Overexpression of AKR1B10 Predicts Poor Prognosis in Gastric Cancer Patients Undergoing Surgical Resection
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
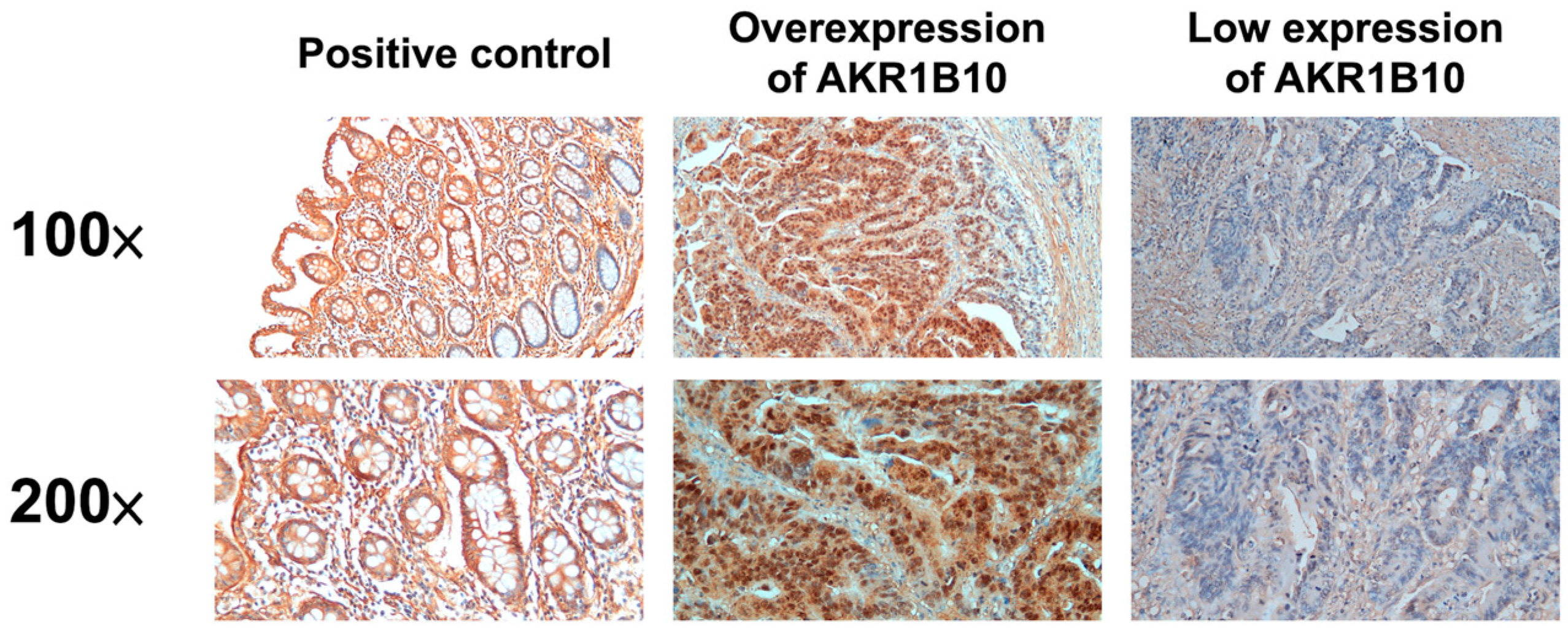
2.2. Immunohistochemistry
2.3. Statistical Analysis
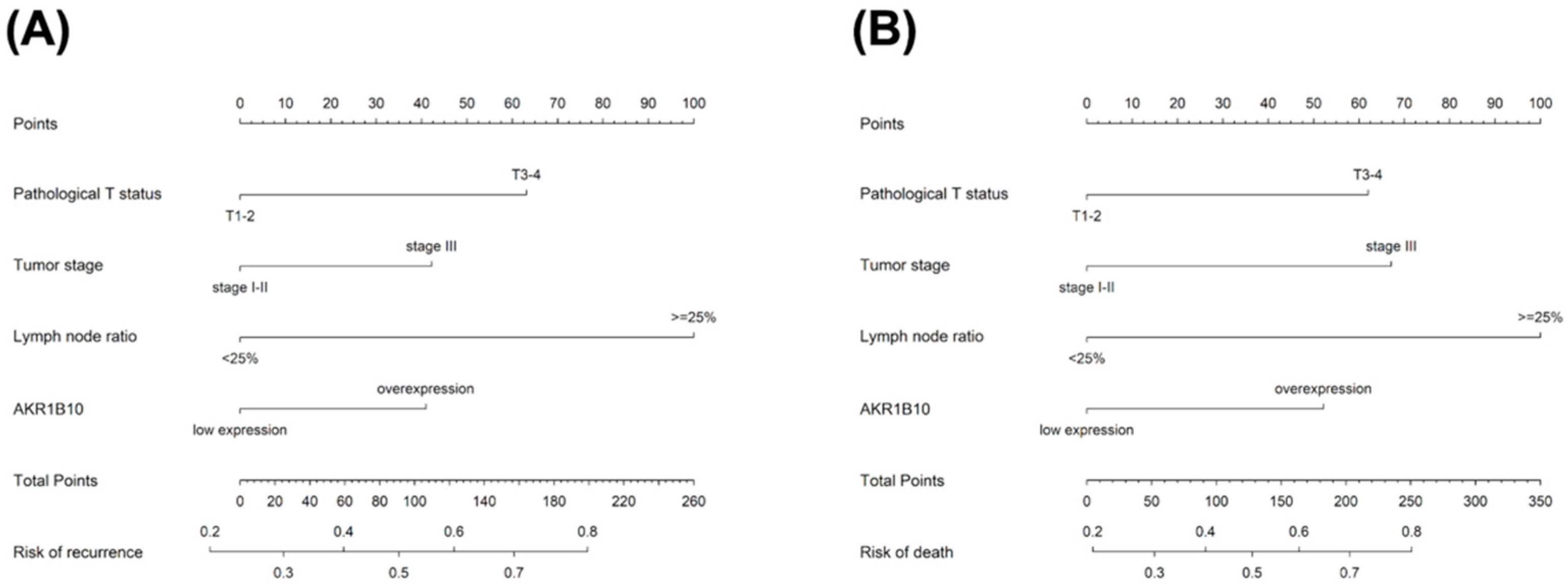
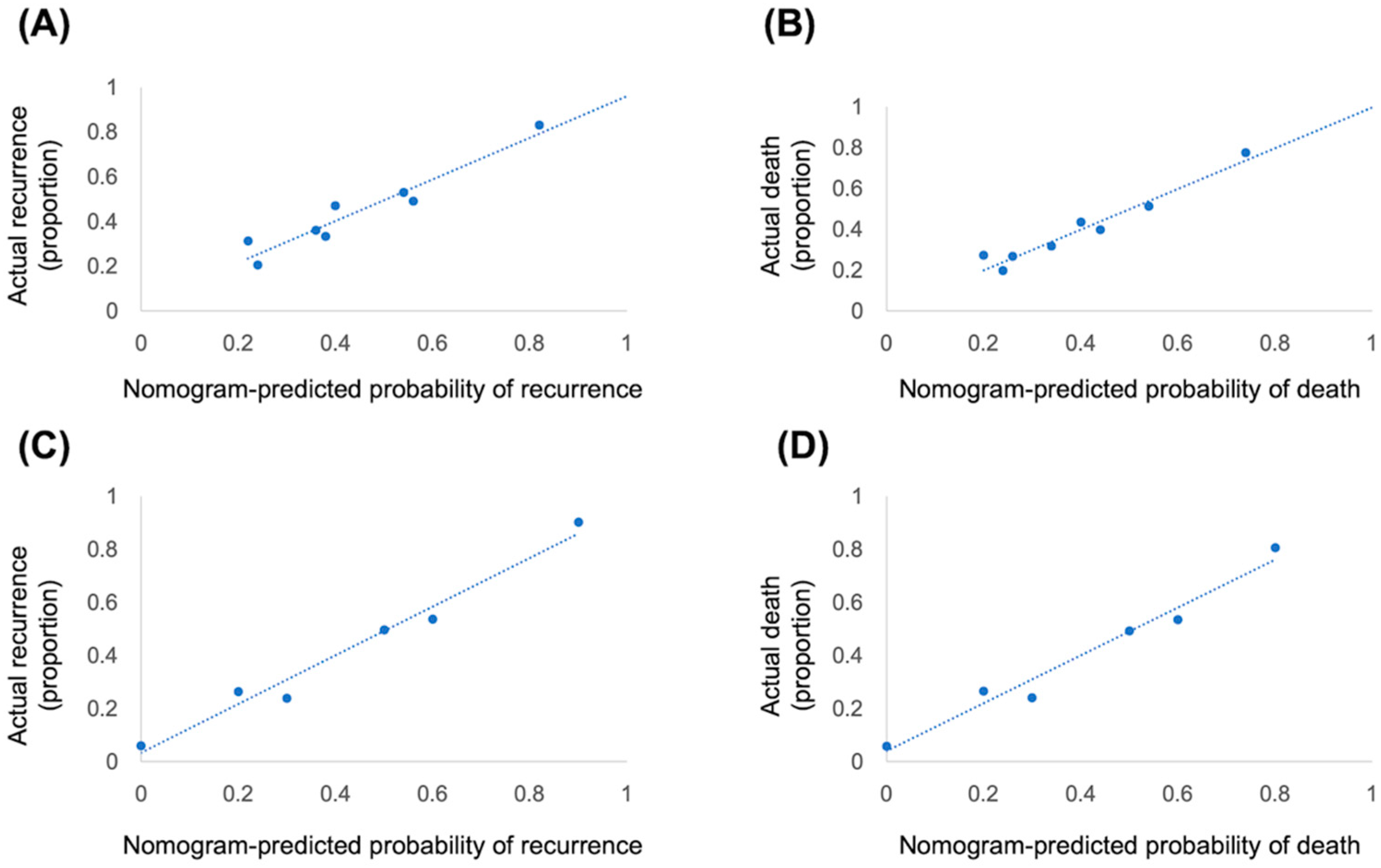
2.4. Construction and Validation of Nomogram
2.5. Ethical Statement
3. Results
3.1. Patient Characteristics
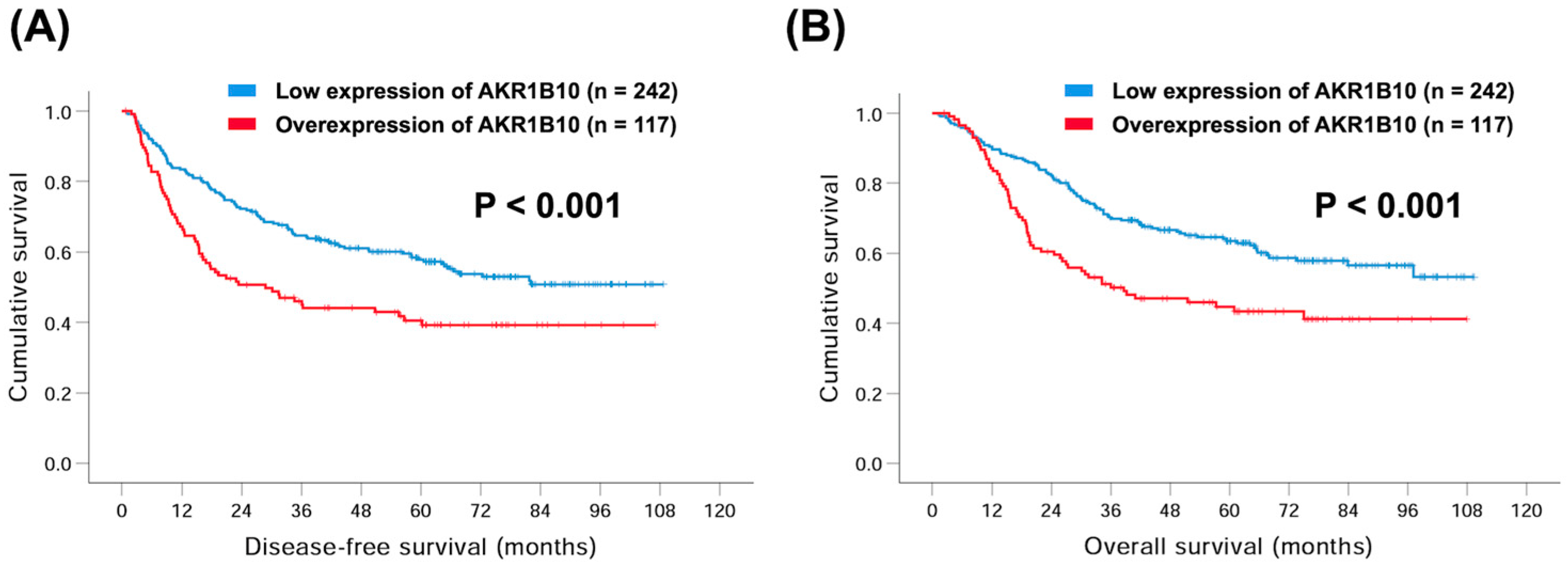
3.2. AKR1B10 Expression and Clinical Outcome
3.3. Subgroup Analyses of AKR1B10 and Survival
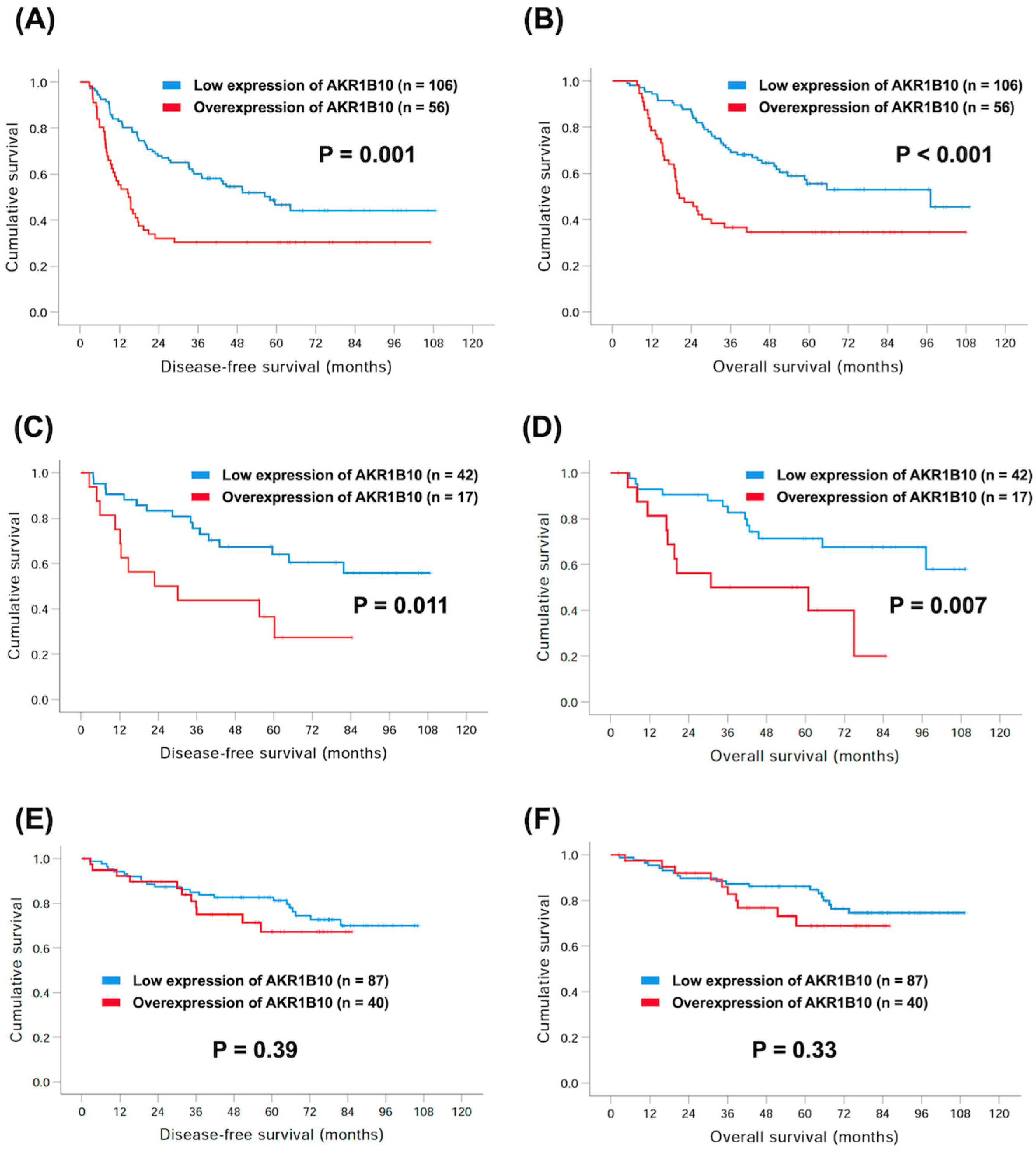
3.4. Nomogram and Validation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cancer Registry Annual Report 1972–2019; Health Promotion Administration, Ministry of Health and Welfare: Taipei City, Taiwan, 2019.
- Bang, Y.J.; Kim, Y.W.; Yang, H.K.; Chung, H.C.; Park, Y.K.; Lee, K.H.; Lee, K.W.; Kim, Y.H.; Noh, S.I.; Cho, J.Y.; et al. Adjuvant capecitabine and oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): A phase 3 open-label, randomised controlled trial. Lancet 2012, 379, 315–321. [Google Scholar] [CrossRef] [PubMed]
- Sakuramoto, S.; Sasako, M.; Yamaguchi, T.; Kinoshita, T.; Fujii, M.; Nashimoto, A.; Furukawa, H.; Nakajima, T.; Ohashi, Y.; Imamura, H.; et al. Adjuvant chemotherapy for gastric cancer with S-1, an oral fluoropyrimidine. N. Engl. J. Med. 2007, 357, 1810–1820. [Google Scholar] [CrossRef] [PubMed]
- Penning, T.M. The aldo-keto reductases (AKRs): Overview. Chem. Biol. Interact. 2015, 234, 236–246. [Google Scholar] [CrossRef] [PubMed]
- Cao, D.; Fan, S.T.; Chung, S.S. Identification and characterization of a novel human aldose reductase-like gene. J. Biol. Chem. 1998, 273, 11429–11435. [Google Scholar] [CrossRef] [PubMed]
- Crosas, B.; Hyndman, D.J.; Gallego, O.; Martras, S.; Pares, X.; Flynn, T.G.; Farres, J. Human aldose reductase and human small intestine aldose reductase are efficient retinal reductases: Consequences for retinoid metabolism. Biochem. J. 2003, 373, 973–979. [Google Scholar] [CrossRef]
- Hyndman, D.J.; Flynn, T.G. Sequence and expression levels in human tissues of a new member of the aldo-keto reductase family. Biochim. Biophys. Acta 1998, 1399, 198–202. [Google Scholar] [CrossRef]
- Fukumoto, S.; Yamauchi, N.; Moriguchi, H.; Hippo, Y.; Watanabe, A.; Shibahara, J.; Taniguchi, H.; Ishikawa, S.; Ito, H.; Yamamoto, S.; et al. Overexpression of the aldo-keto reductase family protein AKR1B10 is highly correlated with smokers’ non-small cell lung carcinomas. Clin. Cancer Res. 2005, 11, 1776–1785. [Google Scholar] [CrossRef]
- Balendiran, G.K.; Martin, H.J.; El-Hawari, Y.; Maser, E. Cancer biomarker AKR1B10 and carbonyl metabolism. Chem. Biol. Interact. 2009, 178, 134–137. [Google Scholar] [CrossRef]
- Li, C.P.; Goto, A.; Watanabe, A.; Murata, K.; Ota, S.; Niki, T.; Aburatani, H.; Fukayama, M. AKR1B10 in usual interstitial pneumonia: Expression in squamous metaplasia in association with smoking and lung cancer. Pathol. Res. Pract. 2008, 204, 295–304. [Google Scholar] [CrossRef]
- Penning, T.M. AKR1B10: A new diagnostic marker of non-small cell lung carcinoma in smokers. Clin. Cancer Res. 2005, 11, 1687–1690. [Google Scholar] [CrossRef]
- Yoshitake, H.; Takahashi, M.; Ishikawa, H.; Nojima, M.; Iwanari, H.; Watanabe, A.; Aburatani, H.; Yoshida, K.; Ishi, K.; Takamori, K.; et al. Aldo-keto reductase family 1, member B10 in uterine carcinomas: A potential risk factor of recurrence after surgical therapy in cervical cancer. Int. J. Gynecol. Cancer Off. J. Int. Gynecol. Cancer Soc. 2007, 17, 1300–1306. [Google Scholar] [CrossRef] [PubMed]
- Scuric, Z.; Stain, S.C.; Anderson, W.F.; Hwang, J.J. New member of aldose reductase family proteins overexpressed in human hepatocellular carcinoma. Hepatology 1998, 27, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Luo, D.X.; Huang, C.; Shen, Y.; Bu, Y.; Markwell, S.; Gao, J.; Liu, J.; Zu, X.; Cao, Z.; et al. AKR1B10 overexpression in breast cancer: Association with tumor size, lymph node metastasis and patient survival and its potential as a novel serum marker. Int. J. Cancer 2012, 131, E862–E871. [Google Scholar] [CrossRef] [PubMed]
- Zhong, L.; Liu, Z.; Yan, R.; Johnson, S.; Zhao, Y.; Fang, X.; Cao, D. Aldo-keto reductase family 1 B10 protein detoxifies dietary and lipid-derived alpha, beta-unsaturated carbonyls at physiological levels. Biochem. Biophys. Res. Commun. 2009, 387, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, F.X.; Gallego, O.; Ardevol, A.; Moro, A.; Dominguez, M.; Alvarez, S.; Alvarez, R.; de Lera, A.R.; Rovira, C.; Fita, I.; et al. Aldo-keto reductases from the AKR1B subfamily: Retinoid specificity and control of cellular retinoic acid levels. Chem. Biol. Interact. 2009, 178, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Quinn, A.M.; Harvey, R.G.; Penning, T.M. Oxidation of PAH trans-dihydrodiols by human aldo-keto reductase AKR1B10. Chem. Res. Toxicol. 2008, 21, 2207–2215. [Google Scholar] [CrossRef]
- Morikawa, Y.; Kezuka, C.; Endo, S.; Ikari, A.; Soda, M.; Yamamura, K.; Toyooka, N.; El-Kabbani, O.; Hara, A.; Matsunaga, T. Acquisition of doxorubicin resistance facilitates migrating and invasive potentials of gastric cancer MKN45 cells through up-regulating aldo-keto reductase 1B10. Chem. Biol. Interact. 2015, 230, 30–39. [Google Scholar] [CrossRef]
- Hashimoto, Y.; Imanishi, K.; Tokui, N.; Okamoto, T.; Okamoto, A.; Hatakeyama, S.; Yoneyama, T.; Koie, T.; Kamimura, N.; Ohyama, C. Carboplatin-gemcitabine combination chemotherapy upregulates AKR1B10 expression in bladder cancer. Int. J. Clin. Oncol. 2013, 18, 177–182. [Google Scholar] [CrossRef]
- Barski, O.A.; Tipparaju, S.M.; Bhatnagar, A. The aldo-keto reductase superfamily and its role in drug metabolism and detoxification. Drug Metab. Rev. 2008, 40, 553–624. [Google Scholar] [CrossRef]
- Wang, C.; Yan, R.; Luo, D.; Watabe, K.; Liao, D.F.; Cao, D. Aldo-keto reductase family 1 member B10 promotes cell survival by regulating lipid synthesis and eliminating carbonyls. J. Biol. Chem. 2009, 284, 26742–26748. [Google Scholar] [CrossRef]
- Ma, J.; Yan, R.; Zu, X.; Cheng, J.M.; Rao, K.; Liao, D.F.; Cao, D. Aldo-keto reductase family 1 B10 affects fatty acid synthesis by regulating the stability of acetyl-CoA carboxylase-alpha in breast cancer cells. J. Biol. Chem. 2008, 283, 3418–3423. [Google Scholar] [CrossRef] [PubMed]
- Shao, X.; Wu, J.; Yu, S.; Zhou, Y.; Zhou, C. AKR1B10 inhibits the proliferation and migration of gastric cancer via regulating epithelial-mesenchymal transition. Aging (Albany NY) 2021, 13, 22298–22314. [Google Scholar] [CrossRef] [PubMed]
- Yao, H.B.; Xu, Y.; Chen, L.G.; Guan, T.P.; Ma, Y.Y.; He, X.J.; Xia, Y.J.; Tao, H.Q.; Shao, Q.S. AKR1B10, a good prognostic indicator in gastric cancer. Eur. J. Surg. Oncol. 2014, 40, 318–324. [Google Scholar] [CrossRef]
- Ahmed, S.M.U.; Jiang, Z.N.; Zheng, Z.H.; Li, Y.; Wang, X.J.; Tang, X. AKR1B10 expression predicts response of gastric cancer to neoadjuvant chemotherapy. Oncol. Lett. 2019, 17, 773–780. [Google Scholar] [CrossRef]
- Liu, R.; Zheng, S.; Yang, C.Y.; Yu, Y.; Peng, S.; Ge, Q.; Lin, Q.; Li, Q.; Shi, W.; Shao, Y. Prognostic value of aldo-keto reductase family 1 member B10 (AKR1B10) in digestive system cancers: A meta-analysis. Medicine 2021, 100, e25454. [Google Scholar] [CrossRef] [PubMed]
- Amin, M.B.; Edge, S.; Greene, F.; Byrd, D.R.; Brookland, R.K.; Washington, M.K.; Gershenwald, J.E.; Compton, C.C.; Hess, K.R.; Sullivan, D.C.; et al. AJCC Cancer Staging Manual, 8th ed.; Springer: New York, NY, USA, 2017. [Google Scholar]
- Okusa, T.; Nakane, Y.; Boku, T.; Takada, H.; Yamamura, M.; Hioki, K.; Yamamoto, M. Quantitative analysis of nodal involvement with respect to survival rate after curative gastrectomy for carcinoma. Surg. Gynecol. Obstet. 1990, 170, 488–494. [Google Scholar] [PubMed]
- Magaki, S.; Hojat, S.A.; Wei, B.; So, A.; Yong, W.H. An Introduction to the Performance of Immunohistochemistry. Methods Mol. Biol. 2019, 1897, 289–298. [Google Scholar] [CrossRef]
- Remmele, W.; Stegner, H.E. Recommendation for uniform definition of an immunoreactive score (IRS) for immunohistochemical estrogen receptor detection (ER-ICA) in breast cancer tissue. Pathologe 1987, 8, 138–140. [Google Scholar]
- Matsuoka, T.; Yashiro, M. Biomarkers of gastric cancer: Current topics and future perspective. World J. Gastroenterol. 2018, 24, 2818–2832. [Google Scholar] [CrossRef]
- Chandrashekar, D.S.; Bashel, B.; Balasubramanya, S.A.H.; Creighton, C.J.; Ponce-Rodriguez, I.; Chakravarthi, B.; Varambally, S. UALCAN: A Portal for Facilitating Tumor Subgroup Gene Expression and Survival Analyses. Neoplasia 2017, 19, 649–658. [Google Scholar] [CrossRef]
- Noh, S.H.; Park, S.R.; Yang, H.K.; Chung, H.C.; Chung, I.J.; Kim, S.W.; Kim, H.H.; Choi, J.H.; Kim, H.K.; Yu, W.; et al. Adjuvant capecitabine plus oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): 5-year follow-up of an open-label, randomised phase 3 trial. Lancet Oncol. 2014, 15, 1389–1396. [Google Scholar] [CrossRef] [PubMed]
- Sasako, M.; Sakuramoto, S.; Katai, H.; Kinoshita, T.; Furukawa, H.; Yamaguchi, T.; Nashimoto, A.; Fujii, M.; Nakajima, T.; Ohashi, Y. Five-year outcomes of a randomized phase III trial comparing adjuvant chemotherapy with S-1 versus surgery alone in stage II or III gastric cancer. J. Clin. Oncol. 2011, 29, 4387–4393. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Liu, R.; Zhang, W.H.; Chen, X.Z.; Liu, K.; Yang, K.; Chen, X.L.; Zhao, L.Y.; Chen, Z.X.; Zhou, Z.G.; et al. Difference Between Signet Ring Cell Gastric Cancers and Non-Signet Ring Cell Gastric Cancers: A Systematic Review and Meta-Analysis. Front. Oncol. 2021, 11, 618477. [Google Scholar] [CrossRef] [PubMed]
- Zhao, B.; Lv, W.; Zhang, J.; Zhang, J.; Huang, B.; Lin, J. Different prognostic significance of signet ring cell histology for early and advanced gastric cancer patients: A systematic review and meta-analysis. Expert Rev. Gastroenterol. Hepatol. 2020, 14, 499–509. [Google Scholar] [CrossRef] [PubMed]
- Zhao, S.; Lv, L.; Zheng, K.; Tian, Y.; Zheng, J.C.; Jiang, C.G. Prognosis and Biological Behavior of Gastric Signet-Ring Cell Carcinoma Better or Worse: A Meta-Analysis. Front. Oncol. 2021, 11, 603070. [Google Scholar] [CrossRef]
| Characteristics | Patient number (%) |
|---|---|
| Age (years) | 66 years old (30–89) |
| Sex | |
| Male | 238 (66.3%) |
| Female | 121 (33.7%) |
| Location | |
| Cardia/Fundus | 34 (9.5%) |
| Body | 134 (37.3%) |
| Antrum | 178 (49.6%) |
| Pylorus | 13 (3.6%) |
| Pathological T status | |
| 1 | 109 (30.4%) |
| 2 | 49 (13.6%) |
| 3 | 87 (24.2%) |
| 4 | 114 (31.8%) |
| Pathological N status | |
| 0 | 170 (47.4%) |
| 1 | 42 (11.7%) |
| 2 | 56 (15.6%) |
| 3 | 91 (25.3%) |
| Pathological tumor stage | |
| I | 127 (35.4%) |
| II | 82 (22.8%) |
| III | 150 (41.8%) |
| Grade | |
| 1 | 28 (7.8%) |
| 2 | 111 (30.9%) |
| 3 | 220 (61.3%) |
| Perineural invasion | |
| Yes | 175 (48.7%) |
| No | 184 (51.3%) |
| Lymphovascular invasion | |
| Yes | 199 (55.4%) |
| No | 160 (44.6%) |
| Gastrectomy | |
| Total | 44 (12.3%) |
| Subtotal | 292 (81.3%) |
| Proximal | 23 (6.4%) |
| Characteristics | Overexpression of AKR1B10 (n = 117) | Low Expression of AKR1B10 (n = 242) | p Value |
|---|---|---|---|
| Age | 0.84 | ||
| <60 years | 37 (31.6%) | 74 (30.6%) | |
| ≥60 years | 80 (68.4%) | 168 (69.4%) | |
| Sex | 0.71 | ||
| Male | 76 (65.0%) | 162 (66.9%) | |
| Female | 41 (35.0%) | 80 (33.1%) | |
| Pathological T status | 0.91 | ||
| 1 + 2 | 52 (44.4%) | 106 (43.8%) | |
| 3 + 4 | 65 (55.6%) | 136 (56.2%) | |
| Pathological N status | 0.75 | ||
| 0 | 54 (46.2%) | 116 (47.9%) | |
| 1 + 2 + 3 | 63 (53.8%) | 126 (52.1%) | |
| Pathological tumor stage | 0.35 | ||
| I + II | 64 (54.7%) | 145 (59.9%) | |
| III | 53 (45.3%) | 97 (40.1%) | |
| Grade | 0.06 | ||
| 1 + 2 | 37 (31.6%) | 102 (42.1%) | |
| 3 | 80 (68.4%) | 140 (57.9%) | |
| Total gastrectomy | 0.001 * | ||
| Yes | 24 (20.5%) | 20 (8.3%) | |
| No | 93 (79.5%) | 222 (91.7%) | |
| Perineural invasion | 0.07 | ||
| Yes | 65 (55.6%) | 110 (45.5%) | |
| No | 52 (44.4%) | 132 (54.5%) | |
| Lymphovascular invasion | 0.11 | ||
| Yes | 72 (61.5%) | 127 (52.5%) | |
| No | 45 (38.5%) | 115 (47.5%) | |
| Lymph node ratio | 0.06 | ||
| <25% | 81 (69.2%) | 190 (78.5%) | |
| ≥25% | 36 (30.8%) | 52 (21.5%) |
| Characteristics | No. of Patients | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|---|
| 5-Year DFS Rate (%) | p-Value | HR (95% CI) | p-Value | ||
| Age | 0.34 | ||||
| <60 years | 111 (30.9%) | 54.7 | |||
| ≥60 years | 248 (69.1%) | 51.1 | |||
| Sex | 0.25 | ||||
| Male | 238 (66.3%) | 49.2 | |||
| Female | 121 (33.7%) | 58.1 | |||
| Pathological T status | <0.001 * | ||||
| 1 + 2 | 52 (44.4%) | 74.7 | |||
| 3 + 4 | 65 (55.6%) | 34.5 | 2.08 (1.36–3.17) | 0.001 * | |
| Pathological N status | <0.001 * | ||||
| 0 | 54 (46.2%) | 71.0 | |||
| 1 + 2 + 3 | 63 (53.8%) | 35.3 | |||
| Pathological tumor stage | <0.001 * | ||||
| I + II | 64 (54.7%) | 70.9 | |||
| III | 53 (45.3%) | 25.9 | 1.62 (1.02–2.59) | 0.043 * | |
| Grade | 0.049 * | ||||
| 1 + 2 | 37 (31.6%) | 58.5 | |||
| 3 | 80 (68.4%) | 48.2 | |||
| Total gastrectomy | 0.014 * | ||||
| Yes | 24 (20.5%) | 37.6 | |||
| No | 93 (79.5%) | 54.3 | |||
| Perineural invasion | <0.001 * | ||||
| Yes | 65 (55.6%) | 32.0 | |||
| No | 52 (44.4%) | 71.1 | |||
| Lymphovascular invasion | <0.001 * | ||||
| Yes | 72 (61.5%) | 39.4 | |||
| No | 45 (38.5%) | 68.3 | |||
| Lymph node ratio | <0.001 * | ||||
| <25% | 81 (69.2%) | 64.1 | |||
| ≥25% | 36 (30.8%) | 15.6 | 2.22 (1.49–3.32) | <0.001 * | |
| AKR1B10 | 0.001 * | ||||
| Overexpression | 117 (32.6%) | 40.5 | 1.81 (1.32–2.47) | <0.001 * | |
| Low expression | 242 (67.4%) | 57.8 | |||
| Characteristics | No. of Patients | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|---|
| 5-Year OS Rate (%) | p-Value | HR (95% CI) | p-Value | ||
| Age | 0.33 | ||||
| <60 years | 111 (30.9%) | 60.7 | |||
| ≥60 years | 248 (69.1%) | 56.1 | |||
| Sex | 0.19 | ||||
| Male | 238 (66.3%) | 55.6 | |||
| Female | 121 (33.7%) | 61.4 | |||
| Pathological T status | <0.001 * | ||||
| 1 + 2 | 52 (44.4%) | 79.4 | |||
| 3 + 4 | 65 (55.6%) | 40.2 | 1.97 (1.24–3.12) | 0.004 * | |
| Pathological N status | <0.001 * | ||||
| 0 | 54 (46.2%) | 76.5 | |||
| 1 + 2 + 3 | 63 (53.8%) | 40.3 | |||
| Pathological tumor stage | <0.001 * | ||||
| I + II | 64 (54.7%) | 77.9 | |||
| III | 53 (45.3%) | 28.2 | 1.83 (1.12–3.00) | 0.017 * | |
| Grade | 0.08 | ||||
| 1 + 2 | 37 (31.6%) | 63.4 | |||
| 3 | 80 (68.4%) | 53.8 | |||
| Total gastrectomy | 0.006 * | ||||
| Yes | 24 (20.5%) | 41.9 | |||
| No | 93 (79.5%) | 59.7 | |||
| Perineural invasion | <0.001 * | ||||
| Yes | 65 (55.6%) | 35.5 | |||
| No | 52 (44.4%) | 77.5 | |||
| Lymphovascular invasion | <0.001 * | ||||
| Yes | 72 (61.5%) | 43.5 | |||
| No | 45 (38.5%) | 74.9 | |||
| Lymph node ratio | <0.001 * | ||||
| <25% | 81 (69.2%) | 70.0 | |||
| ≥25% | 36 (30.8%) | 18.2 | 2.23 (1.48–3.35) | <0.001 * | |
| AKR1B10 | <0.001 * | ||||
| Overexpression | 117 (32.6%) | 44.7 | 1.93 (1.39–2.67) | <0.001 * | |
| Low expression | 242 (67.4%) | 63.5 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, Y.-Y.; Liu, Y.-W.; Huang, G.-K.; Hung, K.-C.; Lin, Y.-H.; Yeh, C.-H.; Yin, S.-M.; Tsai, C.-H.; Chen, Y.-H. Overexpression of AKR1B10 Predicts Poor Prognosis in Gastric Cancer Patients Undergoing Surgical Resection. Curr. Oncol. 2023, 30, 85-99. https://doi.org/10.3390/curroncol30010007
Liu Y-Y, Liu Y-W, Huang G-K, Hung K-C, Lin Y-H, Yeh C-H, Yin S-M, Tsai C-H, Chen Y-H. Overexpression of AKR1B10 Predicts Poor Prognosis in Gastric Cancer Patients Undergoing Surgical Resection. Current Oncology. 2023; 30(1):85-99. https://doi.org/10.3390/curroncol30010007
Chicago/Turabian StyleLiu, Yu-Yin, Yueh-Wei Liu, Gong-Kai Huang, Kuo-Chen Hung, Yu-Hung Lin, Cheng-Hsi Yeh, Shih-Min Yin, Ching-Hua Tsai, and Yen-Hao Chen. 2023. "Overexpression of AKR1B10 Predicts Poor Prognosis in Gastric Cancer Patients Undergoing Surgical Resection" Current Oncology 30, no. 1: 85-99. https://doi.org/10.3390/curroncol30010007
APA StyleLiu, Y.-Y., Liu, Y.-W., Huang, G.-K., Hung, K.-C., Lin, Y.-H., Yeh, C.-H., Yin, S.-M., Tsai, C.-H., & Chen, Y.-H. (2023). Overexpression of AKR1B10 Predicts Poor Prognosis in Gastric Cancer Patients Undergoing Surgical Resection. Current Oncology, 30(1), 85-99. https://doi.org/10.3390/curroncol30010007





