Neoadjuvant Short-Course Radiotherapy Followed by Consolidation Chemotherapy before Surgery for Treating Locally Advanced Rectal Cancer: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Material and Methods
2.1. Search Strategy
2.2. PICOS-Based Inclusion and Exclusion Criteria
2.3. Data Extraction and Quality Assessment
2.4. Statistical Analysis
2.5. Interpretation
3. Results
3.1. Study Selection
3.2. Characteristics of the Included Study
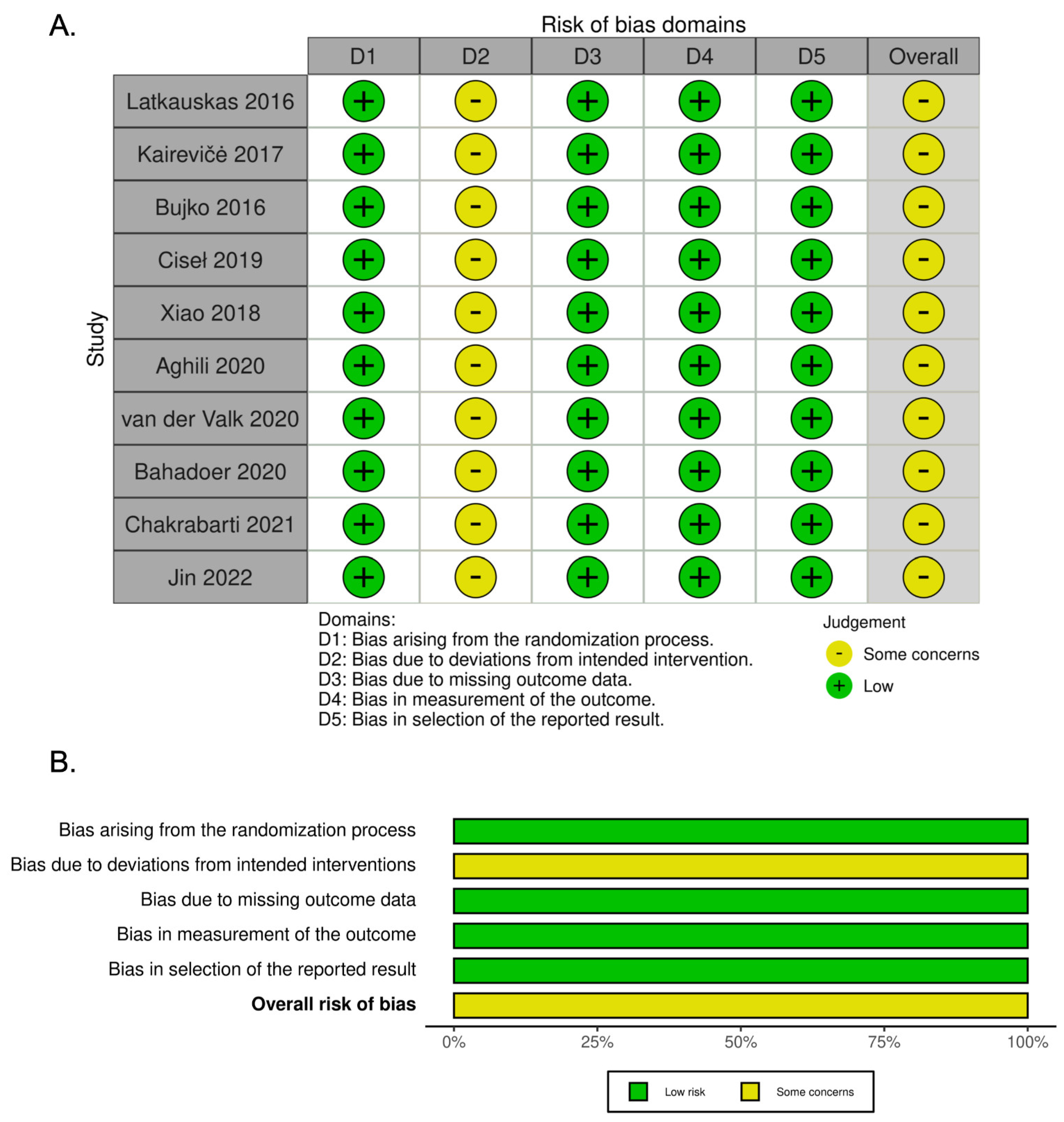
3.3. Quality Analysis
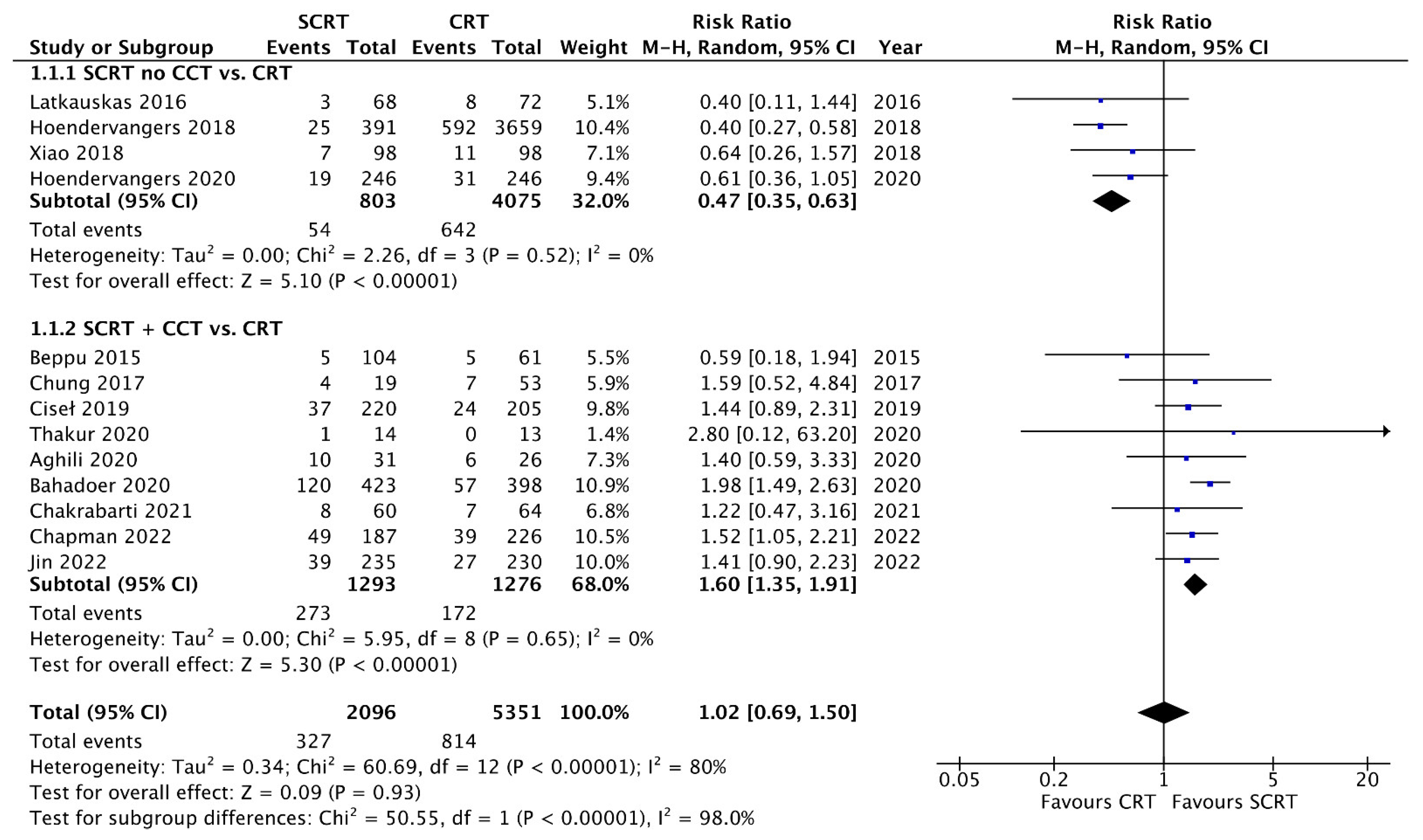
3.4. Tumor Response and pCR Rate
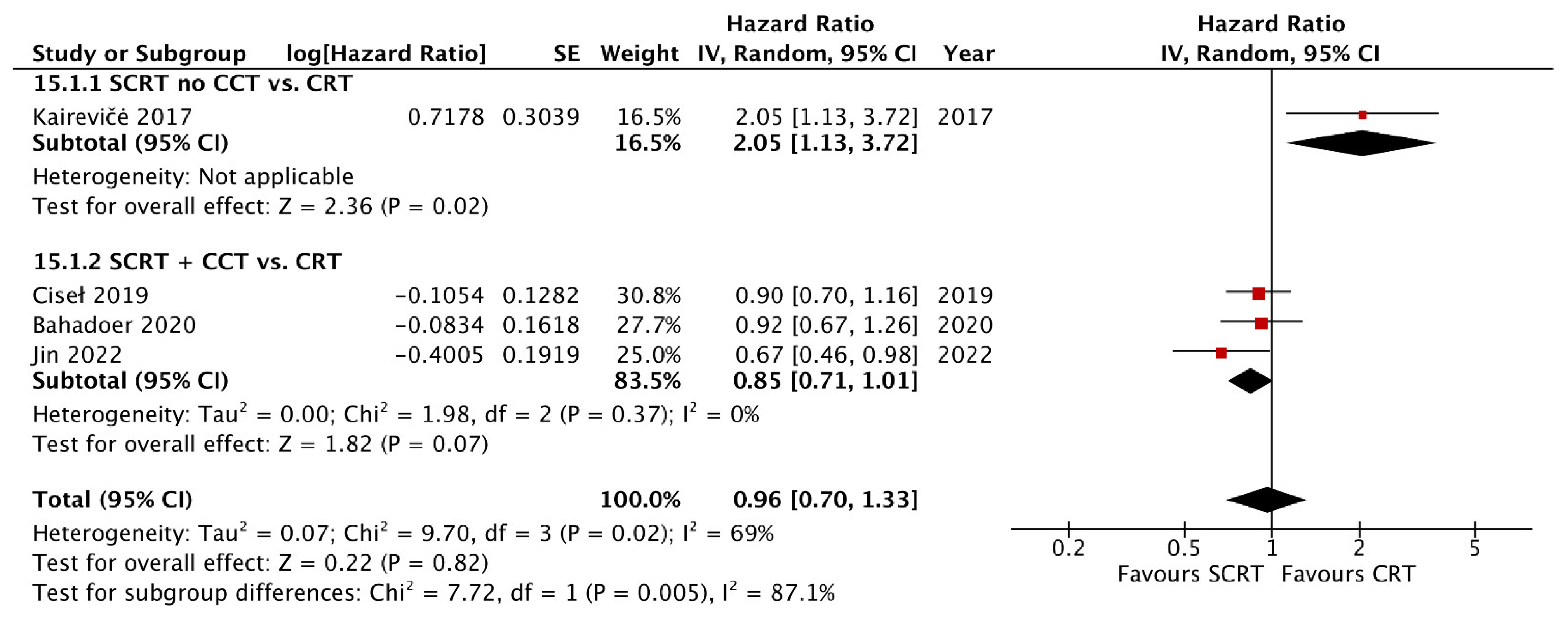
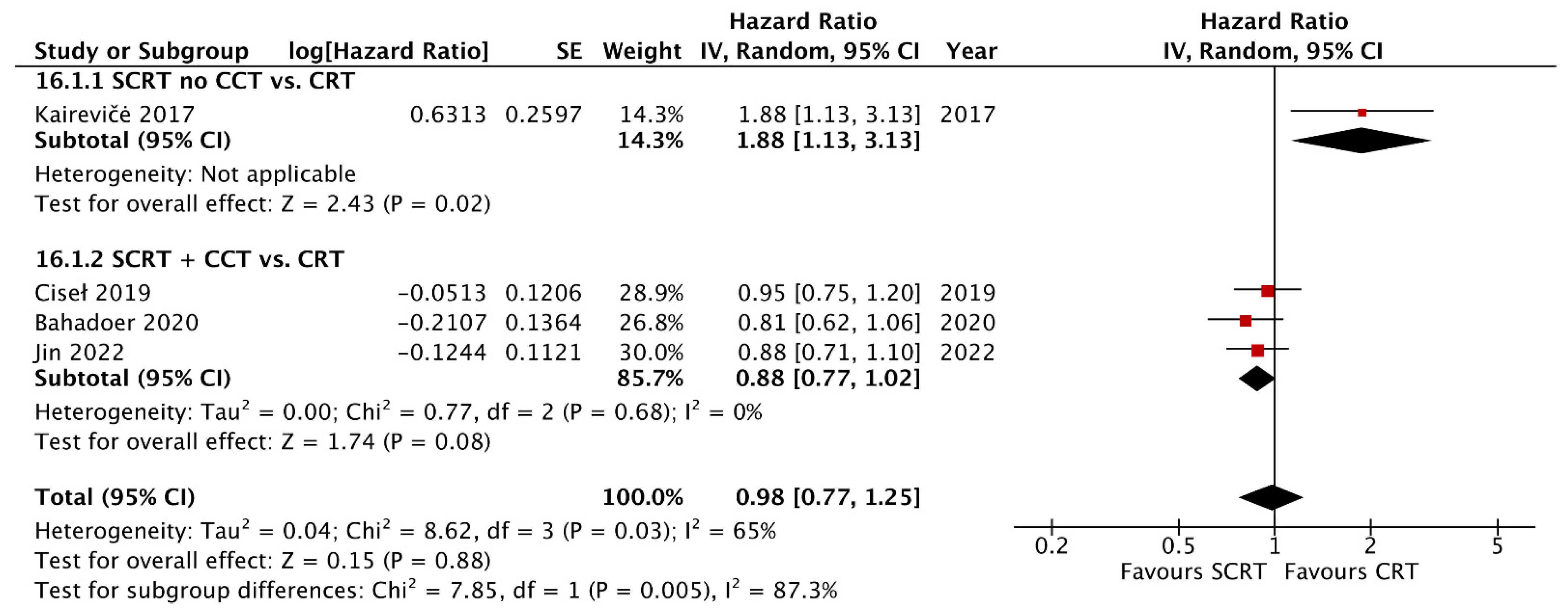
3.5. Overall Survival and Disease-Free Survival
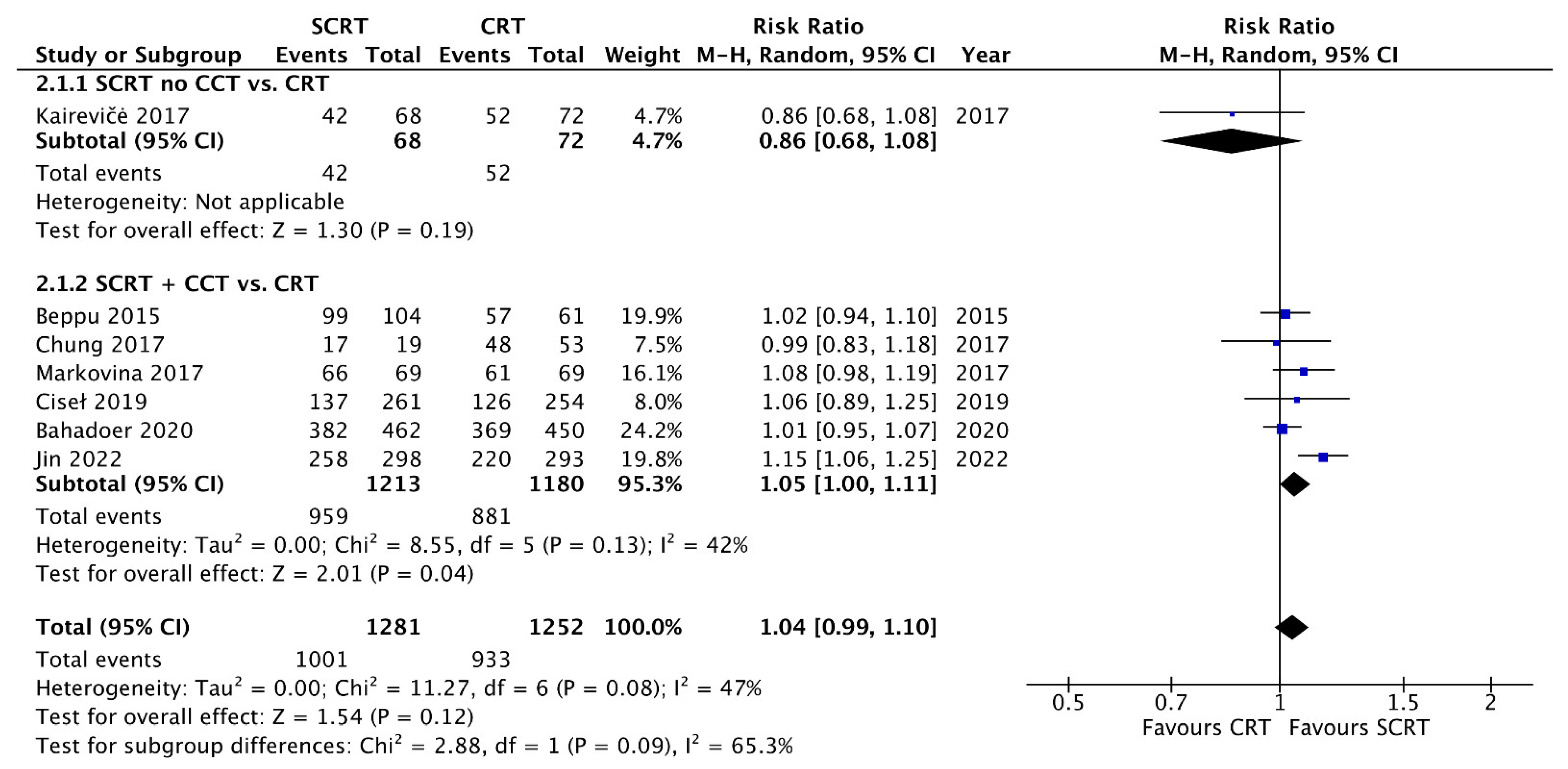
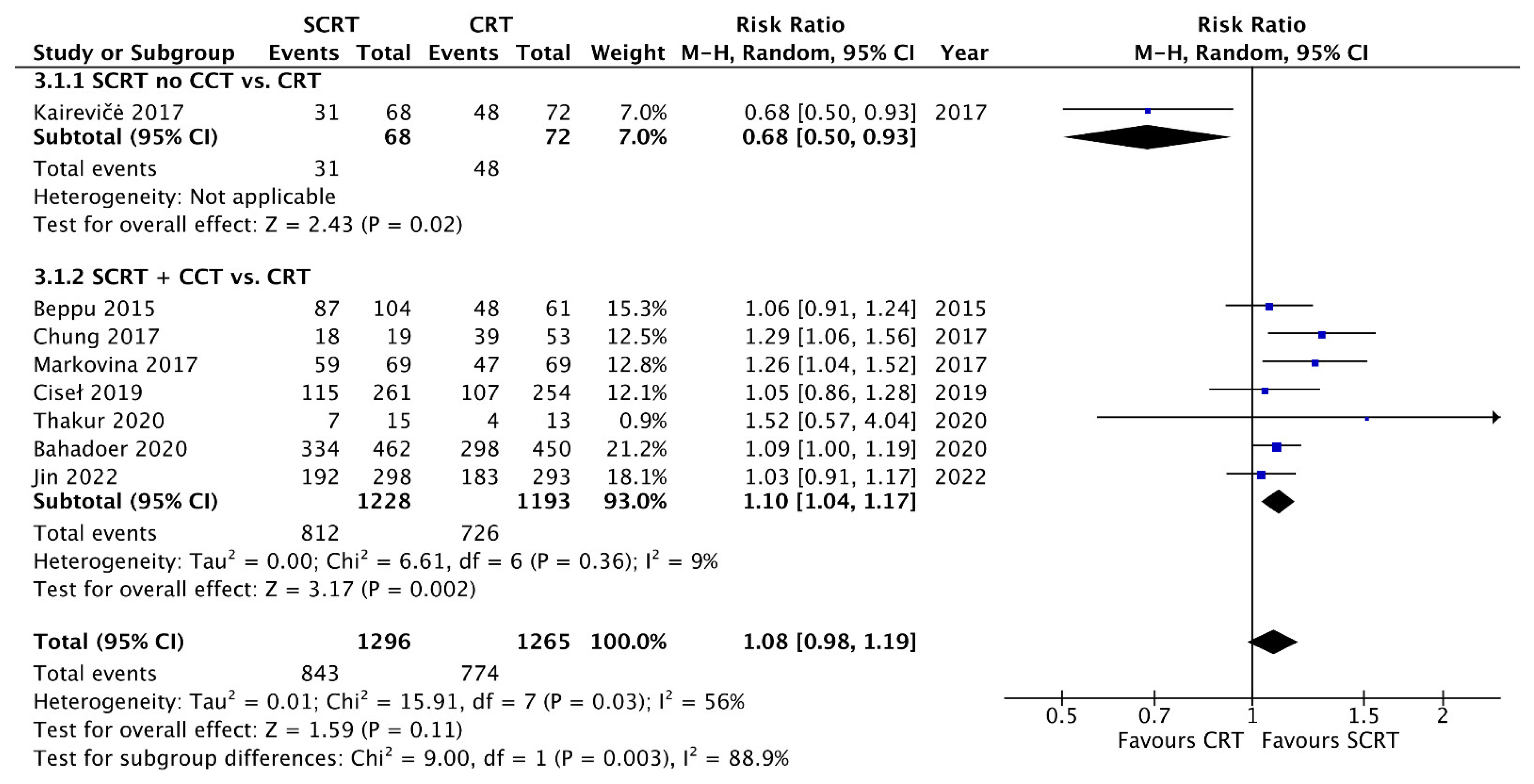
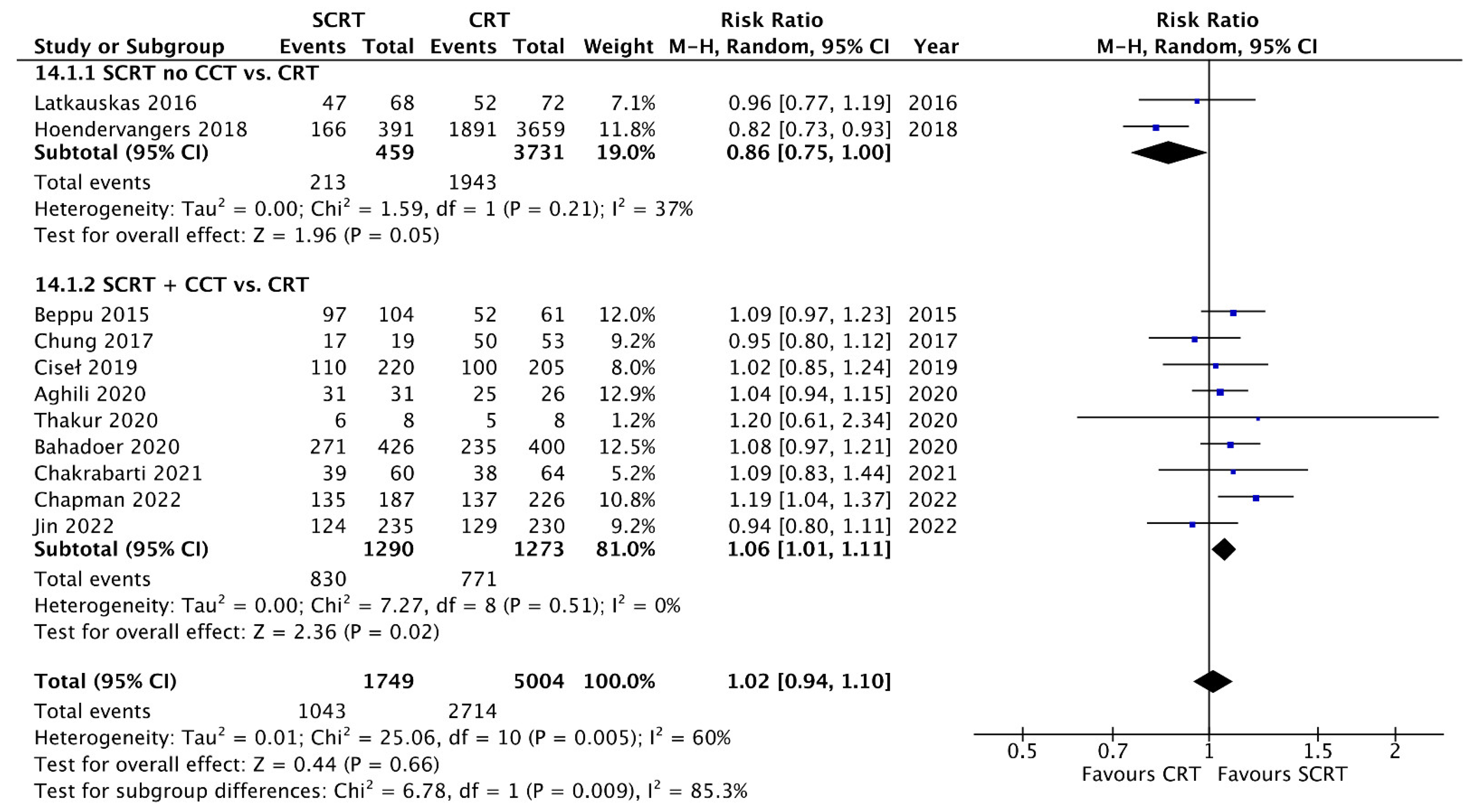
3.6. R0 Resection, Negative CRM, Sphincter-Preservation Rate, and Postoperative Complications
3.7. Acute Toxicity, Late Toxicity, and Compliance of Treatment
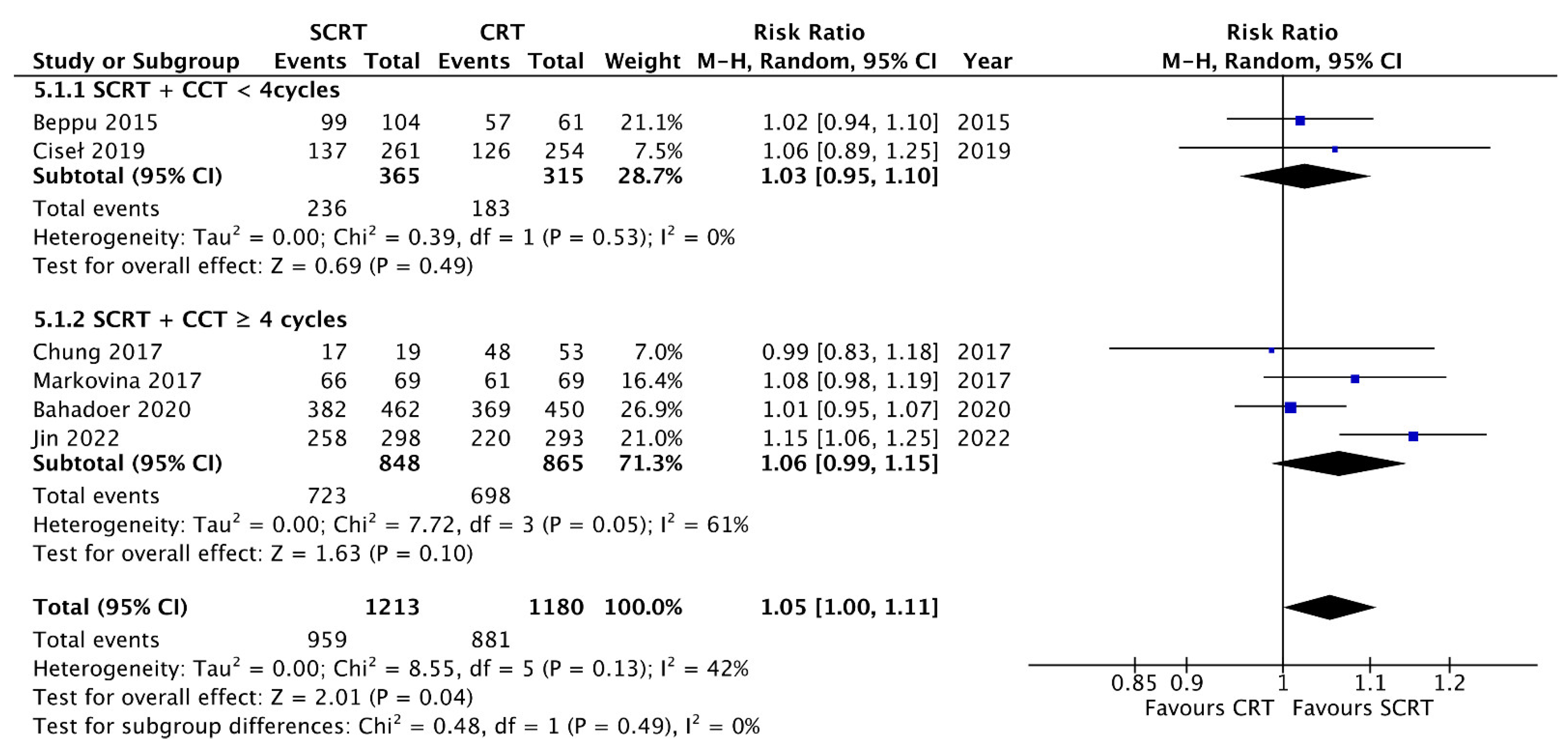
3.8. Subgroup Analysis according to the Consolidation Chemotherapy Cycle
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: Globocan Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Heald, R.J.; Ryall, R.D.H. Recurrence and Survival after Total Mesorectal Excision for Rectal Cancer. Lancet 1986, 327, 1479–1482. [Google Scholar] [CrossRef]
- Yoo, R.N.; Kim, H.J. Total neoadjuvant therapy in locally advanced rectal cancer: Role of systemic chemotherapy. Ann. Gastroenterol. Surg. 2019, 3, 356–367. [Google Scholar] [CrossRef] [PubMed]
- Swedish Rectal Cancer Trial. Improved survival with preoperative radiotherapy in resectable rectal cancer. N. Engl. J. Med. 1997, 336, 980–987. [Google Scholar] [CrossRef] [PubMed]
- Peeters, K.C.; Marijnen, C.; Nagtegaal, I.; Kranenbarg, E.M.-K.; Putter, H.; Wiggers, T.; Rutten, H.; Pahlman, L.; Glimelius, B.; Leer, J.W.; et al. The TME Trial After a Median Follow-up of 6 Years. Ann. Surg. 2007, 246, 693–701. [Google Scholar] [CrossRef]
- Benson, A.B.; Venook, A.P.; Al-Hawary, M.M.; Arain, M.A.; Chen, Y.-J.; Ciombor, K.K.; Cohen, S.; Cooper, H.S.; Deming, D.; Garrido-Laguna, I.; et al. NCCN Guidelines Insights: Rectal Cancer, Version 6.2020: Featured Updates to the NCCN Guidelines. J. Natl. Compr. Cancer Netw. 2020, 18, 806–815. [Google Scholar] [CrossRef]
- Glynne-Jones, R.; Wyrwicz, L.; Tiret, E.; Brown, G.; Rödel, C.; Cervantes, A.; Arnold, D. Rectal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2017, 28, iv22–iv40. [Google Scholar] [CrossRef]
- Bujko, K.; Nowacki, M.P.; Nasierowska-Guttmejer, A.; Michalski, W.; Bebenek, M.; Kryj, M. Long-term results of a randomized trial comparing preoperative short-course radiotherapy with preoperative conventionally fractionated chemoradiation for rectal cancer. Br. J. Surg. 2006, 93, 1215–1223. [Google Scholar] [CrossRef]
- Ngan, S.Y.; Burmeister, B.; Fisher, R.J.; Solomon, M.; Goldstein, D.; Joseph, D.; Ackland, S.P.; Schache, D.; McClure, B.; McLachlan, S.; et al. Randomized Trial of Short-Course Radiotherapy Versus Long-Course Chemoradiation Comparing Rates of Local Recurrence in Patients with T3 Rectal Cancer: Trans-Tasman Radiation Oncology Group Trial 01.04. J. Clin. Oncol. 2012, 30, 3827–3833. [Google Scholar] [CrossRef]
- Sauer, R.; Liersch, T.; Merkel, S.; Fietkau, R.; Hohenberger, W.; Hess, C.; Becker, H.; Raab, H.-R.; Villanueva, M.-T.; Witzigmann, H.; et al. Preoperative Versus Postoperative Chemoradiotherapy for Locally Advanced Rectal Cancer: Results of the German CAO/ARO/AIO-94 Randomized Phase III Trial After a Median Follow-Up of 11 Years. J. Clin. Oncol. 2012, 30, 1926–1933. [Google Scholar] [CrossRef]
- Pettersson, D.; Lörinc, E.; Holm, T.; Iversen, H.; Cedermark, B.; Glimelius, B.; Martling, A. Tumour regression in the randomized Stockholm III Trial of radiotherapy regimens for rectal cancer. Br. J. Surg. 2015, 102, 972–978. [Google Scholar] [CrossRef] [PubMed]
- Erlandsson, J.; Holm, T.; Pettersson, D.; Berglund, A.; Cedermark, B.; Radu, C.; Johansson, H.; Machado, M.; Hjern, F.; Hallböök, O.; et al. Optimal fractionation of preoperative radiotherapy and timing to surgery for rectal cancer (Stockholm III): A multicentre, randomised, non-blinded, phase 3, non-inferiority trial. Lancet Oncol. 2017, 18, 336–346. [Google Scholar] [CrossRef]
- Latkauskas, T.; Pauzas, H.; Kairevice, L.; Petrauskas, A.; Saladzinskas, Z.; Janciauskiene, R.; Gudaityte, J.; Lizdenis, P.; Svagzdys, S.; Tamelis, A.; et al. Preoperative conventional chemoradiotherapy versus short-course radiotherapy with delayed surgery for rectal cancer: Results of a randomized controlled trial. BMC Cancer 2016, 16, 927. [Google Scholar] [CrossRef] [PubMed]
- Bujko, K.; Wyrwicz, L.; Rutkowski, A.; Malinowska, M.; Pietrzak, L.; Kryński, J.; Michalski, W.; Olędzki, J.; Kuśnierz, J.; Zajac, L.; et al. Long-course oxaliplatin-based preoperative chemoradiation versus 5 × 5 Gy and consolidation chemotherapy for cT4 or fixed cT3 rectal cancer: Results of a randomized phase III study. Ann. Oncol. 2016, 27, 834–842. [Google Scholar] [CrossRef]
- Markovina, S.; Youssef, F.; Roy, A.; Aggarwal, S.; Khwaja, S.; DeWees, T.; Tan, B.; Hunt, S.; Myerson, R.J.; Chang, D.T.; et al. Improved Metastasis- and Disease-Free Survival with Preoperative Sequential Short-Course Radiation Therapy and FOLFOX Chemotherapy for Rectal Cancer Compared with Neoadjuvant Long-Course Chemoradiotherapy: Results of a Matched Pair Analysis. Int. J. Radiat. Oncol. Biol. Phys. 2017, 99, 417–426. [Google Scholar] [CrossRef]
- Chung, M.J.; Kim, D.W.; Chung, W.K.; Lee, S.H.; Jeong, S.K.; Hwang, J.K.; Jeong, C.S. Preoperative short- vs. long-course chemoradiotherapy with delayed surgery for locally advanced rectal cancer. Oncotarget 2016, 8, 60479–60486. [Google Scholar] [CrossRef][Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 88, 105906. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2021, 25, 603–605. [Google Scholar] [CrossRef]
- Kairevičė, L.; Latkauskas, T.; Tamelis, A.; Petrauskas, A.; Paužas, H.; Žvirblis, T.; Jaruševičius, L.; Saladžinskas, Ž.; Pavalkis, D.; Jančiauskienė, R. Preoperative Long-Course Chemoradiotherapy plus Adjuvant Chemotherapy versus Short-Course Radiotherapy without Adjuvant Chemotherapy Both with Delayed Surgery for Stage II–III Resectable Rectal Cancer: 5-Year Survival Data of a Randomized Controlled Trial. Medicina 2017, 53, 150–158. [Google Scholar] [CrossRef]
- Hoendervangers, S.; Couwenberg, A.M.; Intven, M.P.W.; van Grevenstein, W.M.U.; Verkooijen, H.M. Comparison of Pathological Complete Response Rates after Neoadjuvant Short-Course Radiotherapy or Chemoradiation Followed by Delayed Surgery in Locally Advanced Rectal Cancer. Eur. J. Surg. Oncol. 2018, 44, 1013–1017. [Google Scholar] [CrossRef] [PubMed]
- Xiao, J.; Teng, W.H.; Liu, S.; Wei, C.; Liu, W.J.; Chen, S.; Zang, W.D. Short-course radiotherapy with delayed surgery versus conventional chemoradiotherapy: Comparison of short-term outcomes in patients with T3-4 rectal cancer. Int. J. Clin. Exp. Med. 2018, 11, 12149–12156. [Google Scholar]
- Hoendervangers, S.; Sparreboom, C.L.; Intven, M.P.W.; Lange, J.F.; Verkooijen, H.M.; Doornebosch, P.G.; Grevenstein, W.M.U.; the Dutch ColoRectal Audit. The Effect of Neoadjuvant Short-Course Radiotherapy and Delayed Surgery versus Chemoradiation on Postoperative Outcomes in Locally Advanced Rectal Cancer Patients—A Propensity Score Matched Nationwide Audit-Based Study. Eur. J. Surg. Oncol. 2020, 46, 1605–1612. [Google Scholar] [CrossRef] [PubMed]
- Ciseł, B.; Pietrzak, L.; Michalski, W.; Wyrwicz, L.; Rutkowski, A.; Kosakowska, E.; Cencelewicz, A.; Spałek, M.; Polkowski, W.; Jankiewicz, M.; et al. Long-course preoperative chemoradiation versus 5 × 5 Gy and consolidation chemotherapy for clinical T4 and fixed clinical T3 rectal cancer: Long-term results of the randomized Polish II study. Ann. Oncol. 2019, 30, 1298–1303. [Google Scholar] [CrossRef]
- Beppu, N.; Matsubara, N.; Noda, M.; Yamano, T.; Kakuno, A.; Doi, H.; Kamikonya, N.; Kimura, F.; Yamanaka, N.; Yanagi, H.; et al. Short-Course Radiotherapy with Delayed Surgery versus Conventional Chemoradiotherapy: A Comparison of the Short- and Long-Term Outcomes in Patients with T3 Rectal Cancer. Surgery 2015, 158, 225–235. [Google Scholar] [CrossRef]
- Aghili, M.; Khalili, N.; Khalili, N.; Babaei, M.; Farhan, F.; Haddad, P.; Salarvand, S.; Keshvari, A.; Fazeli, M.S.; Mohammadi, N.; et al. Short-Course versus Long-Course Neoadjuvant Chemoradiotherapy in Patients with Rectal Cancer: Preliminary Results of a Randomized Controlled Trial. Radiat. Oncol. J. 2020, 38, 119–128. [Google Scholar] [CrossRef]
- Thakur, N.; Seam, R.K.; Gupta, M.K.; Gupta, M.; Fotedar, V.; Vats, S.; Rana, S.; Vias, P.; Ahuja, R. A Prospective Observational Study Comparing Long-Course Conventional Neoadjuvant Chemoradiotherapy with Short-Course Radiotherapy Followed by Consolidation Chemotherapy with Delayed Surgery in Locally Advanced Rectal Cancer. South Asian J. Cancer 2020, 9, 80–85. [Google Scholar] [CrossRef]
- van der Valk, M.J.; Marijnen, C.A.; van Etten, B.; Dijkstra, E.A.; Hilling, D.E.; Kranenbarg, E.M.-K.; Putter, H.; Roodvoets, A.G.; Bahadoer, R.R.; Fokstuen, T.; et al. Compliance and Tolerability of Short-Course Radiotherapy Followed by Preoperative Chemotherapy and Surgery for High-Risk Rectal Cancer—Results of the International Randomized RAPIDO-Trial. Radiother. Oncol. 2020, 147, 75–83. [Google Scholar] [CrossRef]
- Bahadoer, R.R.; Dijkstra, A.E.; van Etten, B.; Marijnen, C.A.M.; Putter, H.; Kranenbarg, E.M.-K.; Roodvoets, A.G.H.; Nagtegaal, I.D.; Beets-Tan, R.G.H.; Blomqvist, L.K.; et al. Short-Course Radiotherapy Followed by Chemotherapy before Total Mesorectal Excision (TME) versus Preoperative Chemoradiotherapy, TME, and Optional Adjuvant Chemotherapy in Locally Advanced Rectal Cancer (RAPIDO): A Randomised, Open-Label, Phase 3 Trial. Lancet Oncol. 2021, 22, 29–42. [Google Scholar] [CrossRef]
- Chakrabarti, D.; Rajan, S.; Akhtar, N.; Qayoom, S.; Gupta, S.; Verma, M.; Srivastava, K.; Kumar, V.; Bhatt, M.L.B.; Gupta, R. Short-Course Radiotherapy with Consolidation Chemotherapy versus Conventionally Fractionated Long-Course Chemoradiotherapy for Locally Advanced Rectal Cancer: Randomized Clinical Trial. Br. J. Surg. 2021, 108, 511–520. [Google Scholar] [CrossRef]
- Chapman, W.C.; Kim, H.; Bauer, P.; Makhdoom, B.A.; Trikalinos, N.A.; Pedersen, K.S.; Glasgow, S.C.; Mutch, M.G.; Silviera, M.L.; Roy, A.; et al. Total Neoadjuvant Therapy with Short-Course Radiation: US Experience of a Neoadjuvant Rectal Cancer Therapy. Dis. Colon Rectum 2022, 65, 198–206. [Google Scholar] [CrossRef] [PubMed]
- Jin, J.; Tang, Y.; Hu, C.; Jiang, L.-M.; Jiang, J.; Li, N.; Liu, W.-Y.; Chen, S.-L.; Li, S.; Lu, N.-N.; et al. Multicenter, Randomized, Phase III Trial of Short-Term Radiotherapy Plus Chemotherapy Versus Long-Term Chemoradiotherapy in Locally Advanced Rectal Cancer (STELLAR). J. Clin. Oncol. 2022, 40, JCO2101667. [Google Scholar] [CrossRef] [PubMed]
- Sell, N.M.; Qwaider, Y.Z.; Goldstone, R.N.; Cauley, C.E.; Cusack, J.C.; Ricciardi, R.; Bordeianou, L.G.; Berger, D.L.; Kunitake, H. Ten-year Survival after Pathologic Complete Response in Rectal Adenocarcinoma. J. Surg. Oncol. 2021, 123, 293–298. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Huang, X.; Gao, P.; Song, Y.; Chen, X.; Lv, X.; Fu, Y.; Xiao, Q.; Ye, S.; Wang, Z. Survival Landscape of Different Tumor Regression Grades and Pathologic Complete Response in Rectal Cancer after Neoadjuvant Therapy Based on Reconstructed Individual Patient Data. BMC Cancer 2021, 21, 1214. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Aguilar, J.; Chow, O.S.; Smith, D.D.; Marcet, J.E.; Cataldo, P.A.; Varma, M.G.; Kumar, A.S.; Oommen, S.; Coutsoftides, T.; Hunt, S.R.; et al. Effect of Adding MFOLFOX6 after Neoadjuvant Chemoradiation in Locally Advanced Rectal Cancer: A Multicentre, Phase 2 Trial. Lancet Oncol. 2015, 16, 957–966. [Google Scholar] [CrossRef]
- van der Valk, M.J.M.; Hilling, D.; Bastiaannet, E.; Kranenbarg, E.M.-K.; Beets, G.L.; Figueiredo, N.; Habr-Gama, A.; O Perez, R.; Renehan, A.G.; van de Velde, C.J.H.; et al. Long-Term Outcomes of Clinical Complete Responders after Neoadjuvant Treatment for Rectal Cancer in the International Watch & Wait Database (IWWD): An International Multicentre Registry Study. Lancet 2018, 391, 2537–2545. [Google Scholar] [CrossRef]
- Coraglio, M.F.; Eleta, M.A.; Kujaruk, M.R.; Oviedo, J.H.; Roca, E.L.; Masciangioli, G.A.; Mendez, G.; Iseas, I.S. Analysis of Long-Term Oncological Results of Clinical versus Pathological Responses after Neoadjuvant Treatment in Locally Advanced Rectal Cancer. World J. Surg. Oncol. 2020, 18, 313. [Google Scholar] [CrossRef]
- Jimenez-Fonseca, P.; Salazar, R.; Valenti, V.; Msaouel, P.; Carmona-Bayonas, A. Is Short-Course Radiotherapy and Total Neoadjuvant Therapy the New Standard of Care in Locally Advanced Rectal Cancer? A Sensitivity Analysis of the RAPIDO Clinical Trial. Ann. Oncol. 2022. [Google Scholar] [CrossRef]
- Marco, M.R.; Zhou, L.; Patil, S.; Marcet, J.E.; Varma, M.G.; Oommen, S.; Cataldo, P.A.; Hunt, S.R.; Kumar, A.; Herzig, D.O.; et al. Consolidation MFOLFOX6 Chemotherapy After Chemoradiotherapy Improves Survival in Patients with Locally Advanced Rectal Cancer. Dis. Colon Rectum 2018, 61, 1146–1155. [Google Scholar] [CrossRef]
- Liang, H.-Q.; Dong, Z.-Y.; Liu, Z.-J.; Luo, J.; Zeng, Q.; Liao, P.-Y.; Wu, D.-H. Efficacy and Safety of Consolidation Chemotherapy during the Resting Period in Patients with Local Advanced Rectal Cancer. Oncol. Lett. 2019, 17, 1655–1663. [Google Scholar] [CrossRef]
- Thavaneswaran, S.; Kok, P.S.; Price, T. Evaluating the addition of oxaliplatin to single agent fluoropyrimidine in the treatment of locally advanced rectal cancer: A systematic review and meta-analysis. Expert Rev. Anticancer Ther. 2017, 17, 965–979. [Google Scholar] [CrossRef] [PubMed]
- Bahadoer, R.; Dijkstra, E. Patterns of Locoregional Failure and Distant Metastases in Patients Treated for Locally Advanced Rectal Cancer in the RAPIDO Trial. Eur. J. Surg. Oncol. 2022, 48, e34. [Google Scholar] [CrossRef]
- Song, J.H.; Lee, J.H.; Kim, S.H.; Um, J.W. Oxaliplatin-Based Adjuvant Chemotherapy Rather than Fluorouracil-Based Chemotherapy in Rectal Cancer Is More Efficient to Decrease Distant Metastasis and Increase Survival after Preoperative Chemoradiotherapy and Surgery: A Meta-Analysis. Int. J. Colorectal Dis. 2022, 37, 649–656. [Google Scholar] [CrossRef] [PubMed]
- Mari, G.M.; Maggioni, D.; Crippa, J.; Costanzi, A.T.M.; Scotti, M.A.; Giardini, V.; Garancini, M.; Cocozza, E.; Borroni, G.; Benzoni, I.; et al. Compliance to Adjuvant Chemotherapy of Patients Who Underwent Surgery for Rectal Cancer: Report from a Multi-Institutional Research Network. World J. Surg. 2019, 43, 2544–2551. [Google Scholar] [CrossRef] [PubMed]
- Diefenhardt, M.; Ludmir, E.B.; Hofheinz, R.-D.; Ghadimi, M.; Minsky, B.D.; Rödel, C.; Fokas, E. Association of Treatment Adherence with Oncologic Outcomes for Patients with Rectal Cancer. JAMA Oncol. 2020, 6, 1416–1421. [Google Scholar] [CrossRef]
- Wang, S.; Wen, F.; Zhang, P.; Wang, X.; Li, Q. Cost-effectiveness analysis of long-course oxaliplatin and bolus of fluorouracil based preoperative chemoradiotherapy vs. 5 × 5Gy radiation plus FOLFOX4 for locally advanced resectable rectal cancer. Radiat. Oncol. 2019, 14, 113. [Google Scholar] [CrossRef]
- Conroy, T.; Bosset, J.-F.; Etienne, P.-L.; Rio, E.; François, É.; Mesgouez-Nebout, N.; Vendrely, V.; Artignan, X.; Bouché, O.; Gargot, D.; et al. Neoadjuvant Chemotherapy with FOLFIRINOX and Preoperative Chemoradiotherapy for Patients with Locally Advanced Rectal Cancer (UNICANCER-PRODIGE 23): A Multicentre, Randomised, Open-Label, Phase 3 Trial. Lancet Oncol. 2021, 22, 702–715. [Google Scholar] [CrossRef]
- Fokas, E.; Allgäuer, M.; Polat, B.; Klautke, G.; Grabenbauer, G.G.; Fietkau, R.; Kuhnt, T.; Staib, L.; Brunner, T.; Grosu, A.-L.; et al. Randomized Phase II Trial of Chemoradiotherapy Plus Induction or Consolidation Chemotherapy as Total Neoadjuvant Therapy for Locally Advanced Rectal Cancer: CAO/ARO/AIO-12. J. Clin. Oncol. 2019, 37, 3212–3222. [Google Scholar] [CrossRef]
- Fokas, E.; Schlenska-Lange, A.; Polat, B.; Klautke, G.; Grabenbauer, G.G.; Fietkau, R.; Kuhnt, T.; Staib, L.; Brunner, T.; Grosu, A.-L.; et al. Chemoradiotherapy Plus Induction or Consolidation Chemotherapy as Total Neoadjuvant Therapy for Patients with Locally Advanced Rectal Cancer. JAMA Oncol. 2022, 8, e215445. [Google Scholar] [CrossRef]
- Kasi, A.; Abbasi, S.; Handa, S.; Al-Rajabi, R.; Saeed, A.; Baranda, J.; Sun, W. Total Neoadjuvant Therapy vs Standard Therapy in Locally Advanced Rectal Cancer. JAMA Netw. Open 2020, 3, e2030097. [Google Scholar] [CrossRef]
- ClinicalTrials.Gov. Available online: https://clinicaltrials.gov/ct2/show/NCT04246684 (accessed on 6 May 2022).



| Study | Enrollment Years | Study Design | Staging | Intervention | Patient Numbers (male%) | Age (Years) | RT Dose | CT Regimen | Interval (Weeks) | ACT Regimen (Completion%) | Follow Up Time (Months) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Latkauskas 2016 [13] | 2007–2013 | RCTs | II–III | SCRT | 68 (63%) | 65.6 | 25 | No | 6–8 | no | 39.7 |
| CRT | 72 (68%) | 63.1 | 50 | Infusion 5FU/LV | 6–8 | Infusion 5FU/LV (72%) | |||||
| Kairevičė 2017 [20] | 2007–2013 | RCTs | II–III | SCRT | 68 (63%) | 65.6 | 25 | No | 6–8 | no | 60.5 |
| CRT | 72 (68%) | 63.1 | 50 | Infusion 5FU/LV | 6–8 | Infusion 5FU/LV (72%) | |||||
| Bujko 2016 [14] | 2008–2014 | RCTs | cT3–4 | SCRT | 261 (70%) | 60 | 25 | FOLFOX × 3 | 12 | oxaliplatin-based (15%) | 35 |
| CRT | 254 (66%) | 59 | 50.4 | Infusion 5FU/LV + Oxaliplatin × 2 | 6 | oxaliplatin-based (11%) | |||||
| Ciseł 2019 [24] | 2008–2014 | RCTs | cT3–4 | SCRT | 261 (70%) | 60 | 25 | FOLFOX × 3 | 12 | No | 7 years |
| CRT | 254 (66%) | 59 | 50.4 | Infusion 5FU/LV + Oxaliplatin × 2 | 6 | No | |||||
| Beppu 2015 [25] | 2007–2013 | retrospective | cT3 | SCRT | 106 (68%) | 61 | 25 | S1 × 10days | 4 | Oral 5-FU (83.7%) | 44 |
| CRT | 61 (73%) | 63 | 45 | S1 + CPT-11 | 6–10 | Oral 5-FU (77%) | 45 | ||||
| Chung 2017 [16] | 2010–2015 | retrospective | II–III | SCRT | 19 (52%) | 72 | 25 | Infusion 5FU/LV × 4 | 8 | Infusion 5 FU/LV (57.9%) | 25 |
| CRT | 53 (71%) | 72 | 50.4 | Infusion 5FU/LV | 8 | Infusion 5FU/LV or Xeloda (73.6%) | 25 | ||||
| Markovina 2017 [15] | 2009–2012 | Phase II trial | cT3–4 | SCRT | 69 (71%) | 57.2 | 25 | FOLFOX × 6 | 4–9 | NA (86%) | 49.4 |
| CRT | 69 (67%) | 56.6 | 40–48 | 5-FU or capecitabine | 6–8 | FOLFOX (100%) | 54.3 | ||||
| Chapman 2022 [31] | 2009–2018 | retrospectivr | II–III | SCRT | 187 (62%) | NA | 25 | FOLFOX 2–6 months | 4 | NA (60.1%) | 28.3 |
| CRT | 226 (67%) | NA | 45–55 | 5-FU | 4 | Oxalipaltin + 5 FU (82.3%) | 41.6 | ||||
| Hoendervangers 2018 [21] | 2008–2014 | retrospective | II–III | SCRT | 391 (50%) | 76 | 25 | No | 9.1 | NA | 2.4 years |
| CRT | 3659 (64%) | 63 | 45–50 | capecitabine | 9.4 | NA | 3.2 years | ||||
| Xiao 2018 [22] | 2014–2017 | RCTs | II–III | SCRT | 98 (48%) | 59.6 | 25 | No | 6–8 | No | NA |
| CRT | 98 (58%) | 59.0 | 50 | Infusion 5FU/LV | 6–8 | 5FU/LV | |||||
| Aghili 2020 [26] | 2016–2020 | RCTs | II–III | SCRT | 33 (55%) | 56 | 25 | Xelox × 3–4 | 8 | NA | 6 |
| CRT | 27 (62%) | 53 | 50–50.4 | Xeloda + Xelox | 8 | NA | 6 | ||||
| Hoendervangers 2020 [23] | 2014–2017 | retrospective | II–III | SCRT | 246 (58%) | 76.7 | 25 | No | 11 | NA | NA |
| CRT | 246 (66%) | 75.9 | 45–50 | capecitabine | 11 | NA | |||||
| Thakur 2020 [27] | 2015–2016 | Prospective | cT3–4 | SCRT | 15 | NA | 25 | Capecitabine + Oxaliplatin × 2 | 4–6 | NA | 22.6 |
| CRT | 13 | NA | 45 | capecitabine | 4–6 | NA | |||||
| van der Valk 2020 [28] | 2011–2016 | RCTs | * cT4, cN2 | SCRT | 460 (65%) | 61 | 25 | FOLFOX × 9 or Capox × 6 | 2–4 | no | NA |
| CRT | 441 (69%) | 61 | 50.4 | capecitabine | 6–8 | CAPOX or FOLFOX | |||||
| Bahadoer 2020 [29] | 2011–2016 | RCTs | * cT4, cN2 | SCRT | 462 (65%) | 62 | 25 | FOLFOX × 9 or Capox × 6 | 2–4 | no | 4.6 years |
| CRT | 450 (69%) | 62 | 50.4 | capecitabine | 6–8 | CAPOX or FOLFOX (47%) | |||||
| Chakrabarti 2021 [30] | 2017–2019 | RCTs | II–III | SCRT | 69 (67%) | 42 | 25 | Capox × 2 | 6–8 | CAPOX (85%) | NA |
| CRT | 71 (66%) | 43 | 50.4 | capecitabine | 8–12 | CAPOX (52%) | |||||
| Jin 2022 [32] | 2015–2018 | RCTs | II–III | SCRT | 302 (72%) | 55 | 25 | CAPOX × 4 | 6–8 | CAPOX ×2 (60%) | 35 |
| CRT | 297 (70%) | 56 | 50 | capecitabine | 6–8 | CAPOX ×6 (48%) |
| Selection | Comparability | Exposure | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Author | Representativeness of the Exposed Cohort | Selection of the Nonexposed Cohort | Ascertainment of Exposure | Demonstration That the Outcome of Interest Was Not Present at the Start of the Study | Comparability of Cohorts Based on the Design or Analysis | Assessment of Outcome | Was Follow-Up Long Enough for Outcomes to Occur | Adequacy of the Follow-Up of Cohorts | NOS |
| Beppu 2015 [25] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Chung 2017 [16] | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| Markovina 2017 [15] | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| Hoendervangers 2018 [21] | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| Hoendervangers 2020 [23] | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| Thakur 2020 [27] | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| Chapman 2022 [31] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Study | Intervention | pCR Rate | Downstaging Rate | R0 Resection Rate | Sphincter Preservation | OS | DFS |
|---|---|---|---|---|---|---|---|
| Latkauskas 2016 [13] | SCRT | 4.4 | 30.9 | 86.5 | 70.3 | 78.0 (3-year) | 59.0 (3-year) |
| CRT | 11.1 | 37.5 | 91.3 | 69.6 | 82.4 (3-year) | 75.1 (3-year) | |
| Kairevičė 2017 [20] | SCRT | 62 (5-year) | 45 (5-year) | ||||
| CRT | 79 (5-year) | 67 (5-year) | |||||
| Bujko 2016 [14] | SCRT | 16 | NA | 77 | 43 | 73 (3-year) | 53 (3-year) |
| CRT | 12 | NA | 71 | 39 | 65 (3-year) | 52 (3-year) | |
| Ciseł 2019 [24] | SCRT | 49 (8-year) | 43 (8-year) | ||||
| CRT | 49 (8-year) | 41 (8-year) | |||||
| Beppu 2015 [25] | SCRT | 4.8 | 37.5 | NA | 93.3 | 95.1 (3-year) | 83.8 (3-year) |
| CRT | 8.2 | 37.7 | NA | 85.2 | 93.1 (3-year) | 73.8 (3-year) | |
| Chung 2017 [16] | SCRT | 21.1 | 47.4 | NA | 89.5 | 90 (2-year) | 93.8 (2-year) |
| CRT | 13.2 | 26.4 | NA | 94.3 | 91.2 (2-year) | 74.0 (2-year) | |
| Markovina 2017 [15] | SCRT | 28 | 75 | NA | 75.4 | 96 (3-year) | 85 (3-year) * |
| CRT | 16 | 41 | NA | 72.5 | 88 (3-year) | 68 (3-year) | |
| Chapman 2022 [31] | SCRT | 26.2 | NA | 94.2 | 72.3 | NA | NA |
| CRT | 17.3 | NA | 89.8 | 60.6 | NA | NA | |
| Hoendervangers 2018 [21] | SCRT | 6.4 | 46.8 | NA | 42.5 | NA | NA |
| CRT | 16.2 | 56.1 | NA | 51.7 | NA | NA | |
| Xiao 2018 [22] | SCRT | 7.14 | 21.43 | NA | NA | NA | NA |
| CRT | 11.22 | 25.51 | NA | NA | NA | NA | |
| Aghili 2020 [26] | SCRT | 32.3 | 80.8 | 100 | 100 | NA | NA |
| CRT | 23.1 | 84.6 | 96.2 | 96.2 | NA | NA | |
| Hoendervangers 2020 [23] | SCRT | 7.7 | NA | 91.9 | NA | NA | NA |
| CRT | 12.6 | NA | 89 | NA | NA | NA | |
| Thakur 2020 [27] | SCRT | 6.7 | 35.7 | 92.8 | 75 | NA | NA |
| CRT | 0 | 53.8 | 92.3 | 62.5 | NA | NA | |
| Bahadoer 2020 [29] | SCRT | 28 | NA | 90 | 63.6 | 89.1 (3-year) | 23.7 (3-year DRTF) |
| CRT | 14 | NA | 90 | 58.8 | 88.8 (3-year) | 30.4 (3-year DRTF) | |
| Chakrabarti 2021 [30] | SCRT | 13.3 | 75.4 | 100 | 65 | NA | NA |
| CRT | 10.9 | 74.6 | 100 | 59.4 | NA | NA | |
| Jin 2022 [32] | SCRT | 16.6 | NA | 91.5 | 52.8 | 86.5 (3-year) | 64.5 (3-year) |
| CRT | 11.7 | NA | 87.8 | 56.1 | 75.1 (3-year) | 62.3 (3-year) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liao, C.-K.; Kuo, Y.-T.; Lin, Y.-C.; Chern, Y.-J.; Hsu, Y.-J.; Yu, Y.-L.; Chiang, J.-M.; Hsieh, P.-S.; Yeh, C.-Y.; You, J.-F. Neoadjuvant Short-Course Radiotherapy Followed by Consolidation Chemotherapy before Surgery for Treating Locally Advanced Rectal Cancer: A Systematic Review and Meta-Analysis. Curr. Oncol. 2022, 29, 3708-3727. https://doi.org/10.3390/curroncol29050297
Liao C-K, Kuo Y-T, Lin Y-C, Chern Y-J, Hsu Y-J, Yu Y-L, Chiang J-M, Hsieh P-S, Yeh C-Y, You J-F. Neoadjuvant Short-Course Radiotherapy Followed by Consolidation Chemotherapy before Surgery for Treating Locally Advanced Rectal Cancer: A Systematic Review and Meta-Analysis. Current Oncology. 2022; 29(5):3708-3727. https://doi.org/10.3390/curroncol29050297
Chicago/Turabian StyleLiao, Chun-Kai, Ya-Ting Kuo, Yueh-Chen Lin, Yih-Jong Chern, Yu-Jen Hsu, Yen-Lin Yu, Jy-Ming Chiang, Pao-Shiu Hsieh, Chien-Yuh Yeh, and Jeng-Fu You. 2022. "Neoadjuvant Short-Course Radiotherapy Followed by Consolidation Chemotherapy before Surgery for Treating Locally Advanced Rectal Cancer: A Systematic Review and Meta-Analysis" Current Oncology 29, no. 5: 3708-3727. https://doi.org/10.3390/curroncol29050297
APA StyleLiao, C.-K., Kuo, Y.-T., Lin, Y.-C., Chern, Y.-J., Hsu, Y.-J., Yu, Y.-L., Chiang, J.-M., Hsieh, P.-S., Yeh, C.-Y., & You, J.-F. (2022). Neoadjuvant Short-Course Radiotherapy Followed by Consolidation Chemotherapy before Surgery for Treating Locally Advanced Rectal Cancer: A Systematic Review and Meta-Analysis. Current Oncology, 29(5), 3708-3727. https://doi.org/10.3390/curroncol29050297





