A Scoping Review on Outcomes and Outcome Measurement Instruments in Rehabilitative Interventions for Patients with Haematological Malignancies Treated with Allogeneic Stem Cell Transplantation
Abstract
1. Introduction
1.1. Rationale
1.2. Objectives
2. Methods
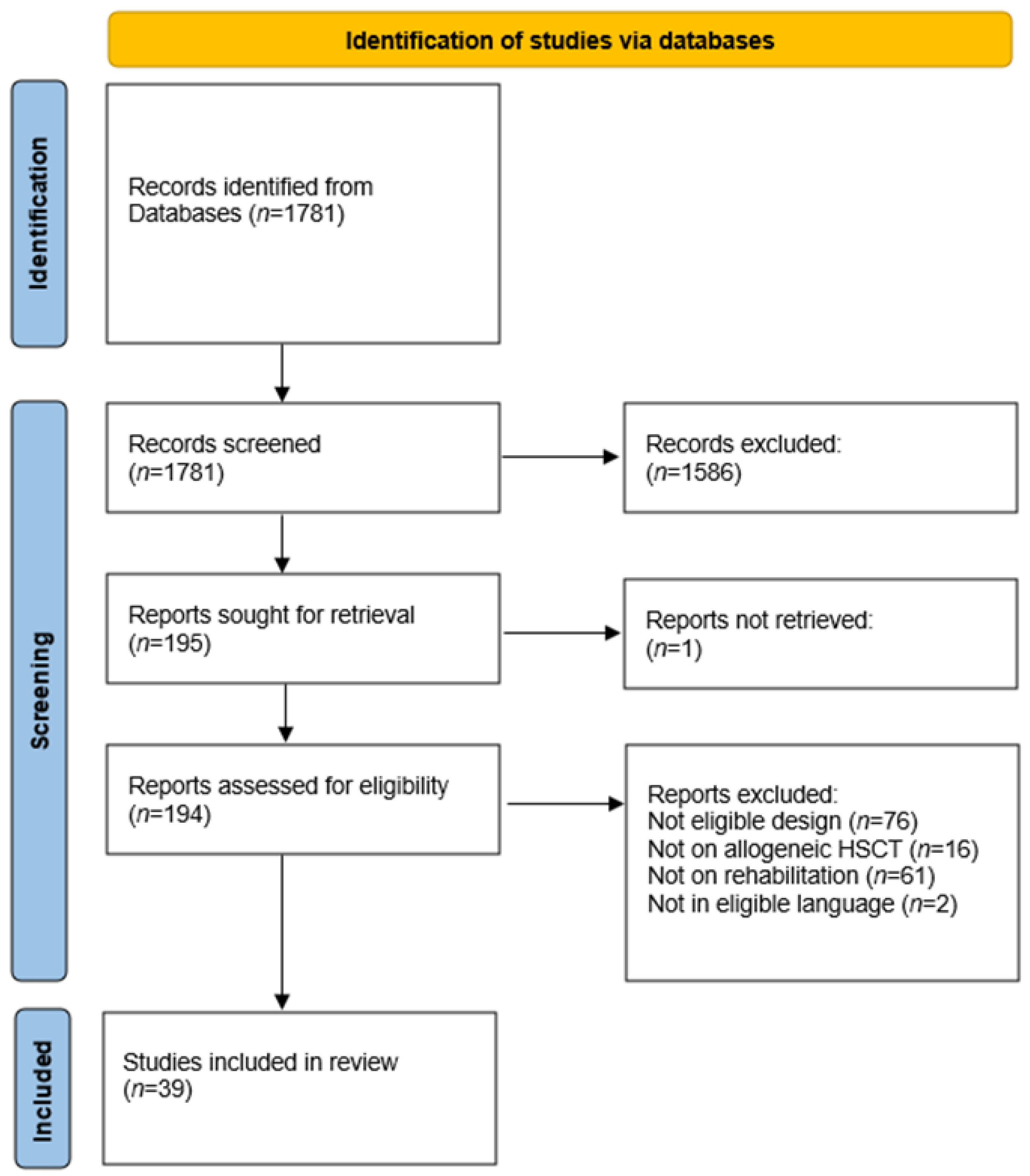
2.1. Data Sources and Study Selection
2.2. Data Extraction, Data Synthesis and Analysis
3. Results
3.1. Core Area Feasibility
3.2. Core Area Life Impact
3.3. Core Area Pathophysiology
3.4. Timing of Measurement
4. Discussion
5. Outcome Excess and Inconsistent Use
6. Outcome Measurement Instrument Excess and Inconsistent Use
7. Timing and Setting of Measurement Inconsistency
8. Allogeneic HSCT vs. HSCT Population
9. Limitations
10. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| HSCT | Hematopoietic Stem Cell Transplantation |
| GvHD | Graft Versus Host Disease |
| IST | Immunosuppressive Therapy |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| EORTC | European Organization for Research and Treatment of Cancer |
| COS | Core Outcome Set |
| IRT | Item Response Theory |
| PROMIS | Patient-Reported Outcomes Measurement Information System |
| FACT | Functional Assessment of Cancer Therapy |
| EBMT | European Society for Blood and Marrow Transplantation |
References
- Majhail, N.S.; Farnia, S.H.; Carpenter, P.A.; Champlin, R.E.; Crawford, S.; Marks, D.I.; Omel, J.L.; Orchard, P.J.; Palmer, J.; Saber, W.; et al. Indications for Autologous and Allogeneic Hematopoietic Cell Transplantation: Guidelines from the American Society for Blood and Marrow Transplantation. Biol. Blood Marrow Transplant. 2015, 21, 1863–1869. [Google Scholar] [CrossRef] [PubMed]
- Copelan, E.A. Hematopoietic stem-cell transplantation. N. Engl. J. Med. 2006, 354, 1813–1826. [Google Scholar] [CrossRef] [PubMed]
- Ghimire, S.; Weber, D.; Mavin, E.; Wang, X.N.; Dickinson, A.M.; Holler, E. Pathophysiology of GvHD and Other HSCT-Related Major Complications. Front. Immunol. 2017, 8, 79. [Google Scholar] [CrossRef] [PubMed]
- Kurosawa, S.; Yamaguchi, T.; Mori, T.; Kanamori, H.; Onishi, Y.; Emi, N.; Fujisawa, S.; Kohno, A.; Nakaseko, C.; Saito, B.; et al. Patient-reported quality of life after allogeneic hematopoietic cell transplantation or chemotherapy for acute leukemia. Bone Marrow Transplant. 2015, 50, 1241–1249. [Google Scholar] [CrossRef]
- Sorror, M.; Storer, B.; Sandmaier, B.M.; Maloney, D.G.; Chauncey, T.R.; Langston, A.; Maziarz, R.T.; Pulsipher, M.; McSweeney, P.A.; Storb, R. Hematopoietic cell transplantation-comorbidity index and Karnofsky performance status are independent predictors of morbidity and mortality after allogeneic nonmyeloablative hematopoietic cell transplantation. Cancer 2008, 112, 1992–2001. [Google Scholar] [CrossRef]
- Wade, D.T. What is rehabilitation? An empirical investigation leading to an evidence-based description. Clin. Rehabil. 2020, 34, 571–583. [Google Scholar] [CrossRef]
- Morishita, S.; Tsubaki, A.; Hotta, K.; Fu, J.; Fujii, S. The benefit of exercise in patients who undergo allogeneic hematopoietic stem cell transplantation. J. Int. Soc. Phys. Rehabil. Med. 2019, 2, 54–61. [Google Scholar] [CrossRef]
- Inoue, J.; Ono, R.; Okamura, A.; Matsui, T.; Takekoshi, H.; Miwa, M.; Kurosaka, M.; Saura, R.; Shimada, T. The impact of early rehabilitation on the duration of hospitalization in patients after allogeneic hematopoietic stem cell transplantation. Transplant. Proc. 2010, 42, 2740–2744. [Google Scholar] [CrossRef]
- Cunningham, B.A.; Morris, G.; Cheney, C.L.; Buergel, N.; Aker, S.N.; Lenssen, P. Effects of resistive exercise on skeletal muscle in marrow transplant recipients receiving total parenteral nutrition. J. Parenter. Enter. Nutr. 1986, 10, 558–563. [Google Scholar] [CrossRef]
- Mohananey, D.; Sarau, A.; Kumar, R.; Lewandowski, D.; Abreu-Sosa, S.M.; Nathan, S.; Okwuosa, T.M. Role of Physical Activity and Cardiac Rehabilitation in Patients Undergoing Hematopoietic Stem Cell Transplantation. JACC Cardio Oncol. 2021, 3, 17–34, Published 2021 Mar 16. [Google Scholar] [CrossRef]
- Persoon, S.; Kersten, M.; Van der Weiden, K.; Buffart, L.; Nollet, F.; Brug, J.; Chinapaw, M. Effects of exercise in patients treated with stem cell transplantation for a hematologic malignancy: A systematic review and meta-analysis. Cancer Treat. Rev. 2013, 39, 682–690. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, B.R.; Califf, R.M.; Cheng, S.K.; Tasneem, A.; Horton, J.; Chiswell, K.; Schulman, K.A.; Dilts, D.M.; Abernethy, A.P. Characteristics of oncology clinical trials: Insights from a systematic analysis of ClinicalTrials.gov. JAMA Intern. Med. 2013, 173, 972–979. [Google Scholar] [CrossRef] [PubMed]
- Boers, M.; Beaton, D.E.; Shea, B.J.; Maxwell, L.J.; Bartlett, S.J.; Bingham, C.O., III; Conaghan, P.G.; D’Agostino, M.A.; de Wit, M.P.; Gossec, L.; et al. OMERACT Filter 2.1: Elaboration of the Conceptual Framework for Outcome Measurement in Health Intervention Studies. J. Rheumatol. 2019, 46, 1021–1027. [Google Scholar] [CrossRef]
- El-Kotob, R.; Giangregorio, L.M. Pilot and feasibility studies in exercise, physical activity, or rehabilitation research. Pilot Feasibility Study 2018, 4, 137. [Google Scholar] [CrossRef]
- Thabane, L.; Ma, J.; Chu, R.; Cheng, J.; Ismaila, A.; Rios, L.P.; Robson, R.; Thabane, M.; Giangregorio, L.; Goldsmith, C.H. A tutorial on pilot studies: The what, why and how. BMC Med. Res. Methodol. 2010, 10, 1. [Google Scholar] [CrossRef]
- Santa Mina, D.; Dolan, L.B.; Lipton, J.H.; Au, D.; Camacho Pérez, E.; Franzese, A.; Alibhai, S.M.; Jones, J.M.; Chang, E. Exercise before, during, and after Hospitalization for Allogeneic Hematological Stem Cell Transplant: A Feasibility Randomized Controlled Trial. J. Clin. Med. 2020, 9, 14. [Google Scholar] [CrossRef]
- Schuler, M.K.; Hornemann, B.; Pawandenat, C.; Kramer, M.; Hentschel, L.; Beck, H.; Kasten, P.; Singer, S.; Schaich, M.; Ehninger, G.; et al. Feasibility of an exercise programme in elderly patients undergoing allogeneic stem cell transplantation—A pilot study. Eur. J. Cancer Care 2016, 25, 839–848. [Google Scholar] [CrossRef]
- Bewarder, M.; Klostermann, A.; Ahlgrimm, M.; Bittenbring, J.T.; Pfreundschuh, M.; Wagenpfeil, S.; Kaddu-Mulindwa, D. Safety and feasibility of electrical muscle stimulation in patients undergoing autologous and allogeneic stem cell transplantation or intensive chemotherapy. Support. Care Cancer 2019, 27, 1013–1020. [Google Scholar] [CrossRef]
- Lu, D.F.; Hart, L.K.; Lutgendorf, S.K.; Oh, H.; Silverman, M. Effects of healing touch and relaxation therapy on adult patients undergoing hematopoietic stem cell transplant: A feasibility pilot study. Cancer Nurs. 2016, 39, E1–E11. [Google Scholar] [CrossRef]
- De Almeida, L.B.; Trevizan, P.F.; Laterza, M.C.; Hallack Neto, A.E.; Perrone, A.; Martinez, D.G. Safety and feasibility of inspiratory muscle training for hospitalized patients undergoing hematopoietic stem cell transplantation: A randomized controlled study. Support. Care Cancer 2020, 28, 3627–3635. [Google Scholar] [CrossRef]
- Wilson, R.W.; Jacobsen, P.B.; Fields, K.K. Pilot study of a home-based aerobic exercise program for sedentary cancer survivors treated with hematopoietic stem cell transplantation. Bone Marrow Transplant. 2005, 35, 721–727. [Google Scholar] [CrossRef] [PubMed]
- Baydoun, M.; Barton, D.L.; Peterson, M.; Wallner, L.P.; Visovatti, M.A.; Arslanian-Engoren, C.; Choi, S.W. Yoga for Cancer-Related Fatigue in Survivors of Hematopoietic Cell Transplantation: A Feasibility Study. J. Pain Symptom Manag. 2020, 59, 702–708. [Google Scholar] [CrossRef] [PubMed]
- Schumacher, H.; Stüwe, S.; Kropp, P.; Diedrich, D.; Freitag, S.; Greger, N.; Junghanss, C.; Freund, M.; Hilgendorf, I. A prospective, randomized evaluation of the feasibility of exergaming on patients undergoing hematopoietic stem cell transplantation. Bone Marrow Transplant. 2018, 53, 584–590. [Google Scholar] [CrossRef]
- Amonoo, H.L.; Kurukulasuriya, C.; Chilson, K.; Onstad, L.; Huffman, J.C.; Lee, S.J. Improving Quality of Life in Hematopoietic Stem Cell Transplantation Survivors Through a Positive Psychology Intervention. Biol. Blood Marrow Transplant. 2020, 26, 1144–1453. [Google Scholar] [CrossRef] [PubMed]
- Rupnik, E.; Skerget, M.; Sever, M.; Zupan, I.P.; Ogrinec, M.; Ursic, B.; Kos, N.; Cernelc, P.; Zver, S. Feasibility and safety of exercise training and nutritional support prior to haematopoietic stem cell transplantation in patients with haematologic malignancies. BMC Cancer 2020, 20, 1142. [Google Scholar] [CrossRef] [PubMed]
- Peters, T.; Erdmann, R.; Hacker, E.D. Exercise Intervention: Attrition, Compliance, Adherence, and Progression Following Hematopoietic Stem Cell Transplantation. Clin. J. Oncol. Nurs. 2018, 22, 97–103. [Google Scholar] [CrossRef]
- Fioritto, A.P.; Oliveira, C.C.; Albuquerque, V.S.; Almeida, L.B.; Granger, C.L.; Denehy, L.; Malaguti, C. Individualized in-hospital exercise training program for people undergoing hematopoietic stem cell transplantation: A feasibility study. Disabil. Rehabil. 2019, 43, 386–392. [Google Scholar] [CrossRef]
- Carlson, L.E.; Smith, D.; Russell, J.; Fibich, C.; Whittaker, T. Individualized exercise program for the treatment of severe fatigue in patients after allogeneic hematopoietic stem-cell transplant: A pilot study. Bone Marrow Transplant. 2006, 37, 945–954. [Google Scholar] [CrossRef]
- Shleton, M.L.; Lee, J.Q.; Morris, S.; Massey, P.R.; Kendall, D.G.; Munsell, M.F. A randomized control trial of a supervised versus a self-directed exercise program for allogenic stem cell transplant patients. Psycho-Oncology 2009, 18, 353–359. [Google Scholar] [CrossRef]
- Pahl, A.; Wehrle, A.; Kneis, S.; Gollhofer, A.; Bertz, H. Whole body vibration training during allogeneic hematopoietic cell transplantation-the effects on patients’ physical capacity. Ann. Hematol. 2020, 99, 635–648. [Google Scholar] [CrossRef]
- Jarden, M.; Nelausen, K.; Boesen, E.; Hovgaard, D.; Adamsen, L. The effect of a multimodal intervention on treatment-related symptoms in patients undergoing hematopoietic stem cell transplantation: A randomized controlled trial. J. Pain Symptom Manag. 2009, 38, 174–190. [Google Scholar] [CrossRef] [PubMed]
- Bargi, G.; Guclu, M.B.; Aribas, Z.; Aki, S.Z.; Sucak, G.T. Inspiratory muscle training in allogeneic hematopoietic stem cell transplantation recipients: A randomized controlled trial. Support. Care Cancer 2016, 24, 647–659. [Google Scholar] [CrossRef]
- Kim, S.D.; Kim, H.S. Effects of a relaxation breathing exercise on fatigue in haemopoietic stem cell transplantation patients. J. Clin. Nurs. 2005, 14, 51–55. [Google Scholar] [CrossRef]
- Baumann, F.T.; Kraut, L.; Schule, K.; Bloch, W.; Fauser, A.A. A controlled randomized study examining the effects of exercise therapy on patients undergoing haematopoietic stem cell transplantation. Bone Marrow Transplant. 2010, 45, 355–362. [Google Scholar] [CrossRef]
- Lounsberry, J.J.; Macrae, H.; Angen, M.; Hoeber, M.; Carlson, L.E. Feasibility study of a telehealth delivered, psychoeducational support group for allogeneic hematopoietic stem cell transplant patients. Psycho-Oncology 2010, 19, 777–781. [Google Scholar] [CrossRef] [PubMed]
- Kaeding, T.S.; Frimmel, M.; Treondlin, F.; Jung, K.; Jung, W.; Wulf, G.; Trümper, L.; Hasenkamp, J. Whole-body vibration training as a supportive therapy during allogeneic haematopoietic stem cell transplantation—A randomised controlled trial. Eur. Oncol. Haematol. 2018, 14, 33–39. [Google Scholar] [CrossRef]
- Wiskemann, J.; Dreger, P.; Schwerdtfeger, R.; Bondong, A.; Huber, G.; Kleindienst, N.; Ulrich, C.M.; Bohus, M. Effects of a partly self-administered exercise program before, during, and after allogeneic stem cell transplantation. Blood 2011, 117, 2604–2613. [Google Scholar] [CrossRef]
- Doro, C.A.; Neto, J.Z.; Cunha, R.; Doro, M.P. Music therapy improves the mood of patients undergoing hematopoietic stem cells transplantation (controlled randomized study). Support. Care Cancer 2017, 25, 1013–1018. [Google Scholar] [CrossRef]
- Jafari, H.; Janati, Y.; Yazdani, J.; Bali, N.; Hassanpour, S. The Effect of Relaxation Technique on Fatigue Levels after Stem Cell Transplant. Iran. J. Nurs. Midwifery Res. 2018, 23, 388–394. [Google Scholar]
- Hacker, E.D.; Collins, E.; Park, C.; Peters, T.; Patel, P.; Rondelli, D. Strength Training to Enhance Early Recovery after Hematopoietic Stem Cell Transplantation. Biol. Blood Marrow Transplant. 2017, 23, 659–669. [Google Scholar] [CrossRef]
- Knols, R.H.; de Bruin, E.D.; Uebelhart, D.; Aufdemkampe, G.; Schanz, U.; Stenner-Liewen, F.; Hitz, F.; Taverna, C.; Aaronson, N.K. Effects of an outpatient physical exercise program on hematopoietic stem-cell transplantation recipients: A randomized clinical trial. Bone Marrow Transplant. 2011, 46, 1245–1255. [Google Scholar] [CrossRef] [PubMed]
- Bird, L.; Arthur, A.; Niblock, T.; Stone, R.; Watson, L.; Cox, K. Rehabilitation programme after stem cell transplantation: Randomized controlled trial. J. Adv. Nurs. 2010, 66, 607–615. [Google Scholar] [CrossRef] [PubMed]
- Grossman, P.; Zwahlen, D.; Halter, J.P.; Passweg, J.R.; Steiner, C.; Kiss, A. A mindfulness-based program for improving quality of life among hematopoietic stem cell transplantation survivors: Feasibility and preliminary findings. Support. Care Cancer 2015, 23, 1105–1112. [Google Scholar] [CrossRef] [PubMed]
- McCabe, C.; Roche, D.; Hegarty, F.; McCann, S. ‘Open Window’: A randomized trial of the effect of new media art using a virtual window on quality of life in patients’ experiencing stem cell transplantation. Psycho-Oncology 2013, 22, 330–337. [Google Scholar] [CrossRef]
- El-Jawahri, A.; Traeger, L.; Greer, J.A.; VanDusen, H.; Fishman, S.R.; LeBlanc, T.W.; Pirl, W.F.; Jackson, V.A.; Telles, J.; Rhodes, A.; et al. Effect of inpatient palliative care during hematopoietic stem-cell transplant on psychological distress 6 months after transplant: Results of a randomized clinical trial. J. Clin. Oncol. 2017, 35, 3714–3721. [Google Scholar] [CrossRef]
- Balck, F.; Zschieschang, A.; Zimmermann, A.; Ordemann, R. A randomized controlled trial of problem-solving training (PST) for hematopoietic stem cell transplant (HSCT) patients: Effects on anxiety, depression, distress, coping and pain. J. Psychosoc. Oncol. 2019, 37, 541–556. [Google Scholar] [CrossRef]
- Potiaumpai, M.; Cutrono, S.; Medina, T.; Koeppel, M.; Pereira, D.L.; Pirl, W.F.; Jacobs, K.A.; Eltoukhy, M.; Signorile, J.F. Multidirectional Walking in Hematopoietic Stem Cell Transplant Patients. Med. Sci. Sports Exerc. 2021, 53, 258–266. [Google Scholar] [CrossRef]
- DuHamel, K.N.; Mosher, C.E.; Winkel, G.; Labay, L.E.; Rini, C.; Meschian, Y.M.; Austin, J.; Greene, P.B.; Lawsin, C.R.; Rusiewicz, A.; et al. Randomized clinical trial of telephone-administered cognitive-behavioral therapy to reduce post-traumatic stress disorder and distress symptoms after hematopoietic stem-cell transplantation. J. Clin. Oncol. 2010, 28, 3754–3761. [Google Scholar] [CrossRef]
- Applebaum, A.J.; DuHamel, K.N.; Winkel, G.; Rini, C.; Greene, P.B.; Mosher, C.E.; Redd, W.H. Therapeutic alliance in telephone-administered cognitive-behavioral therapy for hematopoietic stem cell transplant survivors. J. Consult. Clin. Psychol. 2012, 80, 811–816. [Google Scholar] [CrossRef]
- Jacobsen, P.B.; Le-Rademacher, J.; Jim, H.; Syrjala, K.; Wingard, J.R.; Logan, B.; Wu, J.; Majhail, N.S.; Wood, W.; Rizzo, J.D.; et al. Exercise and stress management training prior to hematopoietic cell transplantation: Blood and Marrow Transplant Clinical Trials Network (BMT CTN) 0902. Biol. Blood Marrow Transplant. 2014, 20, 1530–1536. [Google Scholar] [CrossRef]
- Baumann, F.T.; Zopf, E.M.; Nykamp, E.; Kraut, L.; Schüle, K.; Elter, T.; Fauser, A.A.; Bloch, W. Physical activity for patients undergoing an allogeneic hematopoietic stem cell transplantation: Benefits of a moderate exercise intervention. Eur. J. Haematol. 2011, 87, 148–156. [Google Scholar] [CrossRef] [PubMed]
- DeFor, T.E.; Burns, L.J.; Gold, E.M.; Weisdorf, D.J. A randomized trial of the effect of a walking regimen on the functional status of 100 adult allogeneic donor hematopoietic cell transplant patients. Biol. Blood Marrow Transplant. 2007, 13, 948–955. [Google Scholar] [CrossRef] [PubMed]
- Wood, W.A.; Phillips, B.; Smith-Ryan, A.E.; Wilson, D.; Deal, A.M.; Bailey, C.; Meeneghan, M.; Reeve, B.B.; Basch, E.M.; Bennett, A.V.; et al. Personalized home-based interval exercise training may improve cardiorespiratory fitness in cancer patients preparing to undergo hematopoietic cell transplantation. Bone Marrow Transplant. 2016, 51, 967–972. [Google Scholar] [CrossRef] [PubMed]
- Bom, E.A.; de Souza, C.V.; Thiesen, R.A.; Miranda, E.C.; de Souza, C.A. Evaluation of respiratory conditions in early phase of hematopoietic stem cell transplantation. Rev. Bras. Hematol. Hemoter. 2012, 34, 188–192. [Google Scholar] [CrossRef][Green Version]
- Fayers, P.; Bottomley, A.; on behalf of the EORTC Quality of Life Group and of the Quality of Life Unit. Quality of life research within the EORTC-the EORTC QLQ-C30. European Organisation for Research and Treatment of Cancer. Eur. J. Cancer 2002, 38 (Suppl. 4), S125–S133. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Williamson, P.R.; Altman, D.G.; Bagley, H.; Barnes, K.L.; Blazeby, J.M.; Brookes, S.T.; Clarke, M.; Gargon, E.; Gorst, S.; Harman, N.; et al. The COMET Handbook: Version 1.0. Trials 2017, 18 (Suppl. 3), 280. [Google Scholar] [CrossRef]
- Mitchell, S.A.; Leidy, N.K.; Mooney, K.H.; Dudley, W.N.; Beck, S.L.; LaStayo, P.C.; Cowen, E.W.; Palit, P.; Comis, L.E.; Krumlauf, M.C.; et al. Determinants of functional performance in long-term survivors of allogeneic hematopoietic stem cell transplantation with chronic graft-versus-host disease (cGVHD). Bone Marrow Transplant. 2010, 45, 762–769. [Google Scholar] [CrossRef]
- Morishita, S.; Kaida, K.; Yamauchi, S.; Sota, K.; Ishii, S.; Ikegame, K.; Kodama, N.; Ogawa, H.; Domen, K. Relationship between corticosteroid dose and declines in physical function among allogeneic hematopoietic stem cell transplantation patients. Support Care Cancer 2013, 21, 2161–2169. [Google Scholar] [CrossRef]
- Kramer, M.; Heussner, P.; Herzberg, P.Y.; Andree, H.; Hilgendorf, I.; Leithaeuser, M.; Junghanss, C.; Freund, M.; Wolff, D. Validation of the grip test and human activity profile for evaluation of physical performance during the intermediate phase after allogeneic hematopoietic stem cell transplantation. Support. Care Cancer 2013, 21, 1121–1129. [Google Scholar] [CrossRef]
- Sayre, C.A.; Belza, B.; Shannon Dorcy, K.; Phelan, E.; Whitney, J.D. Patterns of Hand Grip Strength and Detection of Strength Loss in Patients Undergoing Bone Marrow Transplantation: A Feasibility Study. Oncol. Nurs. Forum 2017, 44, 606–614. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hacker, E.D.; Mjukian, M. Review of attrition and adherence in exercise studies following hematopoietic stem cell transplantation. Eur. J. Oncol. Nurs. 2014, 18, 175–182, Epub 2013 Nov 22. Erratum in Eur. J. Oncol. Nurs. 2014, 18, 443. [Google Scholar] [CrossRef] [PubMed]
- Oberoi, S.; Robinson, P.D.; Cataudella, D.; Culos-Reed, S.N.; Davis, H.; Duong, N.; Gibson, F.; Götte, M.; Hinds, P.; Nijhof, S.L.; et al. Physical activity reduces fatigue in patients with cancer and hematopoietic stem cell transplant recipients: A systematic review and meta-analysis of randomized trials. Crit. Rev. Oncol. Hematol. 2018, 122, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Dirou, S.; Chambellan, A.; Chevallier, P.; Germaud, P.; Lamirault, G.; Gourraud, P.A.; Perrot, B.; Delasalle, B.; Forestier, B.; Guillaume, T.; et al. Deconditioning, fatigue and impaired quality of life in long-term survivors after allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant. 2018, 53, 281–290. [Google Scholar] [CrossRef]
- Cella, D.; Yount, S.; Rothrock, N.; Gershon, R.; Cook, K.; Reeve, B.; Ader, D.; Fries, J.F.; Bruce, B.; Rose, M. The Patient-Reported Outcomes Measurement Information System (PROMIS): Progress of an NIH Roadmap cooperative group during its first two years. Med. Care. 2007, 45 (Suppl. 1), S3–S11. [Google Scholar] [CrossRef]
- Karimi, M.; Brazier, J. Health, Health-Related Quality of Life, and Quality of Life: What is the Difference? Pharmacoeconomics 2016, 34, 645–649. [Google Scholar] [CrossRef]
- Van Haren, I.E.; Timmerman, H.; Potting, C.M.; Blijlevens, N.M.; Staal, J.B.; Nijhuis-van der Sanden, M.W. Physical exercise for patients undergoing hematopoietic stem cell transplantation: Systematic review and meta-analyses of randomized controlled trials. Phys. Ther. 2013, 93, 514–528. [Google Scholar] [CrossRef]
- Van der Lans, M.C.M.; Witkamp, F.E.; Oldenmenger, W.H.; Broers, A.E.C. Five Phases of Recovery and Rehabilitation After Allogeneic Stem Cell Transplantation: A Qualitative Study. Cancer Nurs. 2019, 42, 50–57. [Google Scholar] [CrossRef]
- Carreras, E.; Dufour, C.; Mohty, M.; Kröger, N. (Eds.) The EBMT Handbook: Hematopoietic Stem Cell Transplantation and Cellular Therapies [Internet], 7th ed.; Springer: Cham, Switzerland, 2019. [Google Scholar] [PubMed]
| Study Characteristics | |
|---|---|
| Included Studies | N = 39 (YY%) |
| Study Design | |
| RCTs | 24 (62%) |
| Feasibility Studies | 9 (23%) |
| Pilot Studies | 6 (15%) |
| Population | |
| Allogeneic stem cell transplantation | 14 (36%) |
| Allogeneic and autologous stem cell transplantation | 25 (64%) |
| Setting | |
| Hospital | 22 (56%) |
| Outpatient post HSCT | 11 (28%) |
| Outpatient pre HSCT | 3 (8%) |
| Throughout | 2 (5%) |
| Inpatient post HSCT | 1 (3%) |
| Intervention | |
| Psychological Interventions | 5 (13%) |
| Exercise Training | 17 (44%) |
| Respiratory Training | 3 (8%) |
| Physical Modalities | 2 (5%) |
| Relaxation Techniques | 2 (5%) |
| Other | 10 (25%) |
| Language | |
| English | 39 (100%) |
| Country | |
| USA | 13 (34%) |
| Germany | 9 (23%) |
| Canada | 4 (10%) |
| Brazil | 4 (10%) |
| Switzerland | 2 (5%) |
| Other | 7 (18%) |
| CORE AREA «FEASIBILITY» | |||||
|---|---|---|---|---|---|
| Allogeneic | |||||
| Outcomes | Instruments | Design | Phase | Intervention | Reference |
| Feasibility [16,17] N = 2 | Adherence [16] Adverse Events [16] Program completion from 50% of the patients [17] Recruitment [16] | Feasibility Pilot Study [17] | Hospital [17] | Exercise [16,17] | Santa mina et al., 2020 Schuler et al., 2016 |
| HSCT | |||||
| Outcomes | Instruments | Design | Phase | Intervention | Reference |
| Feasibility [18,19,20,21,22,23,24,25,27] N = 7 | Adherence [18,19,20,21,25,27] | Feasibility [18,19,20] Pilot Study [21,25] | Hospital [18,19,20] Outpatient post [21] Outpatient pre [25] | Electric Muscle Stimulation [18] Healing touch [19] Inspiratory muscle training [20] Home based aerobic exercise [6] Exercise Training and Nutritional Support [25] | Bewarder et al., 2019 Lu et al., 2016 De almeida et al., 2020 Wilson et al., 2005 Rupnik et al., 2020 |
| Attrition [20,21,25,27] | Feasibility [20] Pilot Study [21,25] | Hospital [20] Outpatient post [21] Outpatient pre [25] | Inspiratory muscle training [20] Home based aerobic exercise [21] Exercise Training and Nutritional Support [25] | De almeida et al., 2020 Wilson et al., 2005 Rupnik et al., 2020 | |
| Retention [19,22] | Feasibility [19,22] | Hospital [19] Outpatient post [22] | Healing touch [19] Yoga [22] | Lu et al., 2016 Baydoun et al., 2020 | |
| Acceptability [21,25] | Pilot Study [21,25] | Outpatient post [21] Outpatient pre [25] | Home based aerobic exercise [21] Exercise Training and Nutritional Support [25] | Wilson et al., 2005 Rupnik et al., 2020 | |
| Accrual Acceptance [22] | Feasibility [22] | Outpatient post [22] | Yoga [22] | Baydoun et al., 2020 | |
| Adverse Events [22] | Feasibility [22] | Outpatient post [22] | Yoga [22] | Baydoun et al., 2020 | |
| N/A [23] | RCT [23] | Hospital [23] | Exergaming [23] | Schumacher et al., 2018 | |
| Protocol Adherence [22] | Feasibility [22] | Outpatient post [22] | Yoga [22] | Baydoun et al., 2020 | |
| Rate of participant enrolment [24] | Pilot Study [24] | Outpatient post [24] | Positive Psychology Intervention [24] | Amonoo et al., 2020 | |
| Rate of session completion [24] | Pilot Study [24] | Outpatient post [24] | Positive Psychology Intervention [24] | Amonoo et al., 2020 | |
| Recruitment [19,27] | Feasibility [19] | Hospital [19] | Healing touch [19] | Lu et al., 2016 | |
| Recruitment Rate [20] | Feasibility [20] | Hospital [20] | Inspiratory muscle training [20] | De almeida et al., 2020 | |
| Safety [18,20,21] N = 4 | Adverse Events [18,20,21] The WHO bleeding Scale [18] | Feasibility [18,20] Pilot Study [21] | Hospital [18,20] Outpatient post [21] | Electric Muscle Stimulation [18] Inspiratory muscle training [20] Home based aerobic exercise [21] | Bewarder et al., 2019 De almeida et al., 2020 Wilson et al., 2005 |
| Acceptability [24] N = 1 | Rating of ease and utility [24] | Pilot Study [24] | Outpatient post [24] | Positive Psychology Intervention [24] | Amonoo et al., 2020 |
| Adherence [26] N = 1 | Exercise Sessions completed as proportion of the prescribed exercises [26] | RCT [26] | Throughout [26] | Exercise Training [26] | Peters et al., 2018 |
| Attrition [26] N = 1 | N/A [26] | RCT [26] | Throughout [26] | Exercise Training [26] | Peters et al., 2018 |
| Compliance [26] N = 1 | Exercise Sessions completed [26] | RCT [26] | Throughout [26] | Exercise Training [26] | Peters et al., 2018 |
| Progression after initial prescription [26] N = 1 | Added sets, repetitions or exercises [26] | RCT [26] | Throughout [26] | Exercise Training [26] | Peters et al., 2018 |
| Adverse Events [27] | Fioritto et al., 2021 | ||||
| CORE AREA LIFE IMPACT | |||||
| Allogeneic | |||||
| Outcomes | Instruments | Design | Phase | Intervention | Reference |
| Fatigue [16,17,28,29,30,31,32,33] N = 8 | Brief Fatigue Inventory [28,29] | Pilot Study [28] RCT [29] | Outpatient post [28,29] | Individualized Exercise Program [28] Supervised exercise program [29] | Carlson et al., 2006 Shleton et al., 2008 |
| FACT-F [16,28] | Feasibility [16] Pilot Study [28] | Hospital [16] Outpatient post [28] | Exercise [16] Individualized Exercise Program [28] | Santa mina et al., 2020 Carlson et al., 2006 | |
| Multidimensional Fatigue Inventory [16,30] | Feasibility [16] RCT [30] | Hospital [16,30] | Exercise [16] Whole Body Vibration Training [30] | Santa mina et al., 2020 Pahl et al., 2020 | |
| EORTC QLQ FA-13 [17] | Pilot Study [17] | Hospital [17] | Exercise [17] | Schuler et al., 2016 | |
| FACT-An Anemia Scale [31] | RCT [31] | Hospital [31] | Multimodal Intervention [31] | Jarden et al., 2009 | |
| Fatigue Impact Scale (FIS) [32] | RCT [32] | Inpatient post [32] | Inspiratory muscle training [32] | Bargi et al., 2015 | |
| Piper Fatigue Scale [33] | RCT [33] | Hospital [33] | Relaxation Breathing Exercise [33] | Kim et al., 2005 | |
| Depression [16,17,28,32,33] N = 5 | Hospital Anxiety And Depression Scale [17] | Pilot Study [17] | Hospital [17] | Exercise [17] | Schuler et al., 2016 |
| Montgomery-Âsberg Depression Rating Scale (MADRS) [32] | RCT [32] | Inpatient post [32] | Inspiratory muscle training [32] | Bargi et al., 2015 | |
| Structured Clinical Interview [28] | Pilot Study [28] | Outpatient post [28] | Individualized Exercise Program [28] | Carlson et al., 2006 | |
| The Beck Depression Inventory [33] | RCT [33] | Hospital [33] | Relaxation Breathing Exercise [33] | Kim et al., 2005 | |
| The Center for Epidemiological Studies Depression Scale (CES-D) [28] | Pilot Study [28] | Outpatient post [28] | Individualized Exercise Program [28] | Carlson et al., 2006 | |
| The Patient Health Questionnaire 9 (PHQ-9) [16] | Feasibility [16] | Hospital [16] | Exercise [16] | Santa mina et al., 2020 | |
| Quality of Life [17,30,32,34,35] N = 5 | EORTC QLQ-C30 [17,30,32,34] | Pilot Study [17] RCT [30,32,34] | Hospital [17,30,34] Inpatient post [32] | Exercise [17] Inspiratory muscle training [32] Exercise Training [34] Whole Body Vibration Training [30] | Schuler et al., 2016 Bargi et al., 2015 Baumann et al., 2011 Pahl et al., 2020 |
| FACT-BMT [35] | Feasibility [35] | Outpatient post [35] | Telehealth Psychoeducational support [35] | Lounsbery et al., 2010 | |
| Health related Quality of Life [16,31,36,37] N = 4 | EORTC QLQ-C30 [16,31,36,37] | Feasibility [16] RCT [31,36,37] | Hospital [16,31,36] Throughout [37] | Exercise [16] Multimodal Intervention [31] Whole Body Vibration Training [36] Self-administered exercise [37] | Santa mina et al., 2020 Kaeding et al., 2018 Wiskemann et al., 2011 |
| Anxiety [16,33,38] N = 3 | Generalized Anxiety Disorder GAD7 [16] | Feasibility [16] | Hospital [16] | Exercise [16] | Santa mina et al., 2020 |
| The State-Trait Anxiety Inventory [33] | RCT [33] | Hospital [33] | Relaxation Breathing Exercise [33] | Kim et al., 2005 | |
| Visual Analog Scale [38] | RCT [38] | Hospital [38] | Music Therapy [38] | Doro et al., 2017 | |
| Mood [28,38] N = 2 | Profile of Mood States (POMS) [28] | Pilot Study [28] | Outpatient post [28] | Individualized Exercise Program [28] | Carlson et al., 2006 |
| Visual Analog Scale [38] | RCT [38] | Hospital [38] | Music Therapy [38] | Doro et al., 2017 | |
| Distress [37] N = 1 | The National Comprehensive Cancer Network Distress Thermometer [37] | RCT [37] | Throughout [37] | Self-administered exercise [37] | Wiskemann et al., 2011 |
| Perception of Personal Benefits [35] N = 1 | Post Traumatic growth inventory [35] | Feasibility [35] | Outpatient post [35] | Telehealth Psychoeducational support [35] | Lounsbery et al., 2010 |
| Physical Activity [30] N = 1 | Freiburg Questionnaire on physical activity [30] | RCT [30] | Hospital [30] | Whole Body Vibration Training [30] | Pahl et al., 2020 |
| Physical Well Being [37] N = 1 | Hospital Anxiety And Depression Scale [37] | RCT [37] | Throughout [37] | Self-administered exercise [37] | Wiskemann et al., 2011 |
| Psychological Well Being [31] N = 1 | Hospital Anxiety And Depression Scale [31] | RCT [31] | Hospital [31] | Multimodal Intervention [31] | Jarden et al., 2009 |
| Self-efficacy for exercise [16] N = 1 | Exercise Self Efficacy Scale [16] | Feasibility [16] | Hospital [16] | Exercise [16] | Santa mina et al., 2020 |
| Spirituality and Meaning Making [35] N = 1 | FACT-SP [35] | Feasibility [35] | Outpatient post [35] | Telehealth Psychoeducational support [35] | Lounsbery et al., 2010 |
| Subjective Distress [35] N = 1 | Impact of Event Scale Revised [35] | Feasibility [35] | Outpatient post [35] | Telehealth Psychoeducational support [35] | Lounsbery et al., 2010 |
| HSCT | |||||
| Outcomes | Instruments | Design | Phase | Intervention | Reference |
| Fatigue [21,22,39,40,41,42,43] N = 7 | Brief Fatigue Inventory [39] | RCT [39] | Hospital [39] | Relaxation Techniques [39] | Jafari et al., 2018 |
| Chalder Fatigue Scale [40] | RCT [40] | Hospital [40] | Strength Training [40] | Hacker et al., 2017 | |
| EORTC QLQ-C30 [40] | RCT [40] | Hospital [40] | Strength Training [40] | Hacker et al., 2017 | |
| FACT-An Anaemia Scale [41] | RCT [41] | Outpatient post [41] | Outpatient physical exercise [41] | Knols et al., 2011 | |
| Fatigue Symptom Inventory [21] | Pilot Study [21] | Outpatient post [21] | Home based aerobic exercise [21] | Wilson et al., 2005 | |
| Multidimensional Fatigue Inventory [22] | Feasibility [22] | Outpatient post [22] | Yoga [22] | Baydoun et al., 2020 | |
| SF36 [42] | RCT [42] | Outpatient post [42] | Exercise Relaxation Information [42] | Bird et al., 2010 | |
| The Fatigue Questionnaire (FQ) [43] | Feasibility [43] | Outpatient post [43] | Mindfulness based Intervention [43] | Grossman et al., 2015 | |
| Depression [19,23,43,44,45,46] N = 6 | Hospital Anxiety And Depression Scale [23,44,45,46] | RCT [23,44,45,46] | Hospital [23,44,45,46] | Exergaming [23] | Schumacher et al., 2018 |
| Media Art [44] | Mc Cabe et al., 2013 | ||||
| Palliative Care [45] | El Jawahri et al., 2017 | ||||
| Problem Solving Training [46] | Balck et al., 2019 | ||||
| The Centre for Epidemiological Studies Depression Scale (CES-D) [19,43] | Feasibility [19,43] | Hospital [19] | Healing touch [19] | Lu e al 2016 | |
| Outpatient post [43] | Mindfulness based Intervention [43] | Grossman et al., 2015 | |||
| Anxiety [23,43,44,45,46] N = 5 | Hospital Anxiety And Depression Scale [23,44,46] | RCT [23,44,45,46] | Hospital [23,44,45,46] | Exergaming [23] | Schumacher et al., 2018 |
| Media Art [44] | Mc Cabe et al., 2013 | ||||
| Palliative Care [45] | El Jawahri et al., 2017 | ||||
| Problem Solving Training [46] | Balck et al., 2019 | ||||
| The Spielberger Trait Anxiety Scale (STAI) [43] | Feasibility [43] | Outpatient post [43] | Mindfulness based Intervention [43] | Grossman et al., 2015 | |
| Quality of Life [19,34,40,42,45] N = 5 | EORTC QLQ-C30 [34,40] | RCT [34,40] | Hospital [34,40] | Exercise Therapy [34] | Baumann et al., 2010 |
| Strength Training [40] | Hacker et al., 2017 | ||||
| FACT-BMT [19,45] | Feasibility [19] | Hospital [19] | Healing touch [19] | Lu e al 2016 | |
| RCT [45] | Hospital [45] | Palliative Care [45] | El Jawahri et al., 2017 | ||
| The Graham and Longman QoL Questionnaire [42] | RCT [42] | Outpatient post [42] | Exercise Relaxation Information [42] | Bird et al., 2010 | |
| Health related Quality of Life [21,23,25,27,41,43,47] N = 7 | EORTC QLQ-C30 [25,27,41] | RCT [41] Pilot [25] Feasibility [27] | Outpatient post [41] Outpatient pre [25] | Outpatient physical exercise [41] Exercise Training and Nutritional Support [25] Individualized Exercise Training [27] | Knols et al., 2011 Rupnik et al., 2020 Fioritto et al., 2021 |
| FACT [43] | Feasibility [43] | Outpatient post [43] | Mindfulness based Intervention [43] | Grossman et al., 2015 | |
| FACT-BMT [23,47] | RCT [23,47] | Hospital [23,47] | Exergaming [23] Multidirectional Walking [47] | Schumacher et al., 2018 Potiaumpai et al., 2020 | |
| Profile of Health-Related Quality of Life in Chronic Disorders [43] | Feasibility [43] | Outpatient post [43] | Mindfulness based Intervention [43] | Grossman et al., 2015 | |
| SF36 [21,23] | Pilot Study [21] | Outpatient post [21] | Home based aerobic exercise [21] | Wilson et al., 2005 | |
| RCT [23] | Hospital [23] | Exergaming [23] | Schumacher et al., 2018 | ||
| Physical Activity [40,41] | Accelerometry [40] | RCT [40] | Hospital [40] | Strength Training [40] | Hacker et al., 2017 |
| International Physical Activity Questionnaire [41] | RCT [41] | Outpatient post [41] | Outpatient physical exercise [41] | Knols et al., 2011 | |
| The Godin leisure time exercise questionnaire [40] | RCT [40] | Hospital [40] | Strength Training [40] | Hacker et al., 2017 | |
| Distress [19,44] N = 2 | Profile of Mood States (POMS) [19] | Feasibility [19] | Hospital [19] | Healing touch [19] | Lu et al., 2016 |
| The Distress Thermometer [44] | RCT [44] | Hospital [44] | Media Art [44] | Mc Cabe et al., 2013 | |
| Post-traumatic Stress Disorder Symptoms [45,48] N = 2 | Clinician administered PTSD Scale for DSM IV [48] | RCT [48] | Outpatient post [48] | Cognitive Behavioural Therapy [48] | DuHamel et al., 2010 |
| PCL-C [45,48] | RCT [45,48] | Hospital [45] | Palliative Care [45] | El Jawahri et al., 2017 | |
| Outpatient post [33] | Cognitive Behavioural Therapy [48] | DuHamel et al., 2010 | |||
| Psychological distress [46,48] N = 2 | Brief Symptom Inventory [48] | RCT [48] | Outpatient post [48] | Cognitive Behavioural Therapy [48] | DuHamel et al., 2010 |
| SCL-K-9 [46] | RCT [46] | Hospital [46] | Problem Solving Training [46] | Balck et al., 2019 | |
| Bodily Pain [42] | SF36 [42] | RCT [42] | Outpatient post [42] | Exercise Relaxation Information [42] | Bird et al., 2010 |
| Coping [46] N = 1 | The Brief COPE [46] | RCT [46] | Hospital [46] | Problem Solving Training [46] | Balck et al., 2019 |
| Extend of the pain [46] N = 1 | The Questions of Pain [46] | RCT [46] | Hospital [46] | Problem Solving Training [46] | Balck et al., 2019 |
| General Distress [46] N = 1 | The National Comprehensive Cancer Network Distress Thermometer [46] | RCT [46] | Hospital [46] | Problem Solving Training [46] | Balck et al., 2019 |
| General distress and depressive symptoms [49] | Brief Symptom Inventory [49] | RCT [49] | Outpatient post [49] | Telephone administered cognitive behavioural therapy [49] | Applebaum et al., 2012 |
| General Mental Health [42] N = 1 | SF36 [42] | RCT [42] | Outpatient post [42] | Exercise Relaxation Information [42] | Bird et al., 2010 |
| Illness Related PTSD Symptoms [49] | PCL-C [49] | RCT [49] | Outpatient post [49] | Telephone administered cognitive behavioural therapy [49] | Applebaum et al., 2012 |
| Mental Well Being [50] | Cancer and Treatment Distress [50] | RCT [50] | Outpatient pre [50] | Exercise and Stress Management [50] | Jacobsen et al., 2014 |
| Pittsburgh Sleep Quality Index [35] | RCT [35] | Outpatient pre [35] | Exercise and Stress Management [35] | Jacobsen et al., 2014 | |
| Physical Fitness [8] | Human Activity Profile [8] | RCT [8] | Hospital [8] | Exergaming [8] | Schumacher et al., 2018 |
| Physical Functioning [27] | SF36 [27] | RCT [27] | Outpatient post [27] | Exercise Relaxation Information [27] | Bird et al., 2010 |
| Physical Well Being [35] | SF36 [35] | RCT [35] | Outpatient pre [35] | Exercise and Stress Management [35] | Jacobsen et al., 2014 |
| Problem Solving Ability [46] N = 1 | The Social Problem-Solving Inventory-Revised (SPSI-R) [46] | RCT [46] | Hospital [46] | Problem Solving Training [46] | Balck et al., 2019 |
| Psychological health [42] | General Health Questionnaire [42] | RCT [42] | Outpatient post [42] | Exercise Relaxation Information [42] | Bird et al., 2010 |
| Psychological Performance [18] | EORTC QLQ-C30 [18] | Feasibility [18] | Hospital [18] | Electric Muscle Stimulation [18] | Bewarder et al., 2019 |
| Multidimensional Fatigue Inventory [18] | Feasibility [18] | Hospital [18] | Electric Muscle Stimulation [18] | Bewarder et al., 2019 | |
| Quantified Walking Activity [41] | Accelerometry [41] | RCT [41] | Outpatient post [41] | Outpatient physical exercise [41] | Knols et al., 2011 |
| Role Limitation [42] | SF36 [42] | RCT [42] | Outpatient post [42] | Exercise Relaxation Information [42] | Bird et al., 2010 |
| Self-Reported Physical Function [41] | EORTC QLQ-C30 [41] | RCT [41] | Outpatient post [41] | Outpatient physical exercise [41] | Knols et al., 2011 |
| Social Functioning [42] | SF36 [42] | RCT [42] | Outpatient post [42] | Exercise Relaxation Information [42] | Bird et al., 2010 |
| Social support [46] N = 1 | N/A | RCT [46] | Hospital [46] | Problem Solving Training [46] | Balck et al., 2019 |
| Symptom Burden [45] N = 1 | Edmonton Symptom Assessment Scale [45] | RCT [45] | Hospital [45] | Palliative Care [45] | El Jawahri et al., 2017 |
| Therapeutic alliance [49] | Working Alliance Inventory Short Form [49] | RCT [49] | Outpatient post [49] | Telephone-administered cognitive behavioural therapy [49] | Applebaum et al., 2012 |
| Vitality [42] | SF36 [42] | RCT [42] | Outpatient post [42] | Exercise Relaxation Information [42] | Bird et al., 2010 |
| CORE AREA PATHOPHYSIOLOGY | |||||
| Allogeneic | |||||
| Outcomes | Instruments | Design | Phase | Intervention | Reference |
| Endurance [17,51] N = 2 | Bicycle ergometer [17] | Pilot Study [17] | Hospital [17] | Exercise [17] | Schuler et al., 2016 |
| The 6-Minute Walk Test [17] | Pilot Study [17] | Hospital [17] | Exercise [17] | Schuler et al., 2016 | |
| The WHO Scheme [51] | RCT [51] | Hospital [51] | Exercise Training [51] | Baumann et al., 2011 | |
| Functional Performance [30,31] N = 2 | 2 min stair climb test [31] | RCT [31] | Hospital [31] | Multimodal Intervention [31] | Jarden et al., 2009 |
| Chairing test on force plate [30] | RCT [30] | Hospital [30] | Whole Body Vibration Training [30] | Pahl et al., 2020 | |
| Maximum Counter movement jump [30] | RCT [30] | Hospital [30] | Whole Body Vibration Training [30] | Pahl et al., 2020 | |
| Handgrip Strength [16,32] N = 2 | Hand Grip Dynamometer [16,32] | Feasibility [16] RCT [32] | Hospital [16] Inpatient post [32] | Exercise [16] Inspiratory muscle training [32] | Santa mina et al., 2020 Bargi et al., 2015 |
| Physical Performance [28,29] N = 2 | 50-foot walk test [29] | RCT [29] | Outpatient post [29] | Supervised exercise program [29] | Shleton et al., 2008 |
| Blood Lactate Concentrate [28] | Pilot Study [28] | Outpatient post [28] | Individualized Exercise Program [28] | Carlson et al., 2006 | |
| Cardiac Output [28] | Pilot Study [28] | Outpatient post [28] | Individualized Exercise Program [28] | Carlson et al., 2006 | |
| Forward reach [29] | RCT [29] | Outpatient post [29] | Supervised exercise program [29] | Shleton et al., 2008 | |
| Oxygen Uptake (VO2) [28] | Pilot Study [28] | Outpatient post [28] | Individualized Exercise Program [28] | Carlson et al., 2006 | |
| Power Output [28] | Pilot Study [28] | Outpatient post [28] | Individualized Exercise Program [28] | Carlson et al., 2006 | |
| Rating of Perceived Exertion (RPE) [28] | Pilot Study [28] | Outpatient post [28] | Individualized Exercise Program [28] | Carlson et al., 2006 | |
| Respiratory Exchange Ratio [28] | Pilot Study [28] | Outpatient post [28] | Individualized Exercise Program [28] | Carlson et al., 2006 | |
| Stroke Volume [28] | Pilot Study [28] | Outpatient post [28] | Individualized Exercise Program [28] | Carlson et al., 2006 | |
| The 6-Minute Walk Test [29] | RCT [29] | Outpatient post [29] | Supervised exercise program [29] | Shleton et al., 2008 | |
| Timed repeated sit to stand [29] | RCT [29] | Outpatient post [29] | Supervised exercise program [29] | Shleton et al., 2008 | |
| Uniped stance time [29] | RCT [29] | Outpatient post [29] | Supervised exercise program [29] | Shleton et al., 2008 | |
| Ventilatory Threshold [28] | Pilot Study [28] | Outpatient post [28] | Individualized Exercise Program [28] | Carlson et al., 2006 | |
| Pulmonary Function [32,51] N = 2 | Spirometry [32,51] | RCT [32,51] | Hospital [51] Inpatient post [32] | Exercise Training [51] Inspiratory muscle training [32] | Baumann et al., 2011 Bargi et al., 2015 |
| Aerobic endurance performance capacity [36] | The 6-Minute Walk Test [36] | RCT [36] | Hospital [36] | Whole Body Vibration Training [36] | Kaeding et al., 2018 |
| Body Composition [30] | Displacement Plethysmography [30] | RCT [30] | Hospital [30] | Whole Body Vibration Training [30] | Pahl et al., 2020 |
| Body Mass Index [16] | Bioimpendance Analysis [16] | Feasibility [16] | Hospital [16] | Exercise [16] | Santa mina et al., 2020 |
| Cardiorespiratory Fitness [30] | Cardiopulmonary Exercise Testing [30] | RCT [30] | Hospital [30] | Whole Body Vibration Training [30] | Pahl et al., 2020 |
| Functional Aerobic Capacity [16] | 30 Second Sit to Stand Test [16] | Feasibility [16] | Hospital [16] | Exercise [16] | Santa mina et al., 2020 |
| The 6-Minute Walk Test [16] | Feasibility [16] | Hospital [16] | Exercise [16] | Santa mina et al., 2020 | |
| Functional Status [52] | Karnofsky Performance Status Scale [52] | RCT [52] | Hospital [52] | Walking Regimen [52] | DeFor et al., 2007 |
| Isokinetic Leg Performance [36] | Biodex System [36] | RCT [36] | Hospital [36] | Whole Body Vibration Training [36] | Kaeding et al., 2018 |
| Knee Extension Strength [17] | External resistor [17] | Pilot Study [17] | Hospital [17] | Exercise [17] | Schuler et al., 2016 |
| Leucocyte count [33] | Total and differential Counts of white blood cells [33] | RCT [33] | Hospital [33] | Relaxation Breathing Exercise [33] | Kim et al., 2005 |
| Maximal Exercise Capacity [32] | The Modified Incremental Shuttle Walking Test (MISWT) [32] | RCT [32] | Inpatient post [32] | Inspiratory muscle training [32] | Bargi et al., 2015 |
| Muscle Strength [31] | Isotonic muscular strength [31] | RCT [31] | Hospital [31] | Multimodal Intervention [31] | Jarden et al., 2009 |
| Maximal isometric voluntary strength [31] | RCT [31] | Hospital [31] | Multimodal Intervention [31] | Jarden et al., 2009 | |
| Pain [38] | Visual Analog Scale [38] | RCT [38] | Hospital [38] | Music Therapy [38] | Doro et al., 2017 |
| Peak aerobic capacity [16] | Cardiopulmonary Exercise Testing [16] | Feasibility [16] | Hospital [16] | Exercise [16] | Santa mina et al., 2020 |
| Peak Oxygen Consumption [30] | Cardiopulmonary Exercise Testing [30] | RCT [30] | Hospital [30] | Whole Body Vibration Training [30] | Pahl et al., 2020 |
| Peripheral Muscle Strength [32] | Hand-Held Dynamometer [32] | RCT [32] | Inpatient post [32] | Inspiratory muscle training [32] | Bargi et al., 2015 |
| Physical Capacity [31] | Estimated VO2max cycle ergometer [31] | RCT [31] | Hospital [31] | Multimodal Intervention [31] | Jarden et al., 2009 |
| Respiratory Muscle Strength [32] | Mouthpiece device [32] | RCT [32] | Inpatient post [32] | Inspiratory muscle training [32] | Bargi et al., 2015 |
| Strength [51] N = 1 | Isometric Test Digimax [51] | RCT [51] | Hospital [51] | Exercise Training [51] | Baumann et al., 2011 |
| Strength Capacity [30] | Isokinetic Test Knee Extensors [30] | RCT [30] | Hospital [30] | Whole Body Vibration Training [30] | Pahl et al., 2020 |
| Submaximal Exercise Capacity [32] | The 6-Minute Walk Test [32] | RCT [32] | Inpatient post [32] | Inspiratory muscle training [32] | Bargi et al., 2015 |
| Trunk strength [17] | N/A | Pilot Study [17] | Hospital [17] | Exercise [17] | Schuler et al., 2016 |
| Upper Limb Muscle Strength [16] | Hand-Held Dynamometer [16] | Feasibility [16] | Hospital [16] | Exercise [16] | Santa mina et al., 2020 |
| HSCT | |||||
| Outcomes | Instruments | Design | Phase | Intervention | Reference |
| Endurance [23,34] N = 2 | The 2 Minute Walk Test [23] | RCT [23] | Hospital [23] | Exergaming [23] | Schumacher et al., 2018 |
| The WHO Scheme [34] | RCT [34] | Hospital [34] | Exercise Therapy [34] | Baumann et al., 2010 | |
| Treadmill [23] | RCT [23] | Hospital [23] | Exergaming [23] | Schumacher et al., 2018 | |
| Handgrip Strength [23,41] N = 2 | Hand Grip Dynamometer [23,41] | RCT [23,41] | Hospital [23] Outpatient post [41] | Exergaming [23] Outpatient physical exercise [41] | Schumacher et al., 2018 Knols et al., 2011 |
| Aerobic Fitness [21] | Ventilatory Threshold [21] | Pilot Study [21] | Outpatient post [21] | Home based aerobic exercise [21] | Wilson et al., 2005 |
| Blood count [34] | N/A | RCT [34] | Hospital [34] | Exercise Therapy [34] | Baumann et al., 2010 |
| Body Composition [25,41] | Dual x-ray absorptiometry [41] | RCT [41] | Outpatient post [41] | Outpatient physical exercise [41] | Knols et al., 2011 |
| Bioimpendance Analysis [25] | Pilot Study [25] | Outpatient pre [25] | Exercise Training and Nutritional Support [25] | Rupnik et al., 2020 | |
| Cardiorespiratory Fitness [53] | Cardiopulmonary Exercise Testing [53] | Feasibility [53] | Outpatient pre [53] | Home based interval exercise training [53] | Wood et al., 2016 |
| The 6-Minute Walk Test [53] | Feasibility [53] | Outpatient pre [53] | Home based interval exercise training [53] | Wood et al., 2016 | |
| Exercise Capacity [42] | Shuttle Walk Test (SWT) [42] | RCT [42] | Outpatient post [42] | Exercise Relaxation Information [42] | Bird et al., 2010 |
| Functional Ability [40] | 15 Foot Walk Time [40] | RCT [40] | Hospital [40] | Strength Training [40] | Hacker et al., 2017 |
| 30 Second Sit to Stand Test [40] | RCT [40] | Hospital [40] | Strength Training [40] | Hacker et al., 2017 | |
| Timed Stair Climb [40] | RCT [40] | Hospital [40] | Strength Training [40] | Hacker et al., 2017 | |
| Timed Up and Go Test [40] | RCT [40] | Hospital [40] | Strength Training [40] | Hacker et al., 2017 | |
| Functional Exercise Capacity [41] | The 6-Minute Walk Test [41] | RCT [41] | Outpatient post [41] | Outpatient physical exercise [41] | Knols et al., 2011 |
| Functional Capacity [27] | 6 min step test [27] | Feasibility [27] | Hospital [27] | Individualized Exercise Training [27] | Fioritto et al., 2021 |
| Knee Extension Strength [41] | Hand-Held Dynamometer [41] | RCT [41] | Outpatient post [41] | Outpatient physical exercise [41] | Knols et al., 2011 |
| Muscle Strength [25,40] | Arm curl test [40] | RCT [40] | Hospital [40] | Strength Training [40] | Hacker et al., 2017 |
| Hand Grip Dynamometer [25,40] | RCT [40] Pilot Study [25] | Hospital [40] Outpatient pre [25] | Strength Training [40] Exercise Training and Nutritional Support [25] | Hacker et al., 2017 Rupnik et al., 2020 | |
| Rectus femoris cross sectional area [40] | RCT [40] | Hospital [40] | Strength Training [40] | Hacker et al., 2017 | |
| Nausea [35] | SF36 [50] | RCT [50] | Outpatient pre [50] | Exercise and Stress Management [50] | Jacobsen et al., 2014 |
| Physical Performance [18,25] | 8 Foot Walk [18] | Feasibility [18] | Hospital [18] | Electric Muscle Stimulation [18] | Bewarder et al., 2019 |
| Balance Test [18] | Feasibility [18] | Hospital [18] | Electric Muscle Stimulation [18] | Bewarder et al., 2019 | |
| Chair Stands [18] | Feasibility [18] | Hospital [18] | Electric Muscle Stimulation [18] | Bewarder et al., 2019 | |
| The 6-Minute Walk Test [18,25] | Feasibility [18] Pilot Study [25] | Hospital [18] Outpatient pre [25] | Electric Muscle Stimulation [18] Exercise Training and Nutritional Support [25] | Bewarder et al., 2019 Rupnik et al., 2020 | |
| The Short Physical Performance Battery [18] | Feasibility [18] | Hospital [18] | Electric Muscle Stimulation [18] | Bewarder et al., 2019 | |
| 30 Second Sit to Stand Test [25] | Pilot Study [25] | Outpatient pre [25] | Exercise Training and Nutritional Support [25] | Rupnik et al., 2020 | |
| Pulmonary Function [34] | Spirometry [34] | RCT [34] | Hospital [34] | Exercise Therapy [34] | Baumann et al., 2010 |
| Respiratory Function [54] | Tidal Volume, minute volume, maximal inspiratory and expiratory pressures [54] | Pilot Study [54] | Hospital [54] | Respiratory Physiotherapy [54] | Bom et al., 2012 |
| Respiratory Muscle Strength [20] | Maximal Expiratory Pressure [20] | Feasibility [20] | Hospital [20] | Inspiratory muscle training [20] | De almeida et al., 2020 |
| Maximal Inspiratory Pressure [20] | Feasibility [20] | Hospital [20] | Inspiratory muscle training [20] | De almeida et al., 2020 | |
| Respiratory Signs [20] | Peripheral Oxygen Saturation [20] | Feasibility [20] | Hospital [20] | Inspiratory muscle training [20] | De almeida et al., 2020 |
| Respiratory Rate [20] | Feasibility [20] | Hospital [20] | Inspiratory muscle training [20] | De almeida et al., 2020 | |
| Respiratory Symptoms [20] | Medical Records [20] | Feasibility [20] | Hospital [20] | Inspiratory muscle training [20] | De almeida et al., 2020 |
| Strength [34] | Isometric Test Digimax [34] | RCT [34] | Hospital [34] | Exercise Therapy [34] | Baumann et al., 2010 |
| Walking Speed [41] | 50-foot walk test [41] | RCT [41] | Outpatient post [41] | Outpatient physical exercise [41] | Knols et al., 2011 |
| Upper Limb Muscle Strength [27] | Handgrip Dynamometer [27] | Feasibility [27] | Hospital [27] | Individualized Exercise Training [27] | Fioritto et al., 2021 |
| Lower Limb Muscle Strength | 1 min STS [27] | Feasibility [27] | Hospital [27] | Individualized Exercise Training [27] | Fioritto et al., 2021 |
| Physical Function [47] | The 6-Minute Walk Test [47] Timed Up and Go Test [47] The Physical Performance Test [47] | RCT [47] | Hospital [47] | Multidirectional Walking [47] | Potiaumpai et al., 2020 |
| HOSPITAL SETTING | |||||||
|---|---|---|---|---|---|---|---|
| Allogeneic HSCT | |||||||
| T1 | T2 | T3 | T4 | T5 | T6 | T7 | |
| Before Hospitalization | [37] | ||||||
| On Admission | [16,17,30,31,34,36,37,52] | ||||||
| At Baseline | |||||||
| At discharge | [17,30,31,34,36,37] | ||||||
| Before the intervention | [33] | ||||||
| After the intervention | [33] | ||||||
| First Session | [38] | ||||||
| Second Session | [38] | ||||||
| One week before HSCT | [16] | ||||||
| Day − 2 before HSCT | |||||||
| Day − 1 before HSCT | |||||||
| Day + 2 after HSCT | |||||||
| Before HSCT | |||||||
| After HSCT | |||||||
| Second week of Hospitalization | |||||||
| Day + 7 after HSCT | |||||||
| Day + 8 after HSCT | |||||||
| Day + 10 after HSCT | |||||||
| Day + 14 after HSCT | |||||||
| Day + 20 after HSCT | |||||||
| Day + 30 after HSCT | |||||||
| 7 weeks after Hospitalization | [37] | ||||||
| Day + 60 after HSCT | |||||||
| 3 months after HSCT | [17] | ||||||
| Day + 100 after HSCT | [52] | [16] | |||||
| 6 months after HSCT | [30] | ||||||
| 9 months after HSCT | |||||||
| One year after HSCT | [16] | ||||||
| Hospital Setting | |||||||
| HSCT | |||||||
| T1 | T2 | T3 | T4 | T5 | T6 | T7 | |
| Before Hospitalization | [40] | ||||||
| On Admission | [20,23,34,39,44] | ||||||
| At Baseline | [27,45,47] | ||||||
| At discharge | [18,20,27,34] | [44] | |||||
| Before the intervention | [18,19] | ||||||
| After the intervention | [19] | ||||||
| First Session | |||||||
| Second Session | |||||||
| One week before HSCT | [47] | ||||||
| Day − 2 before HSCT | [46] | ||||||
| Day − 1 before HSCT | [54] | [44] | |||||
| Day + 2 after HSCT | [54] | ||||||
| Before HSCT | |||||||
| After HSCT | |||||||
| Second week of Hospitalization | [45] | ||||||
| Day + 7 after HSCT | [44,54] | ||||||
| Day + 8 after HSCT | [39] | ||||||
| Day + 10 after HSCT | [46] | ||||||
| Day + 14 after HSCT | [23] | [39] | |||||
| Day + 20 after HSCT | [46] | ||||||
| Day + 30 after HSCT | [23,47] | ||||||
| 7 weeks after Hospitalization | [40] | ||||||
| Day + 60 after HSCT | [44] | ||||||
| 3 months after HSCT | [45] | ||||||
| Day + 100 after HSCT | [23] | [44] | |||||
| 6 months after HSCT | [45] | [44] | |||||
| 9 months after HSCT | |||||||
| One year after HSCT | |||||||
| NON-Hospital Setting | |||||||
| Allogeneic HSCT | |||||||
| T1 | T2 | T3 | T4 | T5 | T6 | T7 | |
| Before Hospitalization | |||||||
| On Admission | [28] | ||||||
| At Baseline | |||||||
| At discharge | [28] | ||||||
| Before the intervention | [29,32,35] | ||||||
| After the intervention | [29,32,35] | ||||||
| First Session | |||||||
| Second Session | |||||||
| One week before HSCT | |||||||
| Day − 2 before HSCT | |||||||
| Day − 1 before HSCT | |||||||
| Day + 2 after HSCT | |||||||
| Before HSCT | |||||||
| After HSCT | |||||||
| Second week of Hospitalization | |||||||
| Day + 7 after HSCT | |||||||
| Day + 8 after HSCT | |||||||
| Day + 10 after HSCT | |||||||
| Day + 14 after HSCT | |||||||
| Day + 20 after HSCT | |||||||
| Day + 30 after HSCT | |||||||
| 7 weeks after Hospitalization | |||||||
| Day + 60 after HSCT | |||||||
| 3 months after HSCT | |||||||
| Day + 100 after HSCT | |||||||
| 6 months after HSCT | |||||||
| 9 months after HSCT | |||||||
| One year after HSCT | |||||||
| Non-Hospital Setting | |||||||
| HSCT | |||||||
| T1 | T2 | T3 | T4 | T5 | T6 | T7 | |
| Before Hospitalization | |||||||
| On Admission | |||||||
| At Baseline | [21,22,24,25,41,48,49,50] | ||||||
| At discharge | [22,41,42] | ||||||
| Before the intervention | [42,43] | ||||||
| After the intervention | [21,24,43] | [41] | |||||
| First Session | |||||||
| Second Session | |||||||
| One week before HSCT | [25] | ||||||
| Day − 2 before HSCT | |||||||
| Day − 1 before HSCT | |||||||
| Day + 2 after HSCT | |||||||
| Before HSCT | [53] | ||||||
| After HSCT | [53] | ||||||
| Second week of Hospitalization | |||||||
| Day + 7 after HSCT | |||||||
| Day + 8 after HSCT | |||||||
| Day + 10 after HSCT | |||||||
| Day + 14 after HSCT | |||||||
| Day + 20 after HSCT | |||||||
| Day + 30 after HSCT | [50] | ||||||
| 7 weeks after Hospitalization | |||||||
| Day + 60 after HSCT | [50] | ||||||
| 3 months after HSCT | |||||||
| Day + 100 after HSCT | [50] | ||||||
| 6 months after HSCT | [48,49] | [50] | |||||
| 9 months after HSCT | [48,49] | ||||||
| One year after HSCT | [48,49] | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manettas, A.I.; Tsaklis, P.; Kohlbrenner, D.; Mokkink, L.B. A Scoping Review on Outcomes and Outcome Measurement Instruments in Rehabilitative Interventions for Patients with Haematological Malignancies Treated with Allogeneic Stem Cell Transplantation. Curr. Oncol. 2022, 29, 4998-5025. https://doi.org/10.3390/curroncol29070397
Manettas AI, Tsaklis P, Kohlbrenner D, Mokkink LB. A Scoping Review on Outcomes and Outcome Measurement Instruments in Rehabilitative Interventions for Patients with Haematological Malignancies Treated with Allogeneic Stem Cell Transplantation. Current Oncology. 2022; 29(7):4998-5025. https://doi.org/10.3390/curroncol29070397
Chicago/Turabian StyleManettas, Anastasios I., Panagiotis Tsaklis, Dario Kohlbrenner, and Lidwine B. Mokkink. 2022. "A Scoping Review on Outcomes and Outcome Measurement Instruments in Rehabilitative Interventions for Patients with Haematological Malignancies Treated with Allogeneic Stem Cell Transplantation" Current Oncology 29, no. 7: 4998-5025. https://doi.org/10.3390/curroncol29070397
APA StyleManettas, A. I., Tsaklis, P., Kohlbrenner, D., & Mokkink, L. B. (2022). A Scoping Review on Outcomes and Outcome Measurement Instruments in Rehabilitative Interventions for Patients with Haematological Malignancies Treated with Allogeneic Stem Cell Transplantation. Current Oncology, 29(7), 4998-5025. https://doi.org/10.3390/curroncol29070397






