“Well, to Be Honest, I Don’t Have an Idea of What It Might Be”—A Qualitative Study on Knowledge and Awareness Regarding Nonmelanoma Skin Cancer
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
2.3. Data Analysis
3. Results
3.1. Knowledge about NMSC
3.1.1. Familiarity with the Term NMSC and Definitions
3.1.2. Knowledge about Early Signs of NMSC
3.1.3. Risk Factors for NMSC
3.1.4. Perception of Own Knowledge about and Desire for More Information on NMSC
3.2. Awareness Regarding NMSC
3.2.1. Estimated Prevalence of NMSC
3.2.2. Perceived Dangerousness of NMSC
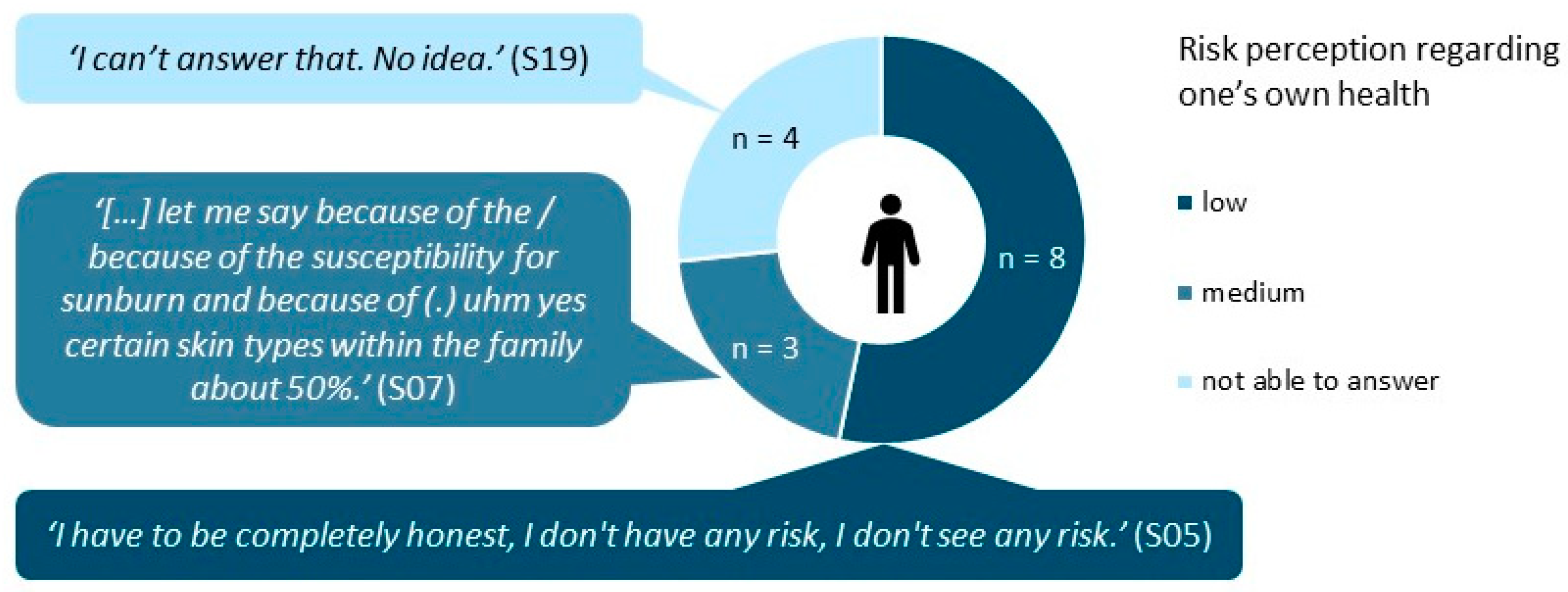
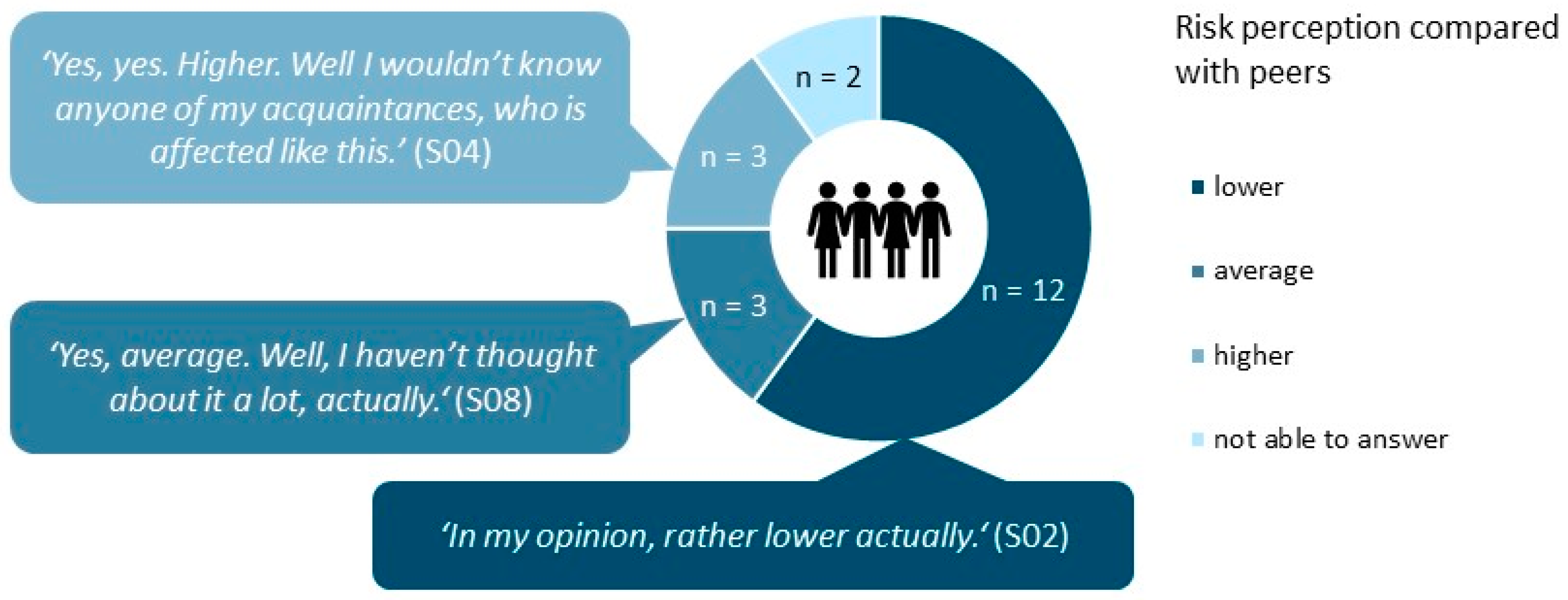
3.2.3. Perception of Risk of NMSC
4. Discussion
4.1. Knowledge about NMSC
4.2. Risk Perception of NMSC
4.3. Desire for More Information on NMSC
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zink, A. Nichtmelanozytärer Hautkrebs: Pathogenese, Prävalenz und Prävention. Der Hautarzt 2017, 68, 919–928. [Google Scholar] [CrossRef] [PubMed]
- Lomas, A.; Leonardi-Bee, J.; Bath-Hextall, F. A systematic review of worldwide incidence of nonmelanoma skin cancer. Br. J. Dermatol. 2012, 166, 1069–1080. [Google Scholar] [CrossRef] [PubMed]
- Linares, M.A.; Zakaria, A.; Nizran, P. Skin Cancer. Prim. Care Clin. Off. Pract. 2015, 42, 645–659. [Google Scholar] [CrossRef] [PubMed]
- Griffin, L.L.; Ali, F.R.; Lear, J.T. Non-melanoma skin cancer. Clin. Med. 2016, 16, 62–65. [Google Scholar] [CrossRef]
- Hu, W.; Fang, L.; Ni, R.; Zhang, H.; Pan, G. Changing trends in the disease burden of non-melanoma skin cancer globally from 1990 to 2019 and its predicted level in 25 years. BMC Cancer 2022, 22, 836. [Google Scholar] [CrossRef] [PubMed]
- American Cancer Society. Cancer Facts & Figures 2022; American Cancer Society: Atlanta, GA, USA, 2022. [Google Scholar]
- Madan, V.; Lear, J.T.; Szeimies, R.-M. Non-melanoma skin cancer. Lancet 2010, 375, 673–685. [Google Scholar] [CrossRef] [PubMed]
- Guy, G.P.; Machlin, S.R.; Ekwueme, D.U.; Yabroff, K.R. Prevalence and Costs of Skin Cancer Treatment in the U.S., 2002−2006 and 2007−2011. Am. J. Prev. Med. 2015, 48, 183–187. [Google Scholar] [CrossRef] [PubMed]
- Gordon, L.; Olsen, C.; Whiteman, D.C.; Elliott, T.M.; Janda, M.; Green, A. Prevention versus early detection for long-term control of melanoma and keratinocyte carcinomas: A cost-effectiveness modelling study. BMJ Open 2020, 10, e034388. [Google Scholar] [CrossRef] [PubMed]
- Day, A.K.; Wilson, C.J.; Hutchinson, A.D.; Roberts, R.M. The role of skin cancer knowledge in sun-related behaviours: A systematic review. J. Health Psychol. 2013, 19, 1143–1162. [Google Scholar] [CrossRef] [PubMed]
- Friman, M.; Huck, J.; Olsson, L.E. Transtheoretical Model of Change during Travel Behavior Interventions: An Integrative Review. Int. J. Environ. Res. Public Health 2017, 14, 581. [Google Scholar] [CrossRef] [PubMed]
- Brewer, N.T.; Chapman, G.B.; Gibbons, F.X.; Gerrard, M.; McCaul, K.D.; Weinstein, N.D. Meta-analysis of the relationship between risk perception and health behavior: The example of vaccination. Health Psychol. 2007, 26, 136–145. [Google Scholar] [CrossRef]
- Schwarzer, R. Modeling Health Behavior Change: How to Predict and Modify the Adoption and Maintenance of Health Behaviors. Appl. Psychol. 2008, 57, 1–29. [Google Scholar] [CrossRef]
- Bränström, R.; Kristjansson, S.; Ullén, H. Risk perception, optimistic bias, and readiness to change sun related behaviour. Eur. J. Public Health 2005, 16, 492–497. [Google Scholar] [CrossRef] [PubMed]
- Seité, S.; del Marmol, V.; Moyal, D.; Friedman, A.J. Public primary and secondary skin cancer prevention, perceptions and knowledge: An international cross-sectional survey. J. Eur. Acad. Dermatol. Venereol. 2017, 31, 815–820. [Google Scholar] [CrossRef] [PubMed]
- Halpern, A.C.; Kopp, L.J. Awareness, knowledge and attitudes to non-melanoma skin cancer and actinic keratosis among the general public. Int. J. Dermatol. 2005, 44, 107–111. [Google Scholar] [CrossRef] [PubMed]
- MacKie, R. Awareness, knowledge and attitudes to basal cell carcinoma and actinic keratoses among the general public within Europe. J. Eur. Acad. Dermatol. Venereol. 2004, 18, 552–555. [Google Scholar] [CrossRef]
- Zink, A.; Schielein, M.; Wildner, M.; Rehfuess, E.A. ‘Try to make good hay in the shade-It won’t work!’. A qualitative interview study on the perspectives of Bavarian farmers regarding primary prevention of skin cancer. Br. J. Dermatol. 2019, 180, 1412–1419. [Google Scholar] [CrossRef]
- Rattay, P.; Michalski, N.; Domanska, O.M.; Kaltwasser, A.; De Bock, F.; Wieler, L.H.; Jordan, S. Differences in risk perception, knowledge and protective behaviour regarding COVID-19 by education level among women and men in Germany. Results from the COVID-19 Snapshot Monitoring (COSMO) study. PLoS ONE 2021, 16, e0251694. [Google Scholar] [CrossRef]
- Diehl, K.; Görig, T.; Osenbrügge, N.; Schilling, L.; Greinert, R.; Schneider, S. Optimistically biased perception of one’s own skin cancer risk: Representative nationwide findings. J. Dtsch. Dermatol. Ges. 2019, 17, 786–798. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Helfferich, C. Interviewplanung und Intervieworganisation. In Die Qualität Qualitativer Daten: Manual für Die Durchführung Qualitativer Interviews; VS Verlag für Sozialwissenschaften: Wiesbaden, Germany, 2009; pp. 167–193. [Google Scholar]
- Fitzpatrick, T. Soleil et peau. J. Med. Esthet. 1975, 2, 33–34. [Google Scholar]
- Kuckartz, U.; Dresing, T.; Rädiker, S.; Stefer, K. Qualitative Evaluation in sieben Schritten. In Qualitative Evaluation. der Einstieg in Die Praxis; VS Verlag für Sozialwissenschaften: Wiesbaden, Germany, 2008; Volume 2, pp. 15–57. [Google Scholar]
- Mayring, P. Qualitative Inhaltsanalyse. Handbuch qualitative Forschung in der Psychologie. In Handbuch Qualitative Forschung in der Psychologie; Mey, G., Mruck, K., Eds.; VS Verlag fur Sozialwissenschaften: Wiesbaden, Germany, 2010; pp. 601–613. [Google Scholar]
- Kuckartz, U.; Rädiker, S. Die Interviews codieren (“Basiscodierung”). In Fokussierte Interviewanalyse mit MAXQDA: Schritt für Schritt; Springer Fachmedien Wiesbaden: Wiesbaden, Germany, 2020; pp. 43–54. [Google Scholar]
- Arnold, A. Basalzellkarzinom und Plattenepithelkarzinom im Fokus. Hautnah Dermatol. 2016, 32, 44–50. [Google Scholar] [CrossRef]
- Connolly, K.L.; Nehal, K.S.; Disa, J.J. Evidence-Based Medicine: Cutaneous Facial Malignancies: Nonmelanoma Skin Cancer. Plast. Reconstr. Surg. 2017, 139, 181e–190e. [Google Scholar] [CrossRef] [PubMed]
- Mackiewicz-Wysocka, M.; Bowszyc-Dmochowska, M.; Strzelecka-Węklar, D.; Dańczak-Pazdrowska, A.; Adamski, Z. Basal cell carcinoma–diagnosis. Contemp. Oncol. 2013, 17, 337–342. [Google Scholar] [CrossRef]
- Sgouros, D.; Milia-Argyti, A.; Arvanitis, D.K.; Polychronaki, E.; Kousta, F.; Panagiotopoulos, A.; Theotokoglou, S.; Syrmali, A.; Theodoropoulos, K.; Stratigos, A.; et al. Actinic Keratoses (AK): An Exploratory Questionnaire-Based Study of Patients’ Illness Perceptions. Curr. Oncol. 2022, 29, 5150–5163. [Google Scholar] [CrossRef]
- Fernandez Figueras, M.T. From actinic keratosis to squamous cell carcinoma: Pathophysiology revisited. J. Eur. Acad. Dermatol. Venereol. 2017, 31, 5–7. [Google Scholar] [CrossRef]
- Miles, A.; Waller, J.; Hiom, S.; Swanston, D. SunSmart? Skin cancer knowledge and preventive behaviour in a British population representative sample. Health Educ. Res. 2005, 20, 579–585. [Google Scholar] [CrossRef]
- Castilho, I.G.; Sousa, M.A.A.; Leite, R.M.S. Fotoexposição e fatores de risco para câncer da pele: Uma avaliação de hábitos e conhecimentos entre estudantes universitários. An. Bras. Dermatol. 2010, 85, 173–178. [Google Scholar] [CrossRef]
- Börner, F.; Greinert, R.; Schütz, H.; Wiedemann, P. UV-Risikowahrnehmung in der Bevölkerung: Ergebnisse einer repräsentativen Umfrage in Deutschland. Gesundheitswesen 2010, 72, e89–e97. [Google Scholar] [CrossRef]
- Didona, D.; Paolino, G.; Bottoni, U.; Cantisani, C. Non Melanoma Skin Cancer Pathogenesis Overview. Biomedicines 2018, 6, 6. [Google Scholar] [CrossRef]
- Diepgen, T.L.; Mahler, V. The epidemiology of skin cancer. Br. J. Dermatol. 2002, 146, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Buster, K.J.; You, Z.; Fouad, M.; Elmets, C. Skin cancer risk perceptions: A comparison across ethnicity, age, education, gender, and income. J. Am. Acad. Dermatol. 2012, 66, 771–779. [Google Scholar] [CrossRef] [PubMed]
- Leiter, U.; Keim, U.; Eigentler, T.; Katalinic, A.; Holleczek, B.; Martus, P.; Garbe, C. Incidence, Mortality, and Trends of Nonmelanoma Skin Cancer in Germany. J. Investig. Dermatol. 2017, 137, 1860–1867. [Google Scholar] [CrossRef]
- Leiter, U.; Heppt, M.V.; Steeb, T.; Amaral, T.; Bauer, A.; Becker, J.C.; Breitbart, E.; Breuninger, H.; Diepgen, T.; Dirschka, T.; et al. S3-Leitlinie „Aktinische Keratose und Plattenepithelkarzinom der Haut”–Kurzfassung, Teil 2: Epidemiologie, chirurgische und systemische Therapie des Plattenepithelkarzinoms, Nachsorge, Prävention und Berufskrankheit. J. Dtsch. Dermatol. Ges. 2020, 18, 400–413. [Google Scholar] [CrossRef]
- Tversky, A.; Kahneman, D. Availability: A heuristic for judging frequency and probability. Cogn. Psychol. 1973, 5, 207–232. [Google Scholar] [CrossRef]
- Peters, E.; McCaul, K.D.; Stefanek, M.; Nelson, W. A Heuristics Approach to Understanding Cancer Risk Perception: Contributions From Judgment and Decision-Making Research. Ann. Behav. Med. 2006, 31, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Emerson, R.W. Convenience Sampling, Random Sampling, and Snowball Sampling: How Does Sampling Affect the Validity of Research? J. Vis. Impair. Blind. 2015, 109, 164–168. [Google Scholar] [CrossRef]
- Kirchherr, J.; Charles, K. Enhancing the sample diversity of snowball samples: Recommendations from a research project on anti-dam movements in Southeast Asia. PLoS ONE 2018, 13, e0201710. [Google Scholar] [CrossRef]
- Nidzvetska, S.; Rodriguez-Llanes, J.M.; Aujoulat, I.; Gil Cuesta, J.; Tappis, H.; Van Loenhout, J.A.F.; Guha-Sapir, D. Maternal and Child Health of Internally Displaced Persons in Ukraine: A Qualitative Study. Int. J. Environ. Res. Public Health 2017, 14, 54. [Google Scholar] [CrossRef]
- Roskin, J.; Aveyard, P. Canadian and English students’ beliefs about waterpipe smoking: A qualitative study. BMC Public Health 2009, 9, 10. [Google Scholar] [CrossRef]
- Potente, S.; McIver, J.; Anderson, C.; Coppa, K. “It’s a Beautiful Day for Cancer”: An Innovative Communication Strategy to Engage Youth in Skin Cancer Prevention. Soc. Mar. Q. 2011, 17, 86–105. [Google Scholar] [CrossRef]
- Roosta, N.; Wong, M.K.; Woodley, D.T. Utilizing hairdressers for early detection of head and neck melanoma: An untapped resource. J. Am. Acad. Dermatol. 2012, 66, 687–688. [Google Scholar] [CrossRef] [PubMed]
| ID | Age | Sex | Migration Background | Highest Education 1 | Retirement | Living Situation | Fitzpatrick Skin Type | Diagnosis of Skin Cancer 2 | NMSC in Social Environment |
|---|---|---|---|---|---|---|---|---|---|
| S01 | 73 | Female | No | Medium | Yes | Alone | III | No | No |
| S02 | 82 | Male | No | Low | Yes | Alone | II | No | No |
| S03 | 83 | Female | Yes | Low | Yes | With children | III | NMSC | Yes |
| S04 | 80 | Female | No | Low | Yes | With spouse | II | NMSC | Yes |
| S05 | 83 | Female | No | Low | Yes | With spouse | III | No | No |
| S06 | 85 | Male | No | High | Yes | With spouse | III | No | No |
| S07 | 54 | Male | No | High | No | With spouse | III | No | Yes |
| S08 | 57 | Female | No | High | Yes | With spouse | I | NMSC | No |
| S09 | 56 | Male | No | High | No | With spouse | II | MM | Yes |
| S10 | 58 | Female | Yes | High | No | With spouse | III | No | Yes |
| S11 | 77 | Male | Yes | Low | Yes | With spouse | II | AK, NMSC, MM | Yes |
| S12 | 85 | Female | No | Low | Yes | With spouse | III | No | No |
| S13 | 83 | Male | Yes | High | Yes | With spouse | II | NMSC | No |
| S14 | 63 | Male | No | High | No | Alone | III | AK | No |
| S15 | 55 | Male | No | Medium | No | Alone | II | No | Yes |
| S16 | 64 | Male | Yes | Other | No | Alone | III | No | No |
| S17 | 75 | Male | No | High | Yes | With spouse | III | No | No |
| S18 | 59 | Female | No | Low | No | With spouse | III | No | Yes |
| S19 | 61 | Female | No | Medium | No | With spouse | II | No | Yes |
| S20 | 65 | Female | No | Low | Yes | With spouse | III | No | No |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brokmeier, L.L.; Diehl, K.; Spähn, B.A.; Jansen, C.; Konkel, T.; Uter, W.; Görig, T. “Well, to Be Honest, I Don’t Have an Idea of What It Might Be”—A Qualitative Study on Knowledge and Awareness Regarding Nonmelanoma Skin Cancer. Curr. Oncol. 2023, 30, 2290-2299. https://doi.org/10.3390/curroncol30020177
Brokmeier LL, Diehl K, Spähn BA, Jansen C, Konkel T, Uter W, Görig T. “Well, to Be Honest, I Don’t Have an Idea of What It Might Be”—A Qualitative Study on Knowledge and Awareness Regarding Nonmelanoma Skin Cancer. Current Oncology. 2023; 30(2):2290-2299. https://doi.org/10.3390/curroncol30020177
Chicago/Turabian StyleBrokmeier, Luisa Leonie, Katharina Diehl, Bianca Annika Spähn, Charlotte Jansen, Tobias Konkel, Wolfgang Uter, and Tatiana Görig. 2023. "“Well, to Be Honest, I Don’t Have an Idea of What It Might Be”—A Qualitative Study on Knowledge and Awareness Regarding Nonmelanoma Skin Cancer" Current Oncology 30, no. 2: 2290-2299. https://doi.org/10.3390/curroncol30020177
APA StyleBrokmeier, L. L., Diehl, K., Spähn, B. A., Jansen, C., Konkel, T., Uter, W., & Görig, T. (2023). “Well, to Be Honest, I Don’t Have an Idea of What It Might Be”—A Qualitative Study on Knowledge and Awareness Regarding Nonmelanoma Skin Cancer. Current Oncology, 30(2), 2290-2299. https://doi.org/10.3390/curroncol30020177






