Cost-Utility of the eHealth Application ‘Oncokompas’, Supporting Incurably Ill Cancer Patients to Self-Manage Their Cancer-Related Symptoms: Results of a Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
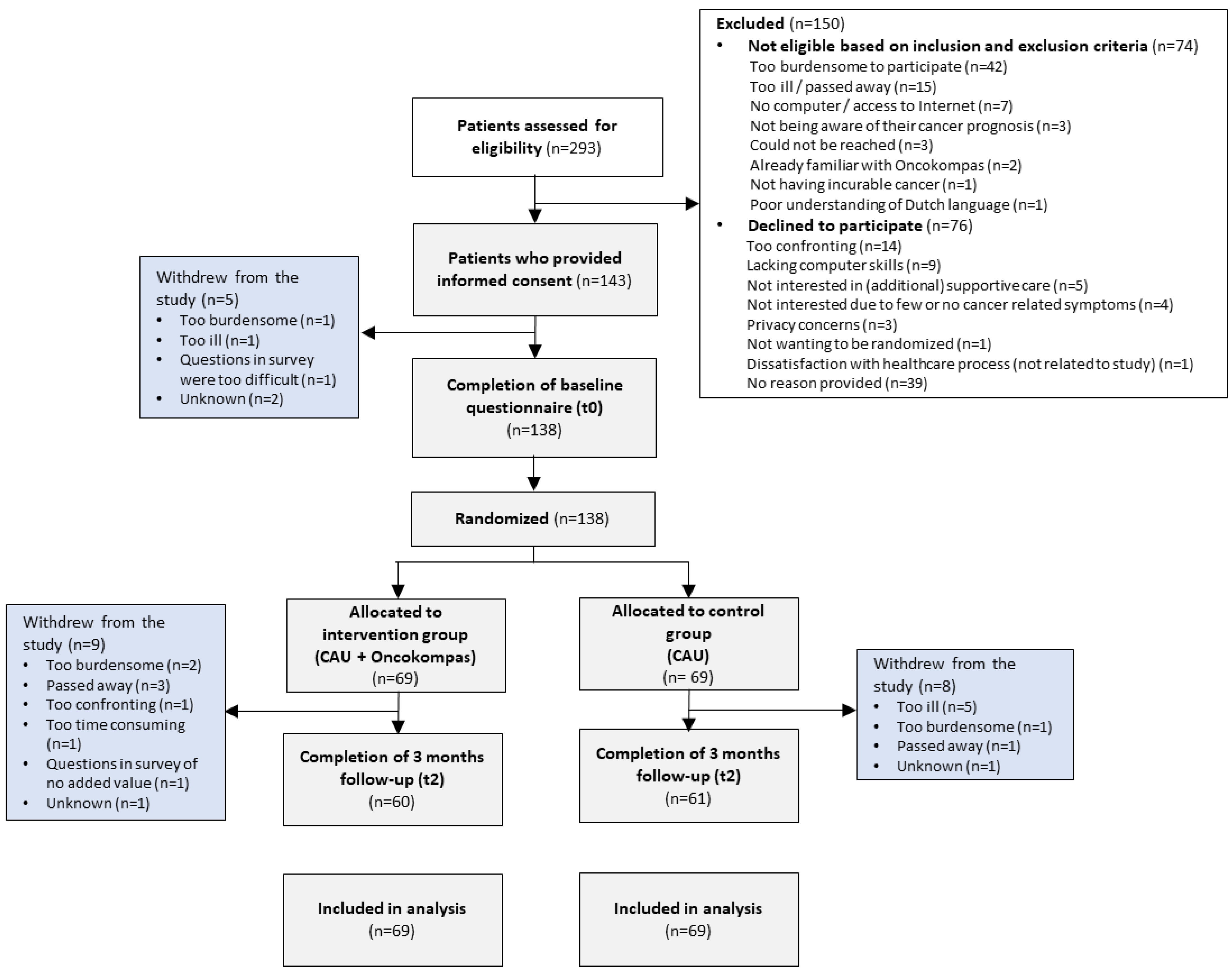
2.1. Study Design and Population
2.2. Randomization and Allocation
2.3. Care as Usual
2.4. Intervention
2.5. Outcome Assessment
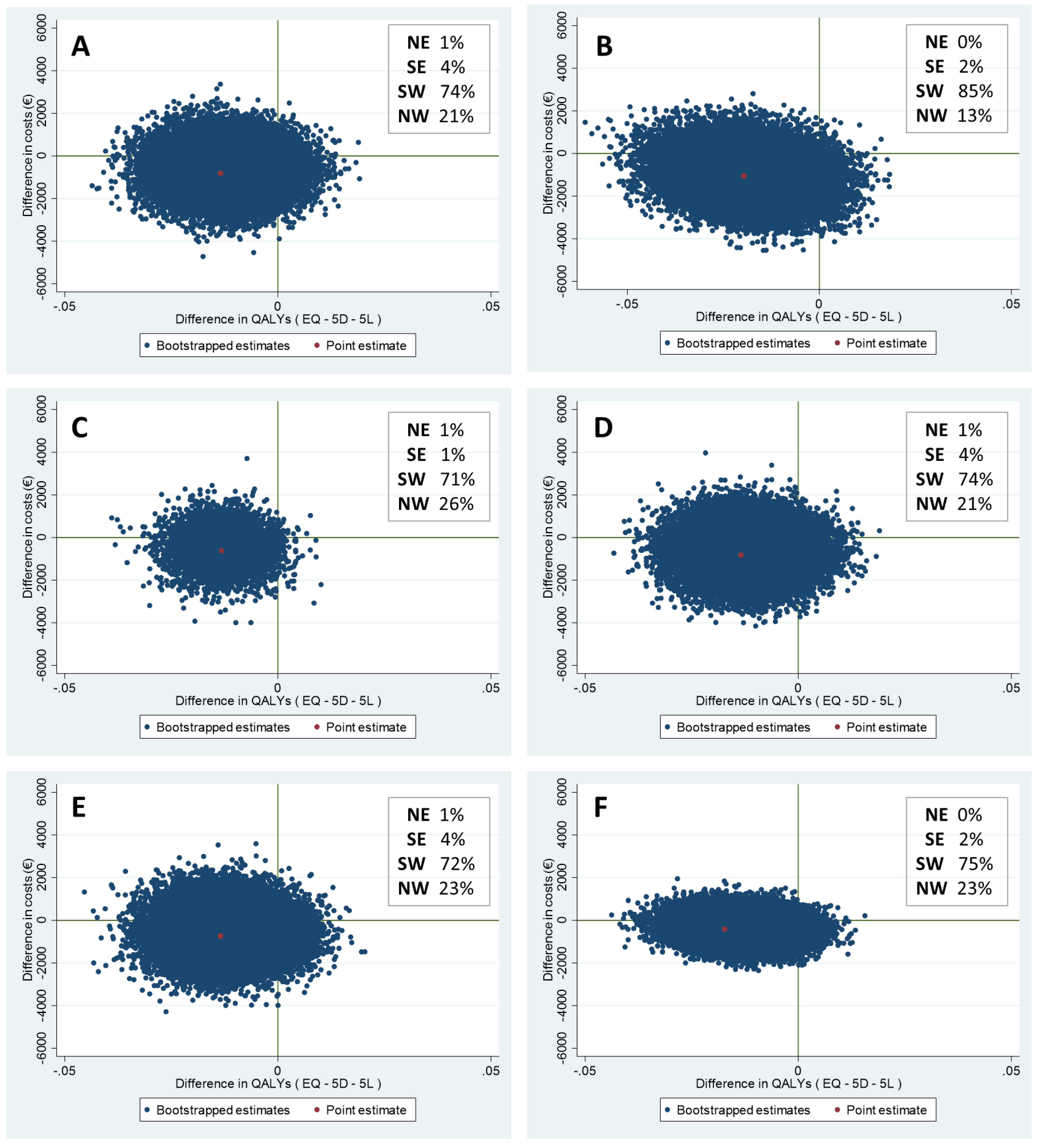
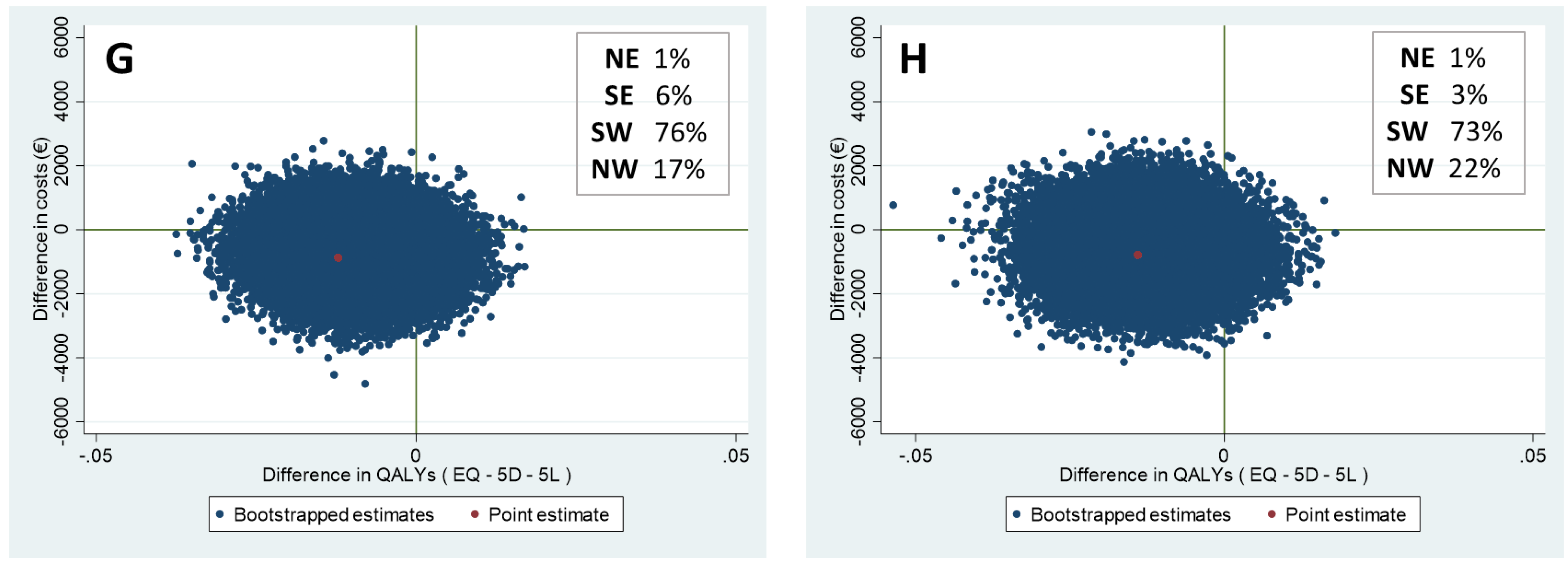
2.6. Statistical Analysis
- Not adjusting the base case analysis for baseline EQ-5D scores and baseline total costs;
- Performing a complete case analysis among patients with complete data at all time-points;
- Including varying intervention costs of Oncokompas (€15 and €100 per user) in the base case analysis;
- Performing the base-case analysis from a healthcare perspective, including only healthcare costs and intervention costs;
- Imputing data for patients who died during the study (to preclude an effect of higher mortality in the intervention group compared to the control group);
- Excluding patients who died during the study (idem).
3. Results
3.1. Study Population
3.2. Costs and Utility Scores at Baseline and Follow-Up
3.3. Cost-Utility Analyses
4. Discussion
Study Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Van Roij, J.; Brom, L.; Youssef-El Soud, M.; van de Poll-Franse, L.; Raijmakers, N.J.H. Social consequences of advanced cancer in patients and their informal caregivers: A qualitative study. Support Care Cancer 2019, 27, 1187–1195. [Google Scholar] [CrossRef] [PubMed]
- Teunissen, S.C.C.M.; Wesker, W.; Kruitwagen, C.; de Haes, H.C.J.M.; Voest, E.E.; de Graeff, A. Symptom Prevalence in Patients with Incurable Cancer: A Systematic Review. J. Pain Symptom Manag. 2007, 34, 94–104. [Google Scholar] [CrossRef] [PubMed]
- Mesquita, A.C.; Chaves, D.C.L.; de Barros, G.A.M. Spiritual needs of patients with cancer in palliative care: An integrative review. Curr. Opin. Support. Palliat. Care 2017, 11, 334–340. [Google Scholar] [CrossRef]
- Aapro, M.; Bossi, P.; Dasari, A.; Fallowfield, L.; Gascón, P.; Geller, M.; Jordan, K.; Kim, J.; Martin, K.; Porzig, S. Digital health for optimal supportive care in oncology: Benefits, limits, and future perspectives. Support. Care Cancer 2020, 28, 4589–4612. [Google Scholar] [CrossRef]
- Widberg, C.; Wiklund, B.; Klarare, A. Patients’ experiences of eHealth in palliative care: An integrative review. BMC Palliat. Care 2020, 19, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Sanyal, C.; Stolee, P.; Juzwishin, D.; Husereau, D. Economic evaluations of eHealth technologies: A systematic review. PLoS ONE 2018, 13, e0198112. [Google Scholar] [CrossRef] [PubMed]
- Lubberding, S.; Van Uden-Kraan, C.F.; Velde, E.A.T.; Cuijpers, P.; Leemans, C.R.; Leeuw, I.M.V.-D. Improving access to supportive cancer care through an eHealth application: A qualitative needs assessment among cancer survivors. J. Clin. Nurs. 2015, 24, 1367–1379. [Google Scholar] [CrossRef] [PubMed]
- Duman-Lubberding, S.; Van Uden-Kraan, C.; Jansen, F.; Witte, B.; Van Der Velden, L.; Lacko, M.; Cuijpers, P.; Leemans, C.; Leeuw, I.V.-D. Feasibility of an eHealth application “OncoKompas” to improve personalized survivorship cancer care. Support. Care Cancer 2015, 24, 2163–2171. [Google Scholar] [CrossRef]
- Hibbard, J.H.; Stockard, J.; Mahoney, E.R.; Tusler, M. Development of the Patient Activation Measure (PAM): Conceptualizing and Measuring Activation in Patients and Consumers. Health Serv. Res. 2004, 39, 1005–1026. [Google Scholar] [CrossRef]
- Schuit, A.S.; Holtmaat, K.; Lissenberg-Witte, B.I.; Eerenstein, S.E.; Zijlstra, J.M.; Eeltink, C.; Becker-Commissaris, A.; van Zuylen, L.; van Linde, M.E.; Oordt, C.W.M.-V.D.H.V.; et al. Efficacy of the eHealth application Oncokompas, facilitating incurably ill cancer patients to self-manage their palliative care needs: A randomized controlled trial. Lancet Reg. Health. Eur. 2022, 18, 100390. [Google Scholar] [CrossRef]
- Jansen, F.; van Zwieten, V.; Coupé, V.M.H.; Leemans, C.R.; Verdonck-de Leeuw, I.M. A Review on Cost-Effectiveness and Cost-Utility of Psychosocial Care in Cancer Patients. Asia-Pacific J. Oncol. Nurs. 2016, 3, 125–136. [Google Scholar] [CrossRef] [PubMed]
- Dieng, M.; Cust, A.E.; Kasparian, N.A.; Mann, G.J.; Morton, R.L. Economic evaluations of psychosocial interventions in cancer: A systematic review. Psychooncology 2016, 25, 1380–1392. [Google Scholar] [CrossRef] [PubMed]
- van der Hout, A.; Jansen, F.; van Uden-Kraan, C.F.; Coupé, V.M.H.; Holtmaat, K.; Nieuwenhuijzen, G.A.; Hardillo, J.A.; Baatenburg de Jong, R.J.; Tiren-Verbeet, N.L.; Sommeijer, D.W.; et al. Cost-utility of an eHealth application ‘Oncokompas’ that supports cancer survivors in self-management: Results of a randomised controlled trial. J. Cancer Surviv. 2021, 15, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Finucane, A.M.; O’Donnell, H.; Lugton, J.; Gibson-Watt, T.; Swenson, C.; Pagliari, C. Digital health interventions in palliative care: A systematic meta-review. NPJ Digit. Med. 2021, 4, 1–10. [Google Scholar]
- Rabarison, K.M.; Bish, C.L.; Massoudi, M.S.; Giles, W.H. Economic Evaluation Enhances Public Health Decision Making. Front. Public Health 2015, 3, 164. [Google Scholar] [CrossRef]
- Bergmo, T.S. How to measure costs and benefits of ehealth interventions: An overview of methods and frameworks. J. Med. Internet Res. 2015, 17, e4521. [Google Scholar] [CrossRef]
- Drummond, M.F.; Sculpher, M.J.; Claxton, K.; Stoddart, G.L.; Torrance, G.W. Methods for the Economic Evaluations of Health Care Programmes, 4th ed.; Oxford University Press: Oxford, UK, 2015. [Google Scholar]
- Whitehead, S.J.; Ali, S. Health outcomes in economic evaluation: The QALY and utilities. Br. Med. Bull. 2010, 96, 5–21. [Google Scholar] [CrossRef]
- Schuit, A.S.; Holtmaat, K.; Hooghiemstra, N.; Jansen, F.; Lissenberg-Witte, B.I.; Coupé, V.M.H.; Van Linde, M.E.; Becker-Commissaris, A.; Reijneveld, J.C.; Zijlstra, J.M.; et al. Efficacy and cost-utility of the eHealth application ‘Oncokompas’, supporting patients with incurable cancer in finding optimal palliative care, tailored to their quality of life and personal preferences: A study protocol of a randomized controlled trial. BMC Palliat. Care 2019, 18, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Bouwmans, C.; Hakkaart-van Roijen, L.; Koopmanschap, M.; Krol, M.; Severens, H.; Brouwer, W. Handleiding iMTA Productivity Cost Questionnaire (iPCQ); iMTA, Erasmus Universiteit: Rotterdam, The Netherlands, 2013. [Google Scholar]
- Bouwmans, C.; Hakkaart-van Roijen, L.; Koopmanschap, M.; Krol, M.; Severens, H.; Brouwer, W. Handleiding iMTA Medical Cost Questionnaire (iMCQ); iMTA, Erasmus Universiteit: Rotterdam, The Netherlands, 2013. [Google Scholar]
- Versteegh, M.M.; Vermeulen, K.M.; Evers, S.M.A.A.; de Wit, G.A.; Prenger, R.; Stolk, E.A. Dutch Tariff for the Five-Level Version of EQ-5D. Value Health 2016, 19, 343–352. [Google Scholar] [CrossRef]
- Hakkaart-van Roijen, L.; van der Linden, N.; Bouwmans, C.; Kanters, T.; Swan Tan, S. Kostenhandleiding: Methodologie van Kostenonderzoek en Referentieprijzen voor Economische Evaluaties in de Gezondheidszorg; Zorginstituut Nederland: Diemen, The Netherlands, 2016; pp. 1–73. Available online: www.zorginstituutnederland.nl/publicaties/publicatie/2016/02/29/richtlijn-voor-het-uitvoeren-van-economische-evaluaties-in-de-gezondheidszorg (accessed on 1 October 2021).
- Kanters, T.A.; Bouwmans-Frijters, C.; Van Der Linden, N.; Tan, S.S.; Roijen, L.H.-V. Update of the Dutch manual for costing studies in health care. PLoS ONE 2017, 12, e0187477. [Google Scholar] [CrossRef]
- IKNL. Cijfers over Kanker. Available online: https://iknl.nl/nkr-cijfers (accessed on 20 March 2022).
- Elliott, R.; Payne, K. Statistical Handling of Data in Economic Analysis Essentials of Economic Evaluation in Healthcare; Pharmaceutical Press: London, UK, 2005. [Google Scholar]
- Smith, S.; Brick, A.; O’Hara, S.; Normand, C. Evidence on the cost and cost-effectiveness of palliative care: A literature review. Palliat. Med. 2014, 28, 130–150. [Google Scholar] [CrossRef] [PubMed]
- Mathew, C.; Hsu, A.T.; Prentice, M.; Lawlor, P.; Kyeremanteng, K.; Tanuseputro, P.; Welch, V. Economic evaluations of palliative care models: A systematic review. Palliat. Med. 2020, 34, 69–82. [Google Scholar] [CrossRef] [PubMed]
- Gardiner, C.; Ingleton, C.; Ryan, T.; Ward, S.; Gott, M. What cost components are relevant for economic evaluations of palliative care, and what approaches are used to measure these costs? A systematic review. Palliat. Med. 2017, 31, 323–337. [Google Scholar] [CrossRef] [PubMed]
- Van Der Hout, A.; van Uden-Kraan, C.F.; Holtmaat, K.; Jansen, F.; Lissenberg-Witte, B.I.; Nieuwenhuijzen, G.A.P.; Hardillo, J.A.; Baatenburg de Jong, R.J.; Tiren-Verbeet, N.L.; Sommeijer, D.W.; et al. Role of eHealth application Oncokompas in supporting self-management of symptoms and health-related quality of life in cancer survivors: A randomised, controlled trial. Lancet Oncol. 2020, 21, 80–94. [Google Scholar] [CrossRef]
- Gomes, B.; Harding, R.; Foley, K.M.; Higginson, I.J. Optimal Approaches to the Health Economics of Palliative Care: Report of an International Think Tank. J. Pain Symptom Manag. 2009, 38, 4–10. [Google Scholar] [CrossRef]
- Round, J. Is a QALY still a QALY at the end of life? J. Health Econ. 2012, 31, 521–527. [Google Scholar] [CrossRef]
- King, M.T.; Costa, D.S.; Aaronson, N.K.; Brazier, J.E.; Cella, D.F.; Fayers, P.M.; Grimison, P.; Janda, M.; Kemmler, G.; Norman, R.; et al. QLU-C10D: A health state classification system for a multi-attribute utility measure based on the EORTC QLQ-C30. Qual. Life Res. 2016, 25, 625–636. [Google Scholar] [CrossRef]
- Turnpenny, A.; Caiels, J.; Whelton, B.; Richardson, L.; Beadle-Brown, J.; Crowther, T.; Forder, J.; Apps, J.; Rand, S. Developing an Easy Read Version of the Adult Social Care Outcomes Toolkit (ASCOT). J. Appl. Res. Intellect. Disabil. 2016, 31, e36–e48. [Google Scholar] [CrossRef]
- van Loon, M.S.; van Leeuwen, K.M.; Ostelo, R.W.J.G.; Bosmans, J.E.; Widdershoven, G.A.M. Quality of life in a broader perspective: Does ASCOT reflect the capability approach? Qual. Life Res. 2018, 27, 1181–1189. [Google Scholar] [CrossRef]
- Jönsson, B. Editorial: Ten arguments for a societal perspective in the economic evaluation of medical innovations. Eur. J. Health Econ. 2009, 10, 357–359. [Google Scholar] [CrossRef]
- Gardiner, C.; Robinson, J.; Connolly, M.; Hulme, C.; Kang, K.; Rowland, C.; Larkin, P.; Meads, D.; Morgan, T.; Gott, M. Equity and the financial costs of informal caregiving in palliative care: A critical debate. BMC Palliat. Care 2020, 19, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Coumoundouros, C.; Brahim, L.O.; Lambert, S.D.; McCusker, J. The direct and indirect financial costs of informal cancer care: A scoping review. Health. Soc. Care Community 2019, 27, e622–e636. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Total Group (n = 138) | Control Group (n = 69) | Intervention Group (n = 69) | p-Value | |||||
|---|---|---|---|---|---|---|---|---|
| Number | % | Number | % | Number | % | |||
| Age in years | 0.29 | |||||||
| Mean (SD) | 61.1 (12.3) | - | 62.3 (11.9) | - | 60.0 (12.7) | - | ||
| IQR | 53–70.3 | - | 54.5–71.5 | - | 51.0–68.5 | - | ||
| Gender | 1.00 | |||||||
| Male | 74 | 55% | 37 | 54% | 37 | 54% | ||
| Female | 64 | 45% | 32 | 46% | 32 | 46% | ||
| Education level | 0.61 | |||||||
| Low/medium/unknown | 73 | 53% | 38 | 55% | 35 | 51% | ||
| High | 65 | 47% | 31 | 45% | 34 | 49% | ||
| Living situation * | 0.38 | |||||||
| Living alone | 28 | 20% | 16 | 24% | 12 | 17% | ||
| Living with kids/partner | 109 | 80% | 52 | 77% | 57 | 83% | ||
| Marital status | 0.82 | |||||||
| Partner | 115 | 83% | 57 | 83% | 58 | 84% | ||
| No partner | 23 | 17% | 12 | 17% | 11 | 16% | ||
| Children | 0.69 | |||||||
| Yes | 106 | 77% | 54 | 79% | 52 | 75% | ||
| No | 32 | 23% | 15 | 22% | 17 | 25% | ||
| Employment | 0.38 | |||||||
| Yes | 51 | 37% | 28 | 41% | 23 | 33% | ||
| Absent from work > 3 months | 29 | 57% | 17 | 61% | 12 | 52% | ||
| No | 87 | 63% | 41 | 59% | 46 | 67% | ||
| Tumor type | 0.83 | |||||||
| Brain tumor | 39 | 29% | 22 | 32% | 17 | 25% | ||
| Gastro-intestinal cancer | 19 | 14% | 10 | 15% | 9 | 13% | ||
| Lung cancer | 17 | 12% | 8 | 12% | 8 | 12% | ||
| Hematological cancer | 16 | 12% | 8 | 12% | 8 | 12% | ||
| Head and neck cancer | 16 | 12% | 7 | 10% | 9 | 13% | ||
| Breast cancer | 15 | 11% | 5 | 7% | 10 | 15% | ||
| Urological cancer | 10 | 7% | 6 | 9% | 4 | 6% | ||
| Other | 4 | 3% | 1 | 1% | 3 | 6% | ||
| Multiple primaries a | 3 | 2% | 2 | 3% | 1 | 1% | ||
| Treatment | 0.55 | |||||||
| No treatment b | 12 | 9% | 7 | 10% | 5 | 7% | ||
| Single, multiple or multimodal treatment | 126 | 91% | 62 | 90% | 64 | 93% | ||
| Comorbidities | 0.43 | |||||||
| None or one comorbidity | 104 | 75% | 54 | 78% | 50 | 73% | ||
| Multiple comorbidities | 34 | 25% | 15 | 22% | 19 | 28% | ||
| Baseline (t0) | 3-Months Follow-Up (t2) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention (N = 69) | Control (N = 69) | Intervention (N = 60) | Control (N = 61) | |||||||
| Price * | Mean | (SD) | Mean | (SD) | Mean | (SD) | Mean | (SD) | ||
| Healthcare costs | 3463 | (3576) | 4771 | (6112) | 2589 | (2458) | 3660 | (4427) | ||
| General practitioner | ||||||||||
| Phone | 18 | 39 | (38) | 39 | (42) | 35 | (42) | 34 | (34) | |
| Home visit | 53 | 16 | (43) | 30 | (68) | 18 | (46) | 25 | (59) | |
| Consultation at practice | 35 | 53 | (64) | 40 | (58) | 40 | (60) | 40 | (55) | |
| Company doctor | 73 | 28 | (60) | 29 | (69) | 30 | (62) | 23 | (53) | |
| Social worker | 69 | 19 | (64) | 24 | (72) | 17 | (62) | 7 | (24) | |
| Physiotherapist | 35 | 172 | (293) | 69 | (169) | 155 | (203) | 104 | (229) | |
| Ergotherapist | 35 | 9 | (39) | 3 | (18) | 3 | (12) | 3 | (16) | |
| Dietitian | 32 | 16 | (35) | 27 | (62) | 12 | (28) | 14 | (44) | |
| Speech therapist | 32 | 2 | (13) | 4 | (20) | 1 | (6) | 3 | (21) | |
| Oral hygienist | 27 | 5 | (11) | 6 | (11) | 5 | (10) | 4 | (10) | |
| Psychologist/psychiatrist ** | 100–131 | 109 | (248) | 58 | (171) | 66 | (174) | 90 | (207) | |
| Medical specialist | ||||||||||
| General hospital | 85 | 25 | (76) | 38 | (134) | 37 | (109) | 21 | (72) | |
| Academic hospital | 174 | 754 | (788) | 1019 | (1249) | 696 | (735) | 796 | (773) | |
| Spiritual counsellor | 137 | 20 | (95) | 24 | (97) | 14 | (65) | 22 | (101) | |
| Home-care (cleaning) | 21 | 50 | (184) | 16 | (131) | 97 | (259) | 9 | (70) | |
| Personal care | 53 | 48 | (265) | 11 | (63) | 25 | (121) | 126 | (970) | |
| Nursing care | 78 | 43 | (177) | 392 | (2346) | 39 | (264) | 348 | (1743) | |
| Emergency care visit | 277 | 72 | (194) | 100 | (232) | 83 | (193) | 59 | (125) | |
| Ambulance to hospital | 550 | 40 | (144) | 56 | (285) | 55 | (195) | 36 | (137) | |
| Day treatment | ||||||||||
| Hospital | 324 | 1226 | (2108) | 1493 | (2482) | 718 | (1378) | 1392 | (2403) | |
| Care centre *** | 72–327 | 0 | (0) | 0 | (0) | 0 | (0) | 0 | (0) | |
| Admission | ||||||||||
| Hospital | 508 | 611 | (1757) | 1230 | (3180) | 322 | (944) | 425 | (1296) | |
| Care center *** | 179–491 | 0 | (0) | 0 | (0) | 0 | (0) | 0 | (0) | |
| Supportive care **** | From 15–67 | 105 | (320) | 51 | (192) | 114 | (320) | 50 | (187) | |
| Costs for patients and their families | 657 | (1504) | 462 | (891) | 780 | (2866) | 856 | (2489) | ||
| Transport and parking costs ***** | 0–9 | 71 | (62) | 82 | (80) | 57 | (45) | 71 | (69) | |
| Alternative treatment | 65 | 2 | (16) | 12 | (66) | 7 | (50) | 30 | (140) | |
| Informal care | 15 | 586 | (1499) | 379 | (882) | 723 | (2865) | 784 | (2469) | |
| Other costs (i.e., productivity losses) | 358 | (1666) | 273 | (1143) | 334 | (2551) | 291 | (1129) | ||
| Absenteeism paid work | 38/hour | 355 | (1666) | 272 | (1143) | 329 | (2551) | 287 | (1113) | |
| Presenteeism paid work | 38/hour | 4 | (20) | 1 | (11) | 5 | (37) | 4 | (25) | |
| TOTAL COSTS | 4479 | (4933) | 5506 | (6521) | 3703 | (4495) | 4806 | (5525) | ||
| Time Point | N | Control Group Mean (SD) | Intervention Group Mean (SD) |
|---|---|---|---|
| EQ-5D | |||
| Baseline (t0) | 138 | 0.79 (0.17) | 0.76 (0.18) |
| 3 months follow-up (t2) | 121 | 0.80 (0.18) | 0.74 (0.21) |
| Costs (€) | QALYs | Incremental Costs | Incremental Effects | ||||
|---|---|---|---|---|---|---|---|
| Group | N | Mean (SEM) | Mean (SEM) | € | 95% CI | QALYs | 95% CI |
| Base case analysis * | −806 | [−2453 to 674] | −0.01 | [−0.03 to 0.001] | |||
| - Control group | 69 | NA | NA | ||||
| - Intervention group | 69 | NA | NA | ||||
| Sensitivity analyses ** | |||||||
| Base case analysis with no correction for baseline EQ-5D and costs | −990 | [−2690 to 594] | −0.02 | [−0.04 to −0.001] *** | |||
| - Control group | 69 | 4590 (689) | 0.20 (0.01) | ||||
| - Intervention group | 69 | 3600 (575) | 0.17 (0.01) | ||||
| Complete case analysis | −611 | [−2384 to 947] | −0.01 | [−0.03 to −0.001] *** | |||
| - Control group | 61 | NA | NA | ||||
| - Intervention group | 60 | NA | NA | ||||
| Analysis with differing intervention costs | |||||||
| €15 | −816 | [−2469 to 690] | −0.01 | [−0.03 to 0.001] | |||
| - Control group | 69 | NA | NA | ||||
| - Intervention group | 69 | NA | NA | ||||
| €100 | −731 | [−2400 to 798] | −0.01 | [−0.03 to 0.001] | |||
| - Control group | 69 | NA | NA | ||||
| - Intervention group | 69 | NA | NA | ||||
| Analysis from healthcare perspective | −401 | [−1393 to 472] | −0.02 | [−0.03 to 0.000] | |||
| - Control group | 69 | NA | NA | ||||
| - Intervention group | 69 | NA | NA | ||||
| Analysis with imputed data for patients who died during the study | −871 | [−2489 to 565] | −0.01 | [−0.03 to 0.003] | |||
| - Control group | 69 | NA | NA | ||||
| - Intervention group | 69 | NA | NA | ||||
| Analysis excluding patients who died during the study | −778 | [−2430 to 742] | −0.01 | [−0.03 to 0.001] | |||
| - Control group | 68 | NA | NA | ||||
| - Intervention group | 66 | NA | NA | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schuit, A.S.; Holtmaat, K.; Coupé, V.M.H.; Eerenstein, S.E.J.; Zijlstra, J.M.; Eeltink, C.; Becker-Commissaris, A.; van Zuylen, L.; van Linde, M.E.; Menke-van der Houven van Oordt, C.W.; et al. Cost-Utility of the eHealth Application ‘Oncokompas’, Supporting Incurably Ill Cancer Patients to Self-Manage Their Cancer-Related Symptoms: Results of a Randomized Controlled Trial. Curr. Oncol. 2022, 29, 6186-6202. https://doi.org/10.3390/curroncol29090486
Schuit AS, Holtmaat K, Coupé VMH, Eerenstein SEJ, Zijlstra JM, Eeltink C, Becker-Commissaris A, van Zuylen L, van Linde ME, Menke-van der Houven van Oordt CW, et al. Cost-Utility of the eHealth Application ‘Oncokompas’, Supporting Incurably Ill Cancer Patients to Self-Manage Their Cancer-Related Symptoms: Results of a Randomized Controlled Trial. Current Oncology. 2022; 29(9):6186-6202. https://doi.org/10.3390/curroncol29090486
Chicago/Turabian StyleSchuit, Anouk S., Karen Holtmaat, Veerle M. H. Coupé, Simone E. J. Eerenstein, Josée M. Zijlstra, Corien Eeltink, Annemarie Becker-Commissaris, Lia van Zuylen, Myra E. van Linde, C. Willemien Menke-van der Houven van Oordt, and et al. 2022. "Cost-Utility of the eHealth Application ‘Oncokompas’, Supporting Incurably Ill Cancer Patients to Self-Manage Their Cancer-Related Symptoms: Results of a Randomized Controlled Trial" Current Oncology 29, no. 9: 6186-6202. https://doi.org/10.3390/curroncol29090486
APA StyleSchuit, A. S., Holtmaat, K., Coupé, V. M. H., Eerenstein, S. E. J., Zijlstra, J. M., Eeltink, C., Becker-Commissaris, A., van Zuylen, L., van Linde, M. E., Menke-van der Houven van Oordt, C. W., Sommeijer, D. W., Verbeek, N., Bosscha, K., Nandoe Tewarie, R., Sedee, R.-J., de Bree, R., de Graeff, A., de Vos, F., Cuijpers, P., ... Jansen, F. (2022). Cost-Utility of the eHealth Application ‘Oncokompas’, Supporting Incurably Ill Cancer Patients to Self-Manage Their Cancer-Related Symptoms: Results of a Randomized Controlled Trial. Current Oncology, 29(9), 6186-6202. https://doi.org/10.3390/curroncol29090486






