Factors Associated with Early Discharge after Non-Emergent Right Colectomy for Colon Cancer: A NSQIP Analysis
Abstract
1. Introduction
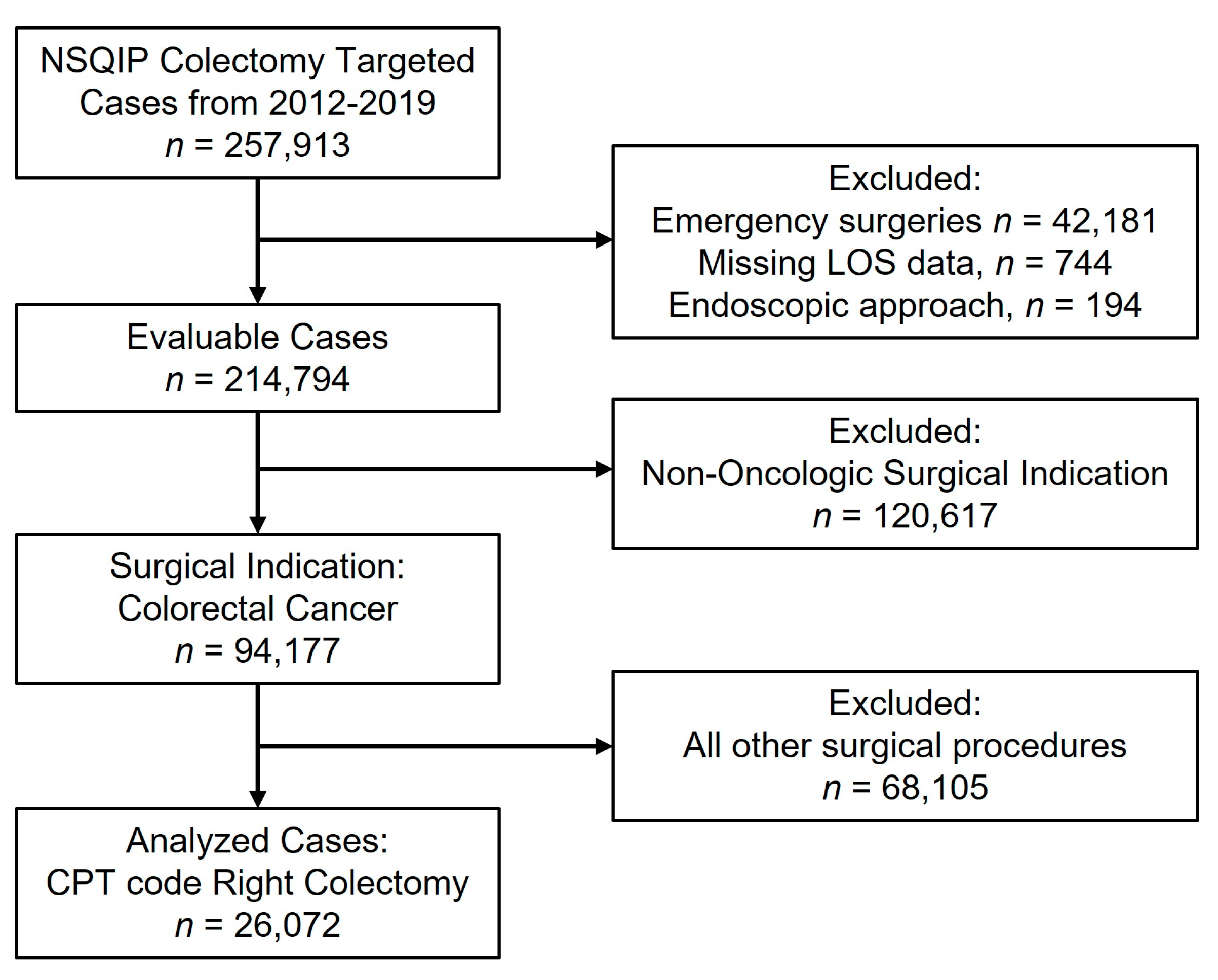
2. Materials and Methods
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gustafsson, U.O.; Scott, M.J.; Schwenk, W.; Demartines, N.; Roulin, D.; Francis, N.; McNaught, C.E.; MacFie, J.; Liberman, A.S.; Soop, M.; et al. Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Clin. Nutr. 2012, 31, 783–800. [Google Scholar] [CrossRef] [PubMed]
- Ljungqvist, O.; Scott, M.; Fearon, K.C. Enhanced Recovery After Surgery: A Review. JAMA Surg. 2017, 152, 292–298. [Google Scholar] [CrossRef] [PubMed]
- Sarin, A.; Litonius, E.S.; Naidu, R.; Yost, C.S.; Varma, M.G.; Chen, L.L. Successful implementation of an Enhanced Recovery After Surgery program shortens length of stay and improves postoperative pain, and bowel and bladder function after colorectal surgery. BMC Anesthesiol. 2016, 16, 55. [Google Scholar] [CrossRef] [PubMed]
- Stephen, A.E.; Berger, D.L. Shortened length of stay and hospital cost reduction with implementation of an accelerated clinical care pathway after elective colon resection. Surgery 2003, 133, 277–282. [Google Scholar] [CrossRef] [PubMed]
- van Vugt, J.L.; Reisinger, K.W.; Derikx, J.P.; Boerma, D.; Stoot, J.H. Improving the outcomes in oncological colorectal surgery. World J. Gastroenterol. 2014, 20, 12445–12457. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, R.L.; Bartlett, E.K.; Ko, C.; Mahmoud, N.; Karakousis, G.C.; Kelz, R.R. Early discharge and readmission after colorectal resection. J. Surg. Res. 2014, 190, 579–586. [Google Scholar] [CrossRef] [PubMed]
- Marcus, R.K.; Lillemoe, H.A.; Rice, D.C.; Mena, G.; Bednarski, B.K.; Speer, B.B.; Ramirez, P.T.; Lasala, J.D.; Navai, N.; Williams, W.H.; et al. Determining the Safety and Efficacy of Enhanced Recovery Protocols in Major Oncologic Surgery: An Institutional NSQIP Analysis. Ann. Surg. Oncol. 2019, 26, 782–790. [Google Scholar] [CrossRef] [PubMed]
- Turrentine, F.E.; McMurry, T.L.; Adams, R.B.; Jones, R.S.; Zaydfudim, V.M. Early Patient Discharge in Selected Patients is Not Associated with Higher Readmission After Major Abdominal Operations. Ann. Surg. 2020, 276, e698–e705. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, J.K.; Keller, D.S.; Samia, H.; Ermlich, B.; Brady, K.M.; Nobel, T.; Stein, S.L.; Delaney, C.P. Discharge within 24 to 72 hours of colorectal surgery is associated with low readmission rates when using Enhanced Recovery Pathways. J. Am. Coll. Surg. 2013, 216, 390–394. [Google Scholar] [CrossRef] [PubMed]
- Levy, B.F.; Scott, M.J.; Fawcett, W.J.; Rockall, T.A. 23-hour-stay laparoscopic colectomy. Dis. Colon Rectum 2009, 52, 1239–1243. [Google Scholar] [CrossRef] [PubMed]
- Saadat, L.V.; Mahvi, D.A.; Jolissaint, J.S.; Gabriel, R.A.; Urman, R.; Gold, J.S.; Whang, E.E. Twenty-Three-Hour-Stay Colectomy Without Increased Readmissions: An Analysis of 1905 Cases from the National Surgical Quality Improvement Program. World J. Surg. 2020, 44, 947–956. [Google Scholar] [CrossRef] [PubMed]
- Watson, M.; Gower, N.; Sierra, B.; Salo, J.C.; Hill, J.S. Enhanced Recovery for Colectomy and Discharge One Day after Operation: How Low Can We Go? J. Am. Coll. Surg. 2018, 227, e106. [Google Scholar] [CrossRef]
- Hendren, S.; Morris, A.M.; Zhang, W.; Dimick, J. Early discharge and hospital readmission after colectomy for cancer. Dis. Colon Rectum 2011, 54, 1362–1367. [Google Scholar] [CrossRef] [PubMed]
- Hassan, I.; Pacheco, P.E.; Markwell, S.J.; Ahad, S. Additional procedures performed during elective colon surgery and their adverse impact on postoperative outcomes. J. Gastrointest. Surg. 2015, 19, 527–534. [Google Scholar] [CrossRef] [PubMed]
- American College of Surgeons National Surgical Quality Improvement Program. Available online: https://www.Facs.Org/quality-programs/acs-nsqip (accessed on 30 November 2022).
- Francis, N.K.; Mason, J.; Salib, E.; Allanby, L.; Messenger, D.; Allison, A.S.; Smart, N.J.; Ockrim, J.B. Factors predicting 30-day readmission after laparoscopic colorectal cancer surgery within an enhanced recovery programme. Color. Dis. 2015, 17, O148–O154. [Google Scholar] [CrossRef] [PubMed]
- Kulaylat, A.N.; Dillon, P.W.; Hollenbeak, C.S.; Stewart, D.B. Determinants of 30-d readmission after colectomy. J. Surg. Res. 2015, 193, 528–535. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Talwar, A.; Chatterjee, S.; Aparasu, R.R. Application of machine learning in predicting hospital readmissions: A scoping review of the literature. BMC Med. Res. Methodol. 2021, 21, 96. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Stansbury, C.; Singh, K.; Ryan, A.M.; Sukul, D.; Mahmoudi, E.; Waljee, A.; Zhu, J.; Nallamothu, B.K. Predicting 30-day hospital readmissions using artificial neural networks with medical code embedding. PLoS ONE 2020, 15, e0221606. [Google Scholar] [CrossRef] [PubMed]
- Xue, B.; Li, D.; Lu, C.; King, C.R.; Wildes, T.; Avidan, M.S.; Kannampallil, T.; Abraham, J. Use of Machine Learning to Develop and Evaluate Models Using Preoperative and Intraoperative Data to Identify Risks of Postoperative Complications. JAMA Netw. Open 2021, 4, e212240. [Google Scholar] [CrossRef] [PubMed]
- Brom, H.; Carthon, J.M.B.; Ikeaba, U.; Chittams, J. Leveraging Electronic Health Records and Machine Learning to Tailor Nursing Care for Patients at High Risk for Readmissions. J. Nurs. Care Qual. 2020, 35, 27–33. [Google Scholar] [CrossRef] [PubMed]
| Factor | Total | Early | Standard | Late | |
|---|---|---|---|---|---|
| N = 26,072 | Discharge | Discharge | Discharge | ||
| N = 3684 | N = 13,414 | N = 8974 | |||
| Age, mean (SD), years | 69.1 (12.9) | 65.3 (11.9) | 68.3 (12.8) | 71.8 (12.8) | |
| Sex | Female | 13,874 (53.2%) | 1899 (13.7%) | 7422 (53.5%) | 4553 (32.8%) |
| Male | 12,198 (46.8%) | 1785 (14.6%) | 5992 (49.1%) | 4421 (36.2%) | |
| Race | Black | 2839 (10.9%) | 359 (12.6%) | 1421 (50.1%) | 1059 (37.3%) |
| Other | 750 (2.9%) | 119 (15.9%) | 396 (52.8%) | 235 (31.3%) | |
| Unknown | 4306 (16.5%) | 487 (11.3%) | 2226 (51.7%) | 1593 (37.0%) | |
| White | 18,177 (69.7%) | 2719 (15.0%) | 9371 (51.6%) | 6087 (33.5%) | |
| Current Smoker | No | 22,895 (87.8%) | 3270 (14.3%) | 11,832 (51.7%) | 7793 (34.0%) |
| Yes | 3177 (12.2%) | 414 (13.0%) | 1582 (49.8%) | 1181 (37.2%) | |
| Diabetes | No | 20,753 (79.6%) | 3079 (14.8%) | 10,663 (51.4%) | 7011 (33.8%) |
| Yes | 5319 (20.4%) | 605 (11.4%) | 2751 (51.7%) | 1963 (36.9%) | |
| Dyspnea | No | 23,188 (88.9%) | 3434 (14.8%) | 12,058 (52.0%) | 7696 (33.2%) |
| At Rest | 142 (0.5%) | 9 (6.3%) | 58 (40.8%) | 75 (52.8%) | |
| Moderate Exertion | 2742 (10.5%) | 241 (8.8%) | 1298 (47.3%) | 1203 (43.9%) | |
| History of Severe COPD | No | 24,474 (93.9%) | 3572 (14.6%) | 12,718 (52.0%) | 8184 (33.4%) |
| Yes | 1598 (6.1%) | 112 (7.0%) | 696 (43.6%) | 790 (49.4%) | |
| CHF (30 Days Before Surgery) | No | 25,647 (98.4%) | 3659 (14.3%) | 13,254 (51.7%) | 8734 (34.1%) |
| Yes | 425 (1.6%) | 25 (5.9%) | 160 (37.6%) | 240 (56.5%) | |
| Hypertension Requiring Medication | No | 10,957 (42.0%) | 1767 (16.1%) | 5825 (53.2%) | 3365 (30.7%) |
| Yes | 15,115 (58.0%) | 1917 (12.7%) | 7589 (50.2%) | 5609 (37.1%) | |
| Ascites | No | 25,889 (99.3%) | 3680 (14.2%) | 13,372 (51.7%) | 8837 (34.1%) |
| Yes | 183 (0.7%) | 4 (2.2%) | 42 (23.0%) | 137 (74.9%) | |
| Currently on Dialysis (Pre-operative) | No | 25,895 (99.3%) | 3674 (14.2%) | 13,343 (51.5%) | 8878 (34.3%) |
| Yes | 177 (0.7%) | 10 (5.6%) | 71 (40.1%) | 96 (54.2%) | |
| T Stage | T0 or Tis | 530 (2.0%) | 118 (22.3%) | 292 (55.1%) | 120 (22.6%) |
| T1 | 2388 (9.2%) | 446 (18.7%) | 1339 (56.1%) | 603 (25.3%) | |
| T2 | 3809 (14.6%) | 659 (17.3%) | 2065 (54.2%) | 1085 (28.5%) | |
| T3 | 12,360 (47.4%) | 1669 (13.5%) | 6437 (52.1%) | 4254 (34.4%) | |
| T4 | 4728 (18.1%) | 430 (9.1%) | 2180 (46.1%) | 2118 (44.8%) | |
| Tx, N/A, Unknown | 2257 (8.7%) | 362 (16.0%) | 1101 (48.8%) | 794 (35.2%) | |
| N Stage | N0 | 13,795 (52.9%) | 2071 (15.0%) | 7257 (52.6%) | 4467 (32.4%) |
| N1 | 6454 (24.8%) | 857 (13.3%) | 3314 (51.3%) | 2283 (35.4%) | |
| N2 | 3472 (13.3%) | 385 (11.1%) | 1705 (49.1%) | 1382 (39.8%) | |
| Nx, N/A, Unknown | 2351 (9.0%) | 371 (15.8%) | 1138 (48.4%) | 842 (35.8%) | |
| M Stage | M0 or Mx | 13,313 (51.1%) | 2085 (15.7%) | 6909 (51.9%) | 4319 (32.4%) |
| M1 | 1780 (6.8%) | 119 (6.7%) | 781 (43.9%) | 880 (49.4%) | |
| N/A, Unknown | 10,979 (42.1%) | 1480 (13.5%) | 5724 (52.1%) | 3775 (34.4%) | |
| Disseminated Cancer | No | 23,397 (89.7%) | 3495 (14.9%) | 12,266 (52.4%) | 7636 (32.6%) |
| Yes | 2675 (10.3%) | 189 (7.1%) | 1148 (42.9%) | 1338 (50.0%) | |
| Pre-Operative Weight Loss (>10% in Last 6 Months) | No | 24,618 (94.4%) | 3581 (14.5%) | 12,793 (52.0%) | 8244 (33.5%) |
| Yes | 1454 (5.6%) | 103 (7.1%) | 621 (42.7%) | 730 (50.2%) | |
| Bleeding Disorders | No | 25,030 (96.0%) | 3617 (14.5%) | 12,969 (51.8%) | 8444 (33.7%) |
| Yes | 1042 (4.0%) | 67 (6.4%) | 445 (42.7%) | 530 (50.9%) | |
| Pre-Operative Sepsis | No | 25,435 (97.6%) | 3672 (14.4%) | 13,241 (52.1%) | 8522 (33.5%) |
| Yes | 637 (2.4%) | 12 (1.9%) | 173 (27.2%) | 452 (71.0%) | |
| Steroid Use for Chronic Conditions | No | 25,084 (96.2%) | 3579 (14.3%) | 12,960 (51.7%) | 8545 (34.1%) |
| Yes | 988 (3.8%) | 105 (10.6%) | 454 (46.0%) | 429 (43.4%) | |
| Functional Health | Independent | 25,166 (96.5%) | 3647 (14.5%) | 13,115 (52.1%) | 8404 (33.4%) |
| Status Prior to Surgery | Partially Dependent | 719 (2.8%) | 29 (4.0%) | 230 (32.0%) | 460 (64.0%) |
| Totally Dependent | 91 (0.3%) | 0 (0.0%) | 25 (27.5%) | 66 (72.5%) | |
| Unknown | 96 (0.4%) | 8 (8.3%) | 44 (45.8%) | 44 (45.8%) | |
| Year of Operation | 2012 | 1411 (5.4%) | 40 (2.8%) | 729 (51.7%) | 642 (45.5%) |
| 2013 | 1530 (5.9%) | 68 (4.4%) | 810 (52.9%) | 652 (42.6%) | |
| 2014 | 2357 (9.0%) | 184 (7.8%) | 1233 (52.3%) | 940 (39.9%) | |
| 2015 | 3066 (11.8%) | 313 (10.2%) | 1565 (51.0%) | 1188 (38.7%) | |
| 2016 | 3716 (14.3%) | 497 (13.4%) | 1893 (50.9%) | 1326 (35.7%) | |
| 2017 | 3993 (15.3%) | 629 (15.8%) | 2077 (52.0%) | 1287 (32.2%) | |
| 2018 | 4581 (17.6%) | 858 (18.7%) | 2314 (50.5%) | 1409 (30.8%) | |
| 2019 | 5418 (20.8%) | 1095 (20.2%) | 2793 (51.6%) | 1530 (28.2%) | |
| Surgery Approach | MIS | 10,645 (40.8%) | 2270 (21.3%) | 6040 (56.7%) | 2335 (21.9%) |
| MIS Converted Open | 1883 (7.2%) | 80 (4.2%) | 833 (44.2%) | 970 (51.5%) | |
| MIS with Open | 6907 (26.5%) | 1167 (16.9%) | 3948 (57.2%) | 1792 (25.9%) | |
| Assist | |||||
| Open | 6637 (25.5%) | 167 (2.5%) | 2593 (39.1%) | 3877 (58.4%) | |
| Any Additional Procedure | No | 16,898 (64.8%) | 2824 (16.7%) | 9169 (54.3%) | 4905 (29.0%) |
| Yes | 9174 (35.2%) | 860 (9.4%) | 4245 (46.3%) | 4069 (44.4%) | |
| Urgent Surgery | No | 21,138 (81.1%) | 3489 (16.5%) | 11,579 (54.8%) | 6070 (28.7%) |
| Yes | 4934 (18.9%) | 195 (4.0%) | 1835 (37.2%) | 2904 (58.9%) | |
| Ureteral Stent | No | 25,436 (97.6%) | 3655 (14.4%) | 13,125 (51.6%) | 8656 (34.0%) |
| Yes | 636 (2.4%) | 29 (4.6%) | 289 (45.4%) | 318 (50.0%) | |
| Enterolysis | No | 24,110 (92.5%) | 3488 (14.5%) | 12,518 (51.9%) | 8104 (33.6%) |
| Yes | 1962 (7.5%) | 196 (10.0%) | 896 (45.7%) | 870 (44.3%) | |
| Ileostomy | No | 25,787 (98.9%) | 3676 (14.3%) | 13,357 (51.8%) | 8754 (33.9%) |
| Yes | 285 (1.1%) | 8 (2.8%) | 57 (20.0%) | 220 (77.2%) | |
| Bowel Resection | No | 25,535 (97.9%) | 3670 (14.4%) | 13,231 (51.8%) | 8634 (33.8%) |
| Yes | 537 (2.1%) | 14 (2.6%) | 183 (34.1%) | 340 (63.3%) | |
| Cholecystectomy | No | 25,611 (98.2%) | 3652 (14.3%) | 13,212 (51.6%) | 8747 (34.2%) |
| Yes | 461 (1.8%) | 32 (6.9%) | 202 (43.8%) | 227 (49.2%) | |
| Abscess Requiring | No | 26,050 (99.9%) | 3684 (14.1%) | 13,411 (51.5%) | 8955 (34.4%) |
| Drainage | Yes | 22 (0.1%) | 0 (0.0%) | 3 (13.6%) | 19 (86.4%) |
| Total Abdominal Hysterectomy | No | 25,983 (99.7%) | 3679 (14.2%) | 13,375 (51.5%) | 8929 (34.4%) |
| Yes | 89 (0.3%) | 5 (5.6%) | 39 (43.8%) | 45 (50.6%) | |
| Ureterolysis | No | 26,028 (99.8%) | 3682 (14.1%) | 13,398 (51.5%) | 8948 (34.4%) |
| Yes | 44 (0.2%) | 2 (4.5%) | 16 (36.4%) | 26 (59.1%) | |
| Hepatectomy | No | 25,861 (99.2%) | 3678 (14.2%) | 13,344 (51.6%) | 8839 (34.2%) |
| Yes | 211 (0.8%) | 6 (2.8%) | 70 (33.2%) | 135 (64.0%) | |
| Sum RVUs Remaining Additional Procedures, Mean (SD) | 4.0 (11.0) | 1.6 (5.2) | 2.9 (8.2) | 6.6 (15.2) | |
| Wound Infection | No | 25,836 (99.1%) | 3677 (14.2%) | 13,333 (51.6%) | 8826 (34.2%) |
| Yes | 236 (0.9%) | 7 (3.0%) | 81 (34.3%) | 148 (62.7%) | |
| Wound Class | Clean/ | 23,928 (91.8%) | 3520 (14.7%) | 12,563 (52.5%) | 7845 (32.8%) |
| Contaminated | |||||
| Contaminated | 1575 (6.0%) | 138 (8.8%) | 687 (43.6%) | 750 (47.6%) | |
| Dirty/Infected | 569 (2.2%) | 26 (4.6%) | 164 (28.8%) | 379 (66.6%) | |
| Anastomotic Leak | No | 25,373 (97.3%) | 3637 (14.3%) | 13,229 (52.1%) | 8507 (33.5%) |
| Yes | 643 (2.5%) | 43 (6.7%) | 153 (23.8%) | 447 (69.5%) | |
| Unknown | 56 (0.2%) | 4 (7.1%) | 32 (57.1%) | 20 (35.7%) | |
| Deep Incisional Surgical Site Infection | No | 25,924 (99.4%) | 3675 (14.2%) | 13,377 (51.6%) | 8872 (34.2%) |
| Yes | 148 (0.6%) | 9 (6.1%) | 37 (25.0%) | 102 (68.9%) | |
| Organ Space Surgical Site Infection | No | 25,159 (96.5%) | 3635 (14.4%) | 13,193 (52.4%) | 8331 (33.1%) |
| Yes | 913 (3.5%) | 49 (5.4%) | 221 (24.2%) | 643 (70.4%) | |
| Pneumonia | No | 25,543 (98.0%) | 3676 (14.4%) | 13,352 (52.3%) | 8515 (33.3%) |
| Yes | 529 (2.0%) | 8 (1.5%) | 62 (11.7%) | 459 (86.8%) | |
| Urinary Tract Infection | No | 25,639 (98.3%) | 3662 (14.3%) | 13,284 (51.8%) | 8693 (33.9%) |
| Yes | 433 (1.7%) | 22 (5.1%) | 130 (30.0%) | 281 (64.9%) | |
| DVT/ Thrombophlebitis | No | 25,744 (98.7%) | 3668 (14.2%) | 13,317 (51.7%) | 8759 (34.0%) |
| Yes | 328 (1.3%) | 16 (4.9%) | 97 (29.6%) | 215 (65.5%) |
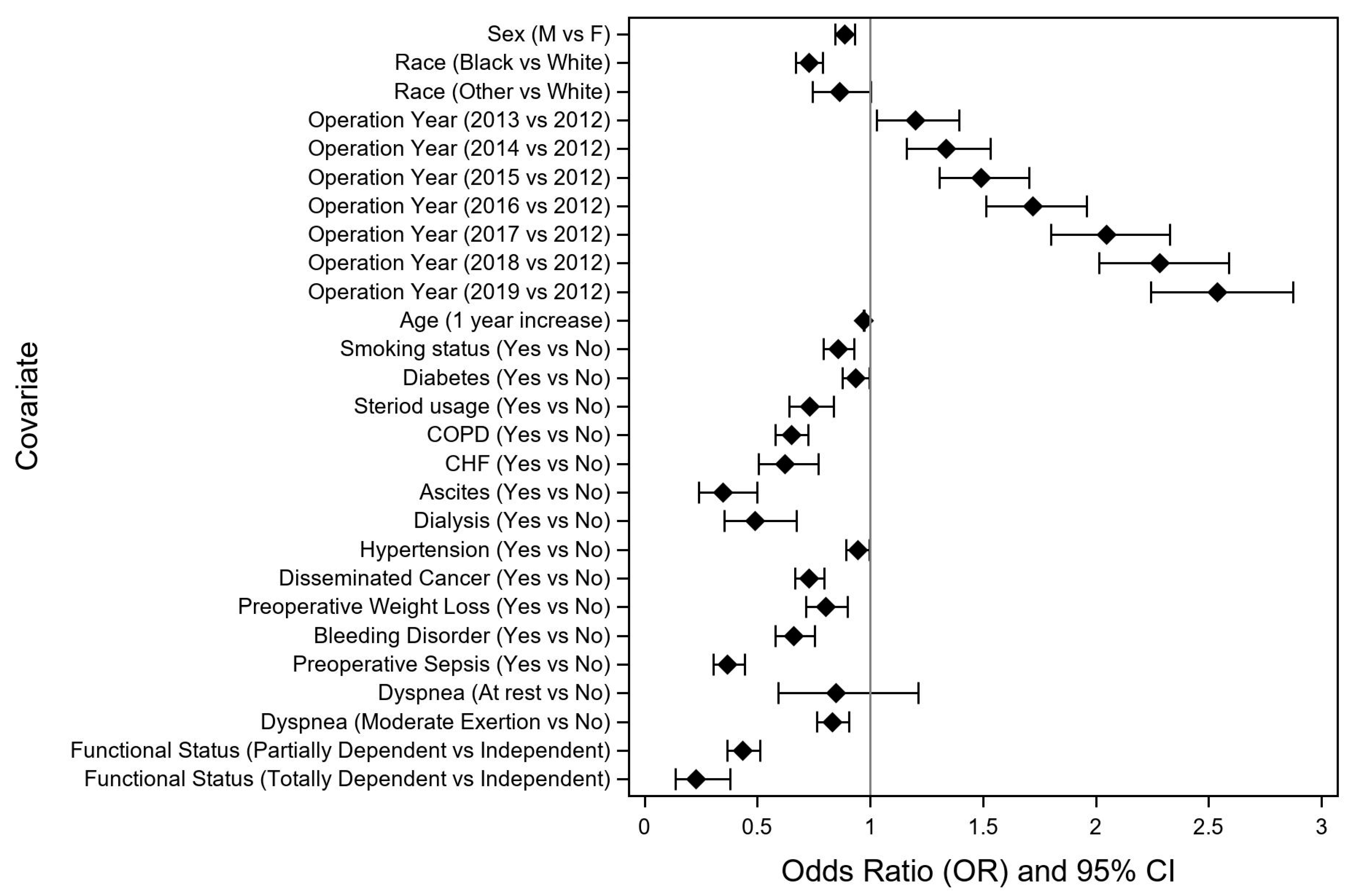
| Factor | Odds Ratio | 95% CI | p Value | |
|---|---|---|---|---|
| Age, 1-year increase | 0.972 | 0.970, 0.974 | <0.0001 | |
| Sex | Male vs. Female | 0.887 | 0.843, 0.932 | <0.0001 |
| Race | Black vs. White | 0.728 | 0.671, 0.791 | <0.0001 |
| Other vs. White | 0.864 | 0.746, 1.002 | 0.0534 | |
| Unknown/Not Reported vs. White | 0.664 | 0.620, 0.712 | <0.0001 | |
| Smoking status | Yes vs. No | 0.859 | 0.794, 0.928 | 0.0001 |
| Diabetes | Yes vs. No | 0.934 | 0.877, 0.996 | 0.0367 |
| Dyspnea | At Rest vs. No | 0.847 | 0.592, 1.213 | 0.3661 |
| Moderate Exertion vs. No | 0.831 | 0.763, 0.906 | <0.0001 | |
| History of Severe COPD | Yes vs. No | 0.650 | 0.581, 0.727 | <0.0001 |
| CHF (30 Days Before Surgery) | Yes vs. No | 0.623 | 0.505, 0.769 | <0.0001 |
| Ascites | Yes vs. No | 0.346 | 0.239, 0.499 | <0.0001 |
| Currently on Dialysis (Pre-Operative) | Yes vs. No | 0.489 | 0.355, 0.673 | <0.0001 |
| Disseminated Cancer | Yes vs. No | 0.729 | 0.667, 0.797 | <0.0001 |
| Pre-Operative Weight Loss (>10% in Last 6 Months) | Yes vs. No | 0.802 | 0.716, 0.898 | 0.0001 |
| Bleeding Disorder | Yes vs. No | 0.661 | 0.580, 0.754 | <0.0001 |
| Pre-Operative Sepsis | Yes vs. No | 0.368 | 0.304, 0.446 | <0.0001 |
| Steroid | Yes vs. No | 0.733 | 0.643, 0.837 | <0.0001 |
| Functional Status | Partially Dependent vs. Independent | 0.434 | 0.366, 0.513 | <0.0001 |
| Totally Dependent vs. Independent | 0.228 | 0.136, 0.380 | <0.0001 | |
| Unknown vs. Independent | 0.761 | 0.502, 1.153 | 0.1973 | |
| Year of Operation | 2013 vs. 2012 | 1.199 | 1.031, 1.396 | 0.0188 |
| 2014 vs. 2012 | 1.335 | 1.162, 1.533 | <0.0001 | |
| 2015 vs. 2012 | 1.493 | 1.308, 1.704 | <0.0001 | |
| 2016 vs. 2012 | 1.722 | 1.513, 1.958 | <0.0001 | |
| 2017 vs. 2012 | 2.048 | 1.802, 2.327 | <0.0001 | |
| 2018 vs. 2012 | 2.283 | 2.013, 2.589 | <0.0001 | |
| 2019 vs. 2012 | 2.538 | 2.242, 2.873 | <0.0001 | |
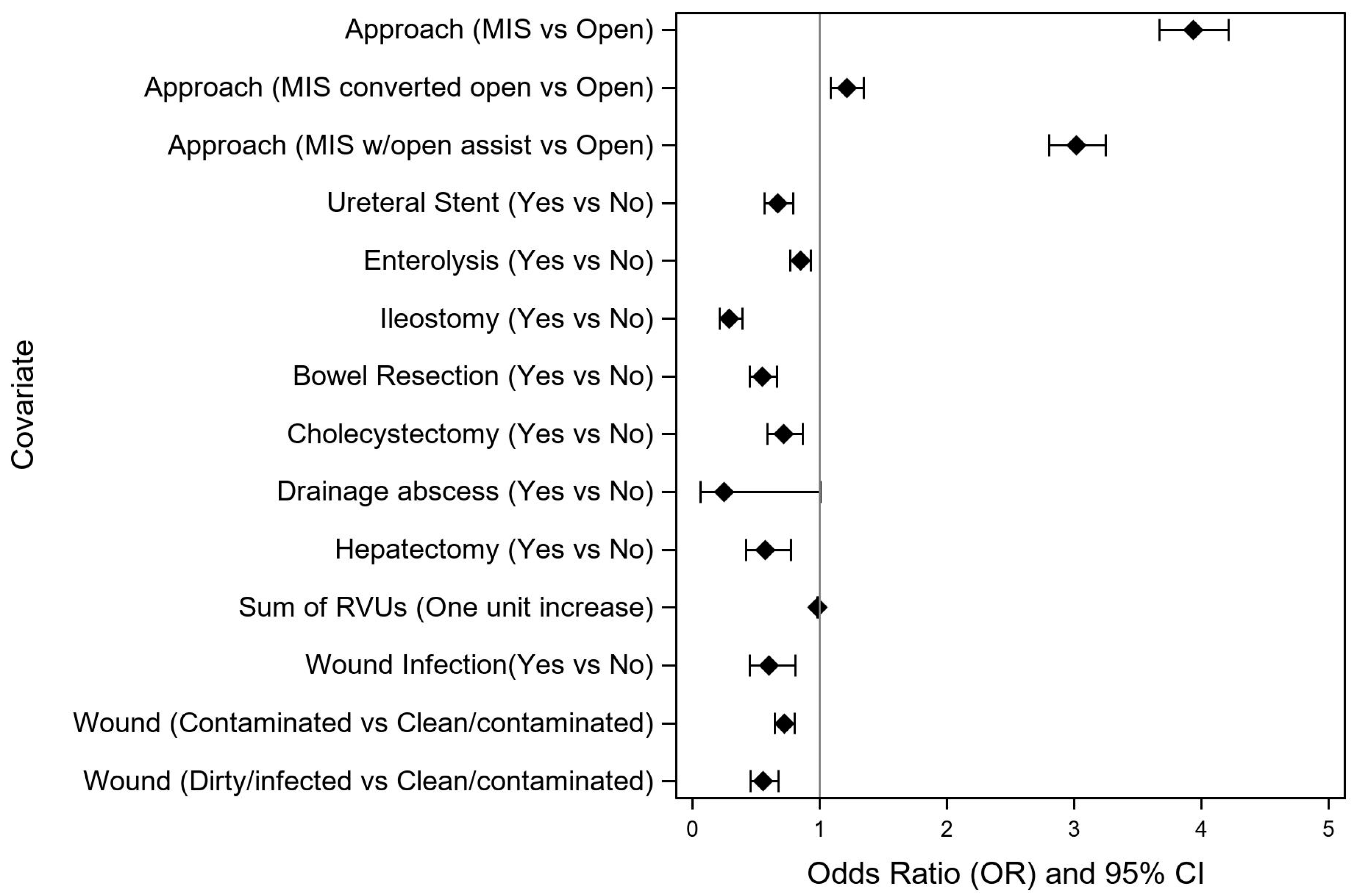
| Surgery Approach | MIS vs. Open | 3.934 | 3.672, 4.214 | <0.0001 |
| MIS converted open vs. Open | 1.209 | 1.087, 1.345 | 0.0005 | |
| MIS with open assist vs. Open | 3.016 | 2.802, 3.247 | <0.0001 | |
| Ureteral Stent | Yes vs. No | 0.669 | 0.566, 0.791 | <0.0001 |
| Enterolysis | Yes vs. No | 0.845 | 0.768, 0.930 | 0.0006 |
| Ileostomy | Yes vs. No | 0.286 | 0.211, 0.388 | <0.0001 |
| Bowel Resection | Yes vs. No | 0.545 | 0.449, 0.661 | <0.0001 |
| Cholecystectomy | Yes vs No | 0.714 | 0.587, 0.867 | 0.0007 |
| Drainage Abscess | Yes vs. No | 0.247 | 0.061, 1.005 | 0.0509 |
| Hepatectomy | Yes vs. No | 0.569 | 0.417, 0.775 | 0.0004 |
| Sum Remaining RVUs additional procedures (one unit increase) | 0.982 | 0.979, 0.985 | <0.0001 | |
| Wound Infection | Yes vs. No | 0.601 | 0.448, 0.808 | 0.0007 |
| Wound Class | Contaminated vs. Clean/Contaminated | 0.719 | 0.646, 0.800 | <0.0001 |
| Dirty/Infected vs. Clean/Contaminated | 0.553 | 0.454, 0.674 | <0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Squires, M.H.; Donahue, E.E.; Wallander, M.L.; Trufan, S.J.; Shea, R.E.; Lindholm, N.F.; Hill, J.S.; Salo, J.C. Factors Associated with Early Discharge after Non-Emergent Right Colectomy for Colon Cancer: A NSQIP Analysis. Curr. Oncol. 2023, 30, 2482-2492. https://doi.org/10.3390/curroncol30020189
Squires MH, Donahue EE, Wallander ML, Trufan SJ, Shea RE, Lindholm NF, Hill JS, Salo JC. Factors Associated with Early Discharge after Non-Emergent Right Colectomy for Colon Cancer: A NSQIP Analysis. Current Oncology. 2023; 30(2):2482-2492. https://doi.org/10.3390/curroncol30020189
Chicago/Turabian StyleSquires, Malcolm H., Erin E. Donahue, Michelle L. Wallander, Sally J. Trufan, Reilly E. Shea, Nicole F. Lindholm, Joshua S. Hill, and Jonathan C. Salo. 2023. "Factors Associated with Early Discharge after Non-Emergent Right Colectomy for Colon Cancer: A NSQIP Analysis" Current Oncology 30, no. 2: 2482-2492. https://doi.org/10.3390/curroncol30020189
APA StyleSquires, M. H., Donahue, E. E., Wallander, M. L., Trufan, S. J., Shea, R. E., Lindholm, N. F., Hill, J. S., & Salo, J. C. (2023). Factors Associated with Early Discharge after Non-Emergent Right Colectomy for Colon Cancer: A NSQIP Analysis. Current Oncology, 30(2), 2482-2492. https://doi.org/10.3390/curroncol30020189





