Pegylated Liposomal Doxorubicin (Caelyx®) as Adjuvant Treatment in Early-Stage Luminal B-like Breast Cancer: A Feasibility Phase II Trial
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Patients
2.3. Treatment
2.4. Primary and Secondary Endpoints
2.5. Follow-Up
2.6. Statistical Analysis
3. Results
3.1. Patients and Tumors’ Characteristics
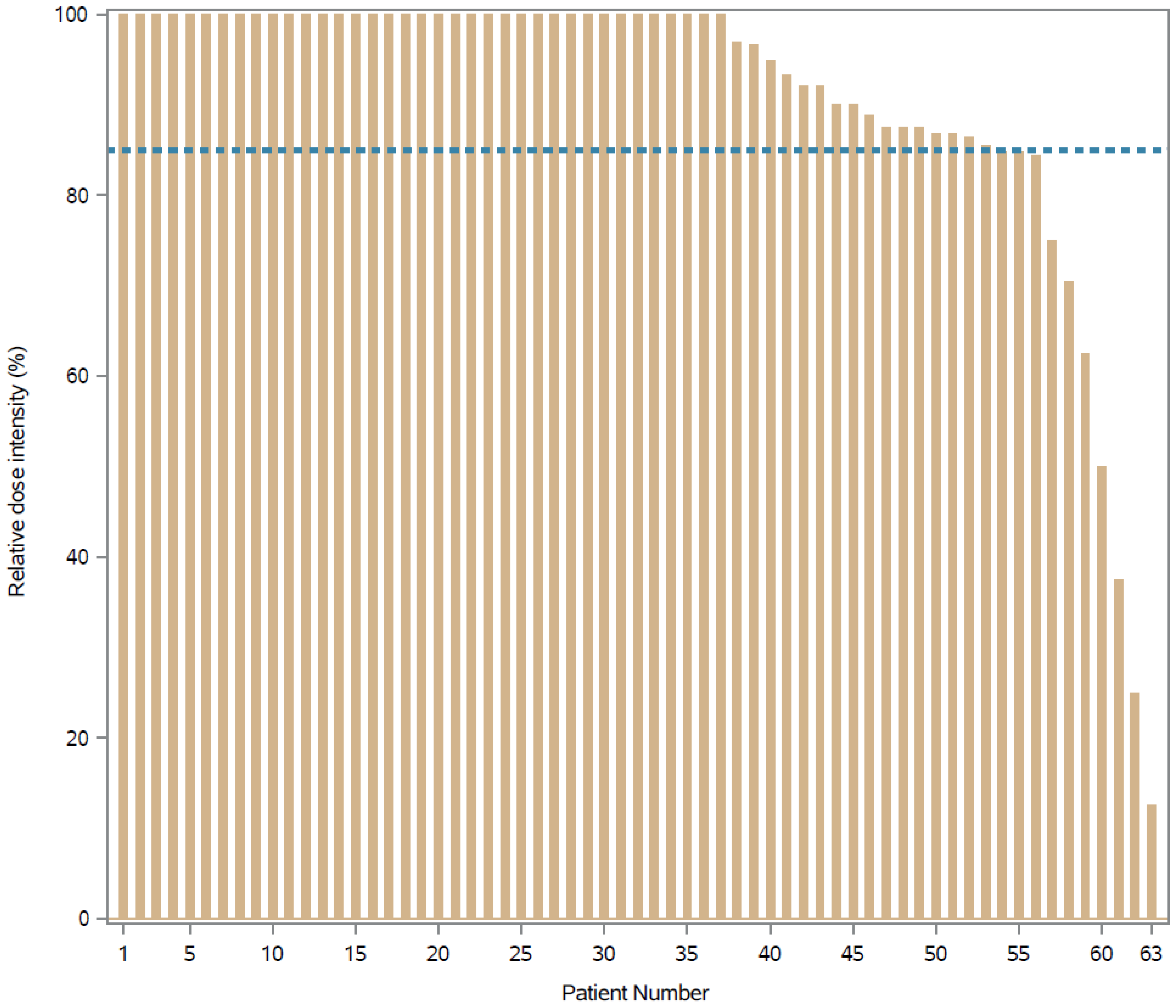
3.2. Relative Dose Intensity
3.3. Adverse Events
3.4. Tolerability
3.5. Survival
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Burstein, H.; Curigliano, G.; Thürlimann, B.; Weber, W.; Poortmans, P.; Regan, M.; Senn, H.; Winer, E.; Gnant, M.; Aebi, S.; et al. Customizing local and systemic therapies for women with early breast cancer: The St. Gallen International Consensus Guidelines for treatment of early breast cancer 2021. Ann. Oncol. 2021, 32, 1216–1235. [Google Scholar] [CrossRef]
- Yan, X.J.; Xu, J.; Gu, Z.H.; Pan, C.M.; Lu, G.; Shen, Y.; Shi, J.Y.; Zhu, Y.M.; Tang, L.; Zhang, X.W.; et al. Breast cancer classification and prognosis based on gene expression profiles from a popula-tion-based study. Proc. Natl. Acad. Sci. USA 2003, 100, 10393–10398. [Google Scholar] [CrossRef] [Green Version]
- Goldhirsch, A.; Wood, W.C.; Coates, A.S.; Gelber, R.D.; Thürlimann, B.; Senn, H.-J. Strategies for subtypes—dealing with the diversity of breast cancer: Highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann. Oncol. 2011, 22, 1736–1747. [Google Scholar] [CrossRef]
- Goldhirsch, A.; Winer, E.P.; Coates, A.S.; Gelber, R.D.; Piccart-Gebhart, M.; Thürlimann, B.; Senn, H.J.; Albain, K.S.; André, F.; Bergh, J.; et al. Personalizing the treatment of women with early breast cancer: Highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2013. Ann Oncol. 2013, 24, 2206–2223. [Google Scholar] [CrossRef]
- Cardoso, F.; Kyriakides, S.; Ohno, S.; Penault-Llorca, F.; Poortmans, P.; Rubio, I.T.; Zackrisson, S.; Senkus, E. Early breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2019, 30, 1194–1220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Franco, Y.L.; Vaidya, T.R.; Ait-Oudhia, S. Anticancer and cardio-protective effects of liposomal doxorubicin in the treatment of breast cancer. Breast Cancer Targets Ther. 2018, 10, 131–141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hamilton, A.; Biganzoli, L.; Coleman, R.; Mauriac, L.; Hennebert, P.; Awada, A.; Nooij, M.; Beex, L.; Piccart, M.; Van Hoorebeeck, I.; et al. EORTC 10968: A phase I clinical and pharmacokinetic study of polyethylene glycol liposomal doxorubicin (Caelyx®, Doxil®) at a 6-week interval in patients with metastatic breast cancer. Ann. Oncol. 2002, 13, 910–918. [Google Scholar] [CrossRef]
- Fraguas-Sánchez, A.; Martín-Sabroso, C.; Fernández-Carballido, A.; Torres-Suárez, A.I. Current status of nanomedicine in the chemotherapy of breast cancer. Cancer Chemother. Pharmacol. 2019, 84, 689–706. [Google Scholar] [CrossRef] [PubMed]
- Ranson, M.R.; Carmichael, J.; O’Byrne, K.; Stewart, S.; Smith, D.; Howell, A. Treatment of advanced breast cancer with sterically stabilized liposomal doxorubicin: Results of a multicenter phase II trial. J. Clin. Oncol. 1997, 15, 3185–3191. [Google Scholar] [CrossRef]
- Lyass, O.; Uziely, B.; Ben-Yosef, R.; Tzemach, D.; Heshing, N.I.; Lotem, M.; Brufman, G.; Gabizon, A. Correlation of toxicity with pharmacokinetics of pegylated liposomal doxorubicin (Doxil) in metastatic breast carcinoma. Cancer 2000, 89, 1037–1047. [Google Scholar] [CrossRef]
- Munzone, E.; Di Pietro, A.; Goldhirsch, A.; Minchella, I.; Verri, E.; Rocca, M.C.; Marenghi, C.; Curigliano, G.; Radice, D.; Adamoli, L.; et al. Metronomic administration of pegylated liposomal-doxorubicin in extensively pre-treated metastatic breast cancer patients: A mono-institutional case-series report. Breast 2010, 19, 33–37. [Google Scholar] [CrossRef]
- O’Brien, M.E.R.; Wigler, N.; Inbar, M.; Rosso, R.; Grischke, E.; Santoro, A.; Catane, R.; Kieback, D.G.; Tomczak, P.; Ackland, S.P.; et al. Reduced cardiotoxicity and comparable efficacy in a phase IIItrial of pegylated liposomal doxorubicin HCl(CAELYX™/Doxil®) versus conventional doxorubicin forfirst-line treatment of metastatic breast cancer. Ann. Oncol. 2004, 15, 440–449. [Google Scholar] [CrossRef]
- Yao, J.; Pan, S.; Fan, X.; Jiang, X.; Yang, Y.; Jin, J.; Liu, Y. Pegylated liposomal doxorubicin as neoadjuvant therapy for stage II–III locally advanced breast cancer. J. Chemother. 2020, 32, 202–207. [Google Scholar] [CrossRef]
- Hung, C.-C.; Yang, Y.; Tsai, I.-C.; Hsu, C.-Y.; Liu, C.-H.; Yang, J.-R. The Efficacy of Pegylated Liposomal Doxorubicin-Based Neoadjuvant Chemotherapy in Breast Cancer: A Retrospective Case-Control Study in Taiwan. Biochem. Res. Int. 2020, 2020, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Gogas, H.; Papadimitriou, C.; Kalofonos, H.; Bafaloukos, D.; Fountzilas, G.; Tsavdaridis, D.; Anagnostopoulos, A.; Onyenadum, A.; Papakostas, P.; Economopoulos, T.; et al. Neoadjuvant chemotherapy with a combination of pegylated liposomal doxorubicin (Caelyx®) and paclitaxel in locally advanced breast cancer: A phase II study by the Hellenic Cooperative Oncology Group. Ann. Oncol. 2002, 13, 1737–1742. [Google Scholar] [CrossRef] [PubMed]
- Rossi, D.; Baldelli, A.M.; Casadei, V.; Fedeli, S.L.; Alessandroni, P.; Catalano, V.; Giordani, P.; Ceccolini, M.; Graziano, F.; Catalano, G. Neoadjuvant chemotherapy with low dose of pegylated liposomal doxorubicin plus weekly paclitaxel in operable and locally advanced breast cancer. Anti-Cancer Drugs 2008, 19, 733–737. [Google Scholar] [CrossRef] [PubMed]
- Artioli, G.; Grazia, A.; Mocellin, S.; Simone, M.; Borgato, L.; Lucia, B.; Cappetta, A.; Alessandro, C.; Bozza, F.; Fernando, B.; et al. Phase II study of neoadjuvant gemcitabine, pegylated liposomal doxorubicin, and docetaxel in locally advanced breast cancer. Anticancer. Res. 2010, 30, 3817–3821. [Google Scholar]
- Torrisi, R.; Montagna, E.; Scarano, E.; Dellapasqua, S.; Cancello, G.; Iorfida, M.; Luini, A.; Veronesi, P.; Viale, G.; Goldhirsch, A.; et al. Neoadjuvant pegylated liposomal doxorubicin in combination with cisplatin and infusional fluoruracil (CCF) with and without endocrine therapy in locally advanced primary or recurrent breast cancer. Breast 2011, 20, 34–38. [Google Scholar] [CrossRef]
- Wang, L.; Hong, Y.; Ma, J.; Han, M.; Zhang, S.; Shan, B.; Liu, Y. Combination of pegylated liposomal doxorubicin and docetaxel as neoadjuvant therapy for breast cancer with axillary lymph node metastasis. J. Int. Med Res. 2020, 48. [Google Scholar] [CrossRef]
- Dellapasqua, S.; Mazza, M.; Rosa, D.; Ghisini, R.; Scarano, E.; Torrisi, R.; Maisonneuve, P.; Viale, G.; Cassano, E.; Veronesi, P.; et al. Pegylated liposomal doxorubicin in combination with low-dose metronomic cyclophosphamide as preoperative treatment for patients with locally advanced breast cancer. Breast 2011, 20, 319–323. [Google Scholar] [CrossRef]
- Tuxen, M.K.; Cold, S.; Tange, U.B.; Balslev, E.; Nielsen, D.L. Phase II study of neoadjuvant pegylated liposomal doxorubicin and cyclophosphamide ± trastuzumab followed by docetaxel in locally advanced breast cancer. Acta Oncol. 2014, 53, 1440–1445. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singal, P.K.; Iliskovic, N. Doxorubicin-Induced Cardiomyopathy. N. Engl. J. Med. 1998, 339, 900–905. [Google Scholar] [CrossRef] [PubMed]
- Zambetti, M.; Moliterni, A.; Materazzo, C.; Stefanelli, M.; Cipriani, S.; Valagussa, P.; Bonadonna, G.; Gianni, L. Long-Term Cardiac Sequelae in Operable Breast Cancer Patients Given Adjuvant Chemotherapy with or Without Doxorubicin and Breast Irradiation. J. Clin. Oncol. 2001, 19, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Praga, C.; Bergh, J.; Bliss, J.; Bonneterre, J.; Cesana, B.; Coombes, R.C.; Fargeot, P.; Folin, A.; Fumoleau, P.; Giuliani, R.; et al. Risk of Acute Myeloid Leukemia and Myelodysplastic Syndrome in Trials of Adjuvant Epirubicin for Early Breast Cancer: Correlation with Doses of Epirubicin and Cyclophosphamide. J. Clin. Oncol. 2005, 23, 4179–4191. [Google Scholar] [CrossRef]
- Puts, M.T.E.; Monette, J.; Girre, V.; Wolfson, C.; Monette, M.; Batist, G.; Bergman, H. Characteristics of older newly diagnosed cancer patients refusing cancer treatments. Support. Care Cancer 2010, 18, 969–974. [Google Scholar] [CrossRef]
- McGarvey, E.L.; Baum, L.D.; Pinkerton, R.C.; Rogers, L.M. Psychological Sequelae and Alopecia Among Women with Cancer. Cancer Pract. 2001, 9, 283–289. [Google Scholar] [CrossRef]
- Kim, I.-R.; Cho, J.-H.; Choi, E.-K.; Kwon, I.G.; Sung, Y.-H.; Lee, J.E.; Nam, S.-J.; Yang, J.-H. Perception, Attitudes, Preparedness and Experience of Chemotherapy-Induced Alopecia among Breast Cancer Patients: A Qualitative Study. Asian Pac. J. Cancer Prev. 2012, 13, 1383–1388. [Google Scholar] [CrossRef]
- Choi, E.K.; Kim, I.-R.; Chang, O.; Kang, D.; Nam, S.-J.; Lee, J.E.; Lee, S.K.; Im, Y.-H.; Park, Y.H.; Yang, J.-H.; et al. Impact of chemotherapy-induced alopecia distress on body image, psychosocial well-being, and depression in breast cancer patients. Psycho-Oncology 2014, 23, 1103–1110. [Google Scholar] [CrossRef]
- Simon, R. Optimal two-stage designs for phase II clinical trials. Control. Clin. Trials 1989, 10, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Morrow, T.; Siegel, M.; Boone, S.; Lawless, G.; Carter, W. Chemotherapy Dose Intensity Determination as a Quality of Care Measure for Managed Care Organizations in the Treatment of Early-Stage Breast Cancer. Am. J. Med Qual. 2002, 17, 218–224. [Google Scholar] [CrossRef]
- Wildiers, H.; Reiser, M. Relative dose intensity of chemotherapy and its impact on outcomes in patients with early breast cancer or aggressive lymphoma. Crit. Rev. Oncol. 2011, 77, 221–240. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.O.; Hsu, N.C.; Moi, S.-H.; Lu, Y.-C.; Hsieh, C.-M.; Chang, K.-J.; Chen, D.-R.; Tu, C.-W.; Wang, H.-C.; Hou, M.-F. Efficacy and toxicity of pegylated liposomal doxorubicin-based chemotherapy in early-stage breast cancer: A multicenter retrospective case-control study. Asia-Pac. J. Clin. Oncol. Hematol. 2018, 14, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Perez, E.A.; Suman, V.J.; Davidson, N.E.; Kaufman, P.A.; Martino, S.; Dakhil, S.R.; Ingle, J.N.; Rodeheffer, R.J.; Gersh, B.J.; Jaffe, A.S. Effect of Doxorubicin Plus Cyclophosphamide on Left Ventricular Ejection Fraction in Patients with Breast Cancer in the North Central Cancer Treatment Group N9831 Intergroup Adjuvant Trial. J. Clin. Oncol. 2004, 22, 3700–3704. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Mohan, N.; Endo, Y.; Shen, Y.; Wu, W.J. Type IIB DNA topoisomerase is downregulated by trastuzumab and doxorubicin to synergize cardiotoxicity. Oncotarget 2017, 9, 6095–6108. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Variable | Level | N = 63 | Percentage (%) |
|---|---|---|---|
| Age (years) | Median (min–max) | 49 (33–76) | |
| Sex | Female | 63 | 100.0 |
| Menopausal status | Pre | 31 | 49.2 |
| Peri | 10 | 15.9 | |
| Post | 22 | 34.9 | |
| ECOG PS | 0 | 62 | 98.4 |
| 1 | 1 | 1.6 | |
| Type of surgery | Mastectomy | 33 | 52.4 |
| Conservative | 30 | 47.6 | |
| Histological type | Ductal | 57 | 90.4 |
| Lobular | 2 | 3.2 | |
| Mixed | 2 | 3.2 | |
| Other | 2 | 3.2 | |
| SNB | No | 8 | 12.7 |
| Yes | 55 | 87.3 | |
| ALND | No | 45 | 71.4 |
| Yes | 18 | 28.6 | |
| Tumor size (mm) | Median (min–max) | 18 (5–65) | |
| T-stage | pT1a | 1 | 1.6 |
| pT1b | 6 | 9.5 | |
| pT1c | 29 | 46.0 | |
| pT2 | 24 | 38.1 | |
| pT3 | 3 | 4.8 | |
| N-stage | pN0/NSentNeg | 33 | 52.4 |
| pN1mi | 7 | 11.1 | |
| pN1a | 19 | 30.2 | |
| pN2a | 2 | 3.2 | |
| pN3a | 2 | 3.2 | |
| TNM stage | IA | 23 | 36.5 |
| IB | 3 | 4.8 | |
| IIA | 18 | 28.6 | |
| IIB | 13 | 20.6 | |
| IIIA | 4 | 6.3 | |
| IIIC | 2 | 3.2 | |
| Grading | G2 | 17 | 27.0 |
| G3 | 46 | 73.0 | |
| Ki-67 expression | Median expression (min–max) | 33% (20–80%) | |
| ≤20% | 2 | 3.2 | |
| >20% | 61 | 96.8 | |
| HER2 status | Negative | 60 | 95.2 |
| Positive | 3 | 4.8 | |
| ER expression | Median expression (min–max) | 95% (15–100%) | |
| >1% | 63 | 100.0 | |
| ≤1% | 0 | 0 | |
| PgR expression | Median expression (min–max) | 80% (0–98%) | |
| >1% | 53 | 84.1 | |
| ≤1% | 10 | 15.9 |
| System Preferred Term | All Grades N (col%) | Grade 1 n (col%) | Grade 2 n (col%) | Grade 3 n (col%) | Grade 4–5 n (col%) |
|---|---|---|---|---|---|
| All related AEs | 164 | 108 | 49 | 7 | 0 |
| Skin and appendages | 71 (43.3) | 45 (63.4) | 21 (29.6) | 5 (7.0) | 0 |
| Palmar-plantar erythrodyestesia | 20 (12.2) | 12 (11.1) | 8 (16.3) | 0 | 0 |
| Erythema | 13 (7.9) | 5 (4.6) | 4 (8.2) | 4 (57.1) | 0 |
| Rash | 10 (6.1) | 7 (6.5) | 3 (6.1) | 0 | 0 |
| Folliculitis | 10 (6.1) | 8 (7.4) | 2 (4.1) | 0 | 0 |
| Eczema | 2 (1.2) | 2 (1.9) | 0 | 0 | 0 |
| Skin dyschromia | 2 (1.2) | 2 (1.9) | 0 | 0 | 0 |
| Dry skin | 2 (1.2) | 2 (1.9) | 0 | 0 | 0 |
| Onychopathy | 3 (1.8) | 1 (0.9) | 2 (4.1) | 0 | 0 |
| Itch | 5 (3.1) | 4 (3.7) | 1 (2.0) | 0 | 0 |
| Other | 4 (2.4) | 2 (1.9) | 1 (2.0) | 1 (14.3) | 0 |
| Gastrointestinal | 42 (25.6) | 31 (73.8) | 11 (26.2) | 0 | 0 |
| Mucositis | 14 (8.5) | 11 (10.2) | 3 (6.1) | 0 | 0 |
| Nausea | 12 (7.3) | 11 (10.2) | 1 (2.0) | 0 | 0 |
| Epigastralgia | 3 (1.8) | 2 (1.9) | 1 (2.0) | 0 | 0 |
| Constipation | 8 (4.9) | 3 (2.8) | 5 (10.2) | 0 | 0 |
| Diarrhea | 1 (0.6) | 1 (0.9) | 0 | 0 | 0 |
| Dysgeusia | 1 (0.6) | 1 (0.9) | 0 | 0 | 0 |
| Abdominal pain | 1 (0.6) | 1 (0.9) | 0 | 0 | 0 |
| Other | 2 (1.2) | 1 (0.9) | 1 (2.0) | 0 | 0 |
| Hepatic | 4 (2.4) | 1 (25.0) | 3 (75.0) | 0 | 0 |
| Transaminases increased | 3 (1.8) | 1 (0.9) | 2 (4.1) | 0 | 0 |
| Bilirubin increased | 1 (0.6) | 0 | 1 (2.0) | 0 | 0 |
| Systemic | 27 (16.5) | 22 (81.5) | 4 (14.8) | 1 (3.7) | 0 |
| Fatigue | 17 (10.4) | 14 (13.0) | 3 (6.1) | 0 | 0 |
| General malaise | 3 (1.8) | 2 (1.9) | 0 | 1 (14.3) | 0 |
| Sweats | 1 (0.6) | 1 (0.9) | 0 | 0 | 0 |
| Fever | 1 (0.6) | 0 | 1 (2.0) | 0 | 0 |
| Headache | 2 (1.2) | 2 (1.9) | 0 | 0 | 0 |
| Dizziness | 1 (0.6) | 1 (0.9) | 0 | 0 | 0 |
| Hot flashes | 2 (1.2) | 2 (1.9) | 0 | 0 | 0 |
| Infusion Related | 4 (2.4) | 0 | 4 (100.0) | 0 | 0 |
| Infusion reaction | 1 (0.6) | 0 | 1 (2.0) | 0 | 0 |
| Chest tightness | 2 (1.2) | 0 | 2 (4.1) | 0 | 0 |
| Lower back pain | 1 (0.6) | 0 | 1 (2.0) | 0 | 0 |
| Hematopoietic | 2 (1.2) | 0 | 1 (50.0) | 1 (50.0) | 0 |
| Leukopenia | 1 (0.6) | 0 | 1 (2.0) | 0 | 0 |
| Neutropenia | 1 (0.6) | 0 | 0 | 1 (14.3) | 0 |
| Cardiovascular | 2 (1.2) | 1 (50.0) | 1 (50.0) | 0 | 0 |
| Hypotension | 1 (0.6) | 1 (0.9) | 0 | 0 | 0 |
| Decreasead LVEF | 1 (0.6) | 0 | 1 (2.0) | 0 | 0 |
| Neuromuscular | 9 (5.5) | 6 (66.7) | 3 (33.3) | 0 | 0 |
| Arthromyalgia | 2 (1.2) | 2 (1.9) | 0 | 0 | 0 |
| Paraesthesia | 3 (1.8) | 2 (1.9) | 1 (2.0) | 0 | 0 |
| Dysesthesia | 3 (1.8) | 1 (0.9) | 2 (4.1) | 0 | 0 |
| Neuralgia | 1 (0.6) | 1 (0.9) | 0 | 0 | 0 |
| Urogenital | 3 (1.8) | 2 (66.7) | 1 (33.3) | 0 | 0 |
| Vaginal dryness | 1 (0.6) | 0 | 1 | 0 | 0 |
| Cystitis | 2 (1.2) | 2 (1.9) | 0 | 0 | 0 |
| All Included Cases | N = 63 | Percentage(%) | |
|---|---|---|---|
| Treatment completed per protocol | 55 | 87.3 | |
| Treatment interrupted | 8 | 12.7 | |
| Cause of definitive interruption | HFS | 2 | 3.2 |
| Rash | 2 | 3.2 | |
| Hyperbilirubinemia | 1 | 1.6 | |
| Decrease ejection fraction | 1 | 1.6 | |
| Infusion reaction | 1 | 1.6 | |
| Physician decision | 1 | 1.6 | |
| Relative dose intensity | |||
| 85% achieved | 55 | 87.3 | |
| 85% not achieved | 8 | 12.7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dellapasqua, S.; Trillo Aliaga, P.; Munzone, E.; Bagnardi, V.; Pagan, E.; Montagna, E.; Cancello, G.; Ghisini, R.; Sangalli, C.; Negri, M.; et al. Pegylated Liposomal Doxorubicin (Caelyx®) as Adjuvant Treatment in Early-Stage Luminal B-like Breast Cancer: A Feasibility Phase II Trial. Curr. Oncol. 2021, 28, 5167-5178. https://doi.org/10.3390/curroncol28060433
Dellapasqua S, Trillo Aliaga P, Munzone E, Bagnardi V, Pagan E, Montagna E, Cancello G, Ghisini R, Sangalli C, Negri M, et al. Pegylated Liposomal Doxorubicin (Caelyx®) as Adjuvant Treatment in Early-Stage Luminal B-like Breast Cancer: A Feasibility Phase II Trial. Current Oncology. 2021; 28(6):5167-5178. https://doi.org/10.3390/curroncol28060433
Chicago/Turabian StyleDellapasqua, Silvia, Pamela Trillo Aliaga, Elisabetta Munzone, Vincenzo Bagnardi, Eleonora Pagan, Emilia Montagna, Giuseppe Cancello, Raffaella Ghisini, Claudia Sangalli, Mara Negri, and et al. 2021. "Pegylated Liposomal Doxorubicin (Caelyx®) as Adjuvant Treatment in Early-Stage Luminal B-like Breast Cancer: A Feasibility Phase II Trial" Current Oncology 28, no. 6: 5167-5178. https://doi.org/10.3390/curroncol28060433
APA StyleDellapasqua, S., Trillo Aliaga, P., Munzone, E., Bagnardi, V., Pagan, E., Montagna, E., Cancello, G., Ghisini, R., Sangalli, C., Negri, M., Mazza, M., Iorfida, M., Cardillo, A., Sciandivasci, A., Bianco, N., De Maio, A. P., Milano, M., Campennì, G. M., Sansonno, L., ... Colleoni, M. (2021). Pegylated Liposomal Doxorubicin (Caelyx®) as Adjuvant Treatment in Early-Stage Luminal B-like Breast Cancer: A Feasibility Phase II Trial. Current Oncology, 28(6), 5167-5178. https://doi.org/10.3390/curroncol28060433





