Risk Factors of Duodenobiliary Reflux-Related Dysfunction of Covered Biliary Metal Stents after Treatment of Duodenal Stricture in Patients with Malignant Biliary and Duodenal Obstruction
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Collection
2.3. Endoscopic and Percutaneous Biliary Drainage Procedure
2.4. Duodenal Metal Stenting and Surgical Gastrojejunostomy
2.5. Statistical Analysis
3. Results
3.1. Patients’ Characteristics
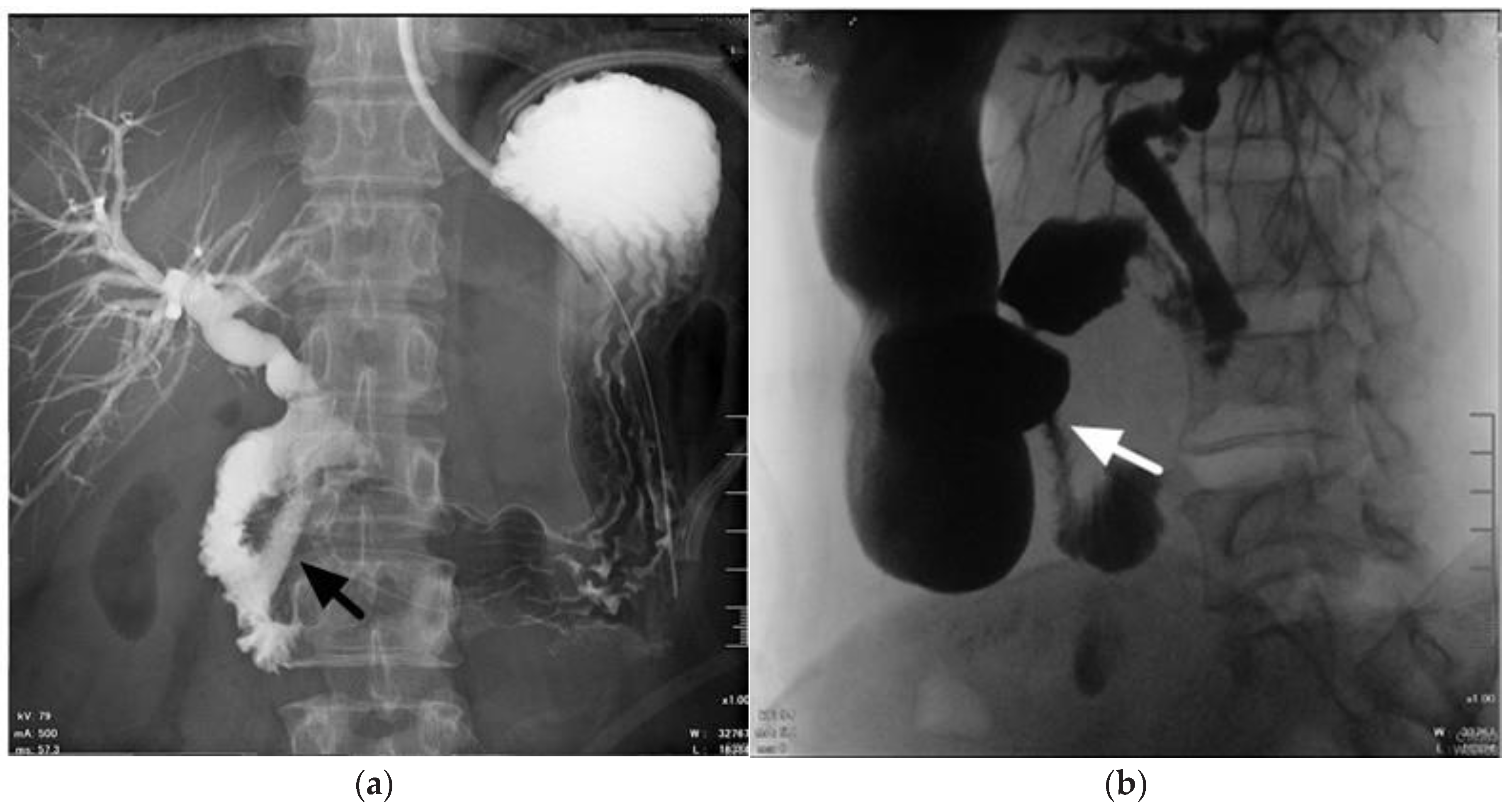
3.2. DBR-Related Biliary SEMS Dysfunction
3.3. Risk Factors of DBR-Related SEMS Dysfunction
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Moss, A.C.; Morris, E.; Leyden, J.; MacMathuna, P. Malignant distal biliary obstruction: A systematic review and meta-analysis of endoscopic and surgical bypass results. Cancer Treat. Rev. 2007, 33, 213–221. [Google Scholar] [CrossRef]
- Almadi, M.A.; Barkun, A.; Martel, M. Plastic vs. self-expandable metal stents for palliation in malignant biliary obstruction: A series of meta-analyses. Off. J. Am. Coll. Gastroenterol. ACG 2017, 112, 260–273. [Google Scholar] [CrossRef]
- Nakai, Y.; Isayama, H.; Komatsu, Y.; Tsujino, T.; Toda, N.; Sasahira, N.; Yamamoto, N.; Hirano, K.; Tada, M.; Yoshida, H. Efficacy and safety of the covered Wallstent in patients with distal malignant biliary obstruction. Gastrointest. Endosc. 2005, 62, 742–748. [Google Scholar] [CrossRef] [PubMed]
- Kogure, H.; Ryozawa, S.; Maetani, I.; Nakai, Y.; Kawakami, H.; Yasuda, I.; Mochizuki, H.; Iwano, H.; Maguchi, H.; Kida, M. A prospective multicenter study of a fully covered metal stent in patients with distal malignant biliary obstruction: WATCH-2 study. Dig. Dis. Sci. 2018, 63, 2466–2473. [Google Scholar] [CrossRef] [PubMed]
- Tringali, A.; Hassan, C.; Rota, M.; Rossi, M.; Mutignani, M.; Aabakken, L. Covered vs. uncovered self-expandable metal stents for malignant distal biliary strictures: A systematic review and meta-analysis. Endoscopy 2018, 50, 631–641. [Google Scholar] [PubMed]
- Hamada, T.; Nakai, Y.; Isayama, H.; Koike, K. Antireflux metal stent for biliary obstruction: Any benefits? Dig. Endosc. 2021, 33, 310–320. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, T.; Fujioka, S.; Yanagisawa, S.; Yanaga, K.; Kakutani, H.; Tajiri, H.; Urashima, M. Placement of a metallic stent across the main duodenal papilla may predispose to cholangitis. Gastrointest. Endosc. 2006, 63, 792–796. [Google Scholar] [CrossRef]
- Misra, S.P.; Dwivedi, M. Reflux of duodenal contents and cholangitis in patients undergoing self-expanding metal stent placement. Gastrointest. Endosc. 2009, 70, 317–321. [Google Scholar] [CrossRef]
- Hamada, T.; Isayama, H.; Nakai, Y.; Togawa, O.; Kogure, H.; Kawakubo, K.; Tsujino, T.; Sasahira, N.; Hirano, K.; Yamamoto, N. Duodenal invasion is a risk factor for the early dysfunction of biliary metal stents in unresectable pancreatic cancer. Gastrointest. Endosc. 2011, 74, 548–555. [Google Scholar] [CrossRef]
- Adler, D.G.; Baron, T.H. Endoscopic palliation of malignant gastric outlet obstruction using self-expanding metal stents: Experience in 36 patients. Am. J. Gastroenterol. 2002, 97, 72. [Google Scholar] [CrossRef]
- Mangiavillano, B.; Khashab, M.A.; Tarantino, I.; Carrara, S.; Semeraro, R.; Auriemma, F.; Bianchetti, M.; Eusebi, L.H.; Chen, Y.-I.; De Luca, L. Success and safety of endoscopic treatments for concomitant biliary and duodenal malignant stenosis: A review of the literature. World J. Gastrointest. Surg. 2019, 11, 53. [Google Scholar] [CrossRef]
- Uemura, S.; Iwashita, T.; Iwata, K.; Mukai, T.; Osada, S.; Sekino, T.; Adachi, T.; Kawai, M.; Yasuda, I.; Shimizu, M. Endoscopic duodenal stent versus surgical gastrojejunostomy for gastric outlet obstruction in patients with advanced pancreatic cancer. Pancreatology 2018, 18, 601–607. [Google Scholar] [CrossRef]
- Nakai, Y.; Hamada, T.; Isayama, H.; Itoi, T.; Koike, K. Endoscopic management of combined malignant biliary and gastric outlet obstruction. Dig. Endosc. 2017, 29, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Dormann, A.; Meisner, S.; Verin, N.; Lang, A.W. Self-expanding metal stents for gastroduodenal malignancies: Systematic review of their clinical effectiveness. Endoscopy 2004, 36, 543–550. [Google Scholar] [CrossRef]
- Graber, I.; Dumas, R.; Filoche, B.; Boyer, J.; Coumaros, D.; Lamouliatte, H.; Legoux, J.; Napoléon, B.; Ponchon, T. The efficacy and safety of duodenal stenting: A prospective multicenter study. Endoscopy 2007, 39, 784–787. [Google Scholar] [CrossRef]
- Piesman, M.; Kozarek, R.A.; Brandabur, J.J.; Pleskow, D.K.; Chuttani, R.; Eysselein, V.E.; Silverman, W.B.; Vargo, J.J.; Waxman, I.; Catalano, M.F. Improved oral intake after palliative duodenal stenting for malignant obstruction: A prospective multicenter clinical trial. Off. J. Am. Coll. Gastroenterol. ACG 2009, 104, 2404–2411. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, R.; Sakai, Y.; Tsuyuguchi, T.; Nishikawa, T.; Fujimoto, T.; Mikami, S.; Sugiyama, H.; Yokosuka, O. Endoscopic management of unresectable malignant gastroduodenal obstruction with a nitinol uncovered metal stent: A prospective Japanese multicenter study. World J. Gastroenterol. 2016, 22, 3837. [Google Scholar] [CrossRef] [PubMed]
- Fiori, E.; Lamazza, A.; Volpino, P.; Burza, A.; Paparelli, C.; Cavallaro, G.; Schillaci, A.; Cangemi, V. Palliative management of malignant antro-pyloric strictures. Gastroenterostomy vs. endoscopic stenting. A randomized prospective trial. Anticancer Res. 2004, 24, 269–272. [Google Scholar] [PubMed]
- Mehta, S.; Hindmarsh, A.; Cheong, E.; Cockburn, J.; Saada, J.; Tighe, R.; Lewis, M.; Rhodes, M. Prospective randomized trial of laparoscopic gastrojejunostomy versus duodenal stenting for malignant gastric outflow obstruction. Surg. Endosc. Other Interv. Tech. 2006, 20, 239–242. [Google Scholar] [CrossRef] [PubMed]
- Hamada, T.; Nakai, Y.; Isayama, H.; Sasaki, T.; Kogure, H.; Kawakubo, K.; Sasahira, N.; Yamamoto, N.; Togawa, O.; Mizuno, S. Duodenal metal stent placement is a risk factor for biliary metal stent dysfunction: An analysis using a time-dependent covariate. Surg. Endosc. 2013, 27, 1243–1248. [Google Scholar] [CrossRef]
- Matsumoto, K.; Kato, H.; Tsutsumi, K.; Mizukawa, S.; Yabe, S.; Seki, H.; Akimoto, Y.; Uchida, D.; Tomoda, T.; Yamamoto, N. Long-term outcomes and risk factors of biliary stent dysfunction after endoscopic double stenting for malignant biliary and duodenal obstructions. Dig. Endosc. 2017, 29, 617–625. [Google Scholar] [CrossRef]
- Mutignani, M.; Tringali, A.; Shah, S.; Perri, V.; Familiari, P.; Iacopini, F.; Spada, C.; Costamagna, G. Combined endoscopic stent insertion in malignant biliary and duodenal obstruction. Endoscopy 2007, 39, 440–447. [Google Scholar] [CrossRef]
- Wu, C.-H.; Lee, M.-H.; Tsou, Y.-K.; Teng, W.; Lin, C.-H.; Sung, K.-F.; Liu, N.-J. Efficacy and Adverse Effects of Self-Expandable Metal Stent Placement for Malignant Duodenal Obstruction: The Papilla of Vater as a Landmark. Cancer Manag. Res. 2020, 12, 10261. [Google Scholar] [CrossRef]
- Hamada, T.; Nakai, Y.; Lau, J.Y.; Moon, J.H.; Hayashi, T.; Yasuda, I.; Hu, B.; Seo, D.-W.; Kawakami, H.; Kuwatani, M. International study of endoscopic management of distal malignant biliary obstruction combined with duodenal obstruction. Scand. J. Gastroenterol. 2018, 53, 46–55. [Google Scholar] [CrossRef] [PubMed]
- Hamada, T.; Isayama, H.; Nakai, Y.; Kogure, H.; Togawa, O.; Kawakubo, K.; Yamamoto, N.; Ito, Y.; Sasaki, T.; Tsujino, T. Novel antireflux covered metal stent for recurrent occlusion of biliary metal stents: A pilot study. Dig. Endosc. 2014, 26, 264–269. [Google Scholar] [CrossRef]
- Hu, B.; Wang, T.-T.; Wu, J.; Shi, Z.-M.; Gao, D.-J.; Pan, Y.-M. Antireflux stents to reduce the risk of cholangitis in patients with malignant biliary strictures: A randomized trial. Endoscopy 2014, 46, 120–126. [Google Scholar] [CrossRef]
- Lee, Y.N.; Moon, J.H.; Choi, H.J.; Choi, M.H.; Lee, T.H.; Cha, S.-W.; Cho, Y.D.; Choi, S.-Y.; Lee, H.K.; Park, S.-H. Effectiveness of a newly designed antireflux valve metal stent to reduce duodenobiliary reflux in patients with unresectable distal malignant biliary obstruction: A randomized, controlled pilot study (with videos). Gastrointest. Endosc. 2016, 83, 404–412. [Google Scholar] [CrossRef] [PubMed]
- Hamada, T.; Isayama, H.; Nakai, Y.; Iwashita, T.; Ito, Y.; Mukai, T.; Yagioka, H.; Saito, T.; Togawa, O.; Ryozawa, S. Antireflux covered metal stent for nonresectable distal malignant biliary obstruction: Multicenter randomized controlled trial. Dig. Endosc. 2019, 31, 566–574. [Google Scholar] [CrossRef] [PubMed]
| Duodenal SEMS (n = 41) | GJJ (n = 13) | p-Value | |
|---|---|---|---|
| Sex, male: female, n:n | 27:14 | 6:7 | p = 0.528 |
| Age, years | 66 ± 13 * | 56 ± 17 * | p = 0.059 |
| Pre-procedure GOOSS score | 0.15 ± 0.38 * | 0.41 ± 0.59 * | p = 0.141 |
| Procedure time, mins | 20.39 ± 6.39 * | 143 ± 65 * | p < 0.001 |
| Post-procedure GOOSS score | 2.22 ± 0.82 * | 1.85 ± 0.81 * | p = 0.157 |
| Clinical success | 30 (96.78%) | 13 (100%) | p = 0.100 |
| Day to intake, days | 4.46 ± 2.31 * | 12.92 ± 7.95 * | p < 0.001 |
| Dysfunction (+) (n = 11) | Dysfunction (-) (n = 43) | p-Value | |
|---|---|---|---|
| Sex, male:female, n:n | 7:4 | 23:20 | p = 0.546 |
| Age, years | 60 ± 15 * | 65 ± 13 * | p = 0.331 |
| TNM stage, III:IV, n:n | 1:10 | 11:32 | p = 0.424 |
| Underlying malignancy | |||
| Pancreatic cancer | 6 (54.55%) | 33 (76.74%) | |
| Duodenal/ampullary cancer | 1 (16.67%) | 4 (9.30%) | |
| Metastatic cancers | 4 (36.36%) | 2 (4.65%) | |
| Bile duct cancer | 0 (0.00%) | 4 (9.30%) | |
| Biliary SEMS | |||
| ERCP/PTBD | 10:1 | 36:7 | p = 0.100 |
| Fully covered/Partially covered | 9:2 | 21:22 | p = 0.087 |
| Treatment for duodenal obstruction | |||
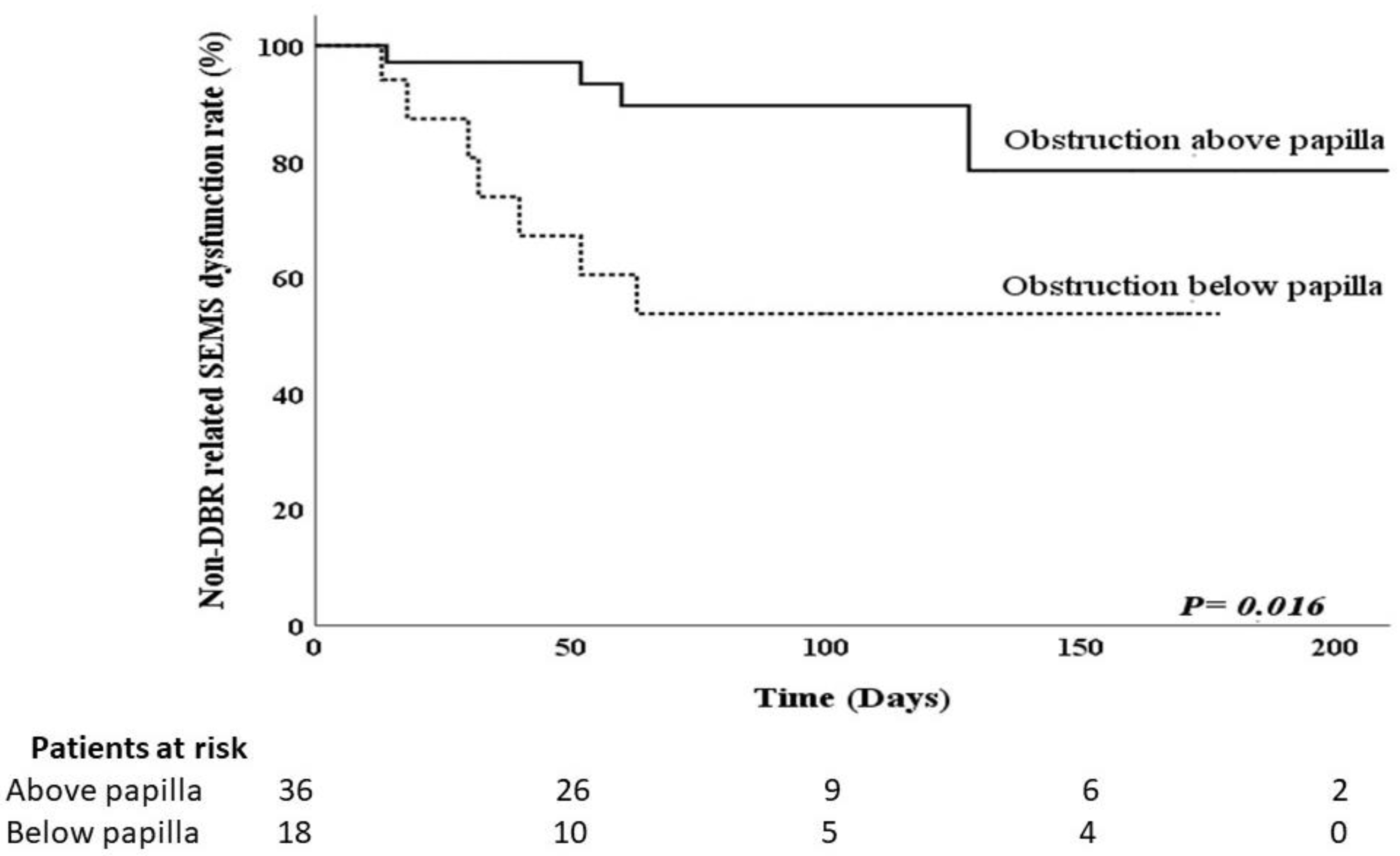
| Stricture above/Below papilla | 4:7 | 32:11 | p = 0.029 |
| Duodenal SEMS: GJJ | 6:5 | 35:8 | p = 0.149 |
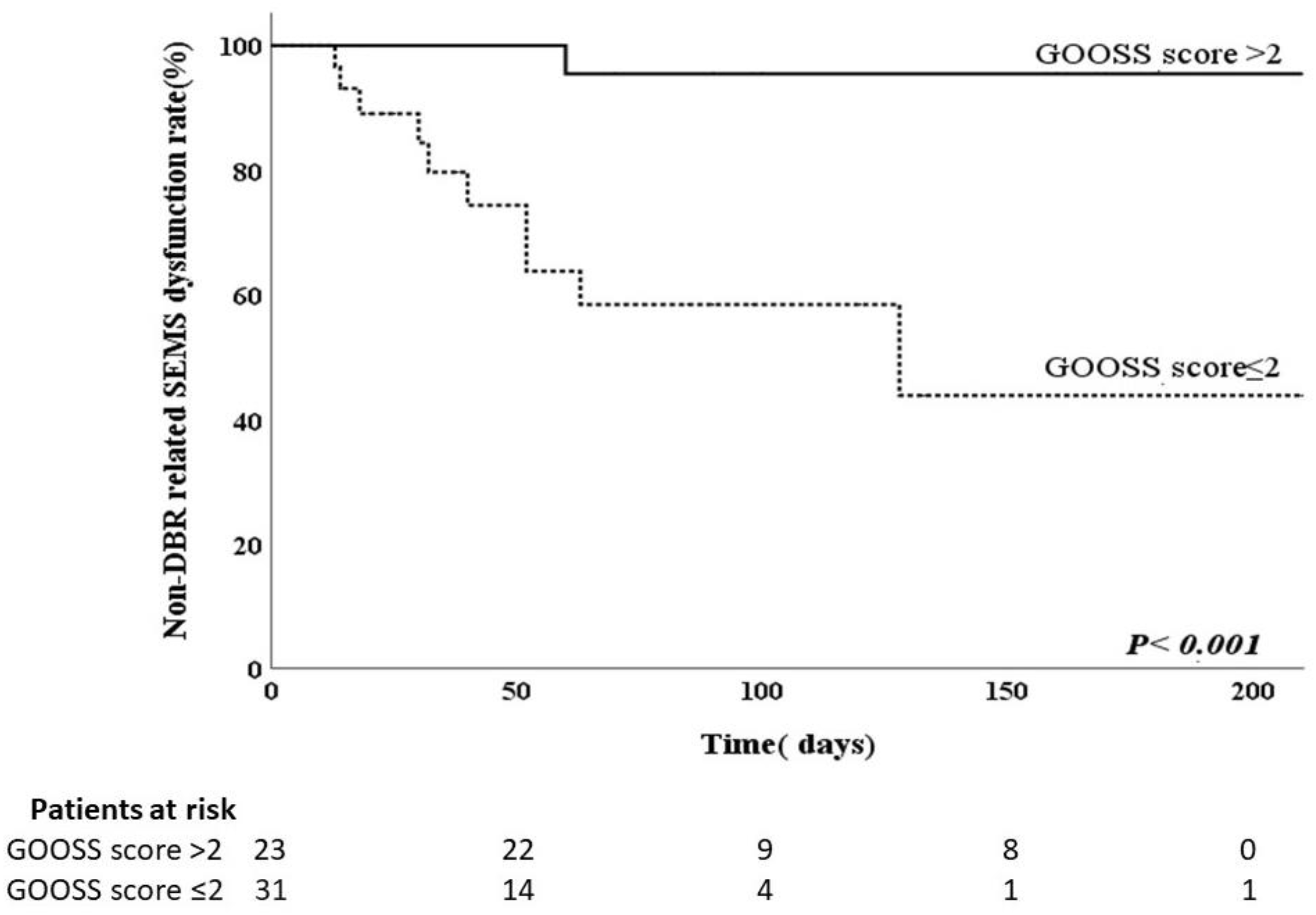
| GOOSS score ≤2 after treatment for duodenal obstruction | 10 (90.90%) | 21 (48.83%) | p = 0.016 |
| Peritoneal carcinomatosis | 6 (64.55%) | 29 (67.44%) | p = 0.489 |
| Chemotherapy | 7 (63.63%) | 28 (65.11%) | p = 0.489 |
| Univariate OR | p-Value | 95% CI for OR | Multivariate OR | p-Value | 95% CI for OR | |
|---|---|---|---|---|---|---|
| Variate | ||||||
| Route of biliary SEMSs | ||||||
| ERCP | 1.994 | |||||
| PTCD | Reference | 0.555 | 0.213–17.713 | |||
| Type of the SEMS | ||||||
| Fully covered | 4.714 | |||||
| Partially covered | Reference | 0.065 | 0.910–24.418 | |||
| Location of duodenal obstruction | ||||||
| Below the papilla of Vater | 5.091 | |||||
| Above the papilla of Vater | Reference | 0.023 | 1.247–20.781 | 5.894 | 0.024 | 1.265–27.459 |
| Duodenal intervention | ||||||
| GJJ | 3.646 | |||||
| Duodenal SEMSs | Reference | 0.073 | 0.887–14.988 | |||
| GOOSS score after treatment for duodenal obstruction | ||||||
| ≤2 | 10.476 | |||||
| >2 | Reference | 0.032 | 1.232–89.115 | 12.000 | 0.028 | 1.301–110.720 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, C.-H.; Lee, M.-H.; Tsou, Y.-K.; Lin, C.-H.; Sung, K.-F.; Pan, K.-T.; Liu, N.-J. Risk Factors of Duodenobiliary Reflux-Related Dysfunction of Covered Biliary Metal Stents after Treatment of Duodenal Stricture in Patients with Malignant Biliary and Duodenal Obstruction. Curr. Oncol. 2021, 28, 3738-3747. https://doi.org/10.3390/curroncol28050319
Wu C-H, Lee M-H, Tsou Y-K, Lin C-H, Sung K-F, Pan K-T, Liu N-J. Risk Factors of Duodenobiliary Reflux-Related Dysfunction of Covered Biliary Metal Stents after Treatment of Duodenal Stricture in Patients with Malignant Biliary and Duodenal Obstruction. Current Oncology. 2021; 28(5):3738-3747. https://doi.org/10.3390/curroncol28050319
Chicago/Turabian StyleWu, Chi-Huan, Mu-Hsien Lee, Yung-Kuan Tsou, Cheng-Hui Lin, Kai-Feng Sung, Kuang-Tse Pan, and Nai-Jen Liu. 2021. "Risk Factors of Duodenobiliary Reflux-Related Dysfunction of Covered Biliary Metal Stents after Treatment of Duodenal Stricture in Patients with Malignant Biliary and Duodenal Obstruction" Current Oncology 28, no. 5: 3738-3747. https://doi.org/10.3390/curroncol28050319
APA StyleWu, C.-H., Lee, M.-H., Tsou, Y.-K., Lin, C.-H., Sung, K.-F., Pan, K.-T., & Liu, N.-J. (2021). Risk Factors of Duodenobiliary Reflux-Related Dysfunction of Covered Biliary Metal Stents after Treatment of Duodenal Stricture in Patients with Malignant Biliary and Duodenal Obstruction. Current Oncology, 28(5), 3738-3747. https://doi.org/10.3390/curroncol28050319





