Acute Care Use by Breast Cancer Patients on Adjuvant Chemotherapy in Alberta: Demonstrating the Importance of Measurement to Improving Quality
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Cohort Creation
2.2. Data Sources and Covariates
2.3. Outcome Definitions
2.4. Statistical Analysis
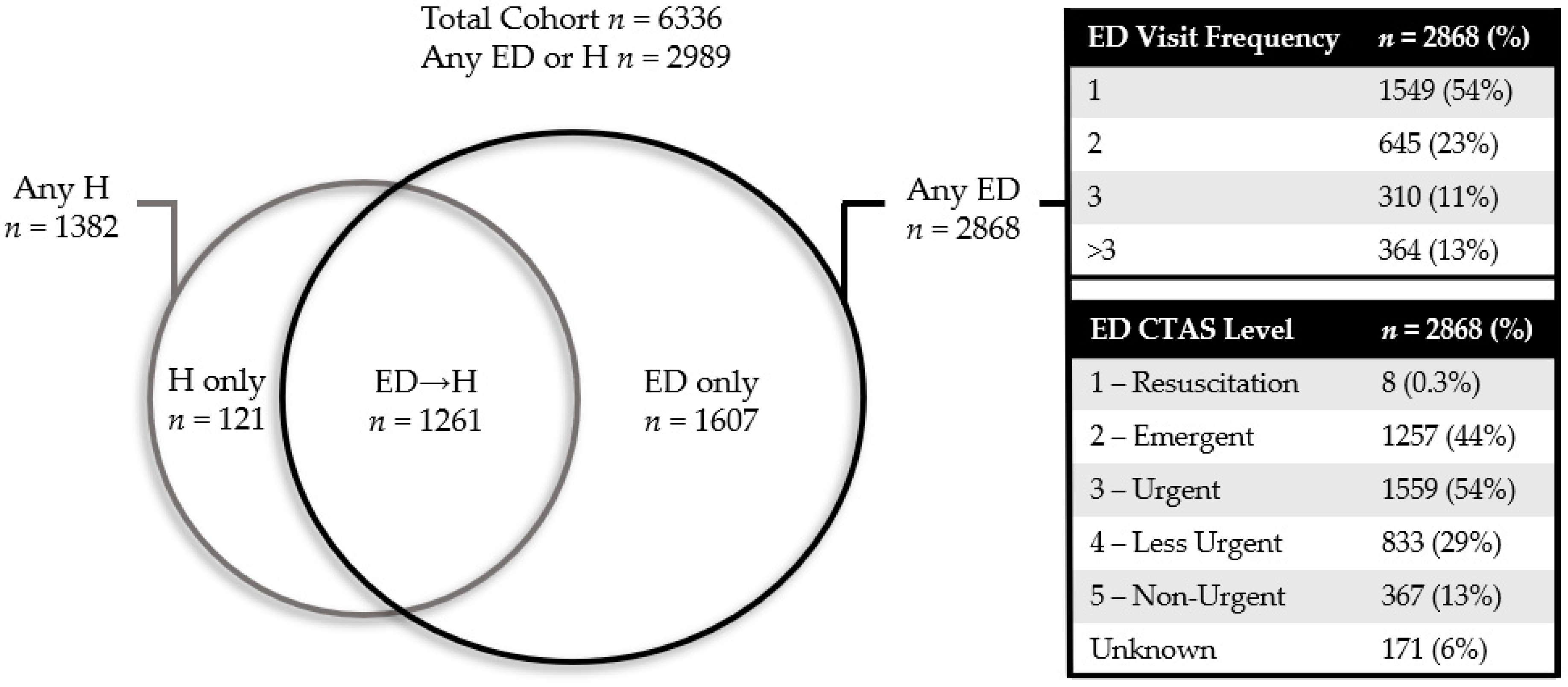
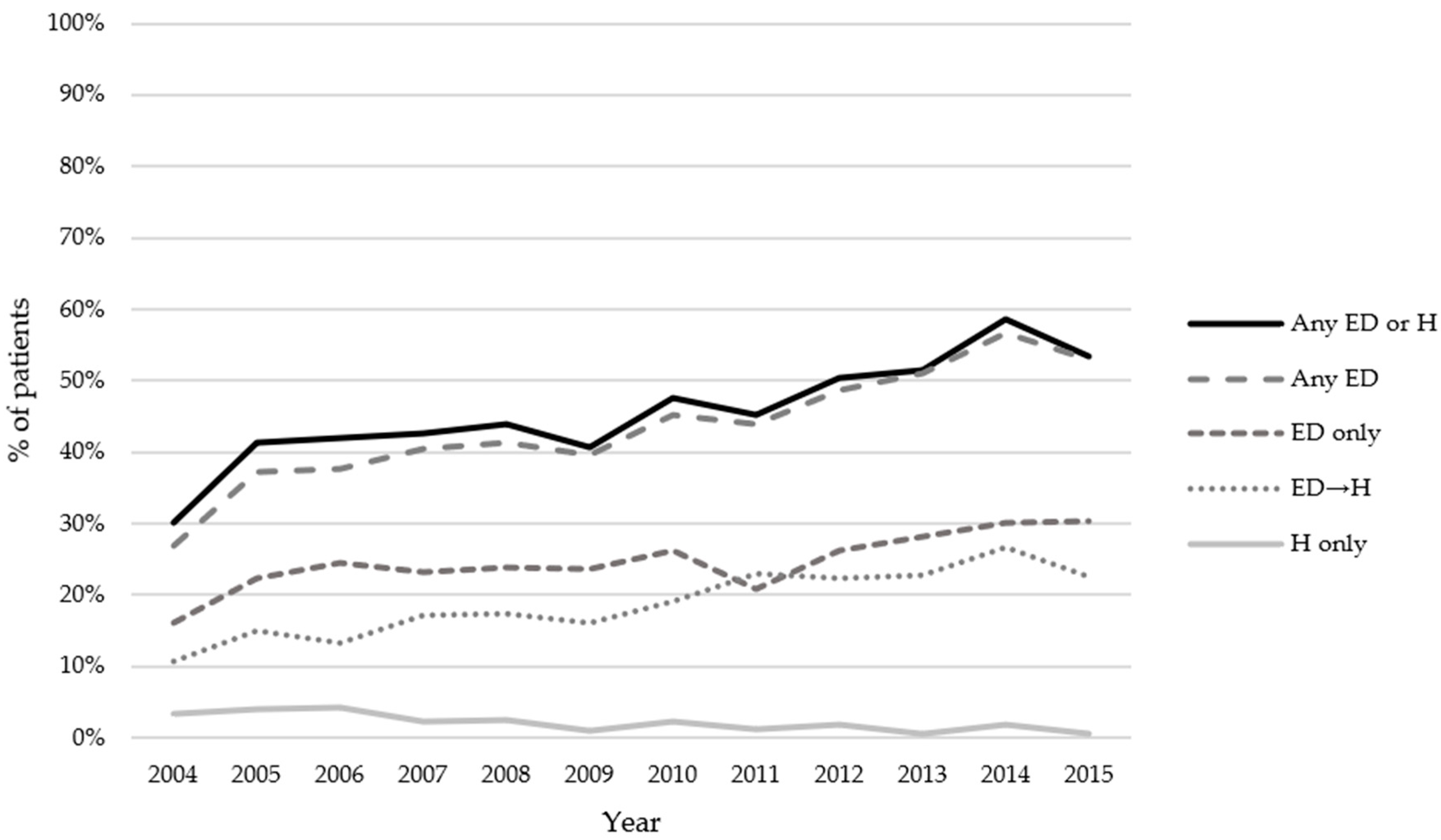
3. Results
Logistic Regression Models for ED and ED→H
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brenner, D.R.; Weir, H.K.; Demers, A.A.; Ellison, L.F.; Louzado, C.; Shaw, A.; Turner, D.; Woods, R.R.; Smith, L.M. Projected Estimates of Cancer in Canada in 2020. CMAJ 2020, 192, E199–E205. [Google Scholar] [CrossRef] [PubMed]
- Hassett, M.J.; O’Malley, A.J.; Pakes, J.R.; Newhouse, J.P.; Earle, C.C. Frequency and cost of chemotherapy-related serious Adverse Effects in a Population Sample of Women With Breast Cancer. J. Natl. Cancer Inst. 2006, 98, 1108–1117. [Google Scholar] [CrossRef] [PubMed]
- Prince, R.M.; Powis, M.; Zer, A.; Atenafu, E.G.; Krzyzanowska, M.K. Hospitalisations and Emergency Department Visits in Cancer Patients Receiving Systemic Therapy: Systematic Review and Meta-Analysis. Eur. J. Cancer Care 2019, 28, e12909. [Google Scholar] [CrossRef] [PubMed]
- Du, X.L.; Osborne, C.; Goodwin, J.S. Population-Based Assessment of Hospitalizations for Toxicity from Chemotherapy in Older Women with Breast Cancer. J. Clin. Oncol. 2002, 20, 4636–4642. [Google Scholar] [CrossRef] [PubMed]
- Powis, M.; Groome, P.; Biswanger, N.; Kendell, C.; Decker, K.M.; Grunfeld, E.; McBride, M.L.; Urquhart, R.; Winget, M.; Porter, G.A.; et al. Cross-Canada Differences in Early-Stage Breast Cancer Treatment and Acute-Care Use. Curr. Oncol. 2019, 26, e624–e639. [Google Scholar] [CrossRef] [PubMed]
- Alberta Health Services Alberta Cancer Registry. 2009 Annual Report of Cancer Statistics; Alberta Health Services: Edmonton, AB, Canada, 2012. [Google Scholar]
- Canadian Institute for Health Information Data Quality Documentation. National Ambulatory Care Reporting System—Current-Year Information, 2019–2020; CIHI: Ottawa, ON, Canada, 2020. [Google Scholar]
- Canadian Institute for Health Information Data Quality Documentation. Discharge Abstract Database—Current-Year Information, 2019–2020; CIHI: Ottawa, ON, Canada, 2020. [Google Scholar]
- Government of Canada, S.C. 2011 Census of Population Program—Data Products. Available online: https://www12.statcan.gc.ca/census-recensement/2011/dp-pd/index-eng.cfm (accessed on 20 July 2021).
- Xu, Y.; Bouchard-Fortier, A.; Olivotto, I.A.; Cheung, W.Y.; Kong, S.; Kornelsen, E.; Laws, A.; Dixon, E.; Dort, J.C.; Craighead, P.S.; et al. “Driving” Rates Down: A Population-Based Study of Opening New Radiation Therapy Centers on the Use of Mastectomy for Breast Cancer. Ann. Surg. Oncol. 2018, 25, 2994–3003. [Google Scholar] [CrossRef] [PubMed]
- Quan, H.; Sundararajan, V.; Halfon, P.; Fong, A.; Burnand, B.; Luthi, J.-C.; Saunders, L.D.; Beck, C.A.; Feasby, T.E.; Ghali, W.A. Coding Algorithms for Defining Comorbidities in ICD-9-CM and ICD-10 Administrative Data. Med. Care 2005, 43, 1130–1139. [Google Scholar] [CrossRef] [PubMed]
- Krzyzanowska, M.K.; Enright, K.; Moineddin, R.; Yun, L.; Powis, M.; Ghannam, M.; Grunfeld, E. Can Chemotherapy-Related Acute Care Visits Be Accurately Identified in Administrative Data? JOP 2017, 14, e51–e58. [Google Scholar] [CrossRef] [PubMed]
- McAlister, F.A.; Tonelli, M.; Wiebe, N.; Lin, M.; Svenson, L.W.; Dean, S. The Ecology of Medical Care for Adults in Alberta, 2002/03 to 2016/17: A Retrospective Cohort Study. Can. Med Assoc. Open Access J. 2020, 8, E169–E177. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fisher, S.; Yasui, Y.; Dabbs, K.; Winget, M. Using Multilevel Models to Explain Variation in Clinical Practice: Surgeon Volume and the Surgical Treatment of Breast Cancer. Ann. Surg. Oncol. 2016, 23, 1845–1851. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.O.A.; Davis, F.; Butts, C.; Winget, M. Waiting Time Intervals for Non-Small Cell Lung Cancer Diagnosis and Treatment in Alberta: Quantification of Intervals and Identification of Risk Factors Associated with Delays. Clin. Oncol. (R Coll. Radiol.) 2016, 28, 750–759. [Google Scholar] [CrossRef] [PubMed]
- Sharma, V.; Weir, D.; Samanani, S.; Simpson, S.H.; Gilani, F.; Jess, E.; Eurich, D.T. Characterisation of Concurrent Use of Prescription Opioids and Benzodiazepine/Z-Drugs in Alberta, Canada: A Population-Based Study. BMJ Open 2019, 9, e030858. [Google Scholar] [CrossRef] [PubMed]
- Enright, K.; Grunfeld, E.; Yun, L.; Moineddin, R.; Ghannam, M.; Dent, S.; Eisen, A.; Trudeau, M.; Kaizer, L.; Earle, C.; et al. Population-Based Assessment of Emergency Room Visits and Hospitalizations among Women Receiving Adjuvant Chemotherapy for Early Breast Cancer. J. Oncol. Pract. 2015, 11, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Cancer Care Ontario. Quality Person-Centred Systemic Treatment in Ontario 2014–2019 Systemic Treatment Provincial Plan; Cancer Care Ontario: Toronto, ON, Canada, 2019. [Google Scholar]
- Barcenas, C.H.; Niu, J.; Zhang, N.; Zhang, Y.; Buchholz, T.A.; Elting, L.S.; Hortobagyi, G.N.; Smith, B.D.; Giordano, S.H. Risk of Hospitalization According to Chemotherapy Regimen in Early-Stage Breast Cancer. J. Clin. Oncol. 2014, 32, 2010–2017. [Google Scholar] [CrossRef] [PubMed]
- Powis, M.; Sutradhar, R.; Gonzalez, A.; Enright, K.A.; Taback, N.A.; Booth, C.M.; Trudeau, M.; Krzyzanowska, M.K. Establishing Achievable Benchmarks for Quality Improvement in Systemic Therapy for Early-Stage Breast Cancer. Cancer 2017, 123, 3772–3780. [Google Scholar] [CrossRef] [PubMed]
- Krzyzanowska, M.K.; Julian, J.A.; Powis, M.; Howell, D.; Earle, C.C.; Enright, K.A.; Mittmann, N.; Trudeau, M.E.; Grunfeld, E. Ambulatory Toxicity Management (AToM) in Patients Receiving Adjuvant or Neo-Adjuvant Chemotherapy for Early Stage Breast Cancer—A Pragmatic Cluster Randomized Trial Protocol. BMC Cancer 2019, 19, 884. [Google Scholar] [CrossRef] [PubMed]
| Variable | Entire Cohort | ED only | ED→H | |
|---|---|---|---|---|
| N = 6336 | N = 1607 | N = 1261 | ||
| Age | Median (IQR) | 52 (45–60) | 52 (45–60) | 53 (46–61) |
| CCI Score | 0 | 4637 (73%) | 1137 (71%) | 853 (68%) |
| 1 | 1327 (21%) | 361 (23%) | 293 (23%) | |
| 2 | 247 (4%) | 72 (5%) | 72 (6%) | |
| >2 | 125 (2%) | 37 (2%) | 43 (3%) | |
| Urban | Rural | 1186 (19%) | 461 (29%) | 275 (22%) |
| Urban | 5148 (81%) | 1146 (71%) | 985 (78%) | |
| Quintile Income | 1 (low) | 783 (12%) | 210 (13%) | 183 (15%) |
| 2 | 1203 (19%) | 325 (20%) | 269 (21%) | |
| 3 | 1163 (18%) | 313 (20%) | 236 (19%) | |
| 4 | 1513 (24%) | 371 (23%) | 280 (22%) | |
| 5 | 1672 (26%) | 388 (24%) | 292 (23%) | |
| Quintile Education | 1 (low) | 944 (15%) | 297 (19%) | 225 (18%) |
| 2 | 1181 (18%) | 343 (21%) | 242 (19%) | |
| 3 | 1280 (20%) | 313 (20%) | 253 (20%) | |
| 4 | 1671 (26%) | 354 (22%) | 314 (25%) | |
| 5 | 1258 (20%) | 300 (19%) | 226 (18%) | |
| Year of Diagnosis | 2004 | 242 (4%) | 39 (2%) | 26 (2%) |
| 2005 | 368 (6%) | 82 (5%) | 55 (4%) | |
| 2006 | 393 (6%) | 96 (6%) | 52 (4%) | |
| 2007 | 483 (8%) | 112 (7%) | 83 (7%) | |
| 2008 | 464 (7%) | 111 (7%) | 81 (6%) | |
| 2009 | 557 (9%) | 132 (8%) | 89 (7%) | |
| 2010 | 570 (9%) | 149 (9%) | 109 (9%) | |
| 2011 | 614 (10%) | 128 (8%) | 141 (11%) | |
| 2012 | 688 (11%) | 180 (11%) | 154 (12%) | |
| 2013 | 648 (10%) | 182 (11%) | 148 (12%) | |
| 2014 | 675 (11%) | 203 (13%) | 180 (14%) | |
| 2015 | 634 (10%) | 193 (12%) | 143 (11%) | |
| Stage | I | 1478 (23%) | 345 (22%) | 274 (22%) |
| II | 3715 (59%) | 972 (61%) | 738 (59%) | |
| III | 1143 (18%) | 290 (18%) | 249 (20%) | |
| T Stage | T1 | 2745 (43%) | 714 (44%) | 529 (42%) |
| T2 | 3141 (50%) | 788 (49%) | 638 (51%) | |
| T3 | 398 (6%) | 91 (6%) | 84 (7%) | |
| T4 | 46 (1%) | 12 (1%) | 9 (1%) | |
| N Stage | N0 | 2949 (47%) | 683 (43%) | 559 (44%) |
| N1 | 2399 (38%) | 670 (42%) | 489 (39%) | |
| N2 | 645 (10%) | 176 (11%) | 133 (11%) | |
| N3 | 343 (5%) | 78 (5%) | 80 (6%) | |
| Biomarker Profile | ER+ or PR+ HER2+ | 658 (10%) | 150 (9%) | 204 (16%) |
| ER+ or PR+ HER2- | 2445 (39%) | 690 (43%) | 490 (39%) | |
| ER- and PR- and HER2+ | 180 (3%) | 42 (3%) | 60 (5%) | |
| ER- and PR- and HER2- | 515 (8%) | 149 (9%) | 113 (9%) | |
| Unknown | 2538 (40%) | 576 (36%) | 394 (31%) | |
| Surgery | Lumpectomy | 3014 (48%) | 744 (46%) | 571 (45%) |
| Mastectomy | 3322 (52%) | 863 (54%) | 690 (55%) | |
| Radiation | No | 1898 (30%) | 464 (29%) | 379 (30%) |
| Yes | 4438 (70%) | 1143 (71%) | 882 (70%) | |
| Regimen Group | Anthracycline/ Non-Taxane | 1155 (18%) | 230 (14%) | 143 (11%) |
| Taxane/ Non-Anthracycline | 2638 (42%) | 641 (40%) | 614 (49%) | |
| Anthracycline/Taxane | 2456 (39%) | 713 (44%) | 486 (39%) | |
| Other | 87 (1%) | 23 (1%) | 18 (1%) | |
| G-CSF Cycles Received | 0 | 3914 (62%) | 970 (60%) | 516 (41%) |
| 1 | 315 (5%) | 81 (5%) | 121 (10%) | |
| 2 | 350 (6%) | 92 (6%) | 137 (11%) | |
| 3 | 764 (12%) | 194 (12%) | 210 (17%) | |
| >3 | 993 (16%) | 270 (17%) | 277 (22%) | |
| Cancer Centre | Community #1 | 210 (3%) | 69 (4%) | 69 (6%) |
| Community #2 | 44 (1%) | 18 (1%) | 14 (1%) | |
| Community #3 | 143 (2%) | 58 (4%) | 33 (3%) | |
| Community #4 | 66 (1%) | 25 (2%) | 8 (1%) | |
| Urban #1 | 2962 (47%) | 819 (51%) | 673 (53%) | |
| Urban #2 | 2739 (43%) | 562 (35%) | 417 (33%) | |
| Multiple | 168 (3%) | 53 (3%) | 46 (4%) | |
| Variable | Univariable OR (95% CI) | Multivariable OR (95% CI) | |
|---|---|---|---|
| Age | Continuous | 1 (0.99 to 1) | 0.99 (0.99 to 1) |
| CCI Score | 0 | Reference | Reference |
| 1 | 1.15 (1 to 1.32) | 1.12 (0.97 to 1.29) | |
| 2 | 1.28 (0.97 to 1.7) | 1.19 (0.89 to 1.6) | |
| >2 | 1.29 (0.88 to 1.91) | 1.17 (0.78 to 1.75) | |
| Urban | Rural | Reference | Reference |
| Urban | 0.45 (0.39 to 0.51) | 0.49 (0.42 to 0.58) | |
| Quintile Income | 1 (low) | Reference | Reference |
| 2 | 1.01 (0.82 to 1.24) | 1.01 (0.82 to 1.24) | |
| 3 | 1 (0.82 to 1.23) | 1.1 (0.89 to 1.37) | |
| 4 | 0.89 (0.73 to 1.08) | 1.08 (0.87 to 1.34) | |
| 5 | 0.82 (0.68 to 1) | 1.14 (0.91 to 1.43) | |
| Quintile Education | 1 (low) | Reference | Reference |
| 2 | 0.89 (0.74 to 1.07) | 1.02 (0.84 to 1.24) | |
| 3 | 0.7 (0.58 to 0.85) | 0.87 (0.71 to 1.07) | |
| 4 | 0.59 (0.49 to 0.7) | 0.78 (0.63 to 0.97) | |
| 5 | 0.68 (0.56 to 0.82) | 0.99 (0.79 to 1.24) | |
| Year of Diagnosis | Continuous | 1.05 (1.03 to 1.07) | 1.06 (1.02 to 1.1) |
| Stage | I | Reference | Reference |
| II | 1.16 (1.01 to 1.34) | 1.06 (0.91 to 1.24) | |
| III | 1.12 (0.93 to 1.34) | 0.95 (0.76 to 1.18) | |
| Biomarker Profile | ER+ or PR+ HER2- | Reference | Reference |
| ER+ or PR+ HER2+ | 0.75 (0.61 to 0.92) | 0.88 (0.71 to 1.09) | |
| ER- and PR- and HER2+ | 0.77 (0.54 to 1.1) | 0.89 (0.62 to 1.29) | |
| ER- and PR- and HER2- | 1.04 (0.84 to 1.28) | 1.06 (0.85 to 1.31) | |
| Other | 0.75 (0.66 to 0.85) | 1.09 (0.87 to 1.37) | |
| Surgery | Lumpectomy | Reference | Reference |
| Mastectomy | 1.07 (0.96 to 1.2) | 1.1 (0.95 to 1.27) | |
| Radiation | No | Reference | Reference |
| Yes | 1.07 (0.95 to 1.21) | 1.05 (0.89 to 1.23) | |
| Regimen Group | Neither | Reference | Reference |
| Anthracycline only | 0.68 (0.41 to 1.12) | 0.88 (0.52 to 1.46) | |
| Both | 1.12 (0.69 to 1.82) | 1.15 (0.69 to 1.91) | |
| Taxane only | 0.88 (0.54 to 1.43) | 0.83 (0.5 to 1.37) | |
| G-CSF Received | No | Reference | Reference |
| Yes | 1.1 (0.98 to 1.24) | 0.88 (0.77 to 1.01) | |
| Cancer Centre | Urban #1 | Reference | Reference |
| Urban #2 | 0.67 (0.6 to 0.76) | 0.71 (0.62 to 0.81) | |
| Community | 1.54 (1.25 to 1.89) | 1.12 (0.89 to 1.41) | |
| Multiple | 1.2 (0.86 to 1.68) | 0.69 (0.48 to 0.99) |
| Variable | Univariable OR (95% CI) | Multivariable OR (95% CI) | |
|---|---|---|---|
| Age | Continuous | 1.01 (1 to 1.01) | 1.01 (1 to 1.01) |
| CCI Score | 0 | Reference | Reference |
| 1 | 1.26 (1.08 to 1.46) | 1.26 (1.07 to 1.47) | |
| 2 | 1.78 (1.33 to 2.37) | 1.65 (1.21 to 2.24) | |
| >2 | 2.33 (1.6 to 3.39) | 2.32 (1.55 to 3.48) | |
| Urban | Rural | Reference | Reference |
| Urban | 0.79 (0.67 to 0.91) | 0.97 (0.81 to 1.16) | |
| Quintile Income | 1 (low) | Reference | Reference |
| 2 | 0.95 (0.76 to 1.17) | 0.92 (0.73 to 1.16) | |
| 3 | 0.84 (0.67 to 1.04) | 0.84 (0.66 to 1.07) | |
| 4 | 0.75 (0.6 to 0.92) | 0.74 (0.58 to 0.94) | |
| 5 | 0.7 (0.57 to 0.86) | 0.74 (0.58 to 0.95) | |
| Quintile Education | 1 (low) | Reference | Reference |
| 2 | 0.82 (0.67 to 1.01) | 0.85 (0.68 to 1.06) | |
| 3 | 0.79 (0.65 to 0.97) | 0.88 (0.7 to 1.12) | |
| 4 | 0.74 (0.61 to 0.9) | 0.91 (0.71 to 1.15) | |
| 5 | 0.7 (0.57 to 0.87) | 0.91 (0.7 to 1.18) | |
| Year of Diagnosis | Continuous | 1.08 (1.06 to 1.1) | 0.97 (0.93 to 1.01) |
| Stage | I | Reference | Reference |
| II | 1.08 (0.93 to 1.26) | 1.08 (0.91 to 1.29) | |
| III | 1.22 (1.01 to 1.48) | 1.24 (0.97 to 1.58) | |
| Biomarker Profile | ER+ or PR+ HER2- | Reference | Reference |
| ER+ or PR+ HER2+ | 1.8 (1.48 to 2.18) | 1.8 (1.46 to 2.22) | |
| ER- and PR- and HER2+ | 2 (1.44 to 2.77) | 2.1 (1.48 to 2.98) | |
| ER- and PR- and HER2- | 1.12 (0.89 to 1.41) | 1.17 (0.91 to 1.49) | |
| Other | 0.73 (0.63 to 0.85) | 1.02 (0.78 to 1.31) | |
| Surgery | Lumpectomy | Reference | Reference |
| Mastectomy | 1.12 (0.99 to 1.27) | 1.06 (0.91 to 1.25) | |
| Radiation | No | Reference | Reference |
| Yes | 0.99 (0.87 to 1.14) | 0.92 (0.77 to 1.1) | |
| Regimen Group | Neither | Reference | Reference |
| Anthracycline only | 0.57 (0.33 to 1) | 0.69 (0.39 to 1.22) | |
| Both | 1 (0.58 to 1.71) | 0.53 (0.3 to 0.94) | |
| Taxane only | 1.23 (0.72 to 2.11) | 0.87 (0.5 to 1.52) | |
| G-CSF Received | No | Reference | Reference |
| Yes | 3.06 (2.69 to 3.47) | 3.96 (3.39 to 4.62) | |
| Cancer Centre | Urban #1 | Reference | Reference |
| Urban #2 | 0.61 (0.53 to 0.7) | 0.56 (0.48 to 0.65) | |
| Community | 1.25 (1 to 1.56) | 0.79 (0.61 to 1.02) | |
| Multiple | 1.29 (0.91 to 1.83) | 1.07 (0.73 to 1.58) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, C.H.D.; Quan, M.L.; Kong, S.; Xu, Y.; Cao, J.Q.; Lupichuk, S.; Barbera, L. Acute Care Use by Breast Cancer Patients on Adjuvant Chemotherapy in Alberta: Demonstrating the Importance of Measurement to Improving Quality. Curr. Oncol. 2021, 28, 4420-4431. https://doi.org/10.3390/curroncol28060375
Wu CHD, Quan ML, Kong S, Xu Y, Cao JQ, Lupichuk S, Barbera L. Acute Care Use by Breast Cancer Patients on Adjuvant Chemotherapy in Alberta: Demonstrating the Importance of Measurement to Improving Quality. Current Oncology. 2021; 28(6):4420-4431. https://doi.org/10.3390/curroncol28060375
Chicago/Turabian StyleWu, Che Hsuan David, May Lynn Quan, Shiying Kong, Yuan Xu, Jeffrey Q. Cao, Sasha Lupichuk, and Lisa Barbera. 2021. "Acute Care Use by Breast Cancer Patients on Adjuvant Chemotherapy in Alberta: Demonstrating the Importance of Measurement to Improving Quality" Current Oncology 28, no. 6: 4420-4431. https://doi.org/10.3390/curroncol28060375
APA StyleWu, C. H. D., Quan, M. L., Kong, S., Xu, Y., Cao, J. Q., Lupichuk, S., & Barbera, L. (2021). Acute Care Use by Breast Cancer Patients on Adjuvant Chemotherapy in Alberta: Demonstrating the Importance of Measurement to Improving Quality. Current Oncology, 28(6), 4420-4431. https://doi.org/10.3390/curroncol28060375





