Abstract
Introduction: We evaluated the association of pre-treatment immunologic biomarkers on the outcomes of early-stage non-small-cell lung cancer (NSCLC) patients treated with stereotactic body radiation therapy (SBRT). Materials and methods: In this retrospective study, all newly diagnosed early-stage NSCLC treated with SBRT between January 2010 and December 2017 were screened and included for further analysis. The pre-treatment neutrophil-lymphocyte ratio (NLR), monocyte lymphocyte ratio (MLR), and platelet-lymphocyte ratio (PLR) were calculated. Overall survival (OS) and recurrence-free survival (RFS) were estimated by Kaplan–Meier. Multivariable models were constructed to determine the impact of different biomarkers and the Akaike information criterion (AIC), index of adequacy, and scaled Brier scores were calculated. Results: A total of 72 patients were identified and 61 were included in final analysis. The median neutrophil count at baseline was 5.4 × 109/L (IQR: 4.17–7.05 × 109/L). Median lymphocyte count was 1.63 × 109/L (IQR: 1.29–2.10 × 109/L), median monocyte count was 0.65 × 109/L (IQR: 0.54–0.83 × 109/L), median platelet count was 260.0 × 109/L (IQR: 211.0–302.0 × 109/L). The median NLR was 3.42 (IQR: 2.38–5.04), median MLR was 0.39 (IQR: 0.31–0.53), and median PLR was 156.4 (IQR: 117.2–197.5). On multivariable regression a higher NLR was associated with worse OS (p = 0.01; HR-1.26; 95% CI 1.04–1.53). The delta AIC between the two multivariable models was 3.4, suggesting a moderate impact of NLR on OS. On multivariable analysis, higher NLR was associated with poor RFS (p = 0.001; NLR^1 HR 0.36; 0.17–0.78; NLR^2 HR-1.16; 95% CI 1.06–1.26) with a nonlinear relationship. The delta AIC between the two multivariable models was 16.2, suggesting a strong impact of NLR on RFS. In our cohort, MLR and PLR were not associated with RFS or OS in multivariable models. Conclusions: Our study suggests NLR, as a biomarker of systemic inflammation, is an independent prognostic factor for OS and RFS. The nonlinear relationship with RFS may indicate a suitable immunological environment is needed for optimal SBRT action and tumoricidal mechanisms. These findings require further validation in independent cohorts.
1. Introduction
Stereotactic body radiation therapy (SBRT) is an effective alternative treatment for patients with early-stage (stages IA, IB, or II) NSCLC who are medically inoperable or unwilling to undergo surgery, with cancer control and survival outcomes comparing favorably with those of surgical resection [1,2]. SBRT has been found to produce greater antitumor efficacy than would be predicted from standard radiological modelling alone, possibly through the superior engagement of the immune system, leading to enhanced antitumor immunity [3,4,5].
Markers of systemic inflammation—including circulating levels of neutrophils, monocytes, and lymphocytes—have been evaluated in the setting of different malignancies and have been found to predict response to therapy and disease outcomes. The neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and monocyte-lymphocyte ratio (MLR) are easily derived and inexpensive markers of systemic inflammation with prognostic value for survival in patients with various solid tumours [6,7,8,9,10].
Clinical outcomes after SBRT for early-stage NSCLC vary significantly between different studies: 3-year overall survival (OS) ranges from 37% to 72%, and recurrence rates vary from 18% to 29% rising the question about the selection of patients who will benefit from SBRT the most [11,12,13,14]. Utilizing prognostic factors—such as NLR, PLR, and MLR—obtained from complete blood count (CBC) could potentially inform decision-making in patients early-stage NSCLC considered for SBRT, given that it is readily obtained, minimally invasive and inexpensive. We, therefore, sought to determine whether pre-treatment immune biomarkers are predictive for cancer control and survival outcomes in patients with early-stage NSCLC managed with SBRT.
2. Materials and Methods
The local research ethics board approved this retrospective study. All newly diagnosed early-stage NSCLC (T1-2N0M0) patients treated with SBRT at CancerCare Manitoba between January 2010 and December 2017 were screened for inclusion and analysis. Patients with a previous history of malignancy apart from skin malignancy (excluding melanoma) were excluded from the study. Pre-treatment staging assessments included positron emission tomography (PET) and/or computed tomography (CT), chest-abdomen and cranial imaging (CT or MRI). Tissue diagnosis was preferred, and in cases where no tissue diagnosis was feasible, cases were discussed in local disease site group meetings for consensus on radiological diagnosis and treatment recommendations. In compliance with RTOG 0236 and RTOG 0815 trial protocols, tumours within 2 cm of the proximal bronchial tree were classified as central RTOG definition, and the rest were considered peripheral in location [2,15]. Peripheral lesions were treated with 48 Gy in 4 fractions, and central lesions were treated with a dose of 60 Gy in 8 fractions. Post-treatment patients were followed up with a CT scan of the chest at 3-, 6-, 12-, and 18-month post-treatment, and then every 12 months subsequently.
Patient-related characteristics were extracted manually from the electronic medical record including age, sex, Eastern Cooperative Oncology Group (ECOG) performance status score, forced expiratory volume in 1 s (FEV₁), diffusing capacity of carbone monoxide (DLCO), NLR pre-SBRT, PLR pre-SBRT, and MLR pre-SBRT. Tumour and treatment-related characteristics included T stage, maximum size (diameter), location, histology, and maximum standard uptake value (SUVmax) of positron emission tomography (PET), internal target volume (ITV) and planning target volume (PTV) and delivered doses. The overall survival (OS) interval was calculated from the date of radiation (first fraction of SBRT) to the date of death (any cause). Recurrence-free survival (RFS) was calculated from first fraction of SBRT to the time of radiological progression or last known follow-up date.
Cox hazard regression was used to assess the association of baseline variables with overall survival and recurrence-free survival. Univariable and multivariable analyses hazard regressions analysis were performed, including the following explanatory variables: NLR, PLR, MLR, ECOG performance status, ITV volume, age, and gender. Polynomial functions were used to account for any nonlinear relationships between predictors and outcomes. This was done because dichotomizing continuous predictors often reduces statistical power and variation between groups (e.g., individuals on either side of a cut point are seen as being very different) and does not indicate the possible nonlinear relationship [16,17]. Nonlinear relationships were presented using log (relative hazard) plots. To assess the impact of individual lymphocyte ratios, three metrics were computed: delta AIC, index of adequacy [18], and increase in integrated scaled Brier [18,19]. For this study, a delta AIC of 10 or more was considered to be a substantial improvement in model fit [20,21]. However, AIC values include sample size in their calculations. Therefore, delta AIC scores will increase in value for the same effect size as cohort size increases. The index of adequacy compares the likelihood ratio test of a model without the lymphocyte ratio to a model with the lymphocyte ratio. One minus the index adequacy indicates the fraction of new information provided by the lymphocyte ratio. The Brier score is the mean squared error and was scaled (1-(Brier/max Brier), where the max Brier is obtained from a Cox regression model without predictors. A scaled Brier score of 0 indicates a random association, and a value of 1 indicates perfect prediction. The proportional hazard assumption was tested using Schoenfeld residual plots. Kaplan–Meier survival plots of predicted values were produced with control variables held at their mean. Predictions were calculated for the 10th, 50th, and 90th percentile of each biomarker ratio.
3. Results
3.1. Patient Characteristics
In total, 72 ES-NSCLC patients were treated with SBRT from January 2010 to December 2017 at our institution, 10 of them were excluded from final analysis on account of missing CBC and one for missing ITV volume. Final cohort consisted of 61 patients included to final analysis. The median age of the cohort was 78 years with an interquartile range (IQR) of 72–82 years). Most of the patients were female (n = 41 (67.2%)), and 20 males (32.8%) were included. Eleven patients (18.0%) had an ECOG performance status 0, 37 patients (60.7%) had ECOG performance status 1–2, and in 13 patients (21.3%), ECOG performance status was unknown. Pretreatment histopathological diagnosis was available for 31 patients (50.8%), including 15 (24.6%) with adenocarcinoma, 10 (16.4%)–with squamous cell carcinoma, 5 (8.2%)–with NSCLC not otherwise specified, and one (1.6%) with biopsy positive for atypical cells not otherwise specified. Histopathology was unknown in 30 patients (49.2%).
The clinical tumour stage was T1a in 50 patients (82%), T1b in 10 patients (16.4%), and T2A in 1 patient (1.6%), respectively. The median tumour size was 2.1 cm with an IQR of 1.6–2.8 cm. The lesions were treated to a dose of 60Gy/8Fr in 9 patients (14.8%), 48Gy/4Fr in 50 patients (82%), and 60Gy/15Fr in two patients (3.3%). Eleven patients (18%) had central tumours. The median ITV and PTV volume were 11.2 and 35.6 cm³, respectively. In our cohort, 30 patients (49.1%) developed disease recurrence. The Median follow-up period was 2.14 years with the range of 0.1–5.6 years. Median OS duration was 3.0 years; 83.4% and 68.5% of patients were alive one year and two years after treatment, respectively. The main characteristics of the patients are illustrated in Table 1.

Table 1.
Patient demographic and characteristics.
The baseline median neutrophil count at baseline was 5.40 × 10⁹/L (IQR: 4.17–7.05 × 10⁹/L), median lymphocyte count was 1.63 × 10⁹/L (IQR: 1.29–2.10 × 10⁹/L), median monocytes count was 0.65 × 10⁹/L (IQR: 0.54–0.83 × 10⁹/L) and median platelet count was 260.0 × 10⁹/L (IQR: 211.0–302.0 × 10⁹/L). Details are illustrated in Figure 1. Median NLR was 3.42 (IQR: 2.38–5.04), median MLR was 0.9 (IQR: 0.31–0.53), and median PLR was 156.4 (IQR: 117.2–197.5) respectively.
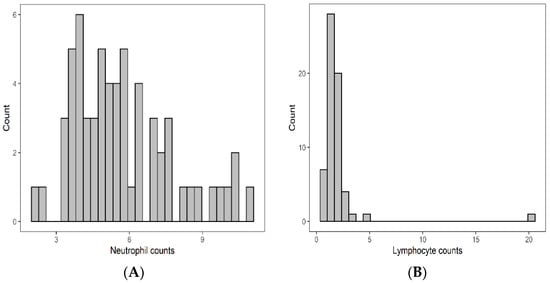
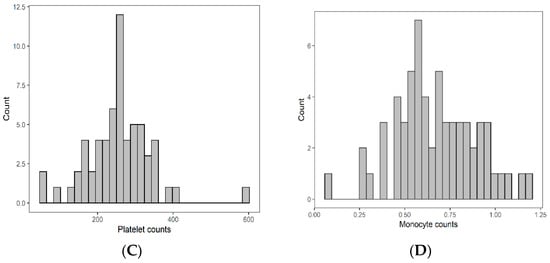
Figure 1.
Pretreatment distribution of neutrophils (A), lymphcytes (B), monocytes (C), and platelet (D).
3.2. Survival Analysis
Univariable and multivariable analyses were performed for NLR, PLR, MLR, ECOG, ITV volume, age, and gender. On univariate analysis, higher NLR was associated with worse OS (p = 0.009; HR-1.27; 95% CI 1.06–1.53) and this relationship was linear (Figure 2). There was no association between PLR and OS (p = 0.833; HR-1.05; 95% CI 0.69–1.59). Similarly, MLR did not affect OS (p = 0.833; HR-2.92; 95% CI 0.62–13.78). Multivariable hazard regression models for overall survival including ECOG and ITV volume showed that higher NLR was associated with decreased OS (p = 0.017; HR-1.26; 95% CI 1.04–1.53), and the delta AIC between the two multivariable models was 3.4, suggesting a moderate impact on OS by NLR. The 1-index of adequacy was 0.52 and scaled integrated brier of 0.11. There was no association between MLR (p = 0.227; HR-2.80; 95% CI 0.53–14.86) and PLR (p = 0.930; HR-1.02; 95% CI 0.57–5.08) and OS; the delta AIC was less than 2, suggesting weak or no impact. Overall survival curves were calculated for 10th, 50th, and 90th percentile of NLR, MLR, and PLR are shown in figure (Figure 3), and demonstrates the larger impact of NLR on OS compared to MLR and PLR through the larger differences in OS estimates. The larger impact of NLR relative to MLR and PLR is also demonstrated with higher 1 minus index of adequacy values and scaled Brier increases (Table 2).
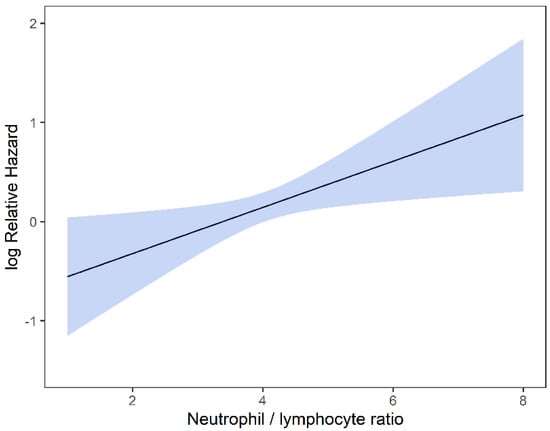
Figure 2.
Risk of death by NLR.
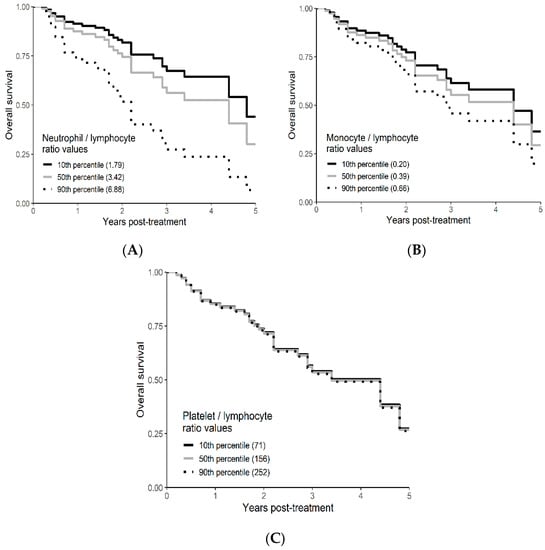
Figure 3.
Kaplan–Meier curves for OS by NLR (A), MLR (B), and PLR (C) using predicted values at the 10th, 50th, and 90th percentile of predictors.

Table 2.
Regression model for OS.
3.3. Recurrence Free Survival Analysis
On univariable analysis, higher NLR was associated with poor RFS (p = 0.01; NLR^1 HR-0.55; 95% CI 0.28–1.09; NLR^2 HR-1.8; 95% CI 1.01–1.17). The relationship between NLR and RFS was nonlinear, and a polynomial function was used (Figure 4). The best RFS was associated with NLR between 3.5–4.0 and the worst was above values 6. There was no statistically significant association between both MLR and PLR and RFS in univariate analysis (p = 0.340; HR-1.96; 95% CI 0.49–7.78 and p = 0.494; HR-1.13; 95% CI 0.80–1.60 respectively). On multivariable analysis, higher NLR was also associated with poor RFS (p = 0.001; NLR^1 HR-0.36; 95% CI 0.17–0.78; NLR^2 HR-1.16; 95% CI 1.06–1.26), and the delta AIC between two models was 16.20, implying a strong impact of NLR on RFS. The 1-index of adequacy was 0.7 and scaled integrated brier of 0.19. In our cohort MLR and PLR were not associated with RFS in multivariable models (p = 0.252; HR-2.35; 95% CI 0.54–10.43 and p = 0.241; HR-1.28; 95% CI0.85–1.92). For MLR and PLR, the delta AIC was less than 2, suggesting weak or no impact. Relapse-free survival curves were calculated based on the 10th, 50th, and 90th percentile of NLR, MLR, and PLR are shown in figure (Figure 5), which demonstrates the larger impact of NLR on RFS than MLR and PLR through larger differences in RFS estimates. The larger impact of NLR relative to MLR and PLR is also demonstrated with higher 1 minus index of adequacy values and scaled Brier increases (Table 3).
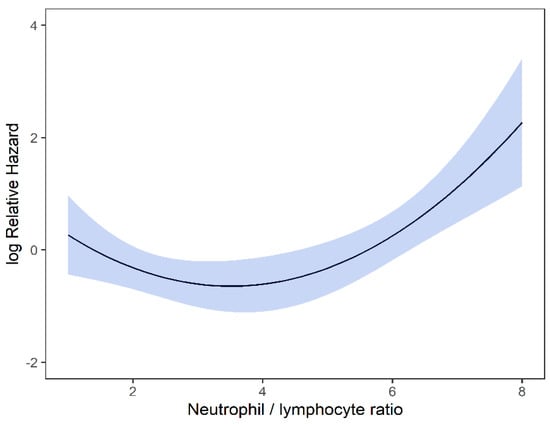
Figure 4.
Risk of RFS by NLR.
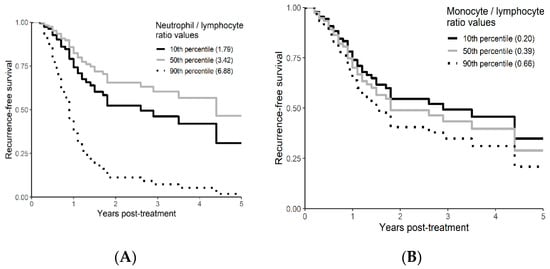
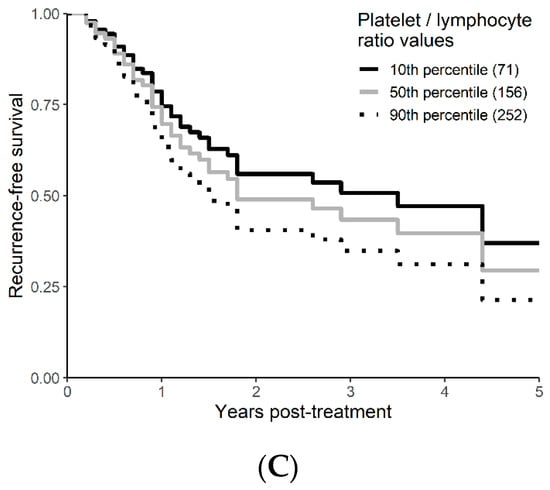
Figure 5.
Kaplan–Meier curves for RFS by NLR (A), MLR (B), and PLR (C) using predicted values at the 10th, 50th, and 90th percentile of predictors.

Table 3.
Regression model for RFS.
3.4. Local Recurrence Free Survival Analysis
On univariable analysis higher NLR was associated with poor RFS (p = 0.01; NLR^1 HR-0.73; 95% CI 0.44–1.21; NLR^2 HR-1.05; 95% CI 1–1.1). The relationship between NLR and LRFS was nonlinear, and a polynomial function was used (Figure 6). The best LRFS was associated with NLR between 2.0–4.0 and the worst was above values 6. There was no statistically significant association between both MLR and PLR and LRFS in univariate analysis (p = 0.18; HR-2.71; 95% CI 0.63–11.69 and p = 0.958; HR-1.01; 95% CI 0.68–1.50 respectively). On multivariable analysis, higher NLR was also associated with poor LRFS (p = 0.021; NLR^1 HR-0.74; 95% CI 0.44–1.23; NLR^2 HR-1.05; 95% CI 1–1.1), and the delta AIC between two models was 4.09, implying a moderate impact of NLR on RFS. The 1-index of adequacy was 0.61 and scaled integrated brier of 0.14. In our cohort, MLR and PLR were not associated with LRFS in multivariable models (p = 0.212; HR-2.72; 95% CI 0.56–13.14 and p = 0.935; HR-0.98; 95% CI 0.66–1.47). For MLR and PLR, the delta AIC was less than 2, suggesting weak or no impact. LRFS survival curves were calculated based on the 10th, 50th, and 90th percentile of NLR, MLR, and PLR are shown in figure (Figure 7), which demonstrates the larger impact of NLR on LRFS than MLR and PLR through larger differences in LRFS estimates. The larger impact of NLR relative to MLR and PLR is also demonstrated with higher 1 minus index of adequacy values and scaled Brier increases (Table 4).
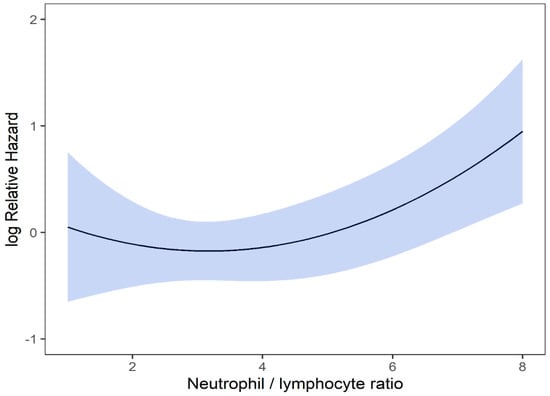
Figure 6.
Risk of LRFS by NLR.
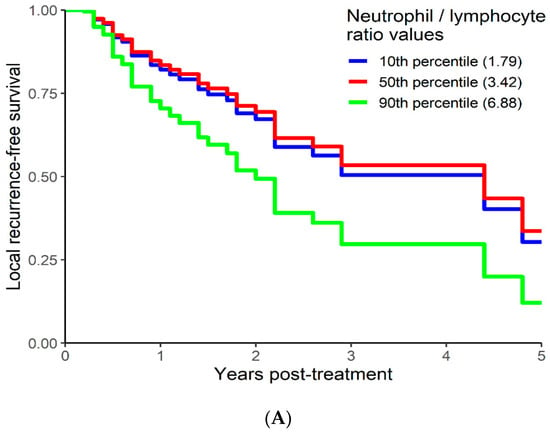
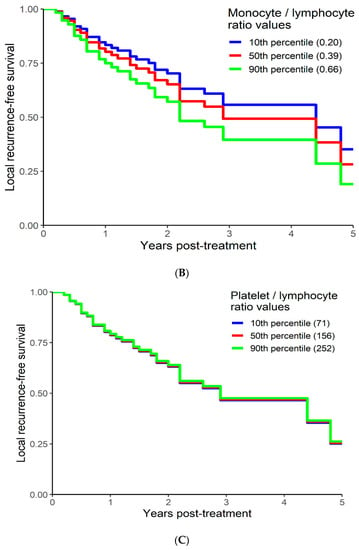
Figure 7.
Kaplan–Meier curves for LRFS by NLR (A), MLR (B), and PLR (C) using predicted values at the 10th, 50th, and 90th percentile of predictors.

Table 4.
Regression model for LRFS.
4. Discussion
Accumulated evidence shows plausible link between inflammation, particularly systemic inflammation, and cancer development and progression [7,8,9,10]. Systemic inflammation is known to promote tumour development and angiogenesis and inhibit apoptosis and has been reported to increase the risk of various cancers, such as liver, colorectal, breast, and lung cancer [7,8,9,10]. Neutrophil, platelet, lymphocyte, monocytes, and the ratios thereof could serve as a measure of inflammatory response and provide prognostic value in oncology [22].
The influence of surrogate markers for systemic inflammation on patient outcomes has been previously assessed and showed mixed findings [23,24,25]. Cannon et al. demonstrated that increased NLR and PLR were associated with poor overall survival with cutoffs of 2.98 and 146, respectively (p = 0.005 for NLR and p = 0.003 for PLR). However, when NLR and PLR were analyzed as continuous variables, they were not significantly associated with OS. Similarly, when NLR and PLR were analyzed as continuous variables, no significant association was found between nonlocal treatment failure and NLR (p = 0.937) and PLR (p = 0.133). Furthermore, no significant cutoff point was observed for NLR (AUC = 0.635; p = 0.15), but a PLR cutoff of 250 was found to maximize sensitivity and specificity (AUC = 0.720; p = 0.02) for nonlocal failure [23]. In a separate cohort, Shaverdian et al. found that higher pretreatment NLR and PLR independently predicted worse OS in early-stage NSCLC patients treated with SBRT on both univariate (p = 0.0003 and p < 0.0001 respectively) and multivariate analysis (HR-1.39; p = 0.0088 and HR-1.07; p = 0.024). The optimal NLR and PLR cutoffs in this study were 2.18 and 187.27, respectively. However, there was no correlation between NLR and PLR and locoregional (p = 0.81 and p = 0.25 respectively) or distant (p = 0.62 and p = 0.91 respectively) treatment failure [24]. Giuliani et al. demonstrated independent correlation between NLR (P < 0.01) and OS in early-stage NSCLC patients treated with SABR. Median OS was 4.3 years (95% CI 3.5 years to not reached) in patients with an NLR equal to or below the median (≤3, “low NLR”) and 2.5 years (95% CI 1.7 to 4.8 years) with NLR above the median (>3, “high NLR”). The correlation between MLR (P < 0.01) and disease-related failure was also found in this study [25]. The recent report with 389 patients showed although NLR was associated with OS, it was associated with non-lung cancer-specific survival and not lung cancer-specific survival [26].
In our study, multivariable models including ECOG and ITV volume showed that higher NLR was associated with decreased OS (p = 0.017; HR-1.26; 95% CI 1.04–1.53), and the delta AIC between the two multivariable models was 3.4, suggesting a moderate impact on OS. Our findings suggest an association between NLR with OS, and these would corroborate findings from previous reports [23,24,25]. We found that the higher pretreatment NLR values independently predicted poor OS.
In multivariable analysis, higher NLR was also associated with poor RFS (p = 0.001; NLR^1 HR-0.36; 95% CI 0.17–0.78; NLR^2 HR-1.16; 95% CI 1.06–1.26), and the delta AIC between two models was 16.20, implying a strong impact on RFS. In our cohort, MLR and PLR were not associated with RFS in multivariable models (p = 0.252; HR-2.35; 95% CI 0.54–10.43 and p = 0.241; HR-1.28; 95% CI0.85–1.92). On multivariable analysis, higher NLR was also associated with poor LRFS (p = 0.021; NLR^1 HR-0.74; 95% CI 0.44–1.23; NLR^2 HR-1.05; 95% CI 1–1.1), and the delta AIC between two models was 4.09, implying a moderate impact of NLR on RFS. The 1-index of adequacy was 0.61 and scaled integrated brier of 0.14. In our cohort MLR and PLR were not associated with LRFS in multivariable models (p = 0.212; HR-2.72; 95% CI 0.56–13.14 and p = 0.935; HR-0.98; 95% CI 0.66–1.47). In contrast to previous reports, our data suggest an NLR correlated with RFS and LRFS [23,24]. The previous studies reported cutoff values, and this may have decreased the sensitivity to detect relationship.
We did not use cutoff values for NLR, and our data demonstrated that, unlike for OS, the relationship of NLR with RFS and LRFS was nonlinear, with the risk of relapse increased when NLR values fell outside the optimal range. In our group of patients with early-stage NSCLC treated with SBRT had a lower RFS with NLR values between 3.5 and 4.5. Similarly, we found lower LRFS with NLR values between 2 and 4. To the best of our knowledge, this is the first study reporting the nonlinear relationship between NLR-RFS and NLR-LRFS. The nonlinear relationship may indicate an optimal immunological environment is needed for optimal SBRT action and tumoricidal mechanisms.
The conventional fractionated radiation therapy revolves around classical “4 Rs” including: repair, reassortment, reoxygenation, and repopulation. However, the radiobiology of SBRT is not fully explained by the 4Rs and resultant DNA damage, and additional mechanisms of vascular damage and antitumor immune response are also implicated [27]. Several reports suggest elevated immunomodulatory expression is associated with SBRT [27,28,29]. Understanding the role of systemic inflammation and its implications in SBRT is critical and of prognostic value. Thus, the utility and prognostic performance of systemic inflammation in stage I NSCLC undergoing SBRT are particularly interesting as the treatment mechanism.
Limitations: our study has several limitations and represents experience at our center, and a small number of patients of which (50.8%) had histopathological confirmation of the diagnosis. In addition, CBC draws from patients in this study were up to 3 months prior to initiation of SBRT, unlike other studies in surgical and chemotherapy series where CBC was done within 1 week to 1 month before treatment. It is unclear if the wider lead-time of CBC testing in our study had any material impact on the study results. Furthermore, the impact of baseline comorbidity (Charleson Comorbidity Index or other similar comorbidity indices) and immunomodulatory or anti-inflammatory medications could not be evaluated, and confounding could not be excluded. Therefore, our findings should be interpreted with caution and need confirmation in larger prospective studies.
5. Conclusions
Our study suggests NLR, as a marker of systemic inflammation, is an independent prognostic factor for worse OS, RFS, and LRFS. The nonlinear relationship with RFS and LRFS may indicate an optimal immunological environment is needed for optimal SBRT action and tumoricidal mechanisms. These findings require further validation in independent cohorts.
Author Contributions
Conceptualization, M.A., B.B., A.C., R.K., S.R.; methodology, M.A., P.L., O.B., S.R.; data curation, M.A. and S.D.; formal analysis, P.L. and O.B.; writing—original draft preparation, M.A. and S.R.; writing—review and editing, M.A., S.D., B.B., A.C., N.A., A.L., J.K., P.L., O.B., W.H., G.S., R.K., and S.R.; supervision, S.R.; project administration, S.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board—Health research ethics board of University of Manitoba and CancerCare Manitoba’s Research and Resource Impact Committee [protocol code HS21629 (H2018:109) and date of approval 28 May 2018].
Informed Consent Statement
Patient consent was waived in view of retrospective nature of study.
Data Availability Statement
The data presented in this study could be shared in deidentified format on specific request, as per local institutional policy. Such request should be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Chang, J.Y.; Senan, S.; Paul, M.A.; Mehran, R.J.; Louie, A.V.; Balter, P.; Groen, H.J.M.; E McRae, S.E.; Widder, J.; Feng, L.; et al. Stereotactic ablative radiotherapy versus lobectomy for operable stage I non-small-cell lung cancer: A pooled analysis of two randomised trials. Lancet Oncol. 2015, 16, 630–637. [Google Scholar] [CrossRef]
- Timmerman, R.; Paulus, R.; Galvin, J.; Michalski, J.; Straube, W.; Bradley, J.; Fakiris, A.; Bezjak, A.; Videtic, G.; Johnstone, D.; et al. Stereotactic body radiation therapy for inoperable early stage lung cancer. JAMA 2010, 303, 1070–1076. [Google Scholar] [CrossRef]
- Brown, J.M.; Carlson, D.J.; Brenner, D.J. The Tumor radiobiology of SRS and SBRT: Are more than the 5 Rs involved? Int. J. Radiat. Oncol. 2014, 88, 254–262. [Google Scholar] [CrossRef]
- Reese, A.S.; Feigenberg, S.J.; Husain, A.; Webb, T.; Hausner, P.F.; Edelman, M.; Feliciano, J.; Tkaczuk, K.H.; Sharma, N.K. Stereotactic Ablative Radiotherapy (SABR): Impact on the immune system and potential for future therapeutic modulation. Mol. Cell. Pharmacol. 2013, 5, 19–25. [Google Scholar]
- Song, C.W.; Kim, M.-S.; Cho, L.C.; Dusenbery, K.; Sperduto, P.W. Radiobiological basis of SBRT and SRS. Int. J. Clin. Oncol. 2014, 19, 570–578. [Google Scholar] [CrossRef]
- Gu, X.; Sun, S.; Gao, X.-S.; Xiong, W.; Qin, S.; Qi, X.; Ma, M.; Li, X.; Zhou, D.; Wang, W.; et al. Prognostic value of platelet to lymphocyte ratio in non-small cell lung cancer: Evidence from 3430 patients. Sci. Rep. 2016, 6, 23893. [Google Scholar] [CrossRef]
- Asher, V.; Lee, J.; Innamaa, A.; Bali, A. Preoperative platelet lymphocyte ratio as an independent prognostic marker in ovarian cancer. Clin. Trans. Oncol. 2011, 13, 499–503. [Google Scholar] [CrossRef]
- Huang, S.H.; Waldron, J.; Milosevic, M.; Shen, X.; Ringash, J.; Su, J.; Tong, L.; Perez-Ordonez, B.; Weinreb, I.; Bayley, A.J.; et al. Prognostic value of pretreatment circulating neutrophils, monocytes, and lymphocytes in oropharyngeal cancer stratified by human papillomavirus status. Cancer 2014, 121, 545–555. [Google Scholar] [CrossRef]
- Kwon, H.-C.; Kim, S.H.; Oh, S.Y.; Lee, S.; Lee, J.H.; Choi, H.-J.; Park, K.-J.; Roh, M.S.; Kim, S.-G.; Kim, H.-J.; et al. Clinical significance of preoperative neutrophil-lymphocyte versus platelet-lymphocyte ratio in patients with operable colorectal cancer. Biomarkers 2012, 17, 216–222. [Google Scholar] [CrossRef]
- Zhou, X.; Du, Y.; Huang, Z.; Xu, J.; Qiu, T.; Wang, J.; Wang, T.; Zhu, W.; Liu, P. Prognostic value of plr in various cancers: A meta-analysis. PLoS ONE 2014, 9, e101119. [Google Scholar] [CrossRef]
- Senthi, S.; Lagerwaard, F.J.; Haasbeek, C.J.; Slotman, B.; Senan, S. Patterns of disease recurrence after stereotactic ablative radiotherapy for early stage non-small-cell lung cancer: A retrospective analysis. Lancet Oncol. 2012, 13, 802–809. [Google Scholar] [CrossRef]
- van den Berg, L.L.; Klinkenberg, T.J.; Groen, H.J.M.; Widder, J. Patterns of recurrence and survival after surgery or stereotactic radiotherapy for early stage NSCLC. J. Thorac. Oncol. 2015, 10, 826–831. [Google Scholar] [CrossRef]
- Brooks, E.D.; Sun, B.; Feng, L.; Verma, V.; Zhao, L.; Gomez, D.R.; Liao, Z.; Jeter, M.; O’Reilly, M.; Welsh, J.W.; et al. Association of long-term outcomes and survival with multidisciplinary salvage treatment for local and regional recurrence after stereotactic ablative radiotherapy for early-stage lung cancer. JAMA Netw. Open 2018, 1, e181390. [Google Scholar] [CrossRef]
- Figlia, V.; Mazzola, R.; Cuccia, F.; Alongi, F.; Mortellaro, G.; Cespuglio, D.; Cucchiara, T.; Iacoviello, G.; Valenti, V.; Molino, M.; et al. Hypo-fractionated stereotactic radiation therapy for lung malignancies by means of helical tomotherapy: Report of feasibility by a single-center experience. La Radiol. Med. 2018, 123, 406–414. [Google Scholar] [CrossRef]
- Bezjak, A.; Paulus, R.; Gaspar, L.E.; Timmerman, R.D.; Straube, W.L.; Ryan, W.F.; Garces, Y.I.; Pu, A.T.; Singh, A.K.; Videtic, G.M.; et al. Safety and efficacy of a five-fraction stereotactic body radiotherapy schedule for centrally located non–small-cell lung cancer: NRG oncology/RTOG 0813 trial. J. Clin. Oncol. 2019, 37, 1316–1325. [Google Scholar] [CrossRef]
- Royston, P.; Altman, D.G.; Sauerbrei, W. Dichotomizing continuous predictors in multiple regression: A bad idea. Stat. Med. 2006, 25, 127–141. [Google Scholar] [CrossRef]
- Altman, D.G.; Royston, P. The cost of dichotomising continuous variables. BMJ 2006, 332, 1080. [Google Scholar] [CrossRef]
- Califf, R.M.; Phillips, H.R., III; Hindman, M.C.; Mark, B.D.; Lee, K.L.; Behar, V.S.; Johnson, R.A.; Pryor, D.B.; Rosati, R.A.; Wagner, G.S.; et al. Prognostic value of a coronary artery jeopardy score. J. Am. Coll. Cardiol. 1985, 5, 1055–1063. [Google Scholar] [CrossRef]
- Gerds, T.A.; Cai, T.; Schumacher, M. The performance of risk prediction models. Biom. J. 2008, 50, 457–479. [Google Scholar] [CrossRef]
- Burnham, K.P.; Anderson, D.R. Model Selection and Multimodel Inference: A Practical Information-Theoretic Approach, 2nd ed.; Springer: New York, NY, USA, 2002. [Google Scholar]
- Hall, C.A. Logistic Regression Models; CRC Press: Boca Raton, FL, USA, 2009. [Google Scholar]
- Roxburgh, C.S.D.; McMillan, D.C. Cancer and systemic inflammation: Treat the tumour and treat the host. Br. J. Cancer 2014, 110, 1409–1412. [Google Scholar] [CrossRef]
- Cannon, N.A.; Meyer, J.; Iyengar, P.; Ahn, C.; Westover, K.; Choy, H.; Timmerman, R. Neutrophil–lymphocyte and platelet–lymphocyte ratios as prognostic factors after stereotactic radiation therapy for early-stage non–small-cell lung cancer. J. Thorac. Oncol. 2015, 10, 280–285. [Google Scholar] [CrossRef]
- Shaverdian, N.; Veruttipong, D.; Wang, J.; Schaue, D.; Kupelian, P.; Lee, P. Pretreatment immune parameters predict for overall survival and toxicity in early-stage non–small-cell lung cancer patients treated with stereotactic body radiation therapy. Clin. Lung Cancer 2016, 17, 39–46. [Google Scholar] [CrossRef]
- Giuliani, M.; Sampson, L.; Wong, O.; Gay, J.; Le, L.; Cho, B.; Brade, A.; Sun, A.; Bezjak, A.; Hope, A. Prognostic value of pretreatment circulating neutrophils, monocytes, and lymphocytes on outcomes in lung stereotactic body radiotherapy. Curr. Oncol. 2016, 23, 362–368. [Google Scholar] [CrossRef][Green Version]
- Kotha, N.V.; Cherry, D.R.; Bryant, A.K.; Nalawade, V.; Stewart, T.F.; Rose, B.S. Prognostic utility of pretreatment neutrophil-lymphocyte ratio in survival outcomes in localized non-small cell lung cancer patients treated with stereotactic body radiotherapy: Selection of an ideal clinical cutoff point. Clin. Transl. Radiat. Oncol. 2021, 28, 133–140. [Google Scholar] [CrossRef]
- Song, C.W.; Glatstein, E.; Marks, L.B.; Emami, B.; Grimm, J.; Sperduto, P.W.; Kim, M.-S.; Hui, S.; Dusenbery, K.E.; Cho, L.C. Biological principles of Stereotactic Body Radiation Therapy (SBRT) and Stereotactic Radiation Surgery (SRS): Indirect cell death. Int. J. Radiat. Oncol. 2021, 110, 21–34. [Google Scholar] [CrossRef]
- Finkelstein, S.E.; Timmerman, R.; McBride, W.H.; Schaue, D.; Hoffe, S.E.; Mantz, C.A.; Wilson, G. The confluence of stereotactic ablative radiotherapy and tumor immunology. Clin. Dev. Immunol. 2011, 2011, 439752. [Google Scholar] [CrossRef]
- Matsumura, S.; Wang, B.; Kawashima, N.; Braunstein, S.; Badura, M.; Cameron, T.O.; Babb, J.; Schneider, R.; Formenti, S.C.; Dustin, M.; et al. Radiation-induced CXCL16 release by breast cancer cells attracts effector T cells. J. Immunol. 2008, 181, 3099–3107. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).