Can Mindfulness-Based Stress Reduction Influence the Quality of Life, Anxiety, and Depression of Women Diagnosed with Breast Cancer? —A Review
Abstract
1. Introduction
Aim
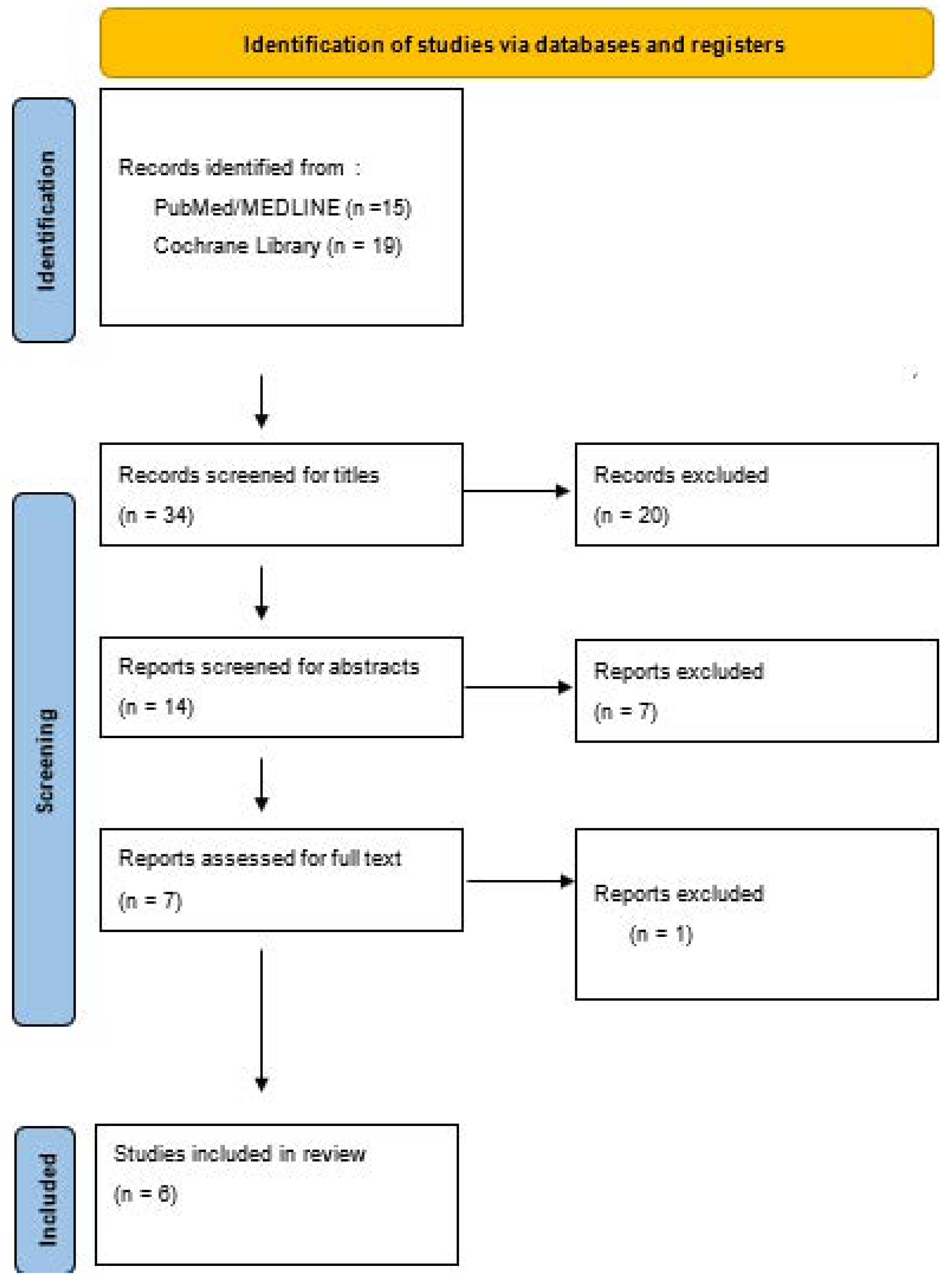
2. Materials and Methods
2.1. Risk of Bias Assessment
2.2. Ethical Consideration
2.3. Definition of Measurement Tools
3. Results
3.1. Primary Outcome: Quality of Life
3.2. Secondary Outcomes: Anxiety and Depression
4. Discussion
5. Conclusions
- (1)
- The duration of the intervention varied between the studies included and did not always last the mandatory eight-week time period of MBSR training, which may have had an adverse impact on the effectiveness of the interventions.
- (2)
- The number of participants in every study was less than 100, which makes it difficult to draw general conclusions about the general population.
- (3)
- Hardly any long-term data were collected in the studies included, which rules out the projection of long-term trends.
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Johannsen, M.; O’Connor, M.; O’Toole, M.S.; Jensen, A.B.; Hojris, I.; Zachariae, R. Efficacy of Mindfulness-Based Cognitive Therapy on Late Post-Treatment Pain in Women Treated for Primary Breast Cancer: A Randomized Controlled Trial. J. Clin. Oncol. 2016, 34, 3390–3399. [Google Scholar] [CrossRef] [PubMed]
- Kabat-Zinn, J. Gesund Durch Meditation, Das Große Buch Der Selbstheilung MIT Mbsr; Kappen, H., Ed.; KNAUR Verlag: Munich, Germany, 2019. [Google Scholar]
- Schell, L.K.; Monsef, I.; Wöckel, A.; Skoetz, N. Mindfulness-based stress reduction for women diagnosed with breast cancer. Cochrane Database Syst. Rev. 2019, 3, Cd011518. [Google Scholar] [CrossRef] [PubMed]
- Elimimian, E.; Elson, L.; Bilani, N.; Farrag, S.E.; Dwivedi, A.K.; Pasillas, R.; Nahleh, Z.A. Long-Term Effect of a Nonrandomized Psychosocial Mindfulness-Based Intervention in Hispanic/Latina Breast Cancer Survivors. Integr. Cancer Ther. 2020, 19, 1534735419890682. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.C.; Lin, G.M.; Yeh, T.L.; Chang, Y.M.; Yang, C.H.; Lo, C.; Yeh, C.Y.; Hu, W.Y. Impact of mindfulness-based stress reduction on female sexual function and mental health in patients with breast cancer. Support. Care Cancer 2022, 30, 4315–4325. [Google Scholar] [CrossRef] [PubMed]
- Lengacher, C.A.; Reich, R.R.; Paterson, C.L.; Shelton, M.; Shivers, S.; Ramesar, S.; Pleasant, M.L.; Budhrani-Shani, P.; Groer, M.; Post-White, J.; et al. A Large Randomized Trial: Effects of Mindfulness-Based Stress Reduction (MBSR) for Breast Cancer (BC) Survivors on Salivary Cortisol and IL-6. Biol. Res. Nurs. 2019, 21, 39–49. [Google Scholar] [CrossRef] [PubMed]
- Mirmahmoodi, M.; Mangalian, P.; Ahmadi, A.; Dehghan, M. The Effect of Mindfulness-Based Stress Reduction Group Counseling on Psychological and Inflammatory Responses of the Women With Breast Cancer. Integr. Cancer Ther. 2020, 19, 1534735420946819. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.C.; Yeh, T.L.; Chang, Y.M.; Hu, W.Y. Short-term Effects of Randomized Mindfulness-Based Intervention in Female Breast Cancer Survivors: A Systematic Review and Meta-analysis. Cancer Nurs. 2021, 44, E703–E714. [Google Scholar] [CrossRef]
- Zhang, Q.; Zhao, H.; Zheng, Y. Effectiveness of mindfulness-based stress reduction (MBSR) on symptom variables and health-related quality of life in breast cancer patients-a systematic review and meta-analysis. Support. Care Cancer 2019, 27, 771–781. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomized studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed]
- Zhou, T.; Guan, H.; Wang, L.; Zhang, Y.; Rui, M.; Ma, A. Health-Related Quality of Life in Patients With Different Diseases Measured With the EQ-5D-5L: A Systematic Review. Front. Public Health 2021, 9, 675523. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.A.; Donegan, D.; Albert, T. The 36-item short form. J. Am. Acad. Orthop. Surg. 2007, 15, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Castaldelli-Maia, J.M.; Marziali, M.E.; Lu, Z.; Martins, S.S. Investigating the effect of national government physical distancing measures on depression and anxiety during the COVID-19 pandemic through meta-analysis and meta-regression. Psychol. Med. 2021, 51, 881–893. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Epstein, N.; Brown, G.; Steer, R.A. An inventory for measuring clinical anxiety: Psychometric properties. J. Consult. Clin. Psychol. 1988, 56, 893–897. [Google Scholar] [CrossRef] [PubMed]
- Toledano-Toledano, F.; Moral de la Rubia, J.; Domínguez-Guedea, M.T.; Nabors, L.A.; Barcelata-Eguiarte, B.E.; Rocha-Pérez, E.; Luna, D.; Leyva-López, A.; Rivera-Rivera, L. Validity and Reliability of the Beck Anxiety Inventory (BAI) for Family Caregivers of Children with Cancer. Int. J. Environ. Res. Public Health 2020, 17, 7765. [Google Scholar] [CrossRef] [PubMed]
- Park, K.; Jaekal, E.; Yoon, S.; Lee, S.H.; Choi, K.H. Diagnostic Utility and Psychometric Properties of the Beck Depression Inventory-II Among Korean Adults. Front. Psychol. 2019, 10, 2934. [Google Scholar] [CrossRef] [PubMed]
- Blodgett, J.M.; Lachance, C.C.; Stubbs, B.; Co, M.; Wu, Y.T.; Prina, M.; Tsang, V.W.L.; Cosco, T.D. A systematic review of the latent structure of the Center for Epidemiologic Studies Depression Scale (CES-D) amongst adolescents. BMC Psychiatry 2021, 21, 197. [Google Scholar] [CrossRef] [PubMed]
| Category | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population | Women over the age of 18, who have been diagnosed with breast cancer, who have no initial psychological co-morbidity and who undergo MBSR | Women younger than 18; women with any psychological illness diagnosed before their breast cancer diagnosis |
| Intervention | Any form of mindfulness-based stress reduction or mindfulness-based cognitive therapy | Any other form of psychological therapy |
| Control | Women suffering from breast cancer that did not receive any form of psychological therapy | Any other forms of therapy beside MBSR |
| Outcomes |
| Other outcomes that cannot be allocated to the intervention |
| Study design |
| Any other study design |
| Publication date | After 2018 | Before 2018 |
| Language | German or English | Any other language |
| Duration | Any duration | No limitations |
| Search | Query | Results |
|---|---|---|
| #1 | breast cancer [Title/Abstract] | 307,817 |
| #2 | breast neoplasm [Title/Abstract] | 1013 |
| #3 | “Breast Neoplasms”[Mesh] Sort by: Most Recent | 321,610 |
| #4 | #1 OR #2 OR #3 | 410,079 |
| #5 | mindfulness based stress reduction [Title/Abstract] | 1189 |
| #6 | #5 OR #6 OR #7 | 1796 |
| #7 | #4 AND #8 | 114 |
| #8 | (“german”[Language]) OR (“english”[Language]) | 29,884,822 |
| #9 | #9 AND #10 | 112 |
| #10 | (“2018/01/01”[Date-Publication]: “3000”[Date-Publication]) | 5,816,422 |
| #11 | quality of life | 473,503 |
| #12 | #10 AND #11 AND #12 | 15 |
| Type of Study | Number of Participants (n) | Primary Outcome | Secondary Outcome | Duration of the Intervention | Number of Included Studies | (Mean) Age | Stage of Disease | Treatment | MBSR Intervention Time Period | |
|---|---|---|---|---|---|---|---|---|---|---|
| Elimimian (2020) [4] | nRCT | n = 94 | Quality of life | Anxiety, Depression | Eight weeks | / | 54.4 (SD = 8.71) | 1–3 | Surgery, chemotherapy and/or radiation therapy | After treatment |
| Chang (2022) [5] | nRCT | n = 51 | Female sexual function, Depression | Quality of life, Anxiety | Six weeks | / | 47.77 (SD = 9.29) | 0–4 | Mainly hormone therapy | During treatment |
| Lengacher (2019) [6] | RCT | n = 322 | Cortisol-levels, IL-6-levels | Depression, Anxiety, Quality of life, Stress | Six weeks | / | 56.6 (SD = 9.7) | 0–3 | Lumpectomy and/or mastectomy Adjuvant radiation and/or chemotherapy | After treatment |
| Mirmahmoodi (2020) [7] | RCT | n = 44 | Depression, Anxiety, Perceived Stress | / | Eight weeks | / | 44.14 (SD = 11.19) | Nonmetastatic stage | Mainly chemotherapy and radiotherapy and surgery | During treatment |
| Chang (2020) [8] | Meta- analysis | n = 36–322 | Depression, Anxiety | Quality of life, Fatigue, Pain | Six–eight weeks | n = 11 | 43–58 * | 0–4 | Mastectomy, lumpectomy, chemotherapy, radiation therapy and hormonal therapy | During, and after treatment |
| Zhang (2018) [9] | Meta- analysis | n = 1505 | Quality of life, Physical function, Pain, Fatigue | Anxiety, Depression, Sleep quality | Four–eight weeks | n = 14 | 40–57 * | 0–3 | No information | During, and after treatment |
| Lengacher (2019) [6] | Mirmahmoodi (2020) [7] | ||
|---|---|---|---|
| Domain 1: Randomisation process | 1.1. Was the allocation sequence random? | Y | Y |
| 1.2. Was the allocation sequence concealed until participants were enrolled and assigned to interventions? | Y | Y | |
| 1.3. Did baseline differences between intervention groups suggest a problem with the randomisation process? | N | N | |
| Risk of bias judgement | Low | Low | |
| Domain 2: Deviations from the intended interventions (effect of assignment to intervention) | 2.1. Were participants aware of their assigned intervention during the trial? | N | N |
| 2.2. Were carers and people delivering the interventions aware of participants assigned intervention during the trial? | Y | Y | |
| 2.3. If Y/PY/NI to 2.1 or 2.2: Were there deviations from the intended intervention that arose because of the trial context? | N | N | |
| 2.4. If Y/PY to 2.3: Were these deviations likely to have affected the outcome? | / | / | |
| 2.5. If Y/PY/NI to 2.4: Were these deviations from intended intervention balanced between groups? | / | / | |
| 2.6. Was an appropriate analysis used to estimate the effect of assignment to intervention? | Y | Y | |
| 2.7. If N/PN/NI to 2.6: Was there potential for a substantial impact (on the result) of the failure to analyse participants in the group to which they were randomised? | / | / | |
| Risk of bias judgement | Low | Low | |
| Domain 3: Risk of bias due to missing outcome data | 3.1. Were data for this outcome available for all, or nearly all, participants randomised? | Y | Y |
| 3.2 If N/PN/NI to 3.1: Is there evidence that the result was not biased by missing outcome data? | / | / | |
| 3.3. If N/PN to 3.2: Could missingness in the outcome depend on its true value? | / | / | |
| 3.4 If Y/PY/NI to 3.3: Is it likely that missingness in the outcome depended on its true value? | / | / | |
| Risk of bias judgement | Low | Low | |
| Domain 4: Risk of bias in measurement of the outcome | 4.1. Was the method of measuring the outcome inappropriate? | N | N |
| 4.2. Could measurement or ascertainment of the outcome have differed between intervention groups? | N | N | |
| 4.3. If N/PN/NI to 4.1 and 4.2: Were outcome assessors aware of the intervention received by study participants? | Y | N | |
| 4.4. If Y/PY/NI to 4.3: Could assessment of the outcome have been influenced by knowledge of intervention received? | Y | N | |
| 4.5. If Y/PY/NI to 4.4: Is it likely that assessment of the outcome was influenced by knowledge of intervention received? | N | / | |
| Risk of bias judgement | Some concerns | Low | |
| Domain 5: Selection of the reported result | 5.1. Were the data that produced this result analysed in accordance with a pre-specified analysis plan that was finalised before unblinded outcome data were available for analysis? | Y | Y |
| Is the numerical result being assessed likely to have been selected on the basis of the results from … | |||
| 5.2. multiple eligible outcome measurements (e.g., scales, definitions, timepoints) within the outcome domain? | N | N | |
| 5.3. multiple eligible analyses of the data? | N | N | |
| Risk of bias judgement | Low | Low | |
| Overall Risk of Bias | Some concerns | Low | |
| Elimimian (2020) [4] | Chang (2022) [5] | ||
|---|---|---|---|
| Bias due to confounding | Potential for confounding? | N | N |
| Appropriate analysis method to control for all the important confounding domains? | Y | Y | |
| Risk of Bias | Low | Low | |
| Bias in selection of participants into the study | Selection based on participants characteristic observed after the start of the intervention? | N | N |
| Most participants followed from the start of the intervention? | Y | Y | |
| Risk of Bias | Low | Low | |
| Bias in classification of interventions | Intervention groups clearly defined? | Y | Y |
| Risk of Bias | Low | Low | |
| Bias due to deviation from intended interventions | Deviations from intended interventions (e.g., High drop-out rate)? | N | N |
| Deviation unbalanced between groups? | N | N | |
| Risk of bias | Low | Low | |
| Bias due to missing data | Outcome data available for nearly all participants? | Y | Y |
| Participants excluded due to missing data? | N | N | |
| Risk of Bias | Low | Low | |
| Bias in measurement of outcomes | Could the outcome measure have been influenced by knowledge of the intervention received? | N | N |
| Were outcome assessors aware of the intervention received by study participants? | NI | N | |
| Were the methods of outcome assessment comparable across intervention groups? | Y | Y | |
| Risk of Bias | Moderate | Low | |
| Bias in selection of the reported result | Results likely to be selected from multiple measurements? | N | N |
| Risk of bias | Low | Low | |
| Randomisation | N | N | |
| Overall risk of bias | Moderate | Low | |
| Test Score | Result |
|---|---|
| 0–4 | Minimal Anxiety |
| 5–9 | Mild Anxiety |
| 10–14 | Moderate Anxiety |
| 15–21 | Severe Anxiety |
| Test Score | Result |
|---|---|
| 0–4 | Minimal Depressive Symptoms |
| 5–9 | Mild Depressive Symptoms |
| 10–14 | Moderate Depressive Symptoms |
| 15–27 | Severe Depressive Symptoms |
| Depression | Anxiety | Stress | |
|---|---|---|---|
| Normal | 0–4 | 0–3 | 0–7 |
| Mild | 5–6 | 4–5 | 8–9 |
| Moderate | 7–10 | 6–7 | 10–12 |
| Severe | 11–13 | 8–9 | 13–16 |
| Extremely Severe | >14 | >10 | >17 |
| Test Score | Result |
|---|---|
| 0–21 | Mild Anxiety |
| 22–35 | Moderate Anxiety |
| >36 | Severe Anxiety |
| Measured (via) | Significant Change | ||
|---|---|---|---|
| Elimimian et al. (2020) [4] | 36-SF | MCS-subscore | Yes |
| PCS-subscore | No | ||
| Lengacher et al. (2017) [6] | 36-SF | Cortisol | No |
| IL-6 | Yes | ||
| Chang et al. (2022) [5] | EQ-5D | No | |
| Zhang et al. (2018) [9] | Meta-analysis | No | |
| Chang et al. (2020) [8] | Meta-analysis | No | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ladenbauer, S.; Singer, J. Can Mindfulness-Based Stress Reduction Influence the Quality of Life, Anxiety, and Depression of Women Diagnosed with Breast Cancer? —A Review. Curr. Oncol. 2022, 29, 7779-7793. https://doi.org/10.3390/curroncol29100615
Ladenbauer S, Singer J. Can Mindfulness-Based Stress Reduction Influence the Quality of Life, Anxiety, and Depression of Women Diagnosed with Breast Cancer? —A Review. Current Oncology. 2022; 29(10):7779-7793. https://doi.org/10.3390/curroncol29100615
Chicago/Turabian StyleLadenbauer, Severin, and Josef Singer. 2022. "Can Mindfulness-Based Stress Reduction Influence the Quality of Life, Anxiety, and Depression of Women Diagnosed with Breast Cancer? —A Review" Current Oncology 29, no. 10: 7779-7793. https://doi.org/10.3390/curroncol29100615
APA StyleLadenbauer, S., & Singer, J. (2022). Can Mindfulness-Based Stress Reduction Influence the Quality of Life, Anxiety, and Depression of Women Diagnosed with Breast Cancer? —A Review. Current Oncology, 29(10), 7779-7793. https://doi.org/10.3390/curroncol29100615





