Postoperative Patient-Reported Outcomes after Uniportal Video-Assisted Thoracoscopic Surgery Using the Perioperative Symptom Assessment for Lung Surgery Scale
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Patient-Reported Outcome Measurements and Data Collection
2.3. Interview Regarding Coughing
2.4. Statistical Analyses
3. Results
3.1. Patients’ Characteristics
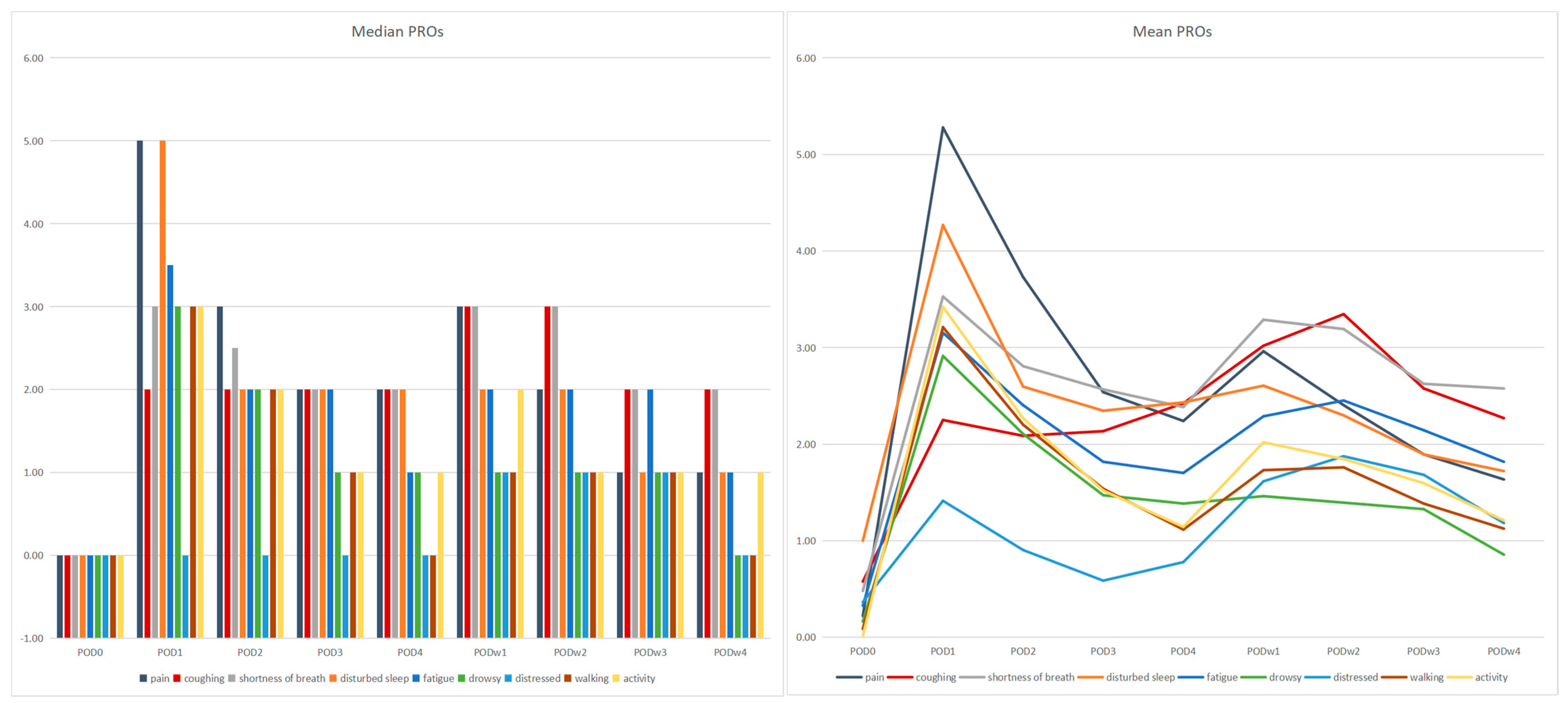
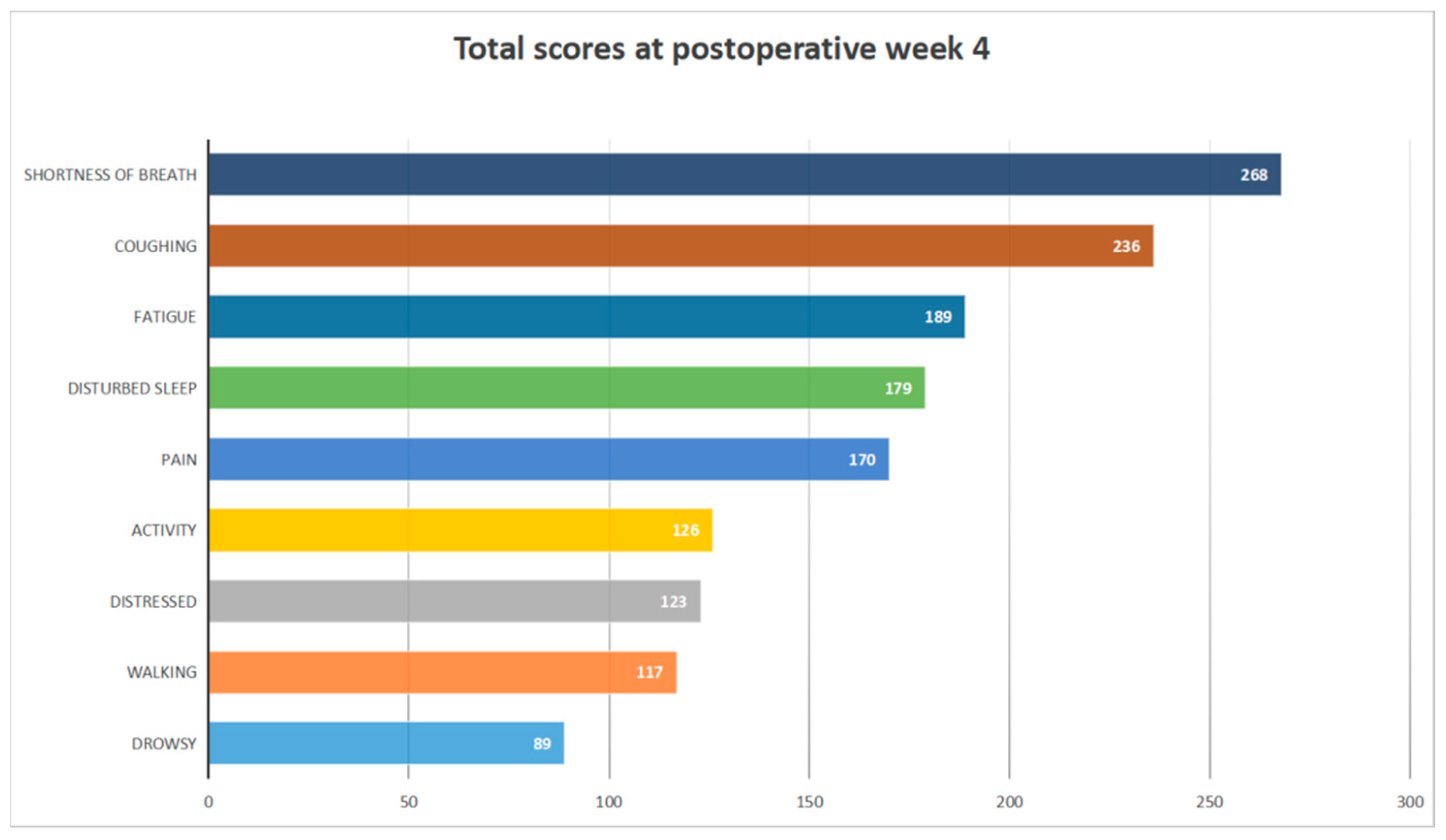
3.2. Patient-Reported Outcome Characteristics
3.3. Interview Regarding Coughing
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kato, H.; Oizumi, H.; Suzuki, J.; Suzuki, K.; Takamori, S. Roles and outcomes of thoracoscopic anatomic lung subsegmentectomy for lung cancer. Interact. Cardiovasc. Thorac. Surg. 2021, 34, 81–90. [Google Scholar] [CrossRef] [PubMed]
- Mei, J.; Pu, Q.; Liao, H.; Liu, L. Initial experience of video-assisted thoracic surgery left upper sleeve lobectomy for lung cancer: Case report and literature review. Thorac. Cancer 2011, 3, 348–352. [Google Scholar] [CrossRef] [PubMed]
- Hartwig, M.G.; D’Amico, T.A. Thoracoscopic lobectomy: The gold standard for early-stage lung cancer? Ann. Thorac. Surg. 2010, 89, S2098–S2101. [Google Scholar] [CrossRef]
- He, J. Thoracic Oncology; People’s Medical Publishing House: Beijing, China, 2013. [Google Scholar]
- Lewis, R.J.; Caccavale, R.J.; Sisler, G.E.; Mackenzie, J.W. One hundred consecutive patients undergoing video-assisted thoracic operations. Ann. Thorac. Surg. 1992, 54, 421–426. [Google Scholar] [CrossRef]
- Wei, X.; Yu, H.; Dai, W.; Mu, Y.; Wang, Y.; Liao, J.; Peng, L.; Han, Y.; Li, Q.; Shi, Q. Patient-Reported Outcomes of Video-Assisted Thoracoscopic Surgery Versus Thoracotomy for Locally Advanced Lung Cancer: A Longitudinal Cohort Study. Ann. Surg. Oncol. 2021, 28, 8358–8371. [Google Scholar] [CrossRef]
- Rocco, G.; Martin-Ucar, A.; Passera, E. Uniportal VATS wedge pulmonary resections. Ann. Thorac. Surg. 2004, 77, 726–728. [Google Scholar] [CrossRef]
- Salati, M.; Brunelli, A.; Xiumè, F.; Refai, M.; Sciarra, V.; Soccetti, A.; Sabbatini, A. Uniportal video-assisted thoracic surgery for primary spontaneous pneumothorax: Clinical and economic analysis in comparison to the traditional approach. Interact. Cardiovasc. Thorac. Surg. 2008, 7, 63–66. [Google Scholar] [CrossRef]
- Gonzalez-Rivas, D.; Fernandez, R.; De La Torre, M.; Bonome, C. Uniportal video-assisted thoracoscopic left upper lobectomy under spontaneous ventilation. J. Thorac. Dis. 2015, 7, 494–495. [Google Scholar] [CrossRef]
- Gonzalez, D.; Paradela, M.; Garcia, J.; Torre, M.D. Single-port video-assisted thoracoscopic lobectomy. Interact. Cardiovasc. Thorac. Surg. 2011, 12, 514–515. [Google Scholar] [CrossRef]
- Jutley, R.S.; Khalil, M.W.; Rocco, G. Uniportal vs. standard three-port VATS technique for spontaneous pneumothorax: Comparison of post-operative pain and residual paraesthesia. Eur. J. Cardio-Thoracic Surg. 2005, 28, 43–46. [Google Scholar] [CrossRef]
- Dai, W.; Dai, Z.; Wei, X.; Pompili, C.; Shi, Q.-L.; Xie, T.-P.; He, J.-T.; Li, Q. Early Patient-Reported Outcomes after Uniportal vs. Multiportal Thoracoscopic Lobectomy. Ann. Thorac. Surg. 2021, 114, 1229–1237. [Google Scholar] [CrossRef] [PubMed]
- Basch, E.; Deal, A.M.; Dueck, A.C.; Scher, H.I.; Kris, M.G.; Hudis, C.; Schrag, D. Overall Survival Results of a Trial Assessing Patient-Reported Outcomes for Symptom Monitoring during Routine Cancer Treatment. JAMA 2017, 318, 197–198. [Google Scholar] [CrossRef] [PubMed]
- Dai, W.; Chang, S.; Pompili, C.; Bin Qiu, B.; Wei, X.; Mu, Y.; Zhang, R.; Shen, C.; Shi, Q.; Li, Q.; et al. Early Postoperative Patient-Reported Outcomes after Thoracoscopic Segmentectomy Versus Lobectomy for Small-Sized Peripheral Non-small-cell Lung Cancer. Ann. Surg. Oncol. 2021, 29, 547–556. [Google Scholar] [CrossRef] [PubMed]
- Reponen, E.; Korja, M.; Tuominen, H. Simple Preoperative Patient-Reported Factors Predict Adverse Outcome after Elective Cranial Neurosurgery. Neurosurgery 2017, 83, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Basch, E. Patient-Reported Outcomes—Harnessing Patients’ Voices to Improve Clinical Care. N. Engl. J. Med. 2017, 376, 105–108. [Google Scholar] [CrossRef]
- Dai, W.; Feng, W.; Zhang, Y.; Wang, X.S.; Liu, Y.; Pompili, C.; Xu, W.; Xie, S.; Wang, Y.; Liao, J.; et al. Patient-Reported Outcome-Based Symptom Management Versus Usual Care after Lung Cancer Surgery: A Multicenter Randomized Controlled Trial. J. Clin. Oncol. 2022, 40, 988–996. [Google Scholar] [CrossRef]
- Rossi, L.A.; Melstrom, L.G.; Fong, Y.; Sun, V. Predicting post-discharge cancer surgery complications via telemonitoring of patient-reported outcomes and patient-generated health data. J. Surg. Oncol. 2021, 123, 1345–1352. [Google Scholar] [CrossRef]
- Bouazza, Y.B.; Chiairi, I.; El Kharbouchi, O.; De Backer, L.; Vanhoutte, G.; Janssens, A.; Van Meerbeeck, J.P. Patient-reported outcome measures (PROMs) in the management of lung cancer: A systematic review. Lung Cancer 2017, 113, 140–151. [Google Scholar] [CrossRef]
- Fagundes, C.P.; Shi, Q.; Vaporciyan, A.A.; Rice, D.C.; Popat, K.U.; Cleeland, C.S.; Wang, X.S. Symptom recovery after thoracic surgery: Measuring patient-reported outcomes with the MD Anderson Symptom Inventory. J. Thorac. Cardiovasc. Surg. 2015, 150, 613–619.e2. [Google Scholar] [CrossRef]
- Mendoza, T.R.; Wang, X.S.; Lu, C.; Palos, G.R.; Liao, Z.; Mobley, G.M.; Kapoor, S.; Cleeland, C.S. Measuring the Symptom Burden of Lung Cancer: The Validity and Utility of the Lung Cancer Module of the M. D. Anderson Symptom Inventory. Oncol. 2011, 16, 217–227. [Google Scholar] [CrossRef]
- Xu, W.; Dai, W.; Gao, Z.; Wang, X.S.; Tang, L.; Pu, Y.; Yu, Q.; Yu, H.; Nie, Y.; Zhuang, W.; et al. Establishment of Minimal Clinically Important Improvement for Patient-Reported Symptoms to Define Recovery after Video-Assisted Thoracoscopic Surgery. Ann. Surg. Oncol. 2022, 29, 5593–5604. [Google Scholar] [CrossRef] [PubMed]
- Shawd, M. 28th Annual Conference of the International Society for Quality of Life Research. Qual. Life Res. 2021, 30 (Suppl. S1), 1–177. [Google Scholar]
- NCCN Guidelines Version 2.2022 Adult Cancer Pain; NCCN.org (National Comprehensive Cancer Network): Plymouth Meeting, PA, USA, 2022.
- NCCN Guidelines Version 2.2022 Cancer-Related Fatigue; NCCN.org (National Comprehensive Cancer Network): Plymouth Meeting, PA, USA, 2022.
- NCCN Guidelines Version 2.2022 Distress Management; NCCN.org (National Comprehensive Cancer Network): Plymouth Meeting, PA, USA, 2022.
- Wei, X.; Liu, Y.; Yu, H.; Dai, W.; Yang, D.; Zhang, K.; Sun, J.; Xu, W.; Gong, R.; Yu, Q.; et al. Protocol of an iterative qualitative study to develop a molecular testing decision aid for shared decision-making in patients with lung cancer after surgery. BMJ Open 2022, 12, e061367. [Google Scholar] [CrossRef]
- Khullar, O.V.; Rajaei, M.H.; Force, S.D.; Binongo, J.N.; Lasanajak, Y.; Robertson, S.; Pickens, A.; Sancheti, M.S.; Lipscomb, J.; Gillespie, T.W.; et al. Pilot Study to Integrate Patient Reported Outcomes after Lung Cancer Operations into the Society of Thoracic Surgeons Database. Ann. Thorac. Surg. 2017, 104, 245–253. [Google Scholar] [CrossRef] [PubMed]
- Boffa, D.J.; Kosinski, A.S.; Furnary, A.P.; Kim, S.; Onaitis, M.W.; Tong, B.C.; Cowper, P.A.; Hoag, J.R.; Jacobs, J.P.; Wright, C.D.; et al. Minimally Invasive Lung Cancer Surgery Performed by Thoracic Surgeons as Effective as Thoracotomy. J. Clin. Oncol. 2018, 36, 2378–2385. [Google Scholar] [CrossRef]
- Berfield, K.K.; Farjah, F.; Mulligan, M.S. Video-Assisted Thoracoscopic Lobectomy for Lung Cancer. Ann. Thorac. Surg. 2018, 107, 603–609. [Google Scholar] [CrossRef]
- Li, N.; Tan, F.W.; Qiu, B.; Li, J.G.; Zhao, J.; Gao, Y.S.; Wang, D.L.; Mao, Y.; Xue, Q.; Mu, J.W.; et al. Comparison of lung cancer surgery in China, 2005 vs. 2015. Zhonghua Zhong Liu Za Zhi [Chin. J. Oncol.] 2018, 40, 300–302. [Google Scholar]
- Wei, X.; Yu, H.; Dai, W.; Xu, W.; Yu, Q.; Pu, Y.; Wang, Y.; Liao, J.; Li, Q.; Shi, Q. Discrepancy in the perception of symptoms among patients and healthcare providers after lung cancer surgery. Support. Care Cancer 2021, 30, 1169–1179. [Google Scholar] [CrossRef]
- Bendixen, M.; Jørgensen, O.D.; Kronborg, C.; Andersen, C.; Licht, P.B. Postoperative pain and quality of life after lobectomy via video-assisted thoracoscopic surgery or anterolateral thoracotomy for early stage lung cancer: A randomised controlled trial. Lancet Oncol. 2016, 17, 836–844. [Google Scholar] [CrossRef]
- Miller, J.I. Physiologic evaluation of pulmonary function in the candidate for lung resection. J. Thorac. Cardiovasc. Surg. 1993, 105, 347–352. [Google Scholar] [CrossRef]
- Iizasa, T.; Suzuki, M.; Yasufuku, K.; Iyoda, A.; Otsuji, M.; Yoshida, S.; Sekine, Y.; Shibuya, K.; Saitoh, Y.; Hiroshima, K.; et al. Preoperative pulmonary function as a prognostic factor for stage I non–small cell lung carcinoma. Ann. Thorac. Surg. 2004, 77, 1896–1902. [Google Scholar] [CrossRef] [PubMed]
- Berry, M.F.; Villamizar-Ortiz, N.R.; Tong, B.C.; Burfeind, W.R.; Harpole, D.H.; D’Amico, T.A.; Onaitis, M.W. Pulmonary Function Tests Do Not Predict Pulmonary Complications after Thoracoscopic Lobectomy. Ann. Thorac. Surg. 2010, 89, 1044–1052. [Google Scholar] [CrossRef] [PubMed]
- Licker, M.J.; Widikker, I.; Robert, J.; Frey, J.-G.; Spiliopoulos, A.; Ellenberger, C.; Schweizer, A.; Tschopp, J.-M. Operative Mortality and Respiratory Complications after Lung Resection for Cancer: Impact of Chronic Obstructive Pulmonary Disease and Time Trends. Ann. Thorac. Surg. 2006, 81, 1830–1837. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Liu, X.; Jia, Y.; Xie, J. Impact of breathing exercises in subjects with lung cancer undergoing surgical resection: A systematic review and meta-analysis. J. Clin. Nurs. 2018, 28, 717–732. [Google Scholar] [CrossRef] [PubMed]
| Variable | Total | Pain | p Value | Cough | p Value | SOB | p Value | DS | p Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0–3 | >3 | 0–3 | >3 | 0–3 | >3 | 0–3 | >3 | ||||||||
| Patients (number) | 104 | 94 | 10 | / | 84 | 20 | / | 82 | 22 | / | 90 | 14 | / | ||
| Age (year), median | 57 | 57 | 62.5 | 0.11 | 57 | 60 | 0.52 | 56 | 60.5 | 0.05 | 57 | 62.5 | 0.34 | ||
| Female/male | 60/44 | 54/40 | 4/6 | 1 | 51/33 | 9/11 | 0.22 | 48/32 | 12/10 | 0.81 | 52/38 | 8/6 | 1 | ||
| BMI, mean | 23.83 | 23.73 | 24.81 | 0.48 | 23.86 | 23.75 | 0.98 | 23.69 | 24.38 | 0.38 | 23.77 | 24.26 | 0.33 | ||
| Smoking index, median | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | ||
| Education level | 0.19 | 0.78 | 0.64 | 0.77 | |||||||||||
| Middle school or below | 61 | 53 | 8 | 53 | 8 | 47 | 14 | 52 | 9 | ||||||
| Above middle school | 43 | 41 | 2 | 31 | 12 | 35 | 8 | 38 | 5 | ||||||
| FEV1, median | 2.63 | 2.66 | 2.11 | 0.01 | 2.64 | 2.39 | 0.38 | 2.64 | 2.47 | 0.15 | 2.64 | 2.18 | 0.02 | ||
| FEV1%, mean | 101.23 | 102.81 | 86.39 | 0.01 | 104.09 | 89.20 | 0.00 | 103.46 | 92.92 | 0.02 | 103.46 | 86.90 | 0.00 | ||
| FEV1%FVC, mean | 79.97 | 80.37 | 76.20 | 0.13 | 79.96 | 79.99 | 0.77 | 80.29 | 78.76 | 0.51 | 80.50 | 76.52 | 0.13 | ||
| MVV, mean | 86.76 | 89.99 | 56.38 | 0.00 | 88.26 | 80.44 | 0.17 | 89.30 | 77.30 | 0.08 | 89.29 | 70.52 | 0.03 | ||
| MVV%, mean | 83.31 | 86.15 | 56.53 | 0.00 | 85.83 | 72.72 | 0.01 | 85.73 | 74.27 | 0.03 | 85.38 | 69.96 | 0.04 | ||
| DLCO SB, median | 7.82 | 7.92 | 7.08 | 0.14 | 7.88 | 7.60 | 0.73 | 7.82 | 7.79 | 0.63 | 7.88 | 7.60 | 0.71 | ||
| DLCO SB%, mean | 94.34 | 94.98 | 88.31 | 0.24 | 95.35 | 90.12 | 0.13 | 94.31 | 94.46 | 0.77 | 94.81 | 91.29 | 0.51 | ||
| Tumor pathologic stage | 0.46 | 0.90 | 0.70 | 0.30 | |||||||||||
| Tis | 15 | 15 | 0 | 12 | 3 | 12 | 3 | 14 | 1 | ||||||
| I | 64 | 57 | 7 | 52 | 12 | 49 | 15 | 57 | 7 | ||||||
| II | 4 | 3 | 1 | 3 | 1 | 3 | 1 | 3 | 1 | ||||||
| III | 3 | 3 | 0 | 2 | 1 | 2 | 1 | 2 | 1 | ||||||
| Benign or other tumor | 18 | 16 | 2 | 15 | 3 | 16 | 2 | 14 | 4 | ||||||
| Tumor histologic type | 0.28 | 0.15 | 1.00 | 0.51 | |||||||||||
| Adenocarcinoma | 77 | 71 | 6 | 65 | 12 | 61 | 16 | 68 | 9 | ||||||
| Non-adenocarcinoma | 27 | 23 | 4 | 19 | 8 | 21 | 6 | 22 | 5 | ||||||
| Extent of the procedure | 0.55 | 0.29 | 0.58 | 0.46 | |||||||||||
| Pneumonectomy | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | ||||||
| Lobectomy | 39 | 34 | 5 | 32 | 7 | 29 | 10 | 32 | 7 | ||||||
| Sub-lobar | 64 | 59 | 5 | 52 | 12 | 52 | 12 | 57 | 7 | ||||||
| Type of lymphadenectomy | 1.00 | 0.79 | 0.81 | 1.00 | |||||||||||
| Systematic dissection | 92 | 83 | 9 | 73 | 19 | 71 | 21 | 79 | 13 | ||||||
| Sampling | 10 | 9 | 1 | 9 | 1 | 9 | 1 | 9 | 1 | ||||||
| Not performed | 2 | 2 | 0 | 2 | 0 | 2 | 0 | 2 | 0 | ||||||
| Operation time(minute), median | 106 | 106.5 | 116 | 0.93 | 107 | 104.5 | 0.64 | 106.5 | 106 | 0.80 | 105.5 | 119 | 0.41 | ||
| Variable | fatigue | p value | drowsy | p value | distressed | p value | walking | p value | activity | p value | |||||
| 0–3 | >3 | 0–3 | >3 | 0–3 | >3 | 0–3 | >3 | 0–3 | >3 | ||||||
| Patients (number) | 89 | 15 | / | 99 | 5 | / | 93 | 11 | / | 94 | 10 | / | 96 | 8 | / |
| Age (year), median | 56 | 65 | 0.00 | 57 | 69 | 0.01 | 57 | 64 | 0.04 | 56.5 | 66 | 0.01 | 57 | 66 | 0.02 |
| Female/male | 54/37 | 6/9 | 0.163 | 60/39 | 0/5 | 0.012 | 56/37 | 4/7 | 0.196 | 55/39 | 5/5 | 0.74 | 56/40 | 4/4 | 0.719 |
| BMI, mean | 23.69 | 24.68 | 0.25 | 23.86 | 23.29 | 0.84 | 23.80 | 24.10 | 0.65 | 23.86 | 23.64 | 0.96 | 23.79 | 24.33 | 0.40 |
| Smoking index, median | 0 | 200 | 0 | 0 | 900 | 0 | 0 | 300 | 0 | 0 | 150 | 0 | 0 | 150 | 0 |
| Education level | 0.09 | 1.00 | 0.76 | 0.74 | 0.72 | ||||||||||
| Middle school or below | 49 | 12 | 58 | 3 | 55 | 6 | 56 | 5 | 57 | 4 | |||||
| Above middle school | 40 | 3 | 41 | 2 | 38 | 5 | 38 | 5 | 39 | 4 | |||||
| FEV1, median | 2.64 | 2.18 | 0.05 | 2.63 | 1.98 | 0.09 | 2.64 | 2.04 | 0.01 | 2.66 | 2.01 | 0.00 | 2.64 | 2.01 | 0.00 |
| FEV1%, mean | 103.57 | 87.32 | 0.00 | 102.48 | 76.38 | 0.01 | 103.88 | 78.76 | 0.00 | 103.49 | 79.96 | 0.00 | 103.09 | 78.90 | 0.00 |
| FEV1%FVC, mean | 80.62 | 76.07 | 0.02 | 80.36 | 72.09 | 0.04 | 80.59 | 74.69 | 0.05 | 80.42 | 75.66 | 0.09 | 80.36 | 75.28 | 0.60 |
| MVV, mean | 90.24 | 66.11 | 0.00 | 88.09 | 60.46 | 0.04 | 89.88 | 60.38 | 0.00 | 90.04 | 55.89 | 0.00 | 89.65 | 52.10 | 0.00 |
| MVV%, mean | 86.71 | 63.11 | 0.00 | 84.70 | 55.78 | 0.02 | 86.48 | 56.50 | 0.00 | 86.26 | 55.58 | 0.00 | 86.00 | 51.04 | 0.00 |
| DLCO SB, median | 7.90 | 7.53 | 0.76 | 7.90 | 6.19 | 0.09 | 7.90 | 7.48 | 0.84 | 7.91 | 6.65 | 0.30 | 7.88 | 7.09 | 0.74 |
| DLCO SB%, mean | 94.84 | 91.37 | 0.23 | 95.28 | 75.74 | 0.03 | 94.84 | 90.11 | 0.19 | 95.08 | 87.37 | 0.06 | 94.60 | 91.28 | 0.21 |
| Tumor pathologic stage | 0.07 | 1.00 | 0.68 | 0.65 | 0.63 | ||||||||||
| Tis | 15 | 0 | 15 | 0 | 14 | 1 | 13 | 2 | 14 | 1 | |||||
| I | 54 | 10 | 60 | 4 | 56 | 8 | 28 | 6 | 59 | 5 | |||||
| II | 2 | 2 | 4 | 0 | 3 | 1 | 3 | 1 | 3 | 1 | |||||
| III | 2 | 1 | 3 | 0 | 3 | 0 | 3 | 0 | 3 | 0 | |||||
| Benign or other tumor | 16 | 2 | 17 | 1 | 17 | 1 | 17 | 1 | 17 | 1 | |||||
| Tumor histologic type | 0.21 | 0.11 | 0.15 | 0.28 | 0.43 | ||||||||||
| Adenocarcinoma | 68 | 9 | 75 | 2 | 71 | 6 | 71 | 6 | 72 | 5 | |||||
| Non-adenocarcinoma | 21 | 6 | 24 | 3 | 22 | 5 | 23 | 4 | 24 | 3 | |||||
| Extent of the procedure | 0.36 | 0.40 | 0.40 | 0.11 | 0.12 | ||||||||||
| Pneumonectomy | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | |||||
| Lobectomy | 31 | 8 | 36 | 3 | 33 | 6 | 32 | 7 | 33 | 6 | |||||
| Sub-lobar | 57 | 7 | 62 | 2 | 59 | 5 | 61 | 3 | 62 | 2 | |||||
| Type of lymphadenectomy | 1.00 | 1.00 | 0.68 | 0.67 | 1.00 | ||||||||||
| Systematic dissection | 78 | 14 | 87 | 5 | 81 | 11 | 82 | 10 | 84 | 8 | |||||
| Sampling | 9 | 1 | 10 | 0 | 10 | 0 | 10 | 0 | 10 | 0 | |||||
| Not performed | 2 | 0 | 2 | 0 | 2 | 0 | 2 | 0 | 2 | 0 | |||||
| Operation time (minute), median | 107 | 101 | 0.89 | 107 | 101 | 0.93 | 105 | 127 | 0.37 | 105 | 143 | 0.05 | 105 | 143 | 0.08 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, D.; Hong, Q.; Zhao, C.; Mu, J. Postoperative Patient-Reported Outcomes after Uniportal Video-Assisted Thoracoscopic Surgery Using the Perioperative Symptom Assessment for Lung Surgery Scale. Curr. Oncol. 2022, 29, 7645-7654. https://doi.org/10.3390/curroncol29100604
Yang D, Hong Q, Zhao C, Mu J. Postoperative Patient-Reported Outcomes after Uniportal Video-Assisted Thoracoscopic Surgery Using the Perioperative Symptom Assessment for Lung Surgery Scale. Current Oncology. 2022; 29(10):7645-7654. https://doi.org/10.3390/curroncol29100604
Chicago/Turabian StyleYang, Ding, Qian Hong, Chenguang Zhao, and Juwei Mu. 2022. "Postoperative Patient-Reported Outcomes after Uniportal Video-Assisted Thoracoscopic Surgery Using the Perioperative Symptom Assessment for Lung Surgery Scale" Current Oncology 29, no. 10: 7645-7654. https://doi.org/10.3390/curroncol29100604
APA StyleYang, D., Hong, Q., Zhao, C., & Mu, J. (2022). Postoperative Patient-Reported Outcomes after Uniportal Video-Assisted Thoracoscopic Surgery Using the Perioperative Symptom Assessment for Lung Surgery Scale. Current Oncology, 29(10), 7645-7654. https://doi.org/10.3390/curroncol29100604





