 30 | 0.7 | 0.4–0.9 | 90 | 1.0 | 0.8–1.2 | 10 | 0.1 | 0.05–0.2 | 0 | - | - |
| Tumours of sellar region c | 10 * | - | - | 10 * | - | - | 10 * | - | - | 5 | 0.1 | 0.03–0.3 |
| Unclassified tumours | 15 | 0.3 | 0.2–0.5 | 25 | 0.3 | 0.2–0.4 | 75 | 0.8 | 0.6–1.0 | 60 | 1.3 | 1.0–1.7 |
| Total | 700 | 15.1 | 14.0–16.3 | 1525 | 16.1 | 15.3–16.9 | 2375 | 24.6 | 23.7–25.6 | 1060 | 22.6 | 21.3–24.0 |
| Age Group (years) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 to 14 | 15 to 39 | 40 to 64 | 65+ | |||||||||
| Histology Group a (Major/Specific) | N | PP | 95% CI | N | PP | 95% CI | N | PP | 95% CI | N | PP | 95% CI |
| Tumours of neuroepithelial tissue | 120 | 2.6 | 2.2–3.1 | 430 | 4.5 | 4.1–5.0 | 310 | 3.2 | 2.9–3.6 | 95 | 2.0 | 1.6–2.5 |
| Pilocytic astrocytoma | ||||||||||||
| Diffuse astrocytoma | ||||||||||||
| Anaplastic astrocytoma | ||||||||||||
| Unique astrocytoma variants d | 15 | 0.3 | 0.2–0.5 | 30 | 0.3 | 0.2–0.5 | 5 * | - | - | 5 * | - | - |
| Glioblastoma | ||||||||||||
| Oligodendroglioma | ||||||||||||
| Anaplastic oligodendroglioma | ||||||||||||
| Oligoastrocytic tumours | ||||||||||||
| Ependymal tumours | 5 | 0.1 | 0.04–0.3 | 85 | 0.9 | 0.7–1.1 | 155 | 1.6 | 1.4–1.9 | 60 | 1.3 | 1.0–1.7 |
| Glioma malignant, NOS b | ||||||||||||
| Choroid plexus tumours | 25 | 0.5 | 0.4–0.5 | 20 | 0.2 | 0.1–0.3 | 25 | 0.3 | 0.2–0.4 | 10 | 0.2 | 0.1–0.4 |
| Neuronal & mixed neuronal-glial tumours | 75 | 1.6 | 1.3–2.0 | 280 | 3.0 | 2.6–3.3 | 115 | 1.2 | 1.0–1.4 | 25 | 0.5 | 0.3–0.8 |
| Tumours of the pineal region | 10 * | - | - | 10 * | 0.1 | 0.05–0.2 | 15 * | 0.1 | 0.05–0.2 | 15 * | - | - |
| Embryonal tumours c | 10 * | - | - | 10 * | - | - | 10 * | - | - | 0 | - | - |
| Other neuroepithelial tumours d | 10 ** | - | - | 10 ** | 0.05 | 0.02–0.1 | 10 ** | - | - | 10 ** | - | - |
| Tumours of cranial & spinal nerves | 40 | 0.9 | 0.6–1.2 | 445 | 4.7 | 4.3–5.1 | 1630 | 16.9 | 16.1–17.8 | 940 | 20.0 | 18.8–21.4 |
| Tumours of meninges | 15 | 0.3 | 0.2–0.5 | 610 | 6.4 | 5.9–7.0 | 4435 | 46.0 | 44.7–47.4 | 4265 | 90.9 | 88.2–93.7 |
| Meningioma | 10 | 0.2 | 0.1–0.4 | 490 | 5.2 | 4.7–5.6 | 4140 | 42.9 | 41.6–44.3 | 4115 | 87.7 | 85.1–90.4 |
| Mesenchymal tumours c | 10 * | - | - | 10 * | 0.1 | 0.05–0.2 | 60 | 0.6 | 0.5–0.8 | 40 | 0.9 | 0.6–1.2 |
| Primary melanocytic lesions d | 10 ** | - | - | 10 ** | - | - | 10 ** | 0.05 | 0.02–0.1 | 10 ** | - | - |
| Other neoplasms related to the meninges c | 105 * | - | - | 105 * | 1.1 | 0.9–1.3 | 225 | 2.3 | 2.0–2.7 | 110 | 2.3 | 1.9–2.8 |
| Lymphomas & hematopoietic neoplasms | 0 | - | - | 0 | - | - | 0 | - | - | 0 | - | - |
| Lymphoma | ||||||||||||
| Other hematopoietic neoplasms | 0 | - | - | 0 | - | - | 0 | - | - | 0 | - | - |
| Germ cell tumours, cysts, & heterotopias | 20 | 0.4 | 0.3–0.7 | 25 | 0.3 | 0.2–0.4 | 20 | 0.2 | 0.1–0.3 | 10 | 0.2 | 0.1–0.4 |
| Tumours of sellar region | 50 | 1.1 | 0.8–1.4 | 970 | 10.2 | 9.6–10.9 | 2335 | 24.2 | 23.3–25.2 | 1655 | 35.3 | 33.6–37.0 |
| Unclassified tumours | 165 | 3.6 | 3.1–4.2 | 795 | 8.4 | 7.8–9.0 | 1615 | 16.8 | 15.9–17.6 | 2080 | 44.3 | 42.5–46.3 |
| Total | 410 | 8.9 | 8.0–9.8 | 3275 | 34.5 | 33.3–35.7 | 10,340 | 107.3 | 105.2–109.3 | 9050 | 192.9 | 188.9–196.9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Walker, E.V.; Zhou, Y.; Wu, Y.; Liu, J.; Climans, S.A.; Davis, F.G.; Yuan, Y. The Incidence and Prevalence of Primary Central Nervous System (CNS) Tumours in Canada (2010–2017), and the Survival of Patients Diagnosed with CNS Tumours (2008–2017). Curr. Oncol. 2023, 30, 4311-4328. https://doi.org/10.3390/curroncol30040329
Walker EV, Zhou Y, Wu Y, Liu J, Climans SA, Davis FG, Yuan Y. The Incidence and Prevalence of Primary Central Nervous System (CNS) Tumours in Canada (2010–2017), and the Survival of Patients Diagnosed with CNS Tumours (2008–2017). Current Oncology. 2023; 30(4):4311-4328. https://doi.org/10.3390/curroncol30040329
Chicago/Turabian StyleWalker, Emily V., Yiling Zhou, Yifan Wu, Jiaqi Liu, Seth A. Climans, Faith G. Davis, and Yan Yuan. 2023. "The Incidence and Prevalence of Primary Central Nervous System (CNS) Tumours in Canada (2010–2017), and the Survival of Patients Diagnosed with CNS Tumours (2008–2017)" Current Oncology 30, no. 4: 4311-4328. https://doi.org/10.3390/curroncol30040329
APA StyleWalker, E. V., Zhou, Y., Wu, Y., Liu, J., Climans, S. A., Davis, F. G., & Yuan, Y. (2023). The Incidence and Prevalence of Primary Central Nervous System (CNS) Tumours in Canada (2010–2017), and the Survival of Patients Diagnosed with CNS Tumours (2008–2017). Current Oncology, 30(4), 4311-4328. https://doi.org/10.3390/curroncol30040329





