Feasibility Study and Clinical Impact of Incorporating Breast Tissue Density in High-Risk Breast Cancer Screening Assessment
Abstract
Key Points:
1. Introduction
2. Methods
3. Results
3.1. Impact on Eligibility for B-MRI through the HROBSP Program
3.2. Feasibility of Incorporating BTD into the IBISv8 Calculation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Boyd, N.F.; Guo, H.; Martin, L.J.; Sun, L.; Stone, J.; Fishell, E.; Jong, R.A.; Hislop, G.; Chiarelli, A.; Minkin, S.; et al. Mammographic density and the risk and detection of breast cancer. N. Engl. J. Med. 2007, 356, 227–236. [Google Scholar] [CrossRef] [PubMed]
- Boyd, N.F.; Dite, G.S.; Stone, J.; Gunasekara, A.; English, D.R.; McCredie, M.R.; Giles, G.G.; Tritchler, D.; Chiarelli, A.; Yaffe, M.J.; et al. Heritability of mammographic density, a risk factor for breast cancer. N. Engl. J. Med. 2002, 347, 886–894. [Google Scholar] [CrossRef]
- Engmann, N.J.; Golmakani, M.K.; Miglioretti, D.L.; Sprague, B.L.; Kerlikowske, K.; Breast Cancer Surveillance, C. Population-Attributable Risk Proportion of Clinical Risk Factors for Breast Cancer. JAMA Oncol. 2017, 3, 1228–1236. [Google Scholar] [CrossRef] [PubMed]
- McCormack, V.A.; dos Santos Silva, I. Breast density and parenchymal patterns as markers of breast cancer risk: A meta-analysis. Cancer Epidemiol. Biomarkers Prev. 2006, 15, 1159–1169. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Zhang, J.; Beeraka, N.M.; Tang, C.; Babayeva, Y.V.; Sinelnikov, M.Y.; Zhang, X.; Zhang, J.; Liu, J.; Reshetov, I.V.; et al. Advances in the Prevention and Treatment of Obesity-Driven Effects in Breast Cancers. Front. Oncol. 2022, 12, 820968. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Lu, P.; Beeraka, N.M.; Sukocheva, O.A.; Madhunapantula, S.V.; Liu, J.; Sinelnikov, M.Y.; Nikolenko, V.N.; Bulygin, K.V.; Mikhaleva, L.M.; et al. Mitochondrial mutations and mitoepigenetics: Focus on regulation of oxidative stress-induced responses in breast cancers. Semin. Cancer Biol. 2022, 83, 556–569. [Google Scholar] [CrossRef]
- Liu, Y.; Chen, C.; Wang, X.; Sun, Y.; Zhang, J.; Chen, J.; Shi, Y. An Epigenetic Role of Mitochondria in Cancer. Cells 2022, 11, 2518. [Google Scholar] [CrossRef]
- Daly, M.B.; Pal, T.; Berry, M.P.; Buys, S.S.; Dickson, P.; Domchek, S.M.; Elkhanany, A.; Friedman, S.; Goggins, M.; Hutton, M.L.; et al. Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2021, 19, 77–102. [Google Scholar] [CrossRef]
- Monticciolo, D.L.; Malak, S.F.; Friedewald, S.M.; Eby, P.R.; Newell, M.S.; Moy, L.; Destounis, S.; Leung, J.W.T.; Hendrick, R.E.; Smetherman, D. Breast Cancer Screening Recommendations Inclusive of All Women at Average Risk: Update from the ACR and Society of Breast Imaging. J. Am. Coll. Radiol. 2021, 18, 1280–1288. [Google Scholar] [CrossRef]
- Vilmun, B.M.; Vejborg, I.; Lynge, E.; Lillholm, M.; Nielsen, M.; Nielsen, M.B.; Carlsen, J.F. Impact of adding breast density to breast cancer risk models: A systematic review. Eur. J. Radiol. 2020, 127, 109019. [Google Scholar] [CrossRef]
- Chiarelli, A.M.; Prummel, M.V.; Muradali, D.; Majpruz, V.; Horgan, M.; Carroll, J.C.; Eisen, A.; Meschino, W.S.; Shumak, R.S.; Warner, E.; et al. Effectiveness of screening with annual magnetic resonance imaging and mammography: Results of the initial screen from the ontario high risk breast screening program. J. Clin. Oncol. 2014, 32, 2224–2230. [Google Scholar] [CrossRef] [PubMed]
- Brentnall, A.R.; Cuzick, J.; Buist, D.S.M.; Bowles, E.J.A. Long-term Accuracy of Breast Cancer Risk Assessment Combining Classic Risk Factors and Breast Density. JAMA Oncol. 2018, 4, e180174. [Google Scholar] [CrossRef] [PubMed]
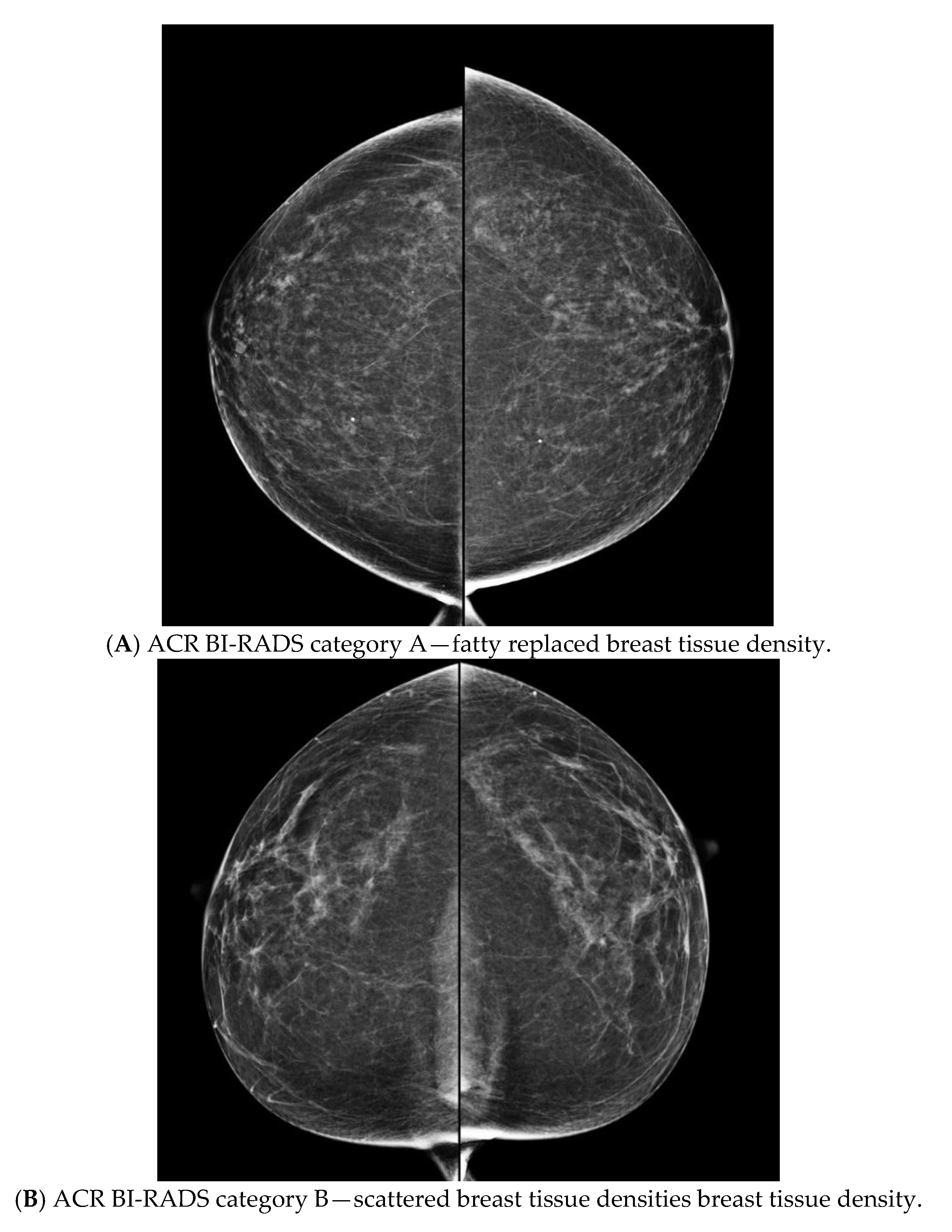
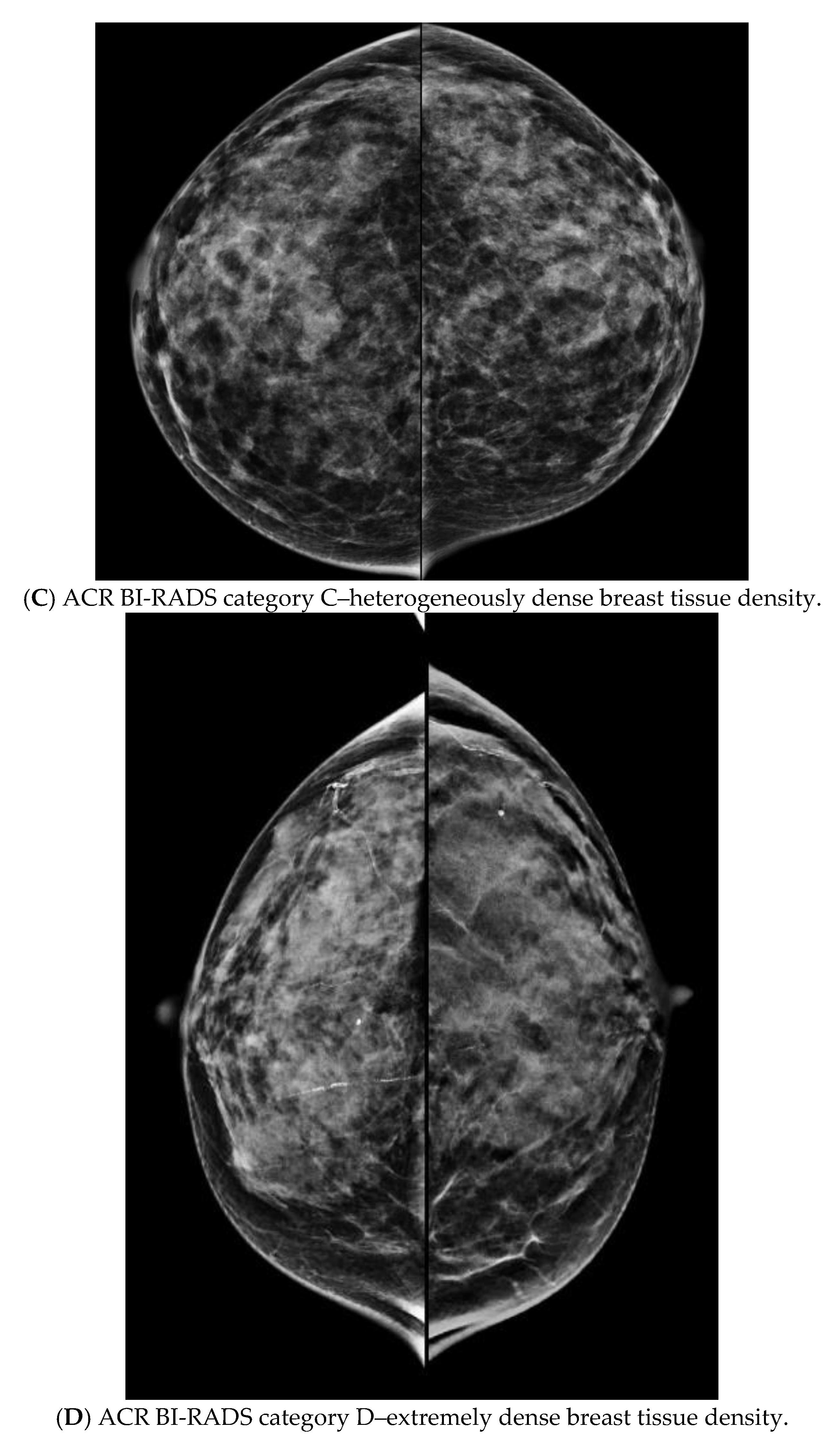
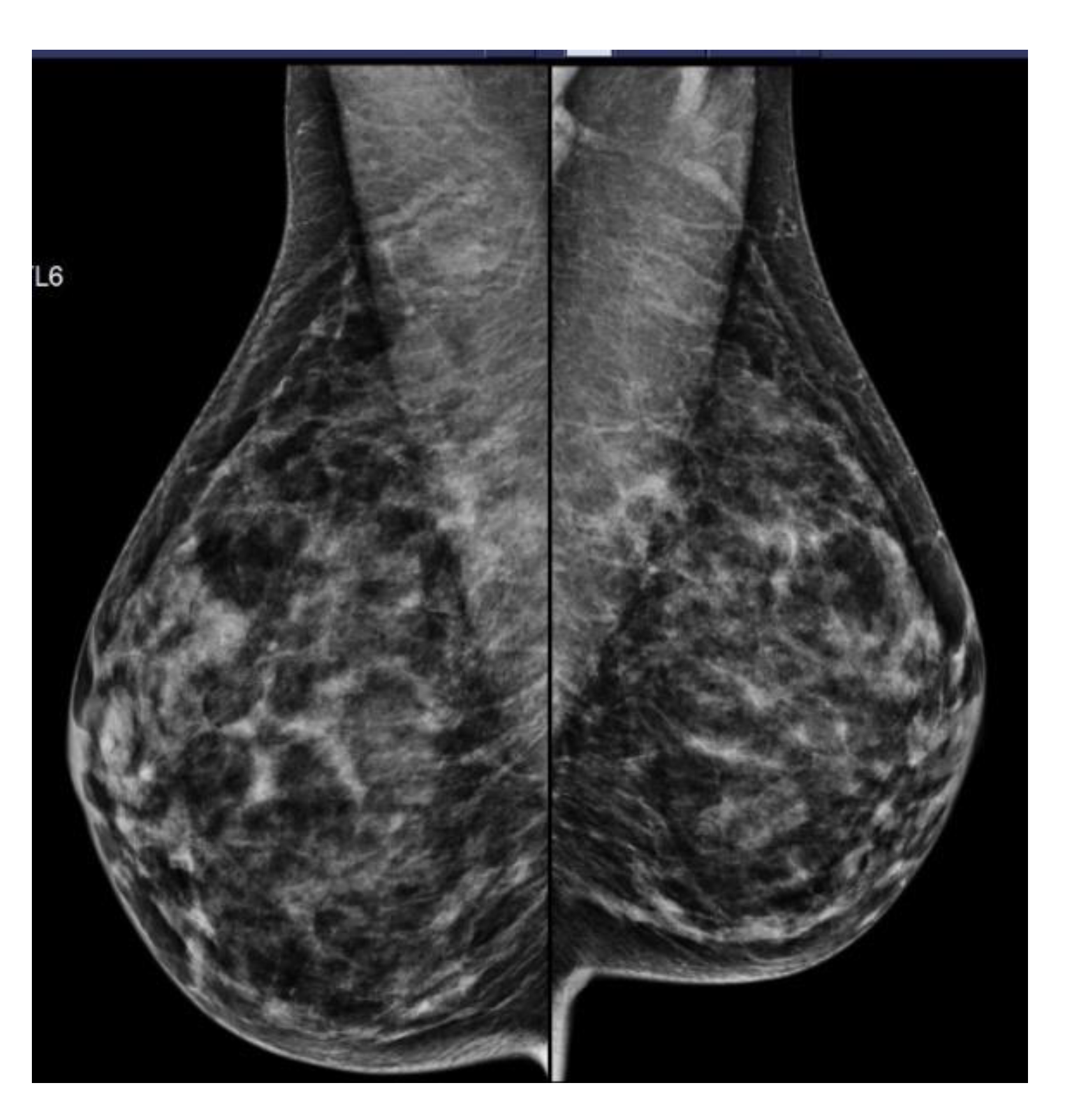
- Sickles, E.; D’Orsi, C.; Bassett, L.W. ACR BI-RADS® Mammography. In ACR BI-RADS® Atlas, Breast Imaging Reporting and Data System; American College of Radiology: Reston, VA, USA, 2013. [Google Scholar]
- Kerlikowske, K.; Zhu, W.; Tosteson, A.N.; Sprague, B.L.; Tice, J.A.; Lehman, C.D.; Miglioretti, D.L.; Breast Cancer Surveillance, C. Identifying women with dense breasts at high risk for interval cancer: A cohort study. Ann. Intern. Med. 2015, 162, 673–681. [Google Scholar] [CrossRef] [PubMed]
- Seely, J.M.; Peddle, S.E.; Yang, H.; Chiarelli, A.M.; McCallum, M.; Narasimhan, G.; Zakaria, D.; Earle, C.C.; Fung, S.; Bryant, H.; et al. Breast Density and Risk of Interval Cancers: The Effect of Annual Versus Biennial Screening Mammography Policies in Canada. Can. Assoc. Radiol. J. 2021, 73, 90–100. [Google Scholar] [CrossRef] [PubMed]
- Geuzinge, H.A.; Bakker, M.F.; Heijnsdijk, E.A.M.; van Ravesteyn, N.T.; Veldhuis, W.B.; Pijnappel, R.M.; de Lange, S.V.; Emaus, M.J.; Mann, R.M.; Monninkhof, E.M.; et al. Cost-Effectiveness of Magnetic Resonance Imaging Screening for Women With Extremely Dense Breast Tissue. J. Natl. Cancer Inst. 2021, 113, 1476–1483. [Google Scholar] [CrossRef] [PubMed]
- Bakker, M.F.; de Lange, S.V.; Pijnappel, R.M.; Mann, R.M.; Peeters, P.H.M.; Monninkhof, E.M.; Emaus, M.J.; Loo, C.E.; Bisschops, R.H.C.; Lobbes, M.B.I.; et al. Supplemental MRI Screening for Women with Extremely Dense Breast Tissue. N. Engl. J. Med. 2019, 381, 2091–2102. [Google Scholar] [CrossRef] [PubMed]
- Destounis, S.; Arieno, A.; Morgan, R.; Roberts, C.; Chan, A. Qualitative Versus Quantitative Mammographic Breast Density Assessment: Applications for the US and Abroad. Diagnostics 2017, 7, 30. [Google Scholar] [CrossRef]
- Destounis, S. Impact on risk categorization with inclusion of mammographic density in the tyrer-cuzick model. In Proceedings of the Radiological Society of North America, Abstract Presentation, Chicago, IL, USA, 28 November–2 December 2021. [Google Scholar]
- Brentnall, A.R.; Cohn, W.F.; Knaus, W.A.; Yaffe, M.J.; Cuzick, J.; Harvey, J.A. A Case-Control Study to Add Volumetric or Clinical Mammographic Density into the Tyrer-Cuzick Breast Cancer Risk Model. J Breast Imaging 2019, 1, 99–106. [Google Scholar] [CrossRef]
- Appavoo, S.; Aldis, A.; Causer, P.; Crystal, P.; Mesurolle, B.; Mundt, Y.; Panu, N.; Seely, J.M.; Wadden, N. Canadian Association of Radiologists (CAR) Practice Guidelines and Technical Standards for Breast Imaging and Intervention; Canadian Association of Radiologists: Ottawa, ON, Canada; Available online: https://car.ca/wp-content/uploads/Breast-Imaging-and-Intervention-2016.pdf (accessed on 17 September 2016).
- Klarenbach, S.; Sims-Jones, N.; Lewin, G.; Singh, H.; Theriault, G.; Tonelli, M.; Doull, M.; Courage, S.; Garcia, A.J.; Thombs, B.D.; et al. Recommendations on screening for breast cancer in women aged 40-74 years who are not at increased risk for breast cancer. CMAJ 2018, 190, E1441–E1451. [Google Scholar] [CrossRef]
- American College of Radiology. ACR BI-RADS Atlas—Mammography, 4th ed.; American College of Radiology: Reston, VA, USA, 2003. [Google Scholar]
- Pesce, K.; Tajerian, M.; Chico, M.J.; Swiecicki, M.P.; Boietti, B.; Frangella, M.J.; Benitez, S. Interobserver and intraobserver variability in determining breast density according to the fifth edition of the BI-RADS(R) Atlas. Radiologia 2020, 62, 481–486. [Google Scholar] [CrossRef]
- Sprague, B.L.; Conant, E.F.; Onega, T.; Garcia, M.P.; Beaber, E.F.; Herschorn, S.D.; Lehman, C.D.; Tosteson, A.N.; Lacson, R.; Schnall, M.D.; et al. Variation in Mammographic Breast Density Assessments Among Radiologists in Clinical Practice: A Multicenter Observational Study. Ann. Intern. Med. 2016, 165, 457–464. [Google Scholar] [CrossRef] [PubMed]
- Carver, T.; Hartley, S.; Lee, A.; Cunningham, A.P.; Archer, S.; Babb de Villiers, C.; Roberts, J.; Ruston, R.; Walter, F.M.; Tischkowitz, M.; et al. CanRisk Tool-A Web Interface for the Prediction of Breast and Ovarian Cancer Risk and the Likelihood of Carrying Genetic Pathogenic Variants. Cancer Epidemiol. Biomarkers Prev. 2021, 30, 469–473. [Google Scholar] [CrossRef] [PubMed]
| Age Groups in Years (Total) | Patient Did Not Have a MG or Was Not Available * | Number of Patients (%) with MG and Density Available | Number of Patients (%) Where Density Increased Calculated Risk ^ | Number of Patients (%) Where Density Decreased Calculated Risk ^^ | Number of Patients (%) Where Density Made Patient Eligible ** | Number of Patients (%) Where Density Made Patient Ineligible | Radiologist Input Required to Assess Density on MG |
|---|---|---|---|---|---|---|---|
| 40–49 (65) | 5 (7.7%) | 60 (92.3%) | 24 (40.0%) | 27 (45.0%) | 6 (10.0%) | 10 (16.7%) | 6 (10.0%) |
| 50–69 (74) | 3 (4.1%) | 71 (95.9%) | 26 (37.1%) | 34 (47.9%) | 3 (4.2%) | 3 (4.2%) | 11 (15.5%) |
| Total (139) | 8 (5.8%) | 131 (94.2%) | 50 (38.5%) | 61 (46.5%) | 9 (6.9%) | 13 (9.9%) | 17 (13.0%) |
| Density Category | Total Women with Mammograms (% of Total) | Became Eligible (% of Women with Density Category) * | Became Ineligible (% of Women with Density Category) |
|---|---|---|---|
| Density A | 10 (7.6%) | 0 (0%) | 2 (20.0%) |
| Density B | 40 (30.5%) | 0(0%) | 6 (15.0%) |
| Density C | 58 (44.3%) | 5 (8.6%) | 5 (8.6%) |
| Density D | 23 (17.7%) | 4 (17.4%) | 0 (0%) |
| Total | 131 | 9 (6.9%) | 13 (9.9%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rusnak, A.; Morrison, S.; Smith, E.; Hastings, V.; Anderson, K.; Aldridge, C.; Zelenietz, S.; Reddick, K.; Regnier, S.; Alie, E.; et al. Feasibility Study and Clinical Impact of Incorporating Breast Tissue Density in High-Risk Breast Cancer Screening Assessment. Curr. Oncol. 2022, 29, 8742-8750. https://doi.org/10.3390/curroncol29110688
Rusnak A, Morrison S, Smith E, Hastings V, Anderson K, Aldridge C, Zelenietz S, Reddick K, Regnier S, Alie E, et al. Feasibility Study and Clinical Impact of Incorporating Breast Tissue Density in High-Risk Breast Cancer Screening Assessment. Current Oncology. 2022; 29(11):8742-8750. https://doi.org/10.3390/curroncol29110688
Chicago/Turabian StyleRusnak, Alison, Shawna Morrison, Erika Smith, Valerie Hastings, Kelly Anderson, Caitlin Aldridge, Sari Zelenietz, Karen Reddick, Sonia Regnier, Ellen Alie, and et al. 2022. "Feasibility Study and Clinical Impact of Incorporating Breast Tissue Density in High-Risk Breast Cancer Screening Assessment" Current Oncology 29, no. 11: 8742-8750. https://doi.org/10.3390/curroncol29110688
APA StyleRusnak, A., Morrison, S., Smith, E., Hastings, V., Anderson, K., Aldridge, C., Zelenietz, S., Reddick, K., Regnier, S., Alie, E., Islam, N., Fasih, R., Peddle, S., Cordeiro, E., Tomiak, E., & Seely, J. M. (2022). Feasibility Study and Clinical Impact of Incorporating Breast Tissue Density in High-Risk Breast Cancer Screening Assessment. Current Oncology, 29(11), 8742-8750. https://doi.org/10.3390/curroncol29110688






