An Epidemiological Update on Indoor Tanning and the Risk of Skin Cancers
Abstract
1. Introduction
2. Epidemiology of Sunbed Use: Variation across Countries and among Individuals
3. Motivations and Influences for Sunbed Use
4. Sunbed Use and Risk of Cutaneous Melanoma
5. Sunbed Use and Risk of Keratinocyte Carcinoma (cSCC and BCC)
6. Preventive Measures against Sunbed Use
6.1. Restrictive Legislation
6.2. Educational Campaigns
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Calzavara-Pinton, P.G.; Arisi, M.; Wolf, P. Sunbeds and carcinogenesis: The need for new regulations and restrictions in Europe from the Euromelanoma perspective. J. Eur. Acad. Derm. Venereol. 2019, 33 (Suppl. 2), 104–109. [Google Scholar] [CrossRef] [PubMed]
- Dessinioti, C.; Stratigos, A.J.; Rigopoulos, D.; Katsambas, A.D. A review of genetic disorders of hypopigmentation: Lessons learned from the biology of melanocytes. Exp. Derm. 2009, 18, 741–749. [Google Scholar] [CrossRef]
- Lin, J.Y.; Fisher, D.E. Melanocyte biology and skin pigmentation. Nature 2007, 445, 843–850. [Google Scholar] [CrossRef]
- Flanagan, N.; Healy, E.; Ray, A.; Philips, S.; Todd, C.; Jackson, I.J.; Birch-Machin, M.A.; Rees, J.L. Pleiotropic effects of the melanocortin 1 receptor (MC1R) gene on human pigmentation. Hum. Mol. Genet. 2000, 9, 2531–2537. [Google Scholar] [CrossRef]
- Dessinioti, C.; Antoniou, C.; Katsambas, A.; Stratigos, A.J. Melanocortin 1 receptor variants: Functional role and pigmentary associations. Photochem. Photobiol. 2011, 87, 978–987. [Google Scholar] [CrossRef] [PubMed]
- Dessinioti, C.; Antoniou, C.; Katsambas, A.; Stratigos, A.J. Basal cell carcinoma: What’s new under the sun. Photochem. Photobiol. 2010, 86, 481–491. [Google Scholar] [CrossRef] [PubMed]
- Kripke, M.L.; Cox, P.A.; Alas, L.G.; Yarosh, D.B. Pyrimidine dimers in DNA initiate systemic immunosuppression in UV-irradiated mice. Proc. Natl. Acad. Sci. USA 1992, 89, 7516–7520. [Google Scholar] [CrossRef]
- Walterscheid, J.P.; Ullrich, S.E.; Nghiem, D.X. Platelet-activating factor, a molecular sensor for cellular damage, activates systemic immune suppression. J. Exp. Med. 2002, 195, 171–179. [Google Scholar] [CrossRef]
- Noonan, F.P.; De Fabo, E.C. Immunosuppression by ultraviolet B radiation: Initiation by urocanic acid. Immunol. Today 1992, 13, 250–254. [Google Scholar] [CrossRef]
- Nilsen, L.T.; Hannevik, M.; Veierod, M.B. Ultraviolet exposure from indoor tanning devices: A systematic review. Br. J. Derm. 2016, 174, 730–740. [Google Scholar] [CrossRef]
- IARC Working Group on the Evluation of Carcinogenic Risks to Humans. A review of human carcinogens. Part D: Radiation. In IARC Monographs on the Evaluation of Carcinogenic Risks to Humans Series; WHO: Geneva, Switzerland, 2012; Available online: https://monographs.iarc.who.int/wp-content/uploads/2018/06/mono100D.pdf (accessed on 4 November 2022).
- Wehner, M.R.; Chren, M.M.; Nameth, D.; Choudhry, A.; Gaskins, M.; Nead, K.T.; Boscardin, W.J.; Linos, E. International prevalence of indoor tanning: A systematic review and meta-analysis. JAMA Derm. 2014, 150, 390–400. [Google Scholar] [CrossRef]
- Rodriguez-Acevedo, A.J.; Green, A.C.; Sinclair, C.; van Deventer, E.; Gordon, L.G. Indoor tanning prevalence after the International Agency for Research on Cancer statement on carcinogenicity of artificial tanning devices: Systematic review and meta-analysis. Br. J. Derm. 2020, 182, 849–859. [Google Scholar] [CrossRef]
- Suppa, M.; Gandini, S.; Njimi, H.; Bulliard, J.L.; Correia, O.; Duarte, A.F.; Peris, K.; Stratigos, A.J.; Nagore, E.; Longo, M.I.; et al. Prevalence and determinants of sunbed use in thirty European countries: Data from the Euromelanoma skin cancer prevention campaign. J. Eur. Acad. Derm. Venereol. 2019, 33 (Suppl. 2), 13–27. [Google Scholar] [CrossRef]
- Suppa, M.; Gandini, S.; Bulliard, J.L.; Daxhelet, M.; Zamagni, M.; Forsea, A.M.; Longo, M.I.; Del Marmol, V. Who, why, where: An overview of determinants of sunbed use in Europe. J. Eur. Acad. Derm. Venereol. 2019, 33 (Suppl. 2), 6–12. [Google Scholar] [CrossRef]
- Mastroeni, S.; Sampogna, F.; Salcedo, N.M.; Ricci, F.; Fania, L.; Antonelli, F.; Abeni, D.; Cristofolini, M. Factors associated with sunbed use among 3692 outpatients in 18 centers of the Italian Cancer League (LILT). Sci. Rep. 2021, 11, 23180. [Google Scholar] [CrossRef]
- Bataille, V.; Boniol, M.; De Vries, E.; Severi, G.; Brandberg, Y.; Sasieni, P.; Cuzick, J.; Eggermont, A.; Ringborg, U.; Grivegnee, A.R.; et al. A multicentre epidemiological study on sunbed use and cutaneous melanoma in Europe. Eur. J. Cancer 2005, 41, 2141–2149. [Google Scholar] [CrossRef]
- Boniol, M.; Autier, P.; Boyle, P.; Gandini, S. Cutaneous melanoma attributable to sunbed use: Systematic review and meta-analysis. BMJ 2012, 345, e4757. [Google Scholar] [CrossRef]
- Bentzen, J.; Krarup, A.F.; Castberg, I.M.; Jensen, P.D.; Philip, A. Determinants of sunbed use in a population of Danish adolescents. Eur. J. Cancer Prev. 2013, 22, 126–130. [Google Scholar] [CrossRef]
- Koster, B.; Thorgaard, C.; Clemmensen, I.H.; Philip, A. Sunbed use in the Danish population in 2007: A cross-sectional study. Prev. Med. 2009, 48, 288–290. [Google Scholar] [CrossRef]
- Krarup, A.F.; Koster, B.; Thorgaard, C.; Philip, A.; Clemmensen, I.H. Sunbed use by children aged 8-18 years in Denmark in 2008: A cross-sectional study. Br. J. Derm. 2011, 165, 214–216. [Google Scholar] [CrossRef]
- Boldeman, C.; Beitner, H.; Jansson, B.; Nilsson, B.; Ullen, H. Sunbed use in relation to phenotype, erythema, sunscreen use and skin diseases. A questionnaire survey among Swedish adolescents. Br. J. Derm. 1996, 135, 712–716. [Google Scholar] [CrossRef]
- Boldeman, C.; Jansson, B.; Nilsson, B.; Ullen, H. Sunbed use in Swedish urban adolescents related to behavioral characteristics. Prev. Med. 1997, 26, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Boldeman, C.; Branstrom, R.; Dal, H.; Kristjansson, S.; Rodvall, Y.; Jansson, B.; Ullen, H. Tanning habits and sunburn in a Swedish population age 13–50 years. Eur. J. Cancer 2001, 37, 2441–2448. [Google Scholar] [CrossRef]
- Moan, J.E.; Baturaite, Z.; Grigalavicius, M.; Juzeniene, A. Sunbed use and cutaneous melanoma in Norway. Scand J. Public Health 2013, 41, 812–817. [Google Scholar] [CrossRef] [PubMed]
- Coups, E.J.; Phillips, L.A. A more systematic review of correlates of indoor tanning. J. Eur. Acad. Derm. Venereol. 2011, 25, 610–616, author reply 617–618. [Google Scholar] [CrossRef]
- Schneider, S.; Kramer, H. Who uses sunbeds? A systematic literature review of risk groups in developed countries. J. Eur. Acad. Derm. Venereol. 2010, 24, 639–648. [Google Scholar] [CrossRef]
- Mansh, M.; Katz, K.A.; Linos, E.; Chren, M.M.; Arron, S. Association of Skin Cancer and Indoor Tanning in Sexual Minority Men and Women. JAMA Derm. 2015, 151, 1308–1316. [Google Scholar] [CrossRef]
- Singer, S.; Tkachenko, E.; Yeung, H.; Mostaghimi, A. Skin cancer and skin cancer risk behaviors among sexual and gender minority populations: A systematic review. J. Am. Acad. Derm. 2020, 83, 511–522. [Google Scholar] [CrossRef]
- Admassu, N.; Pimentel, M.A.; Halley, M.C.; Torres, J.; Pascua, N.; Katz, K.A.; Linos, E. Motivations among sexual-minority men for starting and stopping indoor tanning. Br. J. Derm. 2019, 180, 1529–1530. [Google Scholar] [CrossRef]
- Wester, U.; Boldemann, C.; Jansson, B.; Ullen, H. Population UV-dose and skin area--do sunbeds rival the sun? Health Phys. 1999, 77, 436–440. [Google Scholar] [CrossRef]
- Bali, R.; Ji-Xu, A.; Felton, S.J. The significant health threat from sunbed use as a self treatment in patients with acne. Clin. Exp. Dermatol. 2022, 47, 404–406. [Google Scholar] [CrossRef]
- Nast, A.; Dreno, B.; Bettoli, V.; Bukvic Mokos, Z.; Degitz, K.; Dressler, C.; Finlay, A.Y.; Haedersdal, M.; Lambert, J.; Layton, A.; et al. European evidence-based (S3) guideline for the treatment of acne-update 2016-short version. J. Eur. Acad. Derm. Venereol. 2016, 30, 1261–1268. [Google Scholar] [CrossRef]
- Pagoto, S.L.; Nahar, V.K.; Frisard, C.; Conroy, D.E.; Lemon, S.C.; Oleski, J.; Hillhouse, J. A Comparison of Tanning Habits Among Gym Tanners and Other Tanners. JAMA Derm. 2018, 154, 1090–1091. [Google Scholar] [CrossRef]
- Diehl, K.; Breitbart, E.W.; de Buhr, Y.; Schneider, S.; Gorig, T. Shift in place of tanning bed use from tanning salons to spa, fitness, and beauty facilities: A trend perspective. Photodermatol. Photoimmunol. Photomed. 2022, 38, 83–85. [Google Scholar] [CrossRef]
- Huang, C.M.; Kirchhof, M.G. A Cross-Sectional Study of Indoor Tanning in Fitness Centres. J. Cutan Med. Surg. 2017, 21, 401–407. [Google Scholar] [CrossRef]
- An, S.; Kim, K.; Moon, S.; Ko, K.P.; Kim, I.; Lee, J.E.; Park, S.K. Indoor Tanning and the Risk of Overall and Early-Onset Melanoma and Non-Melanoma Skin Cancer: Systematic Review and Meta-Analysis. Cancers 2021, 13, 5940. [Google Scholar] [CrossRef]
- Burgard, B.; Schope, J.; Holzschuh, I.; Schiekofer, C.; Reichrath, S.; Stefan, W.; Pilz, S.; Ordonez-Mena, J.; Marz, W.; Vogt, T.; et al. Solarium Use and Risk for Malignant Melanoma: Meta-analysis and Evidence-based Medicine Systematic Review. Anticancer Res. 2018, 38, 1187–1199. [Google Scholar] [CrossRef]
- Colantonio, S.; Bracken, M.B.; Beecker, J. The association of indoor tanning and melanoma in adults: Systematic review and meta-analysis. J. Am. Acad. Derm. 2014, 70, 847–857.e18. [Google Scholar] [CrossRef]
- Wehner, M.R.; Shive, M.L.; Chren, M.M.; Han, J.; Qureshi, A.A.; Linos, E. Indoor tanning and non-melanoma skin cancer: Systematic review and meta-analysis. BMJ 2012, 345, e5909. [Google Scholar] [CrossRef]
- International Agency for Research on Cancer Working Group on Artificial Ultraviolet Light and Skin Cancer. The association of use of sunbeds with cutaneous malignant melanoma and other skin cancers: A systematic review. Int. J. Cancer 2007, 120, 1116–1122. [Google Scholar] [CrossRef]
- Gallagher, R.P.; Spinelli, J.J.; Lee, T.K. Tanning beds, sunlamps, and risk of cutaneous malignant melanoma. Cancer Epidemiol. Biomark. Prev. 2005, 14, 562–566. [Google Scholar] [CrossRef] [PubMed]
- Boniol, M.; Autier, P.; Boyle, P.; Gandini, S. Correction: Cutaneous melanoma attributable to sunbed use: Systematic review and meta-analysis. BMJ 2012, 345, E8503. [Google Scholar] [CrossRef] [PubMed]
- Lazovich, D.; Isaksson Vogel, R.; Weinstock, M.A.; Nelson, H.H.; Ahmed, R.L.; Berwick, M. Association Between Indoor Tanning and Melanoma in Younger Men and Women. JAMA Derm. 2016, 152, 268–275. [Google Scholar] [CrossRef] [PubMed]
- Ghiasvand, R.; Rueegg, C.S.; Weiderpass, E.; Green, A.C.; Lund, E.; Veierod, M.B. Indoor Tanning and Melanoma Risk: Long-Term Evidence From a Prospective Population-Based Cohort Study. Am. J. Epidemiol. 2017, 185, 147–156. [Google Scholar] [CrossRef] [PubMed]
- Cust, A.E.; Armstrong, B.K.; Goumas, C.; Jenkins, M.A.; Schmid, H.; Hopper, J.L.; Kefford, R.F.; Giles, G.G.; Aitken, J.F.; Mann, G.J. Sunbed use during adolescence and early adulthood is associated with increased risk of early-onset melanoma. Int. J. Cancer 2011, 128, 2425–2435. [Google Scholar] [CrossRef] [PubMed]
- Veierod, M.B.; Weiderpass, E.; Thorn, M.; Hansson, J.; Lund, E.; Armstrong, B.; Adami, H.O. A prospective study of pigmentation, sun exposure, and risk of cutaneous malignant melanoma in women. J. Natl. Cancer Inst. 2003, 95, 1530–1538. [Google Scholar] [CrossRef]
- Nielsen, K.; Masback, A.; Olsson, H.; Ingvar, C. A prospective, population-based study of 40,000 women regarding host factors, UV exposure and sunbed use in relation to risk and anatomic site of cutaneous melanoma. Int. J. Cancer 2012, 131, 706–715. [Google Scholar] [CrossRef]
- Gandini, S.; Dore, J.F.; Autier, P.; Greinert, R.; Boniol, M. Epidemiological evidence of carcinogenicity of sunbed use and of efficacy of preventive measures. J. Eur. Acad. Derm. Venereol. 2019, 33 (Suppl. 2), 57–62. [Google Scholar] [CrossRef]
- Veierod, M.B.; Adami, H.O.; Lund, E.; Armstrong, B.K.; Weiderpass, E. Sun and solarium exposure and melanoma risk: Effects of age, pigmentary characteristics, and nevi. Cancer Epidemiol. Biomark. Prev. 2010, 19, 111–120. [Google Scholar] [CrossRef]
- Karapetyan, L.; Yang, X.; Wang, H.; Sander, C.A.; Moyer, A.; Wilson, M.; Karunamurthy, A.; Kirkwood, J.M. Indoor tanning exposure in association with multiple primary melanoma. Cancer 2021, 127, 560–568. [Google Scholar] [CrossRef]
- Arnold, M.; Kvaskoff, M.; Thuret, A.; Guenel, P.; Bray, F.; Soerjomataram, I. Cutaneous melanoma in France in 2015 attributable to solar ultraviolet radiation and the use of sunbeds. J. Eur. Acad. Derm. Venereol. 2018, 32, 1681–1686. [Google Scholar] [CrossRef]
- Gredner, T.; Behrens, G.; Stock, C.; Brenner, H.; Mons, U. Cancers Due to Infection and Selected Environmental Factors. Dtsch. Arztebl. Int. 2018, 115, 586–593. [Google Scholar] [CrossRef]
- Hill, A.B. The Environment and Disease: Association or Causation? Proc. R Soc. Med. 1965, 58, 295–300. [Google Scholar] [CrossRef]
- Suppa, M.; Gandini, S. Sunbeds and melanoma risk: Time to close the debate. Curr. Opin. Oncol. 2019, 31, 65–71. [Google Scholar] [CrossRef]
- Christensen, G.B.; Ingvar, C.; Hartman, L.W.; Olsson, H.; Nielsen, K. Sunbed Use Increases Cutaneous Squamous Cell Carcinoma Risk in Women: A Large-scale, Prospective Study in Sweden. Acta. Derm Venereol. 2019, 99, 878–883. [Google Scholar] [CrossRef]
- Lergenmuller, S.; Ghiasvand, R.; Robsahm, T.E.; Green, A.C.; Lund, E.; Rueegg, C.S.; Veierod, M.B. Association of Lifetime Indoor Tanning and Subsequent Risk of Cutaneous Squamous Cell Carcinoma. JAMA Derm. 2019, 155, 1350–1357. [Google Scholar] [CrossRef]
- Liu, F.C.; Grimsrud, T.K.; Veierod, M.B.; Robsahm, T.E.; Ghiasvand, R.; Babigumira, R.; Shala, N.K.; Stenehjem, J.S. Ultraviolet radiation and risk of cutaneous melanoma and squamous cell carcinoma in males and females in the Norwegian Offshore Petroleum Workers cohort. Am. J. Ind. Med. 2021, 64, 496–510. [Google Scholar] [CrossRef]
- Veierod, M.B.; Couto, E.; Lund, E.; Adami, H.O.; Weiderpass, E. Host characteristics, sun exposure, indoor tanning and risk of squamous cell carcinoma of the skin. Int. J. Cancer 2014, 135, 413–422. [Google Scholar] [CrossRef]
- Tierney, P.; de Gruijl, F.R.; Ibbotson, S.; Moseley, H. Predicted increased risk of squamous cell carcinoma induction associated with sunbed exposure habits. Br. J. Derm. 2015, 173, 201–208. [Google Scholar] [CrossRef]
- Kaskel, P.; Lange, U.; Sander, S.; Huber, M.A.; Utikal, J.; Leiter, U.; Krahn, G.; Meurer, M.; Kron, M. Ultraviolet exposure and risk of melanoma and basal cell carcinoma in Ulm and Dresden, Germany. J. Eur. Acad. Derm. Venereol. 2015, 29, 134–142. [Google Scholar] [CrossRef]
- Adalsteinsson, J.A.; Ratner, D.; Olafsdottir, E.; Grant-Kels, J.; Ungar, J.; Silverberg, J.I.; Kristjansson, A.K.; Jonasson, J.G.; Tryggvadottir, L. Basal cell carcinoma: An emerging epidemic in women in Iceland. Br. J. Derm. 2020, 183, 847–856. [Google Scholar] [CrossRef] [PubMed]
- Pandeya, N. Rising incidence of basal cell carcinoma in women in Iceland: Is it sunbed use? Br. J. Derm. 2020, 183, 799–800. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Qureshi, A.A.; Geller, A.C.; Frazier, L.; Hunter, D.J.; Han, J. Use of tanning beds and incidence of skin cancer. J. Clin. Oncol. 2012, 30, 1588–1593. [Google Scholar] [CrossRef] [PubMed]
- Pawlak, M.T.; Bui, M.; Amir, M.; Burkhardt, D.L.; Chen, A.K.; Dellavalle, R.P. Legislation restricting access to indoor tanning throughout the world. Arch. Derm. 2012, 148, 1006–1012. [Google Scholar] [CrossRef] [PubMed]
- SCHEER (Scientific Committee on Health EaER). Opinion on biological effects of ultraviolet radiation relevant to health with particular reference to sunbeds for cosmetic purposes. Available online: https://health.ec.europa.eu/other-pages/health-sc-basic-page/opinion-biological-effects-ultraviolet-radiation-relevant-health-particular-reference-sunbeds_en#modal (accessed on 10 August 2022).
- Yared, W.; Boonen, B.; McElwee, G.; Ferguson, M. Cancer league actions against sunbed use for skin cancer prevention. J. Eur. Acad. Derm. Venereol. 2019, 33 (Suppl. 2), 97–103. [Google Scholar] [CrossRef]
- Longo, M.I.; Bulliard, J.L.; Correia, O.; Maier, H.; Magnusson, S.M.; Konno, P.; Goad, N.; Duarte, A.F.; Olah, J.; Nilsen, L.T.N.; et al. Sunbed use legislation in Europe: Assessment of current status. J. Eur. Acad. Derm. Venereol. 2019, 33 (Suppl. 2), 89–96. [Google Scholar] [CrossRef]
- Diehl, K.; Lindwedel, K.S.; Mathes, S.; Gorig, T.; Gefeller, O. Tanning Bed Legislation for Minors: A Comprehensive International Comparison. Children 2022, 9, 768. [Google Scholar] [CrossRef]
- Reimann, J.; McWhirter, J.E.; Cimino, A.; Papadopoulos, A.; Dewey, C. Impact of legislation on youth indoor tanning behaviour: A systematic review. Prev. Med. 2019, 123, 299–307. [Google Scholar] [CrossRef]
- Gordon, L.G.; Hainsworth, R.; Eden, M.; Epton, T.; Lorigan, P.; Grant, M.; Green, A.C.; Payne, K. Sunbed Use among 11- to 17-Year-Olds and Estimated Number of Commercial Sunbeds in England with Implications for a ‘Buy-Back’ Scheme. Children 2021, 8, 393. [Google Scholar] [CrossRef]
- Qin, J.; Holman, D.M.; Jones, S.E.; Berkowitz, Z.; Guy, G.P., Jr. State Indoor Tanning Laws and Prevalence of Indoor Tanning Among US High School Students, 2009–2015. Am. J. Public Health 2018, 108, 951–956. [Google Scholar] [CrossRef]
- Diehl, K.; Gorig, T.; Greinert, R.; Breitbart, E.W.; Schneider, S. Trends in Tanning Bed Use, Motivation, and Risk Awareness in Germany: Findings from Four Waves of the National Cancer Aid Monitoring (NCAM). Int. J. Env. Res. Public Health 2019, 16, 3913. [Google Scholar] [CrossRef]
- Janda, M.; Sinclair, C. Experience from an outright ban of commercial sunbeds in the Australian context. Br. J. Derm. 2022, 187, 7. [Google Scholar] [CrossRef]
- Eden, M.; Hainsworth, R.; Gordon, L.G.; Epton, T.; Lorigan, P.; Rhodes, L.E.; Marais, R.; Green, A.C.; Payne, K. Cost-effectiveness of a policy-based intervention to reduce melanoma and other skin cancers associated with indoor tanning. Br. J. Derm. 2022, 187, 105–114. [Google Scholar] [CrossRef]
- Guy, G.P., Jr.; Zhang, Y.; Ekwueme, D.U.; Rim, S.H.; Watson, M. The potential impact of reducing indoor tanning on melanoma prevention and treatment costs in the United States: An economic analysis. J. Am. Acad. Derm. 2017, 76, 226–233. [Google Scholar] [CrossRef]
- Gordon, L.G.; Rodriguez-Acevedo, A.J.; Koster, B.; Guy, G.P., Jr.; Sinclair, C.; Van Deventer, E.; Green, A.C. Association of Indoor Tanning Regulations With Health and Economic Outcomes in North America and Europe. JAMA Derm. 2020, 156, 401–410. [Google Scholar] [CrossRef]
- Sontag, J.M.; Noar, S.M. Assessing the Potential Effectiveness of Pictorial Messages to Deter Young Women from Indoor Tanning: An Experimental Study. J. Health Commun. 2017, 22, 294–303. [Google Scholar] [CrossRef]
- Hammond, D. Health warning messages on tobacco products: A review. Tob. Control. 2011, 20, 327–337. [Google Scholar] [CrossRef]
- Boyle, R.; O’Hagan, A.H.; Donnelly, D.; Donnelly, C.; Gordon, S.; McElwee, G.; Gavin, A. Trends in reported sun bed use, sunburn, and sun care knowledge and attitudes in a U.K. region: Results of a survey of the Northern Ireland population. Br. J. Derm. 2010, 163, 1269–1275. [Google Scholar] [CrossRef]
- Koster, B.; Thorgaard, C.; Philip, A.; Clemmensen, H. Sunbed use and campaign initiatives in the Danish population, 2007–2009: A cross-sectional study. J. Eur. Acad. Derm. Venereol. 2011, 25, 1351–1355. [Google Scholar] [CrossRef]
- Aarestrup, C.; Bonnesen, C.T.; Thygesen, L.C.; Krarup, A.F.; Waagstein, A.B.; Jensen, P.D.; Bentzen, J. The effect of a school-based intervention on sunbed use in Danish pupils at continuation schools: A cluster-randomized controlled trial. J. Adolesc. Health 2014, 54, 214–220. [Google Scholar] [CrossRef]
- Tripathi, R.; Tamashunas, N.L.; Xiang, L.; Simmons, E.; Mazmudar, R.S.; Bordeaux, J.S.; Scott, J.F. Limited sun safety education in high school curricula: A pilot study and call to action. Arch. Dermatol. Res. 2022, 314, 85–88. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Kim, Y.; Kornides, M.L.; McRee, A.L.; Mays, D.; Asgari, M.M.; Gilkey, M.B. Correlates of positive parental attitudes towards adolescent indoor tanning in the USA. Br. J. Derm. 2018, 179, 1412–1413. [Google Scholar] [CrossRef] [PubMed]
- Buller, D.B.; Pagoto, S.; Henry, K.L.; Baker, K.; Walkosz, B.J.; Hillhouse, J.; Berteletti, J.; Bibeau, J.; Kinsey, A. Persisting Effects of a Social Media Campaign to Prevent Indoor Tanning: A Randomized Trial. Cancer Epidemiol. Biomark. Prev. 2022, 31, 885–892. [Google Scholar] [CrossRef] [PubMed]
- Cidre Serrano, W.; Chren, M.M.; Resneck, J.S., Jr.; Aji, N.N.; Pagoto, S.; Linos, E. Online Advertising for Cancer Prevention: Google Ads and Tanning Beds. JAMA Derm. 2016, 152, 101–102. [Google Scholar] [CrossRef] [PubMed]
- Morrison, L.; Chen, C.; Torres, J.S.; Wehner, M.; Junn, A.; Linos, E. Facebook advertising for cancer prevention: A pilot study. Br. J. Derm. 2019, 181, 858–859. [Google Scholar] [CrossRef]
- Stapleton, J.L.; Darabos, K.; Carpenter, A.; Lewis, M.J.; Greene, K.; Hudson, S.V. Indoor tanning users’ experiences with tanning salon direct to consumer marketing. J. Am. Acad. Derm. 2015, 72, 1092–1094. [Google Scholar] [CrossRef][Green Version]
- Holman, D.M.; Fox, K.A.; Glenn, J.D.; Guy, G.P., Jr.; Watson, M.; Baker, K.; Cokkinides, V.; Gottlieb, M.; Lazovich, D.; Perna, F.M.; et al. Strategies to reduce indoor tanning: Current research gaps and future opportunities for prevention. Am. J. Prev. Med. 2013, 44, 672–681. [Google Scholar] [CrossRef][Green Version]
- Falzone, A.E.; Brindis, C.D.; Chren, M.M.; Junn, A.; Pagoto, S.; Wehner, M.; Linos, E. Teens, Tweets, and Tanning Beds: Rethinking the Use of Social Media for Skin Cancer Prevention. Am. J. Prev. Med. 2017, 53, S86–S94. [Google Scholar] [CrossRef]
- Adekunle, L.; Chen, R.; Morrison, L.; Halley, M.; Eng, V.; Hendlin, Y.; Wehner, M.R.; Chren, M.M.; Linos, E. Association between financial links to indoor tanning industry and conclusions of published studies on indoor tanning: Systematic review. BMJ 2020, 368, m7. [Google Scholar] [CrossRef]
- Pierret, L.; Suppa, M.; Gandini, S.; Del Marmol, V.; Gutermuth, J. Overview on vitamin D and sunbed use. J. Eur. Acad. Derm. Venereol. 2019, 33 (Suppl. 2), 28–33. [Google Scholar] [CrossRef]
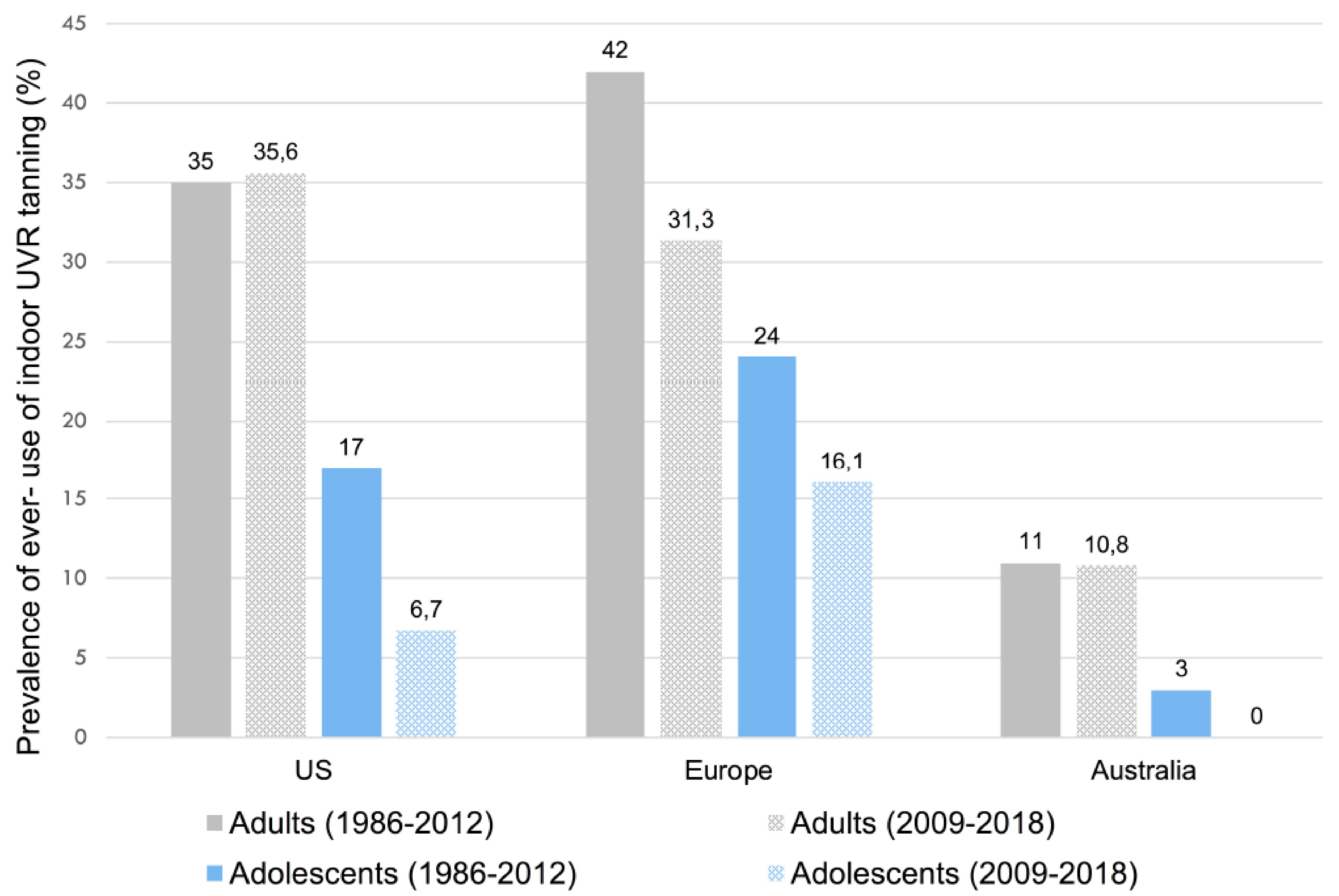
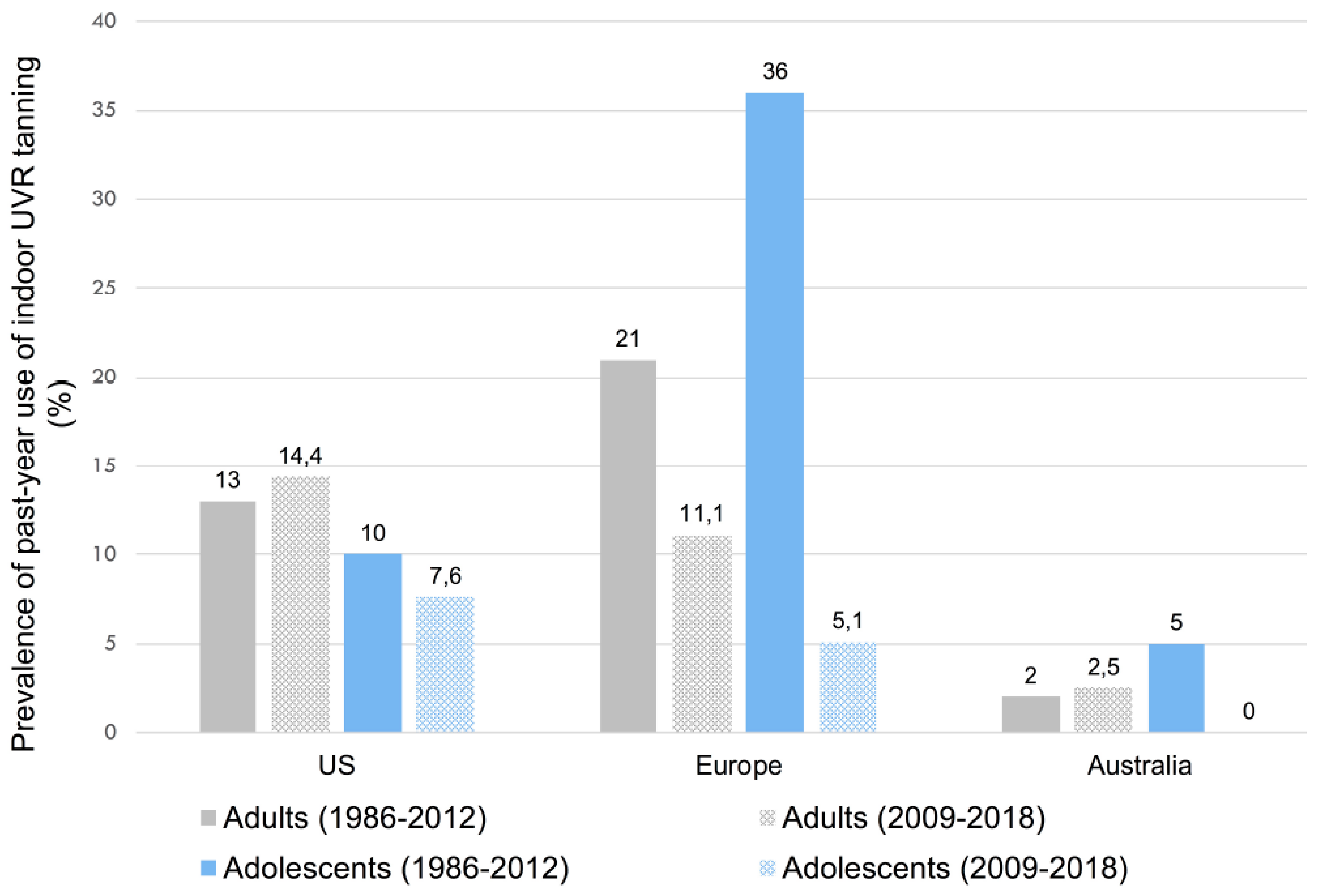
| Reference | Study Type, Study Year | n | Prevalence of Ever-Use of Indoor Tanning, by Region | Prevalence of Ever-Use of Indoor Tanning, by Age and Gender (95% CI) | Prevalence of Past-Year Use of Indoor Tanning, by Region | Prevalence of Past-Year Use of Indoor Tanning, by Age and Gender (95% CI) |
|---|---|---|---|---|---|---|
| Wehner, 2014 [12] | Meta-analysis, 1986–2012 | 491,492 | US Adults: 35% University students: 59% Adolescents: 17% Northern and Western Europe Adults: 42% University students: 12% Adolescents: 24% Australia Adults: 11% University students: - Adolescents: 3% | Adults: 35.7% (27.5–44.0) Female: 39.8% Male: 20.4% University students: 55% (33.0–77.1) Female: 69.3% Male: 40.0% Adolescents: 19.3% (14.7–24.0) Female: 31.5% Male: 14.1% | US Adults: 13% University students: 43% Adolescents: 10% Northern and Western Europe Adults: 21% University students: - Adolescents: 36% Australia Adults: 2% University students: - Adolescents: 5% | Adults: 14.0% (11.5–16.5) Female: 19.0% Male: 9.0% University students: 43.1% (21.7–64.5) Female: 64.9% Male: 26.8% Adolescents: 18.3% (12.6–24.0) Female: 21.3% Male: 7.5% |
| Rodriguez-Acevedo, 2020 [13] | Meta-analysis, 2009–2018 | 401,999 | US/Canada Adults: 35.6% Adolescents: 6.7% Europe Adults: 31.3% Adolescents: 16.1% Australia Adults: 10.8% Adolescents: - | Adults: 31.9% (25.3–39.1) Female: 38.0% Male: 24.9% Adolescents: 9.7% (7.3–12.4) Female: 8.4% Male: 4.0% | US/Canada Adults: 14.4% Adolescents: 7.6% Europe Adults: 11.1% Adolescents: 5.1% Australia Adults: 2.5% Adolescents: - | Adults: 12.5% (9.5–15.6) Female: 16.8% Male: 8.5% Adolescents: 6.7% (4.4–9.6) Female: 8.9% Male: 3.9% |
| Suppa, 2019 [14] | Survey, 2009–2014 | 227,888 | 30 European countries overall prevalence: 10.6% Prevalence: 18–27% Belgium, Denmark, Estonia, Hungary, Italy, Latvia, Norway, Spain Prevalence: 10–18% Croatia, Czech Republic, Germany, Ireland, Lithuania, Poland Russia, Serbia, Sweden Prevalence: <10% Bosnia-Herzegovina, Cyprus, Georgia, Greece, Macdonia(FYROM), Malta, Moldova, Portugal, Romania, Slovenia, Switzerland, Turkey, Ukraine | Adults/elderly: 8.3% Young adults: 17.0% Adolescents: 5.9% |
| Reference (Years of Included Studies) | n Studies a | n Cases Overall | CM Group Studied | Ever Indoor Tanning (vs. Never) RR (95% CI) | Annual Frequency of Indoor Tanning (Times) RR (95% CI) | Early Age at First Use of Indoor Tanning (Years) RR (95% CI) |
|---|---|---|---|---|---|---|
| An, 2021 [37] (Up to 2021) | 36 | 14,583 | CM | 1.27 (1.16–1.39) | <10: 1.33 (1.00–1.78) ≥10: 1.52 (1.22–1.89) | <20: 1.47 (1.16–1.85) ≥20: 1.28 (1.01–1.63) |
| 2 | 1771 | CM < 50 y | 1.75 (1.14–2.69) | - | - | |
| Burgard, 2018 [38] (1981–2015) | 31 | 11,706 | CM | 1.19 (1.05–1.34) | ≤10: 1.13 (0.93–1.38) >10: 1.43 (1.17–1.74) | <25: 1.59 (1.38–1.83) |
| Colantonio, 2014 [39] (1981–2012) | 31 | 14,956 | CM | 1.16 (1.05–1.28) | ≤10:1.07 (0.90–1.26) >10: 1.34 (1.05–1.71) | <25: 1.35 (0.99–1.84) ≥25: 1.11 (0.86–1.42) |
| Boniol, 2012 [18] (1981–2012) | 27 | 11,428 | CM | 1.20 (1.08–1.34) | High:1.42 (1.15–1.74) | <35: 1.59 (1.36–1.85) b |
| IARC, 2007 [41] (1979–2005) | 19 | 7355 | CM | 1.15 (1.00–1.31) | - | <35: 1.75 (1.35–2.26) |
| Gallagher, 2005 [42] (1984–2004) | 10 | 4560 | CM | 1.25 (1.05–1.49) | Longest: 1.61 (1.21–2.12) c | Young adult: 1.69 (1.32–2.18) d |
| Reference (Years of Included Studies) | n Studies | n Cases Overall | KC Studied | Ever Indoor Tanning (vs. Never) RR (95% CI) | Annual Frequency of Indoor Tanning (Times) RR (95% CI) | Early Age at First Use of Indoor Tanning (Years) RR (95% CI) |
|---|---|---|---|---|---|---|
| An, 2021 [37] (Up to 2021) | 18 | 10,406 | KC | 1.40 (1.18–1.65) | <10: 1.32 (1.14–1.52) ≥10: 1.56 (1.31–1.86) | <20: 2.02 (1.44–2.83) ≥20: 1.48 (1.31–1.68) |
| 4 | 1410 | KC < 50 y | 1.81 (1.38–2.37) | - | - | |
| 9 | 2528 | cSCC | 1.58 (1.38–1.81) | <10: 1.46 (1.24–1.71) ≥10: 1.65 (1.30–2.10) | <20: 1.89 (0.90–3.98) ≥20: 1.53 (1.26–1.85) | |
| 1 | 131 | cSCC < 50 y | 1.99 (1.48–2.68) | - | - | |
| 10 | 7643 | BCC | 1.24 (1.00–1.55) | <10: 1.29 (1.01–1.65) ≥10: 1.46 (1.28–1.66) | <20: 1.86 (1.44–2.41) ≥20: 1.51 (1.19–1.92) | |
| 3 | 1049 | BCC < 50 y | 1.79 (1.15–2.77) | - | - | |
| Boniol, 2012 [18] (1981–2012) | 5 | 1242 | cSCC | 2.23 (1.39–3.570) | - | - |
| 6 | 6995 | BCC | 1.09 (1.01–1.18) | - | - | |
| Wehner, 2012 [40] (1985–2012) | 12 | 9328 | KC | - | - | - |
| 6 | - | cSCC | 1.67 (1.29–2.17) | - | Young: 2.02 (0.70–5.86) | |
| 8 | - | BCC | 1.29 (1.08–1.53) | High: 1.50 (0.81–2.77) | Young: 1.40 (1.29–1.52) | |
| IARC, 2007 [41] (1979–2005) | 3 | - | cSCC | 2.25 (1.08–4.70) | - | - |
| 4 | - | BCC | 1.03 (0.56–1.90) | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dessinioti, C.; Stratigos, A.J. An Epidemiological Update on Indoor Tanning and the Risk of Skin Cancers. Curr. Oncol. 2022, 29, 8886-8903. https://doi.org/10.3390/curroncol29110699
Dessinioti C, Stratigos AJ. An Epidemiological Update on Indoor Tanning and the Risk of Skin Cancers. Current Oncology. 2022; 29(11):8886-8903. https://doi.org/10.3390/curroncol29110699
Chicago/Turabian StyleDessinioti, Clio, and Alexander J. Stratigos. 2022. "An Epidemiological Update on Indoor Tanning and the Risk of Skin Cancers" Current Oncology 29, no. 11: 8886-8903. https://doi.org/10.3390/curroncol29110699
APA StyleDessinioti, C., & Stratigos, A. J. (2022). An Epidemiological Update on Indoor Tanning and the Risk of Skin Cancers. Current Oncology, 29(11), 8886-8903. https://doi.org/10.3390/curroncol29110699






