The Relationship between Cancer Caregiver Burden and Psychological Outcomes: The Moderating Role of Social Connectedness
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participant Recruitment
2.2. Measures
2.2.1. Sociodemographic Characteristics
2.2.2. Care-Related and Care Recipient Characteristics
2.2.3. Caregiver Burden
2.2.4. Social Connectedness
2.2.5. Depression and Anxiety
2.2.6. Statistical Analysis
3. Results
3.1. Participants
3.2. Preliminary Data Analyses
3.2.1. Relationships between Caregiver Sociodemographic and Care-Related Characteristics
3.2.2. Relationships between Main Study Variables (Depression, Anxiety, Burden, Social Connectedness) and Sociodemographic Characteristics
3.2.3. Relationships between Main Study Variables (Depression, Anxiety, Social Connectedness, Burden) and Care-Related Characteristics
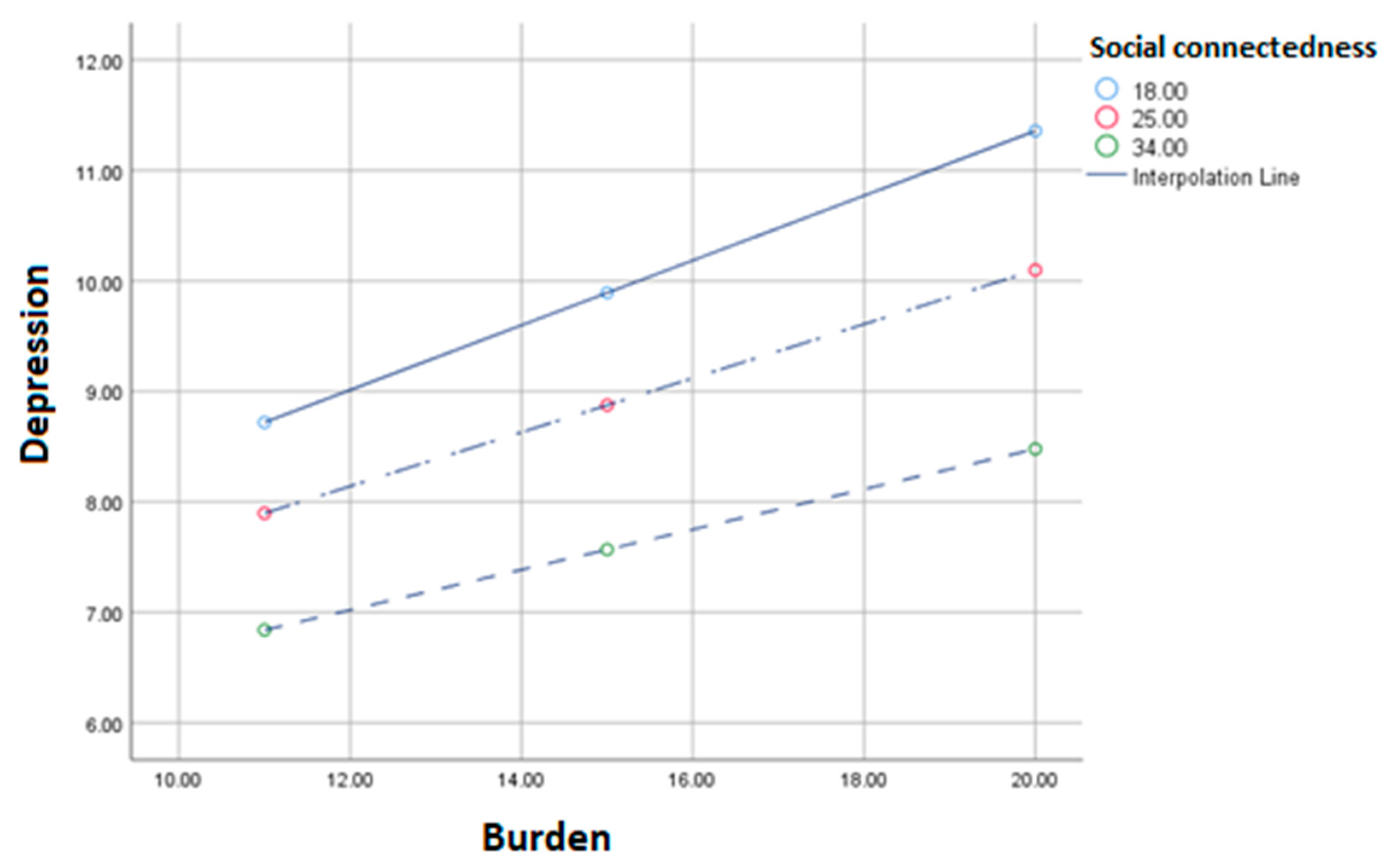
3.2.4. The Moderating Effect of Social Connectedness on the Relationship between Caregiver Burden and Depression and Anxiety Symptoms
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kent, E.E.; Mollica, M.A.; Buckenmaier, S.; Wilder Smith, A. The Characteristics of Informal Cancer Caregivers in the United States. Semin. Oncol. Nurs. 2019, 35, 328–332. [Google Scholar] [CrossRef]
- Sun, V.; Puts, M.; Haase, K.; Pilleron, S.; Hannan, M.; Sattar, S.; Strohscheing, F. The Role of Family Caregivers in the Care of Older Adults with Cancer. Semin. Oncol. Nurs. 2021, 37, 151232. [Google Scholar] [CrossRef]
- Ullgren, H.; Tsitsi, T.; Papastavrou, E.; Charalambous, A. How family caregivers of cancer patients manage symptoms at home: A systematic review. Int. J. Nurs. Stud. 2018, 85, 68–79. [Google Scholar] [CrossRef]
- Kent, E.E.; Rowland, J.H.; Northouse, L.; Litzelman, K.; Chou, W.Y.S.; Shelburne, N.; Timura, C.; O’Mara, A.; Huss, K. Caring for caregivers and patients: Research and clinical priorities for informal cancer caregiving. Cancer 2016, 122, 1987–1995. [Google Scholar] [CrossRef]
- Thana, K.; Lehto, R.; Sikorskii, A.; Wyatt, G. Informal caregiver burden for solid tumour cancer patients: A review and future directions. Psychol. Health 2021, 36, 1514–1535. [Google Scholar] [CrossRef]
- Ge, L.; Mordiffi, S.Z. Factors Associated with Higher Caregiver Burden among Family Caregivers of Elderly Cancer Patients: A Systematic Review. Cancer Nurs. 2017, 40, 471–478. [Google Scholar] [CrossRef] [PubMed]
- Lippiett, K.; Richardson, A.; Myall, M.; Cummings, A.; May, C.R. Patients and informal caregivers’ experiences of burden of treatment in lung cancer and chronic obstructive pulmonary disease (COPD): A systematic review. BMJ Open 2019, 9, e020515. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zarit, S.H.; Reever, K.E.; Bach-Peterson, J. Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist 1980, 20, 649–655. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Junkins, C.C.; Kent, E.; Litzelman, K.; Bevans, M.; Cannady, R.S.; Rosenberg, A.R. Cancer across the ages: A narrative review of caregiver burden for patients of all ages. J. Psychosoc. Oncol. 2020, 38, 782–798. [Google Scholar] [CrossRef]
- Lee, J.E.; Shin, D.W.; Cho, J.; Yang, H.K.; Kim, S.Y.; Yoo, H.S.; Jho, H.J.; Shin, J.Y.; Cho, B.; Park, K.; et al. Caregiver burden, patients’ self-perceived burden, and preference for palliative care among cancer patients and caregivers. Psychooncology 2015, 24, 1545–1551. [Google Scholar] [CrossRef]
- Kuzuya, M.; Enoki, H.; Hasegawa, J.; Izawa, S.; Hirakawa, Y.; Shimokata, H.; Akihisa, I. Impact of caregiver Burden on adverse health outcomes in community-dwelling dependent older care recipients. Am. J. Geriatr. Psychiatry 2011, 19, 382–391. [Google Scholar] [CrossRef]
- O’Rourke, H.; Sidani, S. Definition, determinants, and outcomes of social connectedness for older adults: A scoping review. J. Gerontol. Nurs. 2017, 43, 43–52. [Google Scholar] [CrossRef] [PubMed]
- O’Rourke, H.M.; Collins, L.; Sidani, S. Interventions to address social connectedness and loneliness for older adults: A scoping review. BMC Geriatr. 2018, 18, 214. [Google Scholar] [CrossRef]
- Langford, C.P.H.; Bowsher, J.; Maloney, J.P.; Lillis, P.P. Social support: A conceptual analysis. J. Adv. Nurs. 1997, 25, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.M.; Robbins, S.B. The Relationship between Social Connectedness and Anxiety, Self-Esteem, and Social Identity. J. Couns. Psychol. 1998, 45, 338–345. [Google Scholar] [CrossRef]
- Kim, T.; Nguyen, E.T.; Yuen, E.J.; Nguyen, T.; Sorn, R.; Nguyen, G.T. Differential role of social connectedness in geriatric depression among southeast Asian ethnic groups. Prog. Community Health Partnerships Res. Educ. Action 2015, 9, 483–493. [Google Scholar] [CrossRef]
- Jose, P.E.; Ryan, N.; Pryor, J. Does Social Connectedness Promote a Greater Sense of Well-Being in Adolescence Over Time? J. Res. Adolesc. 2012, 22, 235–251. [Google Scholar] [CrossRef]
- Arslan, G. Psychological Maltreatment, Social Acceptance, Social Connectedness, and Subjective Well-Being in Adolescents. J. Happiness Stud. 2018, 19, 983–1001. [Google Scholar] [CrossRef]
- Schwartz, E.; Shrira, A. Social Connectedness Moderates the Relationship between Warfare Exposure, PTSD Symptoms, and Health among Older Adults. Psychiatry 2019, 82, 158–172. [Google Scholar] [CrossRef]
- Schwartz, E.; Litwin, H. Warfare exposure in later life and cognitive function: The moderating role of social connectedness. Psychiatry Res. 2019, 278, 258–262. [Google Scholar] [CrossRef]
- Jeong, A.; An, J. The moderating role of social support on depression and anxiety for gastric cancer patients and their family caregivers. PLoS ONE 2017, 12. [Google Scholar] [CrossRef]
- Peer, E.; Brandimarte, L.; Samat, S.; Acquisti, A. Beyond the Turk: Alternative Platforms for Crowdsourcing Behavioral Research; Elsevier: Amsterdam, The Netherlands, 2017. [Google Scholar]
- Graessel, E.; Berth, H.; Lichte, T.; Grau, H. Subjective caregiver burden: Validity of the 10-item short version of the Burden Scale for Family Caregivers BSFC-s. BMC Geriatr. 2014, 14, 23. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.M.; Draper, M.; Lee, S. Social connectedness, dysfunctional interpersonal behaviors, and psychological distress: Testing a mediator model. J. Couns. Psychol. 2001, 48, 310–318. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [Green Version]
- Breeman, S.; Cotton, S.; Fielding, S.; Jones, G.T. Normative data for the Hospital Anxiety and Depression Scale. Qual. Life Res. 2015, 24, 391–398. [Google Scholar] [CrossRef] [Green Version]
- Djukanovic, I.; Carlsson, J.; Årestedt, K. Is the Hospital Anxiety and Depression Scale (HADS) a valid measure in a general population 65–80 years old? A psychometric evaluation study. Health Qual. Life Outcomes 2017, 15, 193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hinz, A.; Finck, C.; Gómez, Y.; Daig, I.; Glaesmer, H.; Singer, S. Anxiety and depression in the general population in Colombia: Reference values of the Hospital Anxiety and Depression Scale (HADS). Soc. Psychiatry Psychiatr. Epidemiol. 2014, 49, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Bjelland, I.; Dahl, A.A.; Haug, T.T.; Neckelmann, D. The validity of the Hospital Anxiety and Depression Scale: An updated literature review. J. Psychosom. Res. 2002, 52, 69–77. [Google Scholar] [CrossRef]
- Hayes, A. The PROCESS macro for SPSS and SAS (Version 3.3). Available online: https://www.processmacro.org/index.html (accessed on 3 February 2019).
- Hayes, A.F.; Matthes, J. Computational procedures for probing interactions in OLS and logistic regression: SPSS and SAS implementations. Behav. Res. Methods 2009, 41, 924–936. [Google Scholar] [CrossRef] [Green Version]
- García-Torres, F.; Jacek Jabłoński, M.; Gómez Solís, Á.; Moriana, J.A.; Jaén-Moreno, M.J.; Moreno-Díaz, M.J.; Aranda, E. Social support as predictor of anxiety and depression in cancer caregivers six months after cancer diagnosis: A longitudinal study. J. Clin. Nurs. 2020, 29, 996–1002. [Google Scholar] [CrossRef]
- Sibalija, J.; Savundranayagam, M.Y.; Orange, J.B.; Kloseck, M. Social support, social participation, & depression among caregivers and non-caregivers in Canada: A population health perspective. Aging Ment. Health 2020, 24, 765–773. [Google Scholar] [CrossRef] [PubMed]
- Challands, K.G.; Lacherez, P.; Obst, P.L. Does Online Social Connectedness Buffer Risk of Depression Following Driving Cessation? An Analysis of Older Drivers and Ex-Drivers. Cyberpsychol. Behav. Soc. Netw. 2017, 20, 232–237. [Google Scholar] [CrossRef]
- Taylor, C.T.; Pearlstein, S.L.; Kakaria, S.; Lyubomirsky, S.; Stein, M.B. Enhancing Social Connectedness in Anxiety and Depression Through Amplification of Positivity: Preliminary Treatment Outcomes and Process of Change. Cognit. Ther. Res. 2020, 44, 788–800. [Google Scholar] [CrossRef] [PubMed]
- Decadt, I.; Laenen, A.; Celus, J.; Geyskens, S.; Vansteenlandt, H.; Coolbrandt, A. Caregiver distress and quality of life in primary caregivers of oncology patients in active treatment and follow-up. Eur. J. Cancer Care 2021, 30, 23. [Google Scholar] [CrossRef] [PubMed]
- LeSeure, P.; Chongkham-Ang, S. The experience of caregivers living with cancer patients: A systematic review and meta-synthesis. J. Pers. Med. 2015, 5, 406–439. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Delalibera, M.; Barbosa, A.; Leal, I. Circumstances and consequences of care: Characterization of the family caregiver in palliative care. Cienc. Saude Coletiva 2018, 23, 1105–1117. [Google Scholar] [CrossRef] [Green Version]
- Balfe, M.; Keohane, K.; O’brien, K.; Sharp, L. Social networks, social support and social negativity: A qualitative study of head and neck cancer caregivers’ experiences. Eur. J. Cancer Care 2017, 26, 2015–2021. [Google Scholar] [CrossRef]
- van Roij, J.; Brom, L.; Youssef-El Soud, M.; van de Poll-Franse, L.; Raijmakers, N.J.H. Social consequences of advanced cancer in patients and their informal caregivers: A qualitative study. Support. Care Cancer 2019, 27, 1187–1195. [Google Scholar] [CrossRef] [Green Version]
- Steinman, L.; Parrish, A.; Mayotte, C.; Acevedo, P.B.; Torres, E.; Markova, M.; Boddie, M.; Lachenmayr, S.; Montoya, C.N.; Parker, L.; et al. Increasing Social Connectedness for Underserved Older Adults Living With Depression: A Pre-Post Evaluation of PEARLS. Am. J. Geriatr. Psychiatry 2021, 29, 828–842. [Google Scholar] [CrossRef]
- Given, B.A.; Sherwood, P.; Given, C.W. Support for Caregivers of Cancer Patients: Transition after Active Treatment. Cancer Epidemiol. Biomark. Prev. 2011, 20, 2015–2021. [Google Scholar] [CrossRef] [Green Version]
- Geng, H.; Chuang, D.; Yang, F.; Yang, Y.; Liu, W.; Liu, L.; Tian, H. Prevalence and determinants of depression in caregivers of cancer patients: A systematic review and meta-analysis. Medicine 2018, 97. [Google Scholar] [CrossRef] [PubMed]
- Fu, F.; Zhao, H.; Tong, F.; Chi, I. A systematic review of psychosocial interventions to cancer caregivers. Front. Psychol. 2017, 8, 834. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Sociodemographic Characteristic | Total Sample (n = 189) | |
|---|---|---|
| n | % | |
| Gender | ||
| Male | 36 | 19% |
| Female | 152 | 80.4% |
| Non-binary | 1 | 0.5% |
| Education | ||
| High school (years 7–12) | 27 | 14.3% |
| Vocational | 47 | 24.9% |
| University (undergraduate) | 77 | 40.7% |
| University (postgraduate) | 38 | 20.1% |
| Speaks English at home | 188 | 99.5% |
| Marital status | ||
| Single | 43 | 22.8% |
| In a relationship | 134 | 70.9% |
| Divorced | 7 | 3.7% |
| Widowed | 5 | 2.6% |
| The care recipient is my: | ||
| Spouse/Partner | 20 | 10.6% |
| Mother/Father | 79 | 41.8% |
| Other family member | 40 | 21.1% |
| Friend/Other | 42 | 22.2% |
| Country residing | ||
| UK | 169 | 89.4% |
| Other | 20 | 10.6% |
| Illness/Disability | ||
| None | 106 | 56.1% |
| One condition | 66 | 34.9% |
| Two or more conditions | 17 | 9% |
| Live with care recipient | ||
| Yes, lived with them before diagnosis | 39 | 20.6% |
| Yes, began living with them after diagnosis | 26 | 13.8% |
| No | 124 | 65.6% |
| Care recipient cancer diagnosis type | ||
| Blood cancer | 19 | 10.1% |
| Breast cancer | 42 | 22.2% |
| Gastrointestinal | 17 | 9.0% |
| Genitourinary | 33 | 17.4% |
| Gynecological | 16 | 8.5% |
| Lung cancer | 25 | 13.2% |
| Other | 37 | 19.6% |
| Care recipient currently receiving treatment | ||
| Yes | 155 | 82% |
| No | 34 | 18% |
| Variable | Mean | SD | Correlation Matrix | |||||
|---|---|---|---|---|---|---|---|---|
| Depression | Anxiety | Caregiver Burden | Social Connectedness | Age | Illness/Disability | |||
| Main Study Variables | ||||||||
| Depression | 8.99 | 3.29 | ||||||
| Anxiety | 11.40 | 4.00 | 0.577 ** | |||||
| Caregiver burden | 15.47 | 5.44 | 0.612 ** | 0.522 ** | ||||
| Social connectedness | 26.04 | 7.66 | −0.575 ** | −0.547 ** | −0.561 ** | |||
| Demographic characteristics | ||||||||
| Age | 36.19 | 11.78 | 0.063 | −0.155 * | 0.093 | 0.074 | ||
| Number of caregiver illness/disability | 0.55 | 0.74 | 0.193 ** | 0.163 ** | 0.143 ** | −0.086 | 0.061 | |
| Caregiver characteristics | ||||||||
| Caregiving duration (years) | 2.44 | 3.37 | 0.129 | −0.006 | 0.080 | −0.075 | 0.124 | 0.120 |
| Main Study Variable | Live with Care Recipient (n = 65) | Does Not Live with the Care Recipient (n = 124) | |||||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | df | T | sig | |
| Depression | 9.71 | 3.59 | 8.62 | 3.09 | 187 | −2.18 | 0.03 |
| Anxiety | 12.34 | 3.72 | 10.90 | 4.07 | 187 | −2.37 | 0.02 |
| Caregiver burden | 16.88 | 5.85 | 14.73 | 5.09 | 187 | −2.62 | 0.009 |
| Social connectedness | 23.95 | 7.69 | 27.15 | 7.44 | 187 | 2.77 | 0.006 |
| Effect *, Variable | β | se | t | p-Value | LLCI | ULCI |
|---|---|---|---|---|---|---|
| Direct effect of predictor (caregiver burden) on depression | 0.418 | 0.094 | 4.464 | <0.001 | 0.233 | 0.603 |
| Direct effect of moderator (perceived social connectedness) on depression | −0.041 | 0.059 | −0.695 | 0.488 | −0.158 | 0.076 |
| Direct interaction effect (caregiver burden x perceived social connectedness) on depression | −0.007 | 0.003 | −2.026 | 0.04 | −0.014 | −0.0002 |
| R2 = 0.478, F(6, 182) = 27.747, p < 0.001 | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yuen, E.Y.N.; Wilson, C.J. The Relationship between Cancer Caregiver Burden and Psychological Outcomes: The Moderating Role of Social Connectedness. Curr. Oncol. 2022, 29, 14-26. https://doi.org/10.3390/curroncol29010002
Yuen EYN, Wilson CJ. The Relationship between Cancer Caregiver Burden and Psychological Outcomes: The Moderating Role of Social Connectedness. Current Oncology. 2022; 29(1):14-26. https://doi.org/10.3390/curroncol29010002
Chicago/Turabian StyleYuen, Eva Y. N., and Carlene J. Wilson. 2022. "The Relationship between Cancer Caregiver Burden and Psychological Outcomes: The Moderating Role of Social Connectedness" Current Oncology 29, no. 1: 14-26. https://doi.org/10.3390/curroncol29010002
APA StyleYuen, E. Y. N., & Wilson, C. J. (2022). The Relationship between Cancer Caregiver Burden and Psychological Outcomes: The Moderating Role of Social Connectedness. Current Oncology, 29(1), 14-26. https://doi.org/10.3390/curroncol29010002





