Distal Fibula Reconstruction in Primary Malignant Tumours
Abstract
1. Introduction
2. Materials and Methods
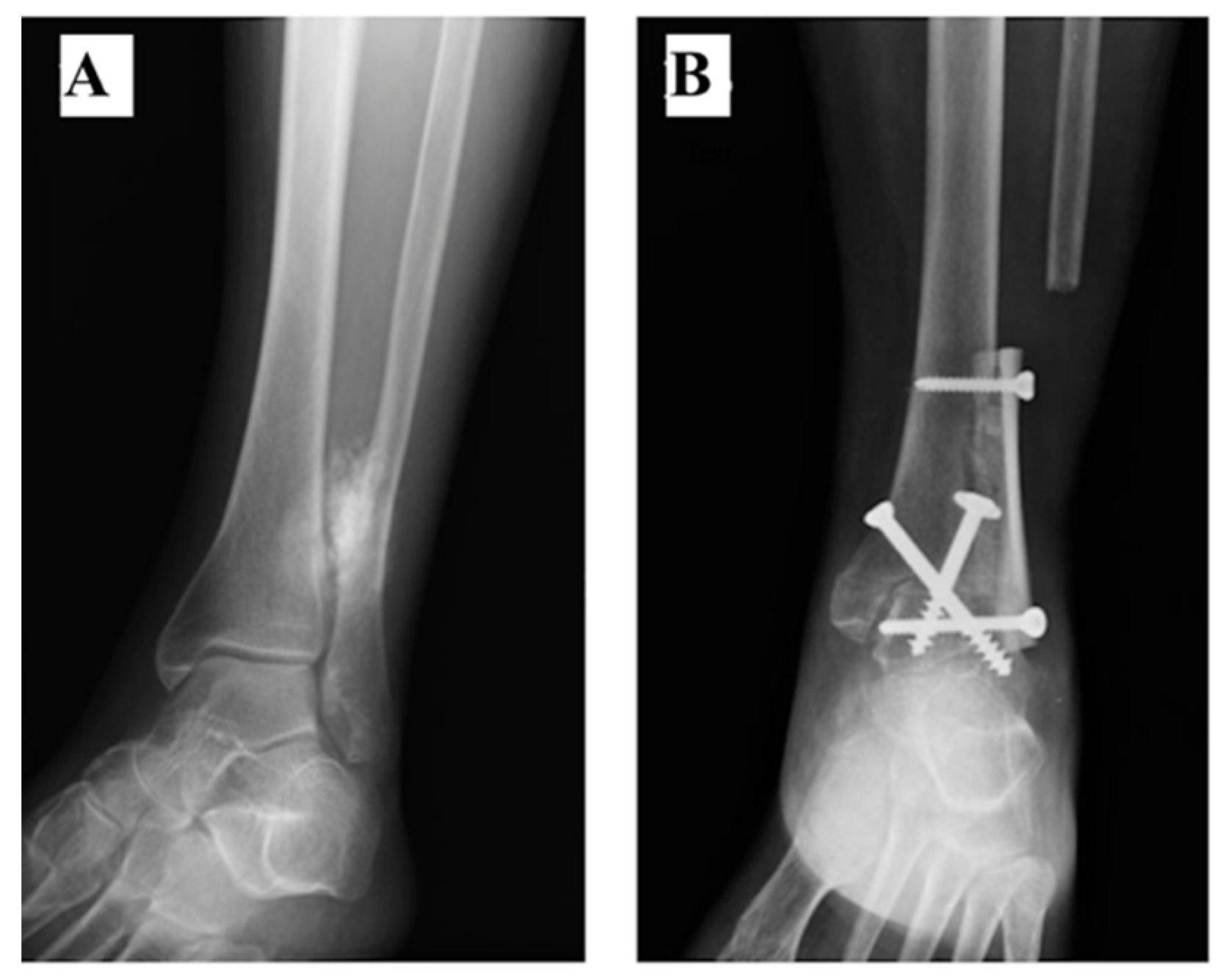
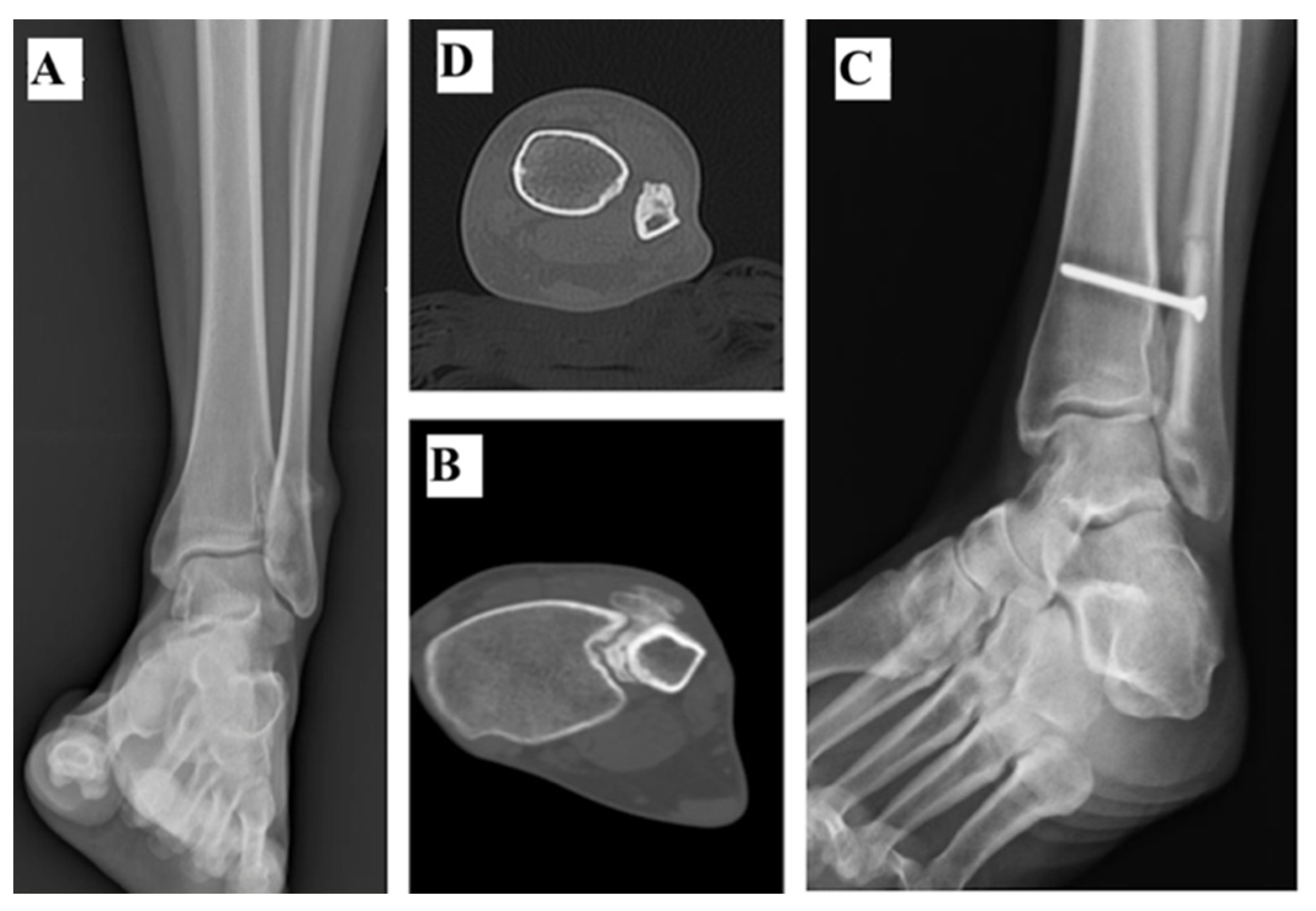
2.1. Tibiotalar Arthrodesis
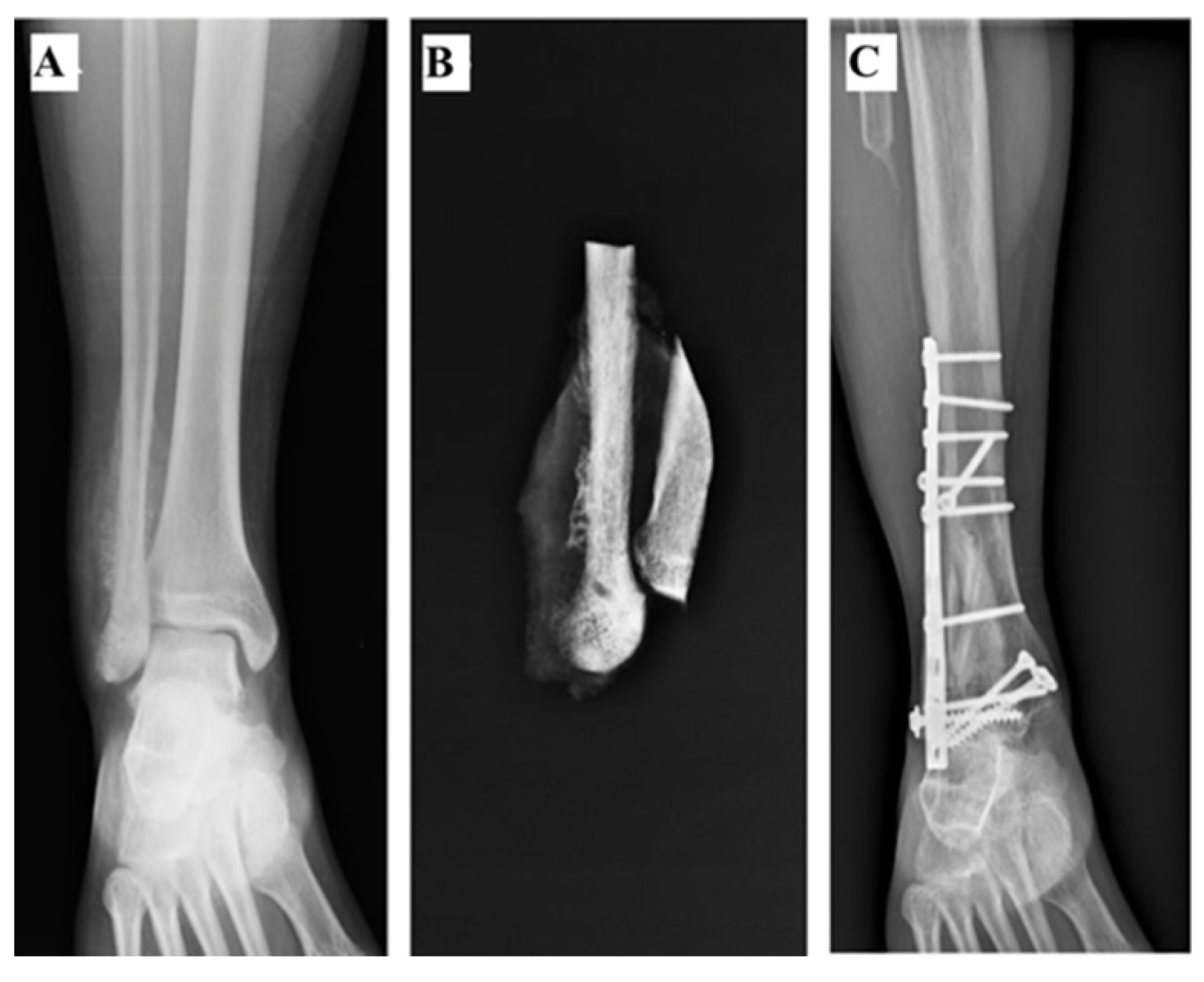
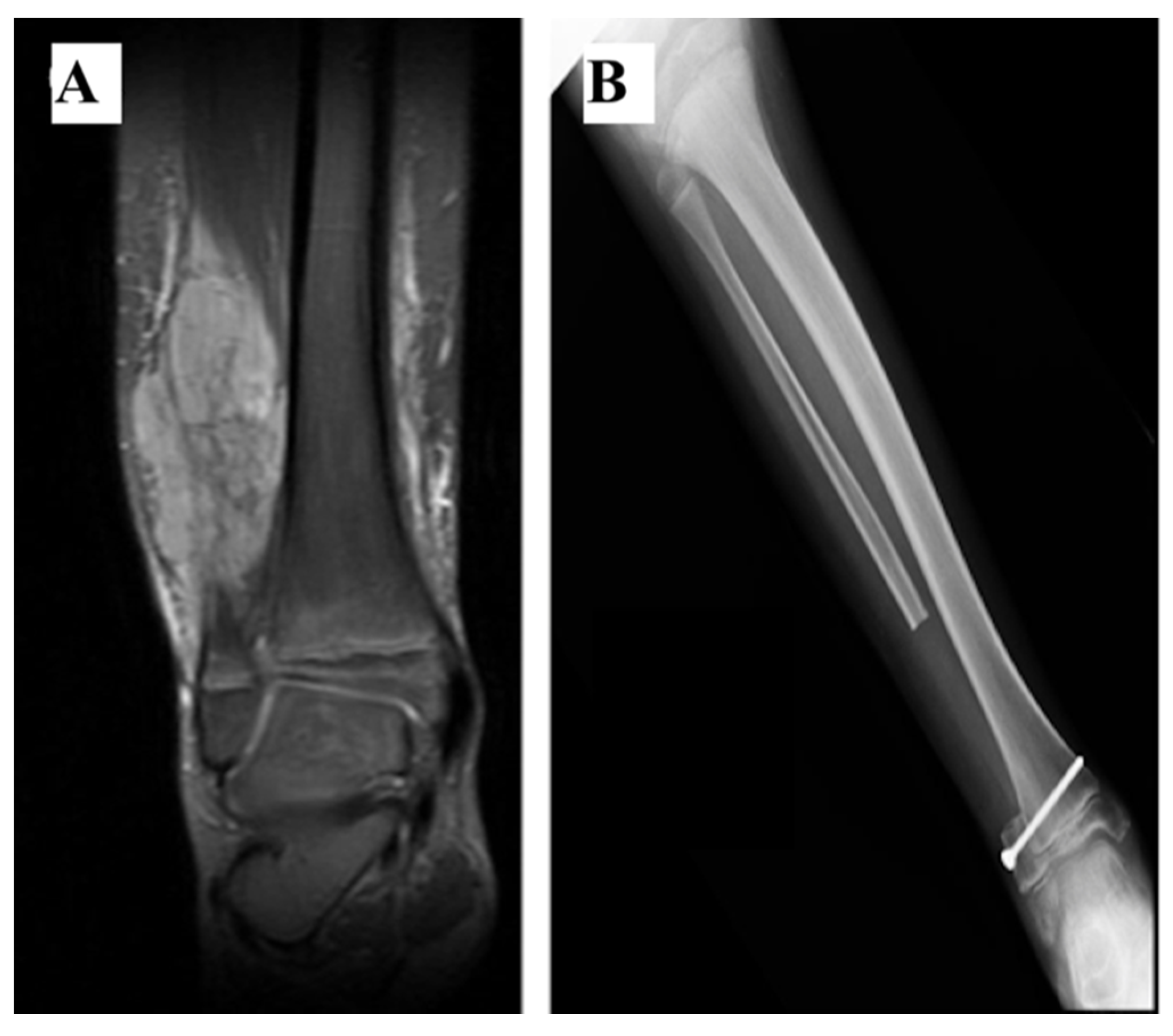
2.2. Rotational Vascularized Fibula Transposition
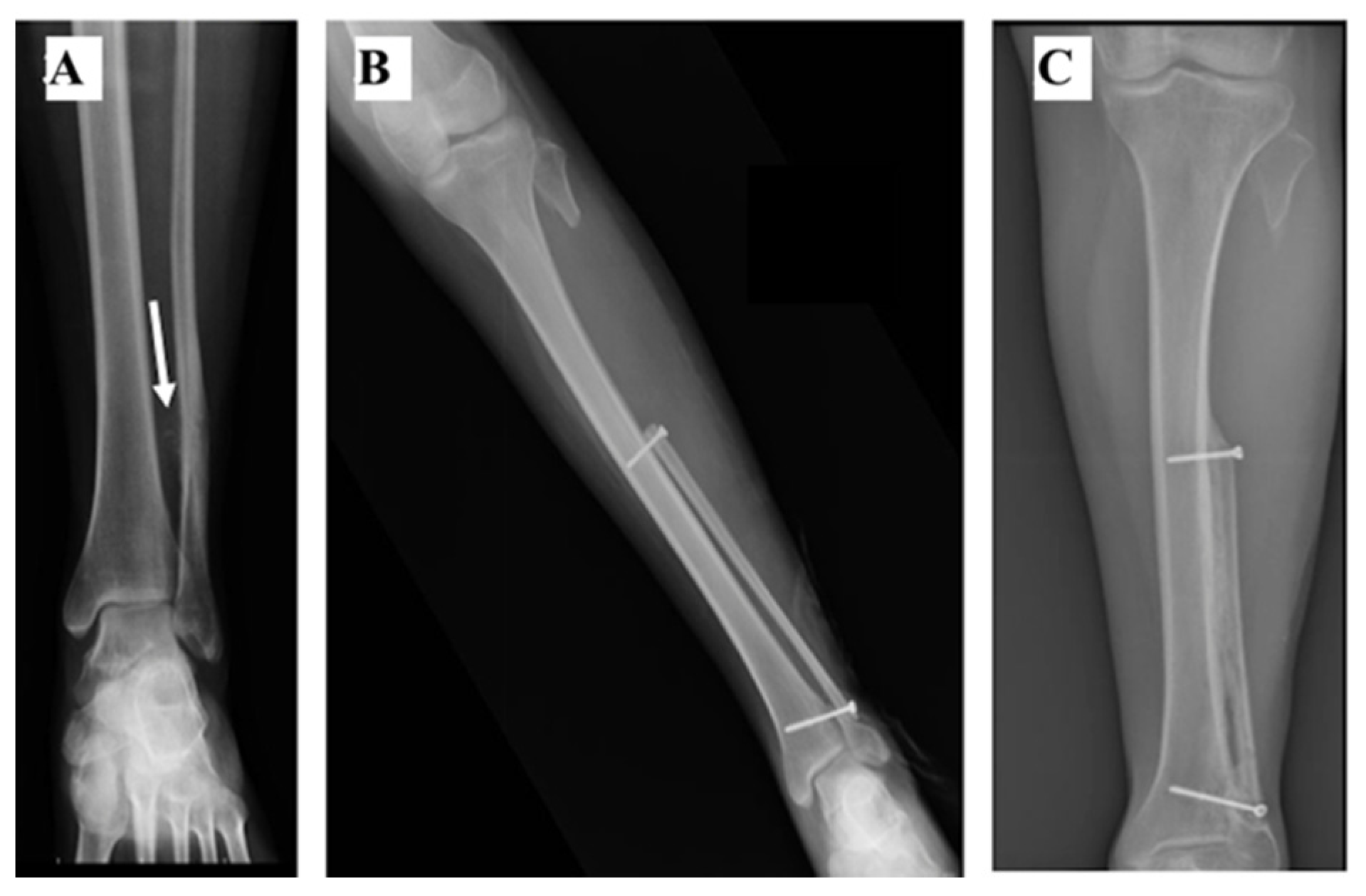
2.3. Non-Vascularized Fibula Transposition
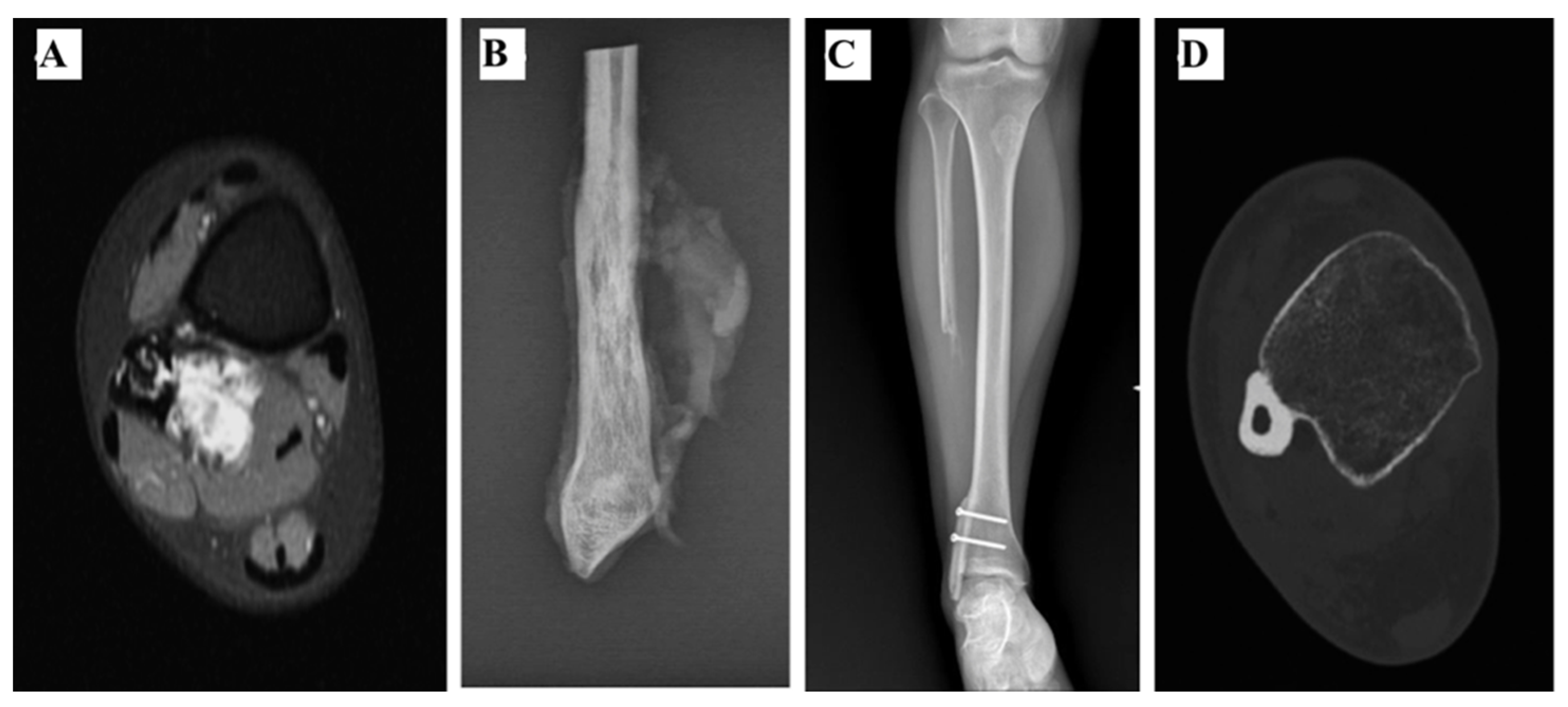
2.4. Intercalary Allograft
2.5. No Reconstruction
3. Results
3.1. Follow-Up
3.2. Surgical Findings
3.3. Clinical and Radiological Findings and Functional Outcome
3.4. Complications
3.5. Local Recurrence and Metastasis
No Local Recurrence Was Observed
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Picci, P. Epidemiology. In Atlas of Musculoskeletal Tumors and Tumorlike Lesions; Picci, P., Manfrini, M., Fabbri, N., Gambarotti, M., Vanel, D., Eds.; Springer International Publishing: Berlin/Heidelberg, Germany, 2014; pp. 3–8. [Google Scholar] [CrossRef]
- Bielack, S.S.; Kempf-Bielack, B.; Delling, G.; Exner, G.U.; Flege, S.; Helmke, K.; Kotz, R.; Salzer-Kuntschik, M.; Werner, M.; Winkelmann, W.; et al. Prognostic Factors in High-Grade Osteosarcoma of the Extremities or Trunk: An Analysis of 1702 Patients Treated on Neoadjuvant Cooperative Osteosarcoma Study Group Protocols. J. Clin. Oncol. 2002, 20, 776–790. [Google Scholar] [CrossRef] [PubMed]
- Zeytoonjian, T.; Mankin, H.J.; Gebhardt, M.C.; Hornicek, F.J. Distal lower extremity sarcomas: Frequency of occurrence and patient survival rate. Foot Ankle Int. 2004, 25, 325–330. [Google Scholar] [CrossRef]
- Brockett, C.L.; Chapman, G.J. Biomechanics of the ankle. Orthop Trauma. 2016, 30, 232–238. [Google Scholar] [CrossRef]
- Leibner, E.D.; Ad-El, D.; Liebergall, M.; Ofiram, E.; London, E.; Peyser, A. Lateral malleolar reconstruction after distal fibular resection. A case report. J. Bone Jt. Surg. Am. 2005, 87, 878–882. [Google Scholar] [CrossRef]
- Jung, S.-T.; Park, H.-W.; Chung, J.-Y. Treatment of a severe neglected valgus deformity after excision of the distal fibula for Ewing’s sarcoma. J. Bone Jt. Surg. Br. 2012, 94, 138–140. [Google Scholar] [CrossRef] [PubMed]
- Capanna, R.; van Horn, J.R.; Biagini, R.; Ruggieri, P.; Bettelli, G.; Campanacci, M. Reconstruction after resection of the distal fibula for bone tumor. Acta Orthop. Scand. 1986, 57, 290–294. [Google Scholar] [CrossRef]
- Abuhassan, F.O.; Shannak, A.O. Subperiosteal resection of aneurysmal bone cysts of the distal fibula. J. Bone Jt. Surg.-Ser. B 2009, 91, 1227–1231. [Google Scholar] [CrossRef]
- de Gauzy, J.S.; Kany, J.; Cahuzac, J.-P. Distal fibular reconstruction with pedicled vascularized fibular head graft: A case report. J. Pediatr. Orthop. B 2002, 11, 176–180. [Google Scholar] [PubMed]
- Gundavda, M.K.; Agarwal, M.G.; Reddy, R.; Bary, A. Reconstructive Challenges of Distal Tibia Bone Tumors: Extracorporeally Irradiated Autograft Combined with a Nonvascularized Autograft Fibula for Superior Reconstruction and Functional Outcomes When Compared to Ipsilateral Pedicled Fibula Transfer Alone. Sarcoma 2021, 2021, 6624550. [Google Scholar] [CrossRef]
- Dieckmann, R.; Ahrens, H.; Streitbürger, A.; Budny, T.B.; Henrichs, M.-P.; Vieth, V.; Gebert, C.; Hardes, J. Reconstruction after wide resection of the entire distal fibula in malignant bone tumours. Int. Orthop. 2011, 35, 87–92. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jamshidi, K.; Mazhar, F.N.; Masdari, Z. Reconstruction of distal fibula with osteoarticular allograft after tumor resection. Foot Ankle Surg. 2013, 19, 31–35. [Google Scholar] [CrossRef]
- Perisano, C.; Marzetti, E.; Spinelli, M.S.; Graci, C.; Fabbriciani, C.; Maffulli, N.; Maccauro, G. Clinical management and surgical treatment of distal fibular tumours: A case series and review of the literature. Int. Orthop. 2012, 36, 1907–1913. [Google Scholar] [CrossRef][Green Version]
- Lee, S.H.; Kim, H.S.; Park, Y.B.; Rhie, T.Y.; Lee, H.K. Prosthetic reconstruction for tumours of the distal tibia and fibula. J. Bone Jt. Surg. Br. 1999, 81, 803–807. [Google Scholar] [CrossRef]
- Lamb, A.; Mueller, J.; Levy, E.; Hobbs, J.L.; Brien, E. Distal fibular excision: A review of the literature and presentation of our reconstruction technique case series. Int. J. Surg. Case Rep. 2021, 80, 105611. [Google Scholar] [CrossRef] [PubMed]
- Marina, N.; Bielack, S.; Whelan, J.; Smeland, S.; Krailo, M.; Sydes, M.R.; Butterfass-Bahloul, T.; Calaminus, G.; Bernstein, M. International collaboration is feasible in trials for rare conditions: The EURAMOS experience. Cancer Treat. Res. 2009, 152, 339–353. [Google Scholar] [CrossRef]
- Righi, A.; Pacheco, M.; Palmerini, E.; Carretta, E.; Gambarotti, M.; Longhi, A.; Magagnoli, G.; Sbaraglia, M.; Manfrini, M.; Picci, P.; et al. Histological response to neoadjuvant chemotherapy in localized Ewing sarcoma of the bone: A retrospective analysis of available scoring tools. Eur. J. Surg. Oncol. 2021, 47, 1778–1783. [Google Scholar] [CrossRef] [PubMed]
- Enneking, W.F.; Spanier, S.S.; Goodman, M.A. A system for the surgical staging of musculoskeletal sarcoma. Clin. Orthop. Relat. Res. 2003, 153, 106–120. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, G.; Sambri, A.; Sebastiani, E.; Caldari, E.; Donati, D. Is unicondylar osteoarticular allograft still a viable option for reconstructions around the knee? Knee 2016, 23, 692–697. [Google Scholar] [CrossRef] [PubMed]
- Enneking, W.F.; Dunham, W.; Gebhardt, M.C.; Malawar, M.; Pritchard, D.J. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin. Orthop. Relat. Res. 1993, 286, 241–246. [Google Scholar] [CrossRef]
- Grimer, R.J.; Taminiau, A.M.; Cannon, S.R. Surgical outcomes in osteosarcoma. J. Bone Jt. Surg.-Ser. B 2002, 84, 395–400. [Google Scholar] [CrossRef]
- Norman-Taylor, F.H.; Sweetnam, D.I.; Fixsen, J.A. Distal fibulectomy for Ewing’s sarcoma. J. Bone Jt. Surg. Br. 1994, 76, 559–562. [Google Scholar] [CrossRef][Green Version]
- Ozaki, T.; Hillmann, A.; Lindner, N.; Winkelmann, W. Surgical treatment of bone sarcomas of the fibula. Analysis of 19 cases. Arch. Orthop. Trauma Surg. 1997, 116, 475–479. [Google Scholar] [CrossRef]
- San-Julian, M.; Duart, J.; de Rada, P.D.; Sierrasesumaga, L. Limb salvage in Ewing’s sarcoma of the distal lower extremity. Foot Ankle Int. 2008, 29, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Schneiderbauer, M.M.; Gullerud, R.; Harmsen, W.S.; Scully, S.P. Fibular osteosarcomas: Contaminated margins may not impact survival. Clin. Orthop. Relat. Res. 2007, 456, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Kanazawa, Y.; Tsuchiya, H.; Nonomura, A.; Takazawa, K.; Yamamoto, N.; Tomita, K. Intentional marginal excision of osteosarcoma of the proximal fibula to preserve limb function. J. Orthop. Sci. 2003, 8, 757–761. [Google Scholar] [CrossRef]
- Rubin, D.I.; Kimmel, D.W.; Cascino, T.L. Outcome of peroneal neuropathies in patients with systemic malignant disease. Cancer 1998, 83, 1602–1606. [Google Scholar] [CrossRef]
- Matsubara, K.; Nigami, H.; Harigaya, H.; Osaki, M.; Baba, K. Peroneal mononeuropathy in pediatric Hodgkin’s disease. Leuk Lymphoma 2001, 40, 205–207. [Google Scholar] [CrossRef]
| Patient # | Age at Surgery and Sex | Diagnosis | Tibial Lateral Cortex Involvement | Enneking Stage | Chemotherapy | Local Postoperative Radiation Therapy | Follow-Up Time (Months) | Oncological Status |
|---|---|---|---|---|---|---|---|---|
| 1 | 71 F | Parosteal Osteosarcoma | Yes | 1B | No | No | 23 | NED |
| 2 | 47 M | Osteosarcoma | Yes | 2B | Yes | No | 26 | DOD |
| 3 | 19 M | Ewing Sarcoma | Yes | 2B | Yes | Yes | 71 | DOD |
| 4 | 27 F | Ewing Sarcoma | Yes | 3 | Yes | Yes | 111 | NED |
| 5 | 19 F | Ewing Sarcoma | Yes | 2B | Yes | No | 18 | NED |
| 6 | 12 M | Ewing Sarcoma | No | 2B | Yes | Yes | 13 | DOD |
| 7 | 37 F | Parosteal Osteosarcoma | No | 1B | No | No | 48 | NED |
| 8 | 14 F | Ewing Sarcoma | No | 3 | Yes | No | 116 | NED |
| 9 | 17 M | Ewing Sarcoma | No | 2B | Yes | Yes | 44 | DOD |
| 10 | 10 M | Ewing Sarcoma | No | 2B | Yes | No | 69 | NED |
| Patient # | ST (min) | RL (cm) | Contaminated RM | Hemi Resection of the Ipsilateral Distal Tibia | Tibiofibular Syndesmosis Resection | Peroneal Nerve Resection | RPM (cm) | RT | BU (Months) | CO | AS | MSTS Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 133 | 7.5 | No | Yes | Yes | No | 0 | TTA | 3 | - | No | 27 |
| 2 | 100 | 11 | No | Yes | Yes | No | 0 | TTA | 4 | Infection | Revision with removal of material | - |
| 3 | 180 | 11.9 | Yes | Yes | Yes | No | 0 | TTA | 12 | - | - | - |
| 4 | 120 | 9.5 | Yes | Yes (periosteal) | No | No | 2 | PedR VFT | 20 | Peroneal nerve palsy Chronic pain | No | 30 |
| 5 | 95 | 11.1 | No | Yes (periosteal) | Yes | No | 0 | FT | 12 | Chronic pain | No | 29 |
| 6 | 118 | 16.5 | Yes | No | Yes | No | 2 | FT | 12 | - | No | 21 |
| 7 | 80 | 4 | No | No | Yes | No | 2 | IA | 3 | - | No | 28 |
| 8 | 115 | 17.8 | No | No | No | Yes | 3 | No | - | Peroneal nerve palsy Chronic pain | No | 27 |
| 9 | 120 | 18 | Yes | No | No | No | 3 | No | - | - | No | - |
| 10 | 73 | 8.5 | No | No | Yes | No | 3 | No | - | Flatfoot | Partial epiphysiodesis Achilles Tendon lengthening | 25 |
| RT | N. of Cases | Author | Complications | MFU (Months) | FO |
|---|---|---|---|---|---|
| AA | 9 | Dieckmann [11] | DWH, Pseudoarthrosis, Talipes equinus, Deep infection, Fracture | 39.9 | E |
| 1 | Ozaki [23] | - | 50 | G | |
| Ped VFT | 2 | Capanna [7] | Reduced ankle mobility | 15 | - |
| 1 | De Gauzy [9] | - | 30 | E | |
| NVFT | 1 | Dieckmann [11] | Intralesional resection (Amputation) | 155 | - |
| 1 | Leibner [5] | - | 60 | E | |
| 1 | Ozaki [23] | Intralesional resection (Amputation) | 43 | P | |
| BC + NVG | 1 | Ozaki [23] | Fatigue Fracture, LLD | 114 | G |
| IG | 3 | Capanna [7] | - | 12 | E |
| 4 | Jamshidi [12] | Valgus deformity, Syndesmosis screw breakage | 38 | E | |
| NR | 1 | Jung [6] | Severe valgus deformity, Limited mobilities, LLD | 84 | - |
| 3 | Ozaki [23] | Wound Necrosis, Drop foot, Intralesional resection (Amputation) | 31 | P | |
| 3 | Capanna [7] | - | 13.5 | E |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khal, A.A.; Zucchini, R.; Giannini, C.; Sambri, A.; Donati, D.M.; De Paolis, M. Distal Fibula Reconstruction in Primary Malignant Tumours. Curr. Oncol. 2021, 28, 3463-3473. https://doi.org/10.3390/curroncol28050299
Khal AA, Zucchini R, Giannini C, Sambri A, Donati DM, De Paolis M. Distal Fibula Reconstruction in Primary Malignant Tumours. Current Oncology. 2021; 28(5):3463-3473. https://doi.org/10.3390/curroncol28050299
Chicago/Turabian StyleKhal, Adyb Adrian, Riccardo Zucchini, Claudio Giannini, Andrea Sambri, Davide Maria Donati, and Massimiliano De Paolis. 2021. "Distal Fibula Reconstruction in Primary Malignant Tumours" Current Oncology 28, no. 5: 3463-3473. https://doi.org/10.3390/curroncol28050299
APA StyleKhal, A. A., Zucchini, R., Giannini, C., Sambri, A., Donati, D. M., & De Paolis, M. (2021). Distal Fibula Reconstruction in Primary Malignant Tumours. Current Oncology, 28(5), 3463-3473. https://doi.org/10.3390/curroncol28050299





