Management of Marginal Zone Lymphoma: A Canadian Perspective
Abstract
1. Introduction
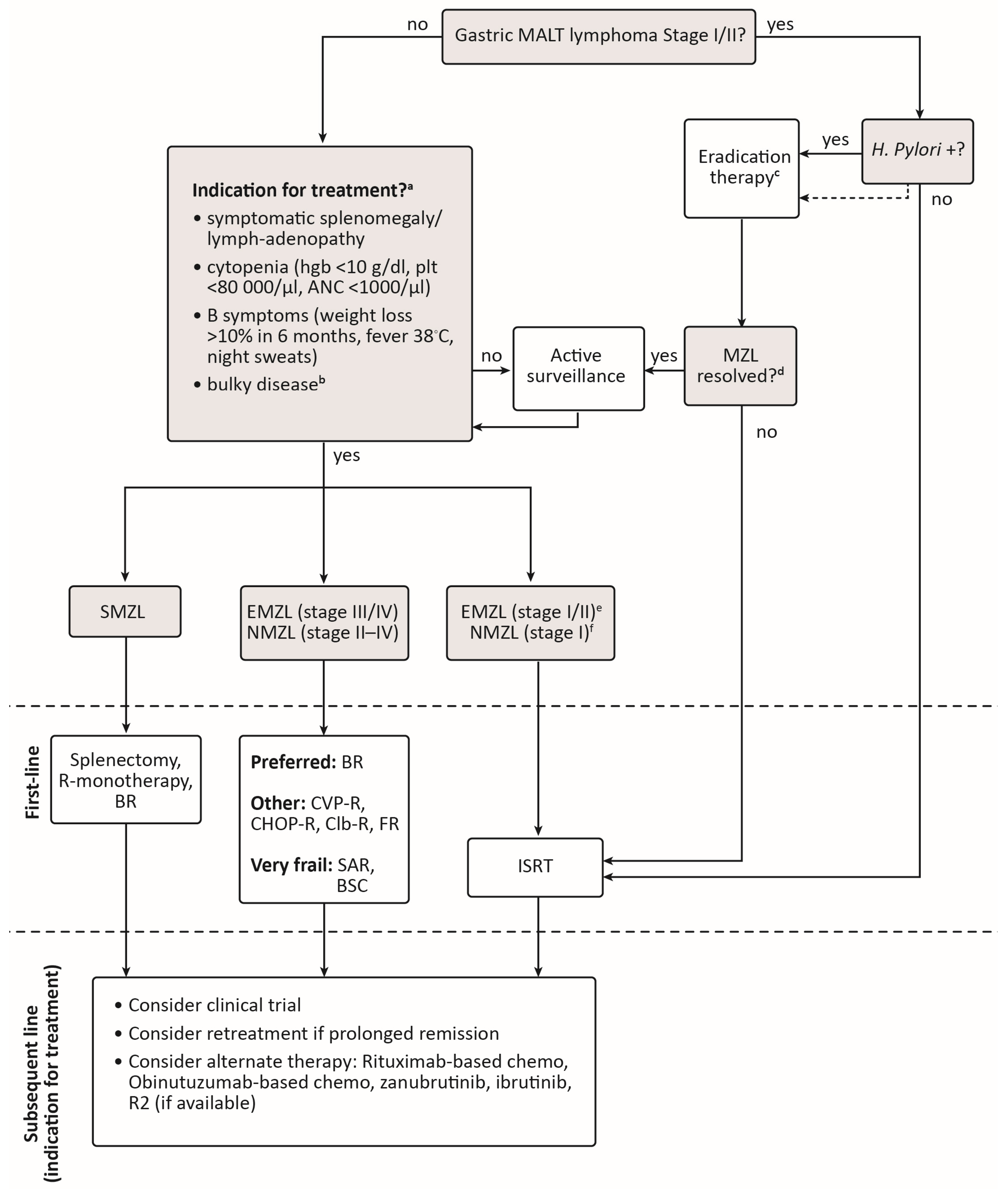
2. Clinical Characteristics of MZL Subtypes
3. Indications for Treatment
4. First-Line Treatment Options
4.1. Pathogen-Directed Therapy
4.2. Local Therapy
4.2.1. Involved-Site Radiation Therapy
4.2.2. Splenectomy
4.3. Systemic Therapy
4.3.1. Single-Agent Rituximab
4.3.2. Chemoimmunotherapy
4.3.3. Maintenance Rituximab
4.3.4. Lenalidomide-Rituximab
| Study Name/Regimen | Phase | Population | CR (%) | PFS | OS | ||
|---|---|---|---|---|---|---|---|
| Median/Landmark | HR (95% CI) | Median/Landmark | HR (95% CI) | ||||
| StiL NHL1 [66,67] BR vs. CHOP-R | 3 | Advanced iNHL or MCL N(ITT) = 514 N(MZL) = 67 | ITT: 40 vs. 30 p = 0.021 MZL: Not reported | Median(ITT): 69.5 vs. 31.2 months Median(MZL): 57.2 vs. 47.2 months | ITT: 0.58 (0.44–0.74) p < 0.0001 MZL: 0.70 (0.34–1.43) p = 0.3249 | 10-year(ITT): 71% vs. 66% 10-year(MZL): Not reported | ITT: 0.82 (0.58–1.15) p = 0.249 MZL: Not reported |
| BRIGHT [65,79] BR vs. CHOP-R or CVP-R | 3 | Advanced iNHL or MCL N(ITT) = 447 N(MZL) = 46 | ITT: 31 vs. 25 p = 0.0225 * MZL: 20 vs. 24 | 5-year(ITT): 66% vs. 56% Median(MZL): Not reported | ITT: 0.61 (0.45–0.85) p = 0.0025 MZL: Not reported | 5-year(ITT): 82% vs. 85% 5-year(MZL): Not reported | ITT: 1.15 (0.72–1.84) p = 0.5461 MZL: Not reported |
| MAINTAIN [73] R-maint vs. Obs | 3 | Advanced NMZL/SMZL after response to BR N = 104 | N/A | Median: NR vs. 92.2 months | 0.35 (0.17–0.76) p = 0.008 | 6-years: 92% vs. 86% | 0.52 (0.20–1.39) |
| IELSG-19 [70] Clb-R vs. Clb vs. R | 3 | EMZL, no prior systemic therapy N = 401 | 79 vs. 63 vs. 56 | Median: NR vs. 8.3 years vs. 6.9 years | Clb-R vs. Clb: 0.62 (0.42 to 0.93) p = 0.0119 | 5-year: 90% vs. 89% vs. 92% | Clb-R vs. Clb: 1.24 (0.69–2.23) p = 0.464 |
| Salar et al., 2009 [71] FR | 2 | EMZL-MALT N = 22 | 90 | 2-year: 88% | N/A | 2-year: 100% | N/A |
| Brown et al., 2009 [72] FR | 2 | Advanced MZL N = 26 | 54 | 3-year: 80% | N/A | 3-year: 87% | N/A |
| AGMT MALT-2 [78] R2 | 2 | EMZL-MALT N = 46 | 54 | 27-month: 91% | N/A | Not reported | N/A |
| Fowler et al., 2014 [77] R2 | 2 | Advanced FL, MZL, SLL N(ITT) = 110 N(MZL) = 30 | ITT: 63 MZL: 67 | Median(ITT): 53.8 months Median(MZL): 53.8 months | N/A | 3-year(ITT): 96% 3-year(MZL): 100% | N/A |
| MALT 2008-01 [68,80] BR | 2 | EMZL-MALT N = 57 | 98 | 7-year: 93% | N/A | 7-year: 96% | N/A |
| BRISMA/ IELSG36 [69] BR | 2 | SMZL N = 56 | 73 | 3-year: 90% | N/A | 3-year: 96% | N/A |
5. Treatment of Relapsed/Refractory MZL
| Study Name/ Regimen | Phase | Population | CR (%) | PFS | OS | ||
|---|---|---|---|---|---|---|---|
| Median/Landmark | HR (95% CI) | Median/Landmark | HR (95% CI) | ||||
| PCYC-1121 [90] Ibrutinib | 2 | R/R MZL after SAR or CIT N = 63 | 10 | Median: 15.7 months | N/A | 33-month: 72% | N/A |
| MAGNOLIA [91,92] Zanubrutinib | 2 | R/R MZL after ≥1 R-based therapy N = 68 | 26 | 24-month: 71% | N/A | 24-month: 86% | N/A |
| AUGMENT [95] R2 vs. placebo-R | 3 | R/R FL or MZL N(ITT) = 358 N(MZL) = 63 | ITT: 34 vs. 18 MZL: 29 vs. 13 | Median(ITT): 39.4 vs. 14.1 months Median(MZL): 20.2 vs. 25.2 months | ITT: 0.46 (0.34–0.62) p < 0.001 MZL: 1.00 (0.47–2.13) | 2-year(ITT): 93% vs. 87% 2-year(MZL): 82% vs. 94% | ITT: 0.61 (0.33–1.13) MZL: 2.89 (0.56–14.92) |
| GADOLIN [89] Bendamustine-obinutuzumab vs. bendamustine | 3 | Rituximab- refractory iNHL N(ITT) = 396 N(MZL) = 46 | ITT: 17 vs. 17 MZL: Not reported | Median(ITT): NR vs. 14.9 months Median(MZL): Not reported | ITT: 0.55 (0.40–0.74) p = 0.0001 MZL: 0.94 (0.46–1.90) | Median(ITT): NR vs. NR Median(MZL): Not reported | ITT: 0.82 (0.52–1.30) p = 0.40 MZL: Not reported |
| Gopal et al., 2014 [83] Idelalisib | 2 | iNHL refractory to R + alkylating agent N(ITT) = 125 N(MZL) = 15 | ITT: 6 MZL: Not reported | Median(ITT): 11 months Median(MZL): Not reported | N/A | Median(ITT): 20.3 months Median(MZL): Not reported | N/A |
| DYNAMO [84] Duvelisib | 2 | iNHL refractory to R + chemotherapy N(ITT) = 129 N(MZL) = 18 | ITT: 2 MZL: 6 | Median(ITT): 9.5 months Median(MZL): not reported | N/A | Median(ITT): 28.9 months Median(MZL): not reported | N/A |
| CHRONOS-1 [81] Copanlisib | 2 | R/R iNHL, ≥2 prior therapies N(ITT) = 142 N(MZL) = 23 | ITT: 17 MZL: 13 | Median(ITT): 12.5 months Median(MZL): not reported | N/A | Median(ITT): 42.6 months Median(MZL): not reported | N/A |
| CHRONOS-3 [86] Copanlisib-R vs. placebo-R | 3 | iNHL relapsed after anti-CD20 therapy N(ITT) = 458 N(MZL) = 95 | ITT: 34 vs. 15 MZL: 39 vs. 10 | Median(ITT): 21.5 vs. 13.8 months Median(MZL): 22.1 vs. 11.5 months | ITT: 0.52 (0.39–0.69) p < 0.0001 MZL: 0.48 (0.25–0.92) p = 0.012 | 36-month(ITT): 83% vs. 81% 36-month(MZL): Not reported | ITT: 1.07 (0.63–1.82) MZL: not reported |
| UNITY-NHL [97] Umbralisib | 2b | R/R iNHL after ≥1 anti-CD20 therapy N(ITT) = 208 N(MZL) = 69 | ITT: 9 MZL: 16 | Median(ITT): Not reported Median(MZL): NR | N/A | Not reported | N/A |
6. Summary and Canadian Perspective
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sriskandarajah, P.; Dearden, C.E. Epidemiology and environmental aspects of marginal zone lymphomas. Best Pract. Res. Clin. Haematol. 2017, 30, 84–91. [Google Scholar] [CrossRef] [PubMed]
- Goede, V. Marginal zone lymphoma in elderly and geriatric patients. Best Pract. Res. Clin. Haematol. 2017, 30, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Cerhan, J.R.; Habermann, T.M. Epidemiology of marginal zone lymphoma. Ann. Lymphoma 2021, 5, 1. [Google Scholar] [CrossRef]
- Di Rocco, A.; Petrucci, L.; Assanto, G.M.; Martelli, M.; Pulsoni, A. Extranodal Marginal Zone Lymphoma: Pathogenesis, Diagnosis and Treatment. Cancers 2022, 14, 1742. [Google Scholar] [CrossRef]
- Cheah, C.Y.; Zucca, E.; Rossi, D.; Habermann, T.M. Marginal zone lymphoma: Present status and future perspectives. Haematologica 2022, 107, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Luminari, S.; Merli, M.; Rattotti, S.; Tarantino, V.; Marcheselli, L.; Cavallo, F.; Varettoni, M.; Bianchi, B.; Merli, F.; Tedeschi, A.; et al. Early progression as a predictor of survival in marginal zone lymphomas: An analysis from the FIL-NF10 study. Blood 2019, 134, 798–801. [Google Scholar] [CrossRef]
- Conconi, A.; Martinelli, G.; Thiéblemont, C.; Ferreri, A.J.; Devizzi, L.; Peccatori, F.; Ponzoni, M.; Pedrinis, E.; Dell’Oro, S.; Pruneri, G.; et al. Clinical activity of rituximab in extranodal marginal zone B-cell lymphoma of MALT type. Blood 2003, 102, 2741–2745. [Google Scholar] [CrossRef]
- Laurent, C.; Cook, J.R.; Yoshino, T.; Quintanilla-Martinez, L.; Jaffe, E.S. Follicular lymphoma and marginal zone lymphoma: How many diseases? Virchows Archiv. 2023, 482, 149–162. [Google Scholar] [CrossRef]
- Jaffe, E.S.; Harris, N.L.; Stein, H.; Vardiman, J.W. (Eds.) World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of Haematopoietic and Lymphoid Tissues; IARC Press: Lyon, France, 2001. [Google Scholar]
- Berger, F.; Traverse-Glehen, A.; Felman, P.; Callet-Bauchu, E.; Baseggio, L.; Gazzo, S.; Thieblemont, C.; French, M.; Magaud, J.P.; Salles, G.; et al. Clinicopathologic features of Waldenström’s macroglobulinemia and marginal zone lymphoma: Are they distinct or the same entity? Clin. Lymphoma 2005, 5, 220–224. [Google Scholar] [CrossRef]
- Treon, S.P.; Xu, L.; Yang, G.; Zhou, Y.; Liu, X.; Cao, Y.; Sheehy, P.; Manning, R.J.; Patterson, C.J.; Tripsas, C.; et al. MYD88 L265P somatic mutation in Waldenström’s macroglobulinemia. N. Engl. J. Med. 2012, 367, 826–833. [Google Scholar] [CrossRef]
- Raderer, M.; Wöhrer, S.; Streubel, B.; Troch, M.; Turetschek, K.; Jäger, U.; Skrabs, C.; Gaiger, A.; Drach, J.; Puespoek, A.; et al. Assessment of Disease Dissemination in Gastric Compared With Extragastric Mucosa-Associated Lymphoid Tissue Lymphoma Using Extensive Staging: A Single-Center Experience. J. Clin. Oncol. 2006, 24, 3136–3141. [Google Scholar] [CrossRef] [PubMed]
- Santos, T.S.d.; Tavares, R.S.; Farias, D.L.C.d. Splenic marginal zone lymphoma: A literature review of diagnostic and therapeutic challenges. Rev. Bras. de Hematol. e Hemoter. 2017, 39, 146–154. [Google Scholar] [CrossRef] [PubMed]
- Epperla, N.; Zhao, Q.; Shea, L.; Karmali, R.; Torka, P.; Seijung Oh, T.; Anampa-Guzman, A.; Jordan Bruno, X.; Umyarova, E.; Lindsey, K.; et al. Impact of Monoclonal Protein at Diagnosis on Outcomes in Patients with Marginal Zone Lymphoma: A Multicenter Cohort Study. Blood 2022, 140, 420–422. [Google Scholar] [CrossRef]
- Traverse-Glehen, A.; Baseggio, L.; Salles, G.; Felman, P.; Berger, F. Splenic marginal zone B-cell lymphoma: A distinct clinicopathological and molecular entity. Recent advances in ontogeny and classification. Curr. Opin. Oncol. 2011, 23, 441–448. [Google Scholar] [CrossRef]
- Gebhart, J.; Lechner, K.; Skrabs, C.; Sliwa, T.; Müldür, E.; Ludwig, H.; Nösslinger, T.; Vanura, K.; Stamatopoulos, K.; Simonitsch-Klupp, I.; et al. Lupus anticoagulant and thrombosis in splenic marginal zone lymphoma. Thromb. Res. 2014, 134, 980–984. [Google Scholar] [CrossRef]
- Basset, M.; Defrancesco, I.; Milani, P.; Nuvolone, M.; Rattotti, S.; Foli, A.; Mangiacavalli, S.; Varettoni, M.; Benvenuti, P.; Cartia, C.S.; et al. Nonlymphoplasmacytic lymphomas associated with light-chain amyloidosis. Blood 2020, 135, 293–296. [Google Scholar] [CrossRef] [PubMed]
- Stübgen, J.-P. Autoantibody-Mediated Sensory Polyneuropathy Associated with Indolent B-Cell Non-Hodgkin’s Lymphoma: A Report of Two Cases. J. Clin. Neurol. 2015, 11, 283. [Google Scholar] [CrossRef]
- Zucca, E.; Arcaini, L.; Buske, C.; Johnson, P.W.; Ponzoni, M.; Raderer, M.; Ricardi, U.; Salar, A.; Stamatopoulos, K.; Thieblemont, C.; et al. Marginal zone lymphomas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2020, 31, 17–29. [Google Scholar] [CrossRef]
- Van Den Brand, M.; Van Krieken, J.H.J.M. Recognizing nodal marginal zone lymphoma: Recent advances and pitfalls. A systematic review. Haematologica 2013, 98, 1003–1013. [Google Scholar] [CrossRef]
- Perrone, S.; D’Elia, G.M.; Annechini, G.; Ferretti, A.; Tosti, M.E.; Foà, R.; Pulsoni, A. Splenic marginal zone lymphoma: Prognostic factors, role of watch and wait policy, and other therapeutic approaches in the rituximab era. Leuk Res. 2016, 44, 53–60. [Google Scholar] [CrossRef]
- Fischbach, W.; Dorlöchter, C. Patients with gastric MALT lymphoma revealing persisting endoscopic abnormalities after successful eradication of Helicobacter pylori can be safely managed by a watch-and-wait strategy. Z. Gastroenterol. 2019, 57, 593–599. [Google Scholar] [CrossRef] [PubMed]
- Joffe, E.; Leyfman, Y.; Drill, E.; Rajeeve, S.; Zelenetz, A.D.; Palomba, M.L.; Moskowitz, C.H.; Portlock, C.; Noy, A.; Horwitz, S.M.; et al. Active surveillance of primary extranodal marginal zone lymphoma of bronchus-associated lymphoid tissue. Blood Adv. 2021, 5, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.; Zhou, K.; Peng, Z.; Liang, L.; Cao, J.; Mei, J. Surgery and chemotherapy cannot improve the survival of patients with early-stage mucosa-associated lymphoid tissue derived primary pulmonary lymphoma. Front. Oncol. 2022, 12, 965727. [Google Scholar] [CrossRef] [PubMed]
- Luminari, S.; Cesaretti, M.; Marcheselli, L.; Rashid, I.; Madrigali, S.; Maiorana, A.; Federico, M. Decreasing incidence of gastric MALT lymphomas in the era of anti-Helicobacter pylori interventions: Results from a population-based study on extranodal marginal zone lymphomas. Ann. Oncol. 2010, 21, 855–859. [Google Scholar] [CrossRef] [PubMed]
- Parsonnet, J.; Hansen, S.; Rodriguez, L.; Gelb, A.B.; Warnke, R.A.; Jellum, E.; Orentreich, N.; Vogelman, J.H.; Friedman, G.D. Helicobacter pylori Infection and Gastric Lymphoma. N. Engl. J. Med. 1994, 330, 1267–1271. [Google Scholar] [CrossRef] [PubMed]
- Zullo, A.; Hassan, C.; Andriani, A.; Cristofari, F.; De Francesco, V.; Ierardi, E.; Tomao, S.; Morini, S.; Vaira, D. Eradication therapy for Helicobacter pylori in patients with gastric MALT lymphoma: A pooled data analysis. Am. J. Gastroenterol. 2009, 104, 1932–1937, quiz 8. [Google Scholar] [CrossRef]
- Jung, K.; Kim, D.H.; Seo, H.I.; Gong, E.J.; Bang, C.S. Efficacy of eradication therapy in Helicobacter pylori-negative gastric mucosa-associated lymphoid tissue lymphoma: A meta-analysis. Helicobacter 2021, 26, e12774. [Google Scholar] [CrossRef]
- Xie, Y.-L.; He, C.-Y.; Wei, S.-Q.; Guan, W.-J.; Jiang, Z. Clinical efficacy of the modified Helicobacter pylori eradication therapy for Helicobacter pylori-negative gastric mucosa-associated lymphoid tissue lymphoma: A meta analysis. Chin. Med. J. 2020, 133, 1337–1346. [Google Scholar] [CrossRef]
- Liu, H.; Ye, H.; Ruskone-Fourmestraux, A.; De Jong, D.; Pileri, S.; Thiede, C.; Lavergne, A.; Boot, H.; Caletti, G.; Wündisch, T.; et al. T(11;18) is a marker for all stage gastric MALT lymphomas that will not respond to H. pylori eradication. Gastroenterology 2002, 122, 1286–1294. [Google Scholar] [CrossRef]
- Ferreri, A.J.M.; Ponzoni, M.; Guidoboni, M.; Resti, A.G.; Politi, L.S.; Cortelazzo, S.; Demeter, J.; Zallio, F.; Palmas, A.; Muti, G.; et al. Bacteria-Eradicating Therapy With Doxycycline in Ocular Adnexal MALT Lymphoma: A Multicenter Prospective Trial. JNCI J. Natl. Cancer Inst. 2006, 98, 1375–1382. [Google Scholar] [CrossRef] [PubMed]
- Chanudet, E.; Zhou, Y.; Bacon, C.M.; Wotherspoon, A.C.; Müller-Hermelink, H.K.; Adam, P.; Dong, H.Y.; de Jong, D.; Li, Y.; Wei, R.; et al. Chlamydia psittaci is variably associated with ocular adnexal MALT lymphoma in different geographical regions. J. Pathol. 2006, 209, 344–351. [Google Scholar] [CrossRef] [PubMed]
- Vargas, R.L.; Fallone, E.; Felgar, R.E.; Friedberg, J.W.; Arbini, A.A.; Andersen, A.A.; Rothberg, P.G. Is there an association between ocular adnexal lymphoma and infection with Chlamydia psittaci? The University of Rochester experience. Leuk Res. 2006, 30, 547–551. [Google Scholar] [CrossRef] [PubMed]
- Aigelsreiter, A.; Leitner, E.; Deutsch, A.J.; Kessler, H.H.; Stelzl, E.; Beham-Schmid, C.; Beham, A.; Krugmann, J.; Dinges, H.P.; Linkesch, W.; et al. Chlamydia psittaci in MALT lymphomas of ocular adnexals: The Austrian experience. Leuk Res. 2008, 32, 1292–1294. [Google Scholar] [CrossRef] [PubMed]
- Collina, F.; Chiara, A.D.; Renzo, A.D.; Rosa, G.D.; Botti, G.; Franco, R. Chlamydia psittaci in ocular adnexa MALT lymphoma: A possible role in lymphomagenesis and a different geographical distribution. Infect. Agents Cancer 2012, 7, 8. [Google Scholar] [CrossRef] [PubMed]
- Köller, M.C.; Aigelsreiter, A. Chlamydia psittaci in Ocular Adnexal MALT Lymphoma: A Possible Causative Agent in the Pathogenesis of This Disease. Curr. Clin. Microbiol. Rep. 2018, 5, 261–267. [Google Scholar] [CrossRef]
- Roggero, E.; Zucca, E.; Mainetti, C.; Bertoni, F.; Valsangiacomo, C.; Pedrinis, E.; Borisch, B.; Piffaretti, J.C.; Cavalli, F.; Isaacson, P.G. Eradication of Borrelia burgdorferi infection in primary marginal zone B-cell lymphoma of the skin. Hum. Pathol. 2000, 31, 263–268. [Google Scholar] [CrossRef]
- Kütting, B.; Bonsmann, G.; Metze, D.; Luger, T.A.; Cerroni, L. Borrelia burgdorferi-associated primary cutaneous B cell lymphoma: Complete clearing of skin lesions after antibiotic pulse therapy or intralesional injection of interferon alfa-2a. J. Am. Acad. Dermatol. 1997, 36, 311–314. [Google Scholar] [CrossRef]
- Lecuit, M.; Abachin, E.; Martin, A.; Poyart, C.; Pochart, P.; Suarez, F.; Bengoufa, D.; Feuillard, J.; Lavergne, A.; Gordon, J.I.; et al. Immunoproliferative Small Intestinal Disease Associated with Campylobacter jejuni. N. Engl. J. Med. 2004, 350, 239–248. [Google Scholar] [CrossRef]
- Kassan, S.S.; Thomas, T.L.; Moutsopoulos, H.M.; Hoover, R.; Kimberly, R.P.; Budman, D.R.; Costa, J.; Decker, J.L.; Chused, T.M. Increased risk of lymphoma in sicca syndrome. Ann. Intern. Med. 1978, 89, 888–892. [Google Scholar] [CrossRef]
- Royer, B.; Cazals-Hatem, D.; Sibilia, J.; Agbalika, F.; Cayuela, J.-M.; Soussi, T.; Maloisel, F.D.R.; Clauvel, J.-P.; Brouet, J.-C.; Mariette, X. Lymphomas in Patients With Sjögren’s Syndrome Are Marginal Zone B-Cell Neoplasms, Arise in Diverse Extranodal and Nodal Sites, and Are Not Associated With Viruses. Blood 1997, 90, 766–775. [Google Scholar] [CrossRef]
- Voulgarelis, M.; Dafni, U.G.; Isenberg, D.A.; Moutsopoulos, H.M. Malignant lymphoma in primary Sjögren’s syndrome: A multicenter, retrospective, clinical study by the European concerted action on Sjögren’s syndrome. Arthritis Rheum. 1999, 42, 1765–1772. [Google Scholar] [CrossRef] [PubMed]
- Derringer, G.A.; Thompson, L.D.; Frommelt, R.A.; Bijwaard, K.E.; Heffess, C.S.; Abbondanzo, S.L. Malignant lymphoma of the thyroid gland: A clinicopathologic study of 108 cases. Am. J. Surg. Pathol. 2000, 24, 623–639. [Google Scholar] [CrossRef] [PubMed]
- Karvounis, E.; Kappas, I.; Angelousi, A.; Makris, G.-M.; Kassi, E. Mucosa-Associated Lymphoid Tissue Lymphoma of the Thyroid Gland: A Systematic Review of the Literature. Eur. Thyroid J. 2020, 9, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Mele, A.; Pulsoni, A.; Bianco, E.; Musto, P.; Szklo, A.; Sanpaolo, M.G.; Iannitto, E.; De Renzo, A.; Martino, B.; Liso, V.; et al. Hepatitis C virus and B-cell non-Hodgkin lymphomas: An Italian multicenter case-control study. Blood 2003, 102, 996–999. [Google Scholar] [CrossRef]
- Kelaidi, C.; Rollot, F.; Park, S.; Tulliez, M.; Christoforov, B.; Calmus, Y.; Podevin, P.; Bouscary, D.; Sogni, P.; Blanche, P.; et al. Response to antiviral treatment in hepatitis C virus-associated marginal zone lymphomas. Leukemia 2004, 18, 1711–1716. [Google Scholar] [CrossRef]
- Arcaini, L.; Vallisa, D.; Rattotti, S.; Ferretti, V.V.; Ferreri, A.J.M.; Bernuzzi, P.; Merli, M.; Varettoni, M.; Chiappella, A.; Ambrosetti, A.; et al. Antiviral treatment in patients with indolent B-cell lymphomas associated with HCV infection: A study of the Fondazione Italiana Linfomi. Ann. Oncol. 2014, 25, 1404–1410. [Google Scholar] [CrossRef]
- Yahalom, J.; Xu, A.J.; Noy, A.; Lobaugh, S.; Chelius, M.; Chau, K.; Portlock, C.; Hajj, C.; Imber, B.S.; Straus, D.J.; et al. Involved-site radiotherapy for Helicobacter pylori–independent gastric MALT lymphoma: 26 years of experience with 178 patients. Blood Adv. 2021, 5, 1830–1836. [Google Scholar] [CrossRef]
- Goda, J.S.; Gospodarowicz, M.; Pintilie, M.; Wells, W.; Hodgson, D.C.; Sun, A.; Crump, M.; Tsang, R.W. Long-term outcome in localized extranodal mucosa-associated lymphoid tissue lymphomas treated with radiotherapy. Cancer 2010, 116, 3815–3824. [Google Scholar] [CrossRef]
- Lowry, L.; Smith, P.; Qian, W.; Falk, S.; Benstead, K.; Illidge, T.; Linch, D.; Robinson, M.; Jack, A.; Hoskin, P. Reduced dose radiotherapy for local control in non-Hodgkin lymphoma: A randomised phase III trial. Radiother. Oncol. 2011, 100, 86–92. [Google Scholar] [CrossRef]
- Yahalom, J.; Illidge, T.; Specht, L.; Hoppe, R.T.; Li, Y.-X.; Tsang, R.; Wirth, A. Modern Radiation Therapy for Extranodal Lymphomas: Field and Dose Guidelines From the International Lymphoma Radiation Oncology Group. Int. J. Radiat. Oncol. Biol. Phys. 2015, 92, 11–31. [Google Scholar] [CrossRef]
- Pinnix, C.C.; Dabaja, B.S.; Milgrom, S.A.; Smith, G.L.; Abou, Z.; Nastoupil, L.; Romaguera, J.; Turturro, F.; Fowler, N.; Fayad, L.; et al. Ultra-low-dose radiotherapy for definitive management of ocular adnexal B-cell lymphoma. Head Neck 2017, 39, 1095–1100. [Google Scholar] [CrossRef] [PubMed]
- Cerrato, M.; Orlandi, E.; Vella, A.; Bartoncini, S.; Iorio, G.C.; Bongiovanni, D.; Capriotti, F.; Boccomini, C.; Vassallo, F.; Cavallin, C.; et al. Efficacy of low-dose radiotherapy (2 Gy × 2) in the treatment of marginal zone and mucosa-associated lymphoid tissue lymphomas. Br. J. Radiol. 2021, 94, 20210012. [Google Scholar] [CrossRef]
- ChacóN, J.I.; Mollejo, M.; MuñOz, E.; Algara, P.; Mateo, M.; Lopez, L.; Andrade, J.S.; Carbonero, I.G.A.; MartıίNez, B.; Piris, M.A.; et al. Splenic marginal zone lymphoma: Clinical characteristics and prognostic factors in a series of 60 patients. Blood 2002, 100, 1648–1654. [Google Scholar] [CrossRef]
- Xing, K.H.; Kahlon, A.; Skinnider, B.F.; Connors, J.M.; Gascoyne, R.D.; Sehn, L.H.; Savage, K.J.; Slack, G.W.; Shenkier, T.N.; Klasa, R.; et al. Outcomes in splenic marginal zone lymphoma: Analysis of 107 patients treated in British Columbia. Br. J. Haematol. 2015, 169, 520–527. [Google Scholar] [CrossRef] [PubMed]
- Kalpadakis, C.; Pangalis, G.A.; Angelopoulou, M.K.; Sachanas, S.; Kontopidou, F.N.; Yiakoumis, X.; Kokoris, S.I.; Dimitriadou, E.M.; Dimopoulou, M.N.; Moschogiannis, M.; et al. Treatment of Splenic Marginal Zone Lymphoma With Rituximab Monotherapy: Progress Report and Comparison With Splenectomy. Oncologist 2013, 18, 190–197. [Google Scholar] [CrossRef] [PubMed]
- Lenglet, J.; Traullé, C.; Mounier, N.; Benet, C.; Munoz-Bongrand, N.; Amorin, S.; Noguera, M.E.; Traverse-Glehen, A.; Ffrench, M.; Baseggio, L.; et al. Long-term follow-up analysis of 100 patients with splenic marginal zone lymphoma treated with splenectomy as first-line treatment. Leuk Lymphoma 2014, 55, 1854–1860. [Google Scholar] [CrossRef] [PubMed]
- Pata, G.; Damiani, E.; Bartoli, M.; Solari, S.; Anastasia, A.; Pagani, C.; Tucci, A.; Ragni, F. Peri-operative complications and hematologic improvement after first-line splenectomy for splenic marginal zone lymphoma. Leuk. Lymphoma 2016, 57, 1467–1470. [Google Scholar] [CrossRef] [PubMed]
- Arcaini, L.; Rossi, D.; Paulli, M. Splenic marginal zone lymphoma: From genetics to management. Blood 2016, 127, 2072–2081. [Google Scholar] [CrossRef]
- Lossos, I.S.; Morgensztern, D.; Blaya, M.; Alencar, A.; Pereira, D.; Rosenblatt, J. Rituximab for treatment of chemoimmunotherapy naive marginal zone lymphoma. Leuk. Lymphoma 2007, 48, 1630–1632. [Google Scholar] [CrossRef]
- Raderer, M.; Jäger, G.; Brugger, S.; Püspök, A.; Fiebiger, W.; Drach, J.; Wotherspoon, A.; Chott, A. Rituximab for treatment of advanced extranodal marginal zone B cell lymphoma of the mucosa-associated lymphoid tissue lymphoma. Oncology 2003, 65, 306–310. [Google Scholar] [CrossRef]
- Tsimberidou, A.M.; Catovsky, D.; Schlette, E.; O’Brien, S.; Wierda, W.G.; Kantarjian, H.; Garcia-Manero, G.; Wen, S.; Do, K.-A.; Lerner, S.; et al. Outcomes in patients with splenic marginal zone lymphoma and marginal zone lymphoma treated with rituximab with or without chemotherapy or chemotherapy alone. Cancer 2006, 107, 125–135. [Google Scholar] [CrossRef]
- Bennett, M.; Sharma, K.; Yegena, S.; Gavish, I.; Dave, H.P.; Schechter, G.P. Rituximab monotherapy for splenic marginal zone lymphoma. Haematologica 2005, 90, 856–858. [Google Scholar]
- Kalpadakis, C.; Pangalis, G.A.; Sachanas, S.; Tsirkinidis, P.; Kontopidou, F.N.; Moschogiannis, M.; Yiakoumis, X.; Koulieris, E.; Dimopoulou, M.N.; Kokkoris, S.I.; et al. Rituximab monotherapy in splenic marginal zone lymphoma: Prolonged responses and potential benefit from maintenance. Blood 2018, 132, 666–670. [Google Scholar] [CrossRef] [PubMed]
- Flinn, I.W.; Van Der Jagt, R.; Kahl, B.S.; Wood, P.; Hawkins, T.E.; Macdonald, D.; Hertzberg, M.; Kwan, Y.-L.; Simpson, D.; Craig, M.; et al. Randomized trial of bendamustine-rituximab or R-CHOP/R-CVP in first-line treatment of indolent NHL or MCL: The BRIGHT study. Blood 2014, 123, 2944–2952. [Google Scholar] [CrossRef] [PubMed]
- Rummel, M.J.; Niederle, N.; Maschmeyer, G.; Banat, G.A.; von Grünhagen, U.; Losem, C.; Kofahl-Krause, D.; Heil, G.; Welslau, M.; Balser, C.; et al. Bendamustine plus rituximab versus CHOP plus rituximab as first-line treatment for patients with indolent and mantle-cell lymphomas: An open-label, multicentre, randomised, phase 3 non-inferiority trial. Lancet 2013, 381, 1203–1210. [Google Scholar] [CrossRef]
- Rummel, M.J.; Maschmeyer, G.; Ganser, A.; Heider, A.; von Gruenhagen, U.; Losem, C.; Heil, G.; Welslau, M.; Balser, C.; Kaiser, U.; et al. Bendamustine plus rituximab (B-R) versus CHOP plus rituximab (CHOP-R) as first-line treatment in patients with indolent lymphomas: Nine-year updated results from the StiL NHL1 study. J. Clin. Oncol. 2017, 35, 7501. [Google Scholar] [CrossRef]
- Salar, A.; Domingo-Domenech, E.; Panizo, C.; Nicolás, C.; Bargay, J.; Muntañola, A.; Canales, M.; Bello, J.L.; Sancho, J.M.; Tomás, J.F.; et al. Long-term results of a phase 2 study of rituximab and bendamustine for mucosa-associated lymphoid tissue lymphoma. Blood 2017, 130, 1772–1774. [Google Scholar] [CrossRef]
- Iannitto, E.; Bellei, M.; Amorim, S.; Ferreri, A.J.M.; Marcheselli, L.; Cesaretti, M.; Haioun, C.; Mancuso, S.; Bouabdallah, K.; Gressin, R.; et al. Efficacy of bendamustine and rituximab in splenic marginal zone lymphoma: Results from the phase II BRISMA/IELSG36 study. Br. J. Haematol. 2018, 183, 755–765. [Google Scholar] [CrossRef] [PubMed]
- Zucca, E.; Conconi, A.; Martinelli, G.; Bouabdallah, R.; Tucci, A.; Vitolo, U.; Martelli, M.; Pettengell, R.; Salles, G.; Sebban, C.; et al. Final Results of the IELSG-19 Randomized Trial of Mucosa-Associated Lymphoid Tissue Lymphoma: Improved Event-Free and Progression-Free Survival With Rituximab Plus Chlorambucil Versus Either Chlorambucil or Rituximab Monotherapy. J. Clin. Oncol. 2017, 35, 1905–1912. [Google Scholar] [CrossRef]
- Salar, A.; Domingo-Domenech, E.; Estany, C.; Canales, M.A.; Gallardo, F.; Servitje, O.; Fraile, G.; Montalbán, C. Combination therapy with rituximab and intravenous or oral fludarabine in the first-line, systemic treatment of patients with extranodal marginal zone B-cell lymphoma of the mucosa-associated lymphoid tissue type. Cancer 2009, 115, 5210–5217. [Google Scholar] [CrossRef]
- Brown, J.R.; Friedberg, J.W.; Feng, Y.; Scofield, S.; Phillips, K.; Dal Cin, P.; Joyce, R.; Takvorian, R.W.; Fisher, D.C.; Fisher, R.I.; et al. A phase 2 study of concurrent fludarabine and rituximab for the treatment of marginal zone lymphomas. Br. J. Haematol. 2009, 145, 741–748. [Google Scholar] [CrossRef] [PubMed]
- Rummel, M.J.; Koenigsmann, M.; Chow, K.U.; Knauf, W.; Lerchenmuller, C.A.; Losem, C.; Goerner, M.; Hertenstein, B.; Decker, T.; Ganser, A.; et al. Two years rituximab maintenance vs. observation after first line treatment with bendamustine plus rituximab (B-R) in patients with marginal zone lymphoma (MZL): Results of a prospective, randomized, multicenter phase 2 study (the StiL NHL7-2008 MAINTAIN trial). J. Clin. Oncol. 2018, 36, 7515. [Google Scholar]
- Aksoy, S.; Dizdar, O.; Hayran, M.; Harputluoğlu, H. Infectious complications of rituximab in patients with lymphoma during maintenance therapy: A systematic review and meta-analysis. Leuk Lymphoma 2009, 50, 357–365. [Google Scholar] [CrossRef] [PubMed]
- Shree, T.; Shankar, V.; Lohmeyer, J.J.K.; Czerwinski, D.K.; Schroers-Martin, J.G.; Rodriguez, G.M.; Beygi, S.; Kanegai, A.M.; Corbelli, K.S.; Gabriel, E.; et al. CD20-Targeted Therapy Ablates De Novo Antibody Response to Vaccination but Spares Preestablished Immunity. Blood Cancer Discov. 2022, 3, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Vijenthira, A.; Gong, I.; Betschel, S.D.; Cheung, M.; Hicks, L.K. Vaccine response following anti-CD20 therapy: A systematic review and meta-analysis of 905 patients. Blood Adv. 2021, 5, 2624–2643. [Google Scholar] [CrossRef] [PubMed]
- Fowler, N.H.; Davis, R.E.; Rawal, S.; Nastoupil, L.; Hagemeister, F.B.; McLaughlin, P.; Kwak, L.W.; Romaguera, J.E.; Fanale, M.A.; Fayad, L.E.; et al. Safety and activity of lenalidomide and rituximab in untreated indolent lymphoma: An open-label, phase 2 trial. Lancet Oncol. 2014, 15, 1311–1318. [Google Scholar] [CrossRef] [PubMed]
- Kiesewetter, B.; Willenbacher, E.; Willenbacher, W.; Egle, A.; Neumeister, P.; Voskova, D.; Mayerhoefer, M.E.; Simonitsch-Klupp, I.; Melchardt, T.; Greil, R.; et al. A phase 2 study of rituximab plus lenalidomide for mucosa-associated lymphoid tissue lymphoma. Blood 2017, 129, 383–385. [Google Scholar] [CrossRef]
- Flinn, I.W.; Van Der Jagt, R.; Kahl, B.; Wood, P.; Hawkins, T.; Macdonald, D.; Simpson, D.; Kolibaba, K.; Issa, S.; Chang, J.; et al. First-Line Treatment of Patients With Indolent Non-Hodgkin Lymphoma or Mantle-Cell Lymphoma With Bendamustine Plus Rituximab Versus R-CHOP or R-CVP: Results of the BRIGHT 5-Year Follow-Up Study. J. Clin. Oncol. 2019, 37, 984–991. [Google Scholar] [CrossRef]
- Salar, A.; Domingo-Domenech, E.; Panizo, C.; Nicolás, C.; Bargay, J.; Muntañola, A.; Canales, M.; Bello, J.L.; Sancho, J.M.; Tomás, J.F.; et al. First-line response-adapted treatment with the combination of bendamustine and rituximab in patients with mucosa-associated lymphoid tissue lymphoma (MALT2008-01): A multicentre, single-arm, phase 2 trial. Lancet Haematol. 2014, 1, e104–e111. [Google Scholar] [CrossRef]
- Dreyling, M.; Santoro, A.; Mollica, L.; Leppä, S.; Follows, G.; Lenz, G.; Kim, W.S.; Nagler, A.; Dimou, M.; Demeter, J.; et al. Long-term safety and efficacy of the PI3K inhibitor copanlisib in patients with relapsed or refractory indolent lymphoma: 2-year follow-up of the CHRONOS-1 study. Am. J. Hematol. 2020, 95, 362–371. [Google Scholar] [CrossRef]
- United States Food & Drug Administration. FDA Investigating Possible Increased Risk of Death with Lymphoma Medicine Ukoniq (umbralisib). Available online: https://www.fda.gov/drugs/development-approval-process-drugs/fda-investigating-possible-increased-risk-death-lymphoma-medicine-ukoniq-umbralisib (accessed on 23 December 2022).
- Gopal, A.K.; Kahl, B.S.; De Vos, S.; Wagner-Johnston, N.D.; Schuster, S.J.; Jurczak, W.J.; Flinn, I.W.; Flowers, C.R.; Martin, P.; Viardot, A.; et al. PI3Kδ Inhibition by Idelalisib in Patients with Relapsed Indolent Lymphoma. N. Engl. J. Med. 2014, 370, 1008–1018. [Google Scholar] [CrossRef] [PubMed]
- Flinn, I.W.; Miller, C.B.; Ardeshna, K.M.; Tetreault, S.; Assouline, S.E.; Mayer, J.; Merli, M.; Lunin, S.D.; Pettitt, A.R.; Nagy, Z.; et al. DYNAMO: A Phase II Study of Duvelisib (IPI-145) in Patients With Refractory Indolent Non-Hodgkin Lymphoma. J. Clin. Oncol. 2019, 37, 912–922. [Google Scholar] [CrossRef] [PubMed]
- Dreyling, M.; Santoro, A.; Mollica, L.; Leppä, S.; Follows, G.A.; Lenz, G.; Kim, W.S.; Nagler, A.; Panayiotidis, P.; Demeter, J.; et al. Phosphatidylinositol 3-Kinase Inhibition by Copanlisib in Relapsed or Refractory Indolent Lymphoma. J. Clin. Oncol. 2017, 35, 3898–3905. [Google Scholar] [CrossRef]
- Matasar, M.J.; Capra, M.; Özcan, M.; Lv, F.; Li, W.; Yañez, E.; Sapunarova, K.; Lin, T.; Jin, J.; Jurczak, W.; et al. Copanlisib plus rituximab versus placebo plus rituximab in patients with relapsed indolent non-Hodgkin lymphoma (CHRONOS-3): A double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Oncol. 2021, 22, 678–689. [Google Scholar] [CrossRef] [PubMed]
- Freeman, C.L.; Kridel, R.; Moccia, A.A.; Savage, K.J.; Villa, D.R.; Scott, D.W.; Gerrie, A.S.; Ferguson, D.; Cafferty, F.; Slack, G.W.; et al. Early progression after bendamustine-rituximab is associated with high risk of transformation in advanced stage follicular lymphoma. Blood 2019, 134, 761–764. [Google Scholar] [CrossRef]
- Salles, G.A.; Morschhauser, F.; Solal-Céligny, P.; Thieblemont, C.; Lamy, T.; Tilly, H.; Gyan, E.; Lei, G.; Wenger, M.; Wassner-Fritsch, E.; et al. Obinutuzumab (GA101) in Patients With Relapsed/Refractory Indolent Non-Hodgkin Lymphoma: Results from the Phase II GAUGUIN Study. J. Clin. Oncol. 2013, 31, 2920–2926. [Google Scholar] [CrossRef] [PubMed]
- Sehn, L.H.; Chua, N.; Mayer, J.; Dueck, G.; Trněný, M.; Bouabdallah, K.; Fowler, N.; Delwail, V.; Press, O.; Salles, G.; et al. Obinutuzumab plus bendamustine versus bendamustine monotherapy in patients with rituximab-refractory indolent non-Hodgkin lymphoma (GADOLIN): A randomised, controlled, open-label, multicentre, phase 3 trial. Lancet Oncol. 2016, 17, 1081–1093. [Google Scholar] [CrossRef]
- Noy, A.; De Vos, S.; Coleman, M.; Martin, P.; Flowers, C.R.; Thieblemont, C.; Morschhauser, F.; Collins, G.P.; Ma, S.; Peles, S.; et al. Durable ibrutinib responses in relapsed/refractory marginal zone lymphoma: Long-term follow-up and biomarker analysis. Blood Adv. 2020, 4, 5773–5784. [Google Scholar] [CrossRef]
- Opat, S.; Tedeschi, A.; Linton, K.; McKay, P.; Hu, B.; Chan, H.; Jin, J.; Sobieraj-Teague, M.; Zinzani, P.L.; Coleman, M.; et al. The MAGNOLIA Trial: Zanubrutinib, a Next-Generation Bruton Tyrosine Kinase Inhibitor, Demonstrates Safety and Efficacy in Relapsed/Refractory Marginal Zone Lymphoma. Clin. Cancer Res. 2021, 27, 6323–6332. [Google Scholar] [CrossRef]
- Opat, S.; Tedeschi, A.; Hu, B.; Linton, K.M.; McKay, P.; Chan, H.; Jin, J.; Sun, M.; Sobieraj-Teague, M.; Zinzani, P.L.; et al. Long-Term Efficacy and Safety of Zanubrutinib in Patients with Relapsed/Refractory (R/R) Marginal Zone Lymphoma (MZL): Final Analysis of the Magnolia (BGB-3111-214) Trial. Blood 2022, 140, 573–576. [Google Scholar] [CrossRef]
- Tam, C.S.; Opat, S.; D’Sa, S.; Jurczak, W.; Lee, H.-P.; Cull, G.; Owen, R.G.; Marlton, P.; Wahlin, B.E.; Sanz, R.G.; et al. A randomized phase 3 trial of zanubrutinib vs ibrutinib in symptomatic Waldenström macroglobulinemia: The ASPEN study. Blood 2020, 136, 2038–2050. [Google Scholar] [CrossRef]
- Brown, J.R.; Eichhorst, B.; Hillmen, P.; Jurczak, W.; Kaźmierczak, M.; Lamanna, N.; O’Brien, S.M.; Tam, C.S.; Qiu, L.; Zhou, K.; et al. Zanubrutinib or Ibrutinib in Relapsed or Refractory Chronic Lymphocytic Leukemia. N. Engl. J. Med. 2022, 388, 319–332. [Google Scholar] [CrossRef]
- Leonard, J.P.; Trneny, M.; Izutsu, K.; Fowler, N.H.; Hong, X.; Zhu, J.; Zhang, H.; Offner, F.; Scheliga, A.; Nowakowski, G.S.; et al. AUGMENT: A Phase III Study of Lenalidomide Plus Rituximab Versus Placebo Plus Rituximab in Relapsed or Refractory Indolent Lymphoma. J. Clin. Oncol. 2019, 37, 1188–1199. [Google Scholar] [CrossRef] [PubMed]
- Kiesewetter, B.; Greil, R.; Willenbacher, W.; Neumeister, P.; Fridrik, M.A.; Markus, R. AGMT MALT-2: A Phase II Study of Rituximab Plus Lenalidomide in Patients with Extranodal Marginal Zone B-Cell Lymphoma of the Mucosa-Associated Lymphoid Tissue (MALT lymphoma). Blood 2015, 126, 3973. [Google Scholar] [CrossRef]
- Fowler, N.H.; Samaniego, F.; Jurczak, W.; Ghosh, N.; Derenzini, E.; Reeves, J.A.; Knopińska-Posłuszny, W.; Cheah, C.Y.; Phillips, T.; Lech-Maranda, E.; et al. Umbralisib, a Dual PI3Kδ/CK1ε Inhibitor in Patients With Relapsed or Refractory Indolent Lymphoma. J. Clin. Oncol. 2021, 39, 1609–1618. [Google Scholar] [CrossRef]
- Zinzani, P.L.; Minotti, G. Anti-CD19 monoclonal antibodies for the treatment of relapsed or refractory B-cell malignancies: A narrative review with focus on diffuse large B-cell lymphoma. J. Cancer Res. Clin. Oncol. 2022, 148, 177–190. [Google Scholar] [CrossRef]
- Neelapu, S.S.; Locke, F.L.; Bartlett, N.L.; Lekakis, L.J.; Miklos, D.B.; Jacobson, C.A.; Braunschweig, I.; Oluwole, O.O.; Siddiqi, T.; Lin, Y.; et al. Axicabtagene Ciloleucel CAR T-Cell Therapy in Refractory Large B-Cell Lymphoma. N. Engl. J. Med. 2017, 377, 2531–2544. [Google Scholar] [CrossRef]
- Schuster, S.J.; Bishop, M.R.; Tam, C.S.; Waller, E.K.; Borchmann, P.; McGuirk, J.P.; Jäger, U.; Jaglowski, S.; Andreadis, C.; Westin, J.R.; et al. Tisagenlecleucel in Adult Relapsed or Refractory Diffuse Large B-Cell Lymphoma. N. Engl. J. Med. 2019, 380, 45–56. [Google Scholar] [CrossRef] [PubMed]
- Salles, G.; Duell, J.; González Barca, E.; Tournilhac, O.; Jurczak, W.; Liberati, A.M.; Nagy, Z.; Obr, A.; Gaidano, G.; André, M.; et al. Tafasitamab plus lenalidomide in relapsed or refractory diffuse large B-cell lymphoma (L-MIND): A multicentre, prospective, single-arm, phase 2 study. Lancet Oncol. 2020, 21, 978–988. [Google Scholar] [CrossRef]
- Caimi, P.F.; Ai, W.; Alderuccio, J.P.; Ardeshna, K.M.; Hamadani, M.; Hess, B.; Kahl, B.S.; Radford, J.; Solh, M.; Stathis, A.; et al. Loncastuximab tesirine in relapsed or refractory diffuse large B-cell lymphoma (LOTIS-2): A multicentre, open-label, single-arm, phase 2 trial. Lancet Oncol. 2021, 22, 790–800. [Google Scholar] [CrossRef]
- Viardot, A.; Goebeler, M.-E.; Hess, G.; Neumann, S.; Pfreundschuh, M.; Adrian, N.; Zettl, F.; Libicher, M.; Sayehli, C.; Stieglmaier, J.; et al. Phase 2 study of the bispecific T-cell engager (BiTE) antibody blinatumomab in relapsed/refractory diffuse large B-cell lymphoma. Blood 2016, 127, 1410–1416. [Google Scholar] [CrossRef] [PubMed]
- Brice, P.; Bastion, Y.; Lepage, E.; Brousse, N.; Haïoun, C.; Moreau, P.; Straetmans, N.; Tilly, H.; Tabah, I.; Solal-Céligny, P. Comparison in low-tumor-burden follicular lymphomas between an initial no-treatment policy, prednimustine, or interferon alfa: A randomized study from the Groupe d’Etude des Lymphomes Folliculaires. Groupe d’Etude des Lymphomes de l’Adulte. J. Clin. Oncol. 1997, 15, 1110–1117. [Google Scholar] [CrossRef]
- Wilder, R.B.; Jones, D.; Tucker, S.L.; Fuller, L.M.; Ha, C.S.; McLaughlin, P.; Hess, M.A.; Cabanillas, F.; Cox, J.D. Long-term results with radiotherapy for Stage I-II follicular lymphomas. Int. J. Radiat. Oncol. Biol. Phys. 2001, 51, 1219–1227. [Google Scholar] [CrossRef] [PubMed]
- Petersen, P.M.; Gospodarowicz, M.; Tsang, R.; Pintilie, M.; Wells, W.; Hodgson, D.; Sun, A.; Crump, M.; Patterson, B.; Bailey, D. Long-term outcome in stage I and II follicular lymphoma following treatment with involved field radiation therapy alone. J. Clin. Oncol. 2004, 22, 6521. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peters, A.; Keating, M.-M.; Nikonova, A.; Doucette, S.; Prica, A. Management of Marginal Zone Lymphoma: A Canadian Perspective. Curr. Oncol. 2023, 30, 1745-1759. https://doi.org/10.3390/curroncol30020135
Peters A, Keating M-M, Nikonova A, Doucette S, Prica A. Management of Marginal Zone Lymphoma: A Canadian Perspective. Current Oncology. 2023; 30(2):1745-1759. https://doi.org/10.3390/curroncol30020135
Chicago/Turabian StylePeters, Anthea, Mary-Margaret Keating, Anna Nikonova, Sarah Doucette, and Anca Prica. 2023. "Management of Marginal Zone Lymphoma: A Canadian Perspective" Current Oncology 30, no. 2: 1745-1759. https://doi.org/10.3390/curroncol30020135
APA StylePeters, A., Keating, M.-M., Nikonova, A., Doucette, S., & Prica, A. (2023). Management of Marginal Zone Lymphoma: A Canadian Perspective. Current Oncology, 30(2), 1745-1759. https://doi.org/10.3390/curroncol30020135





