Quality of End-of-Life Care for People with Advanced Non-Small Cell Lung Cancer in Ontario: A Population-Based Study
Abstract
:1. Introduction
Purpose
2. Materials and Methods
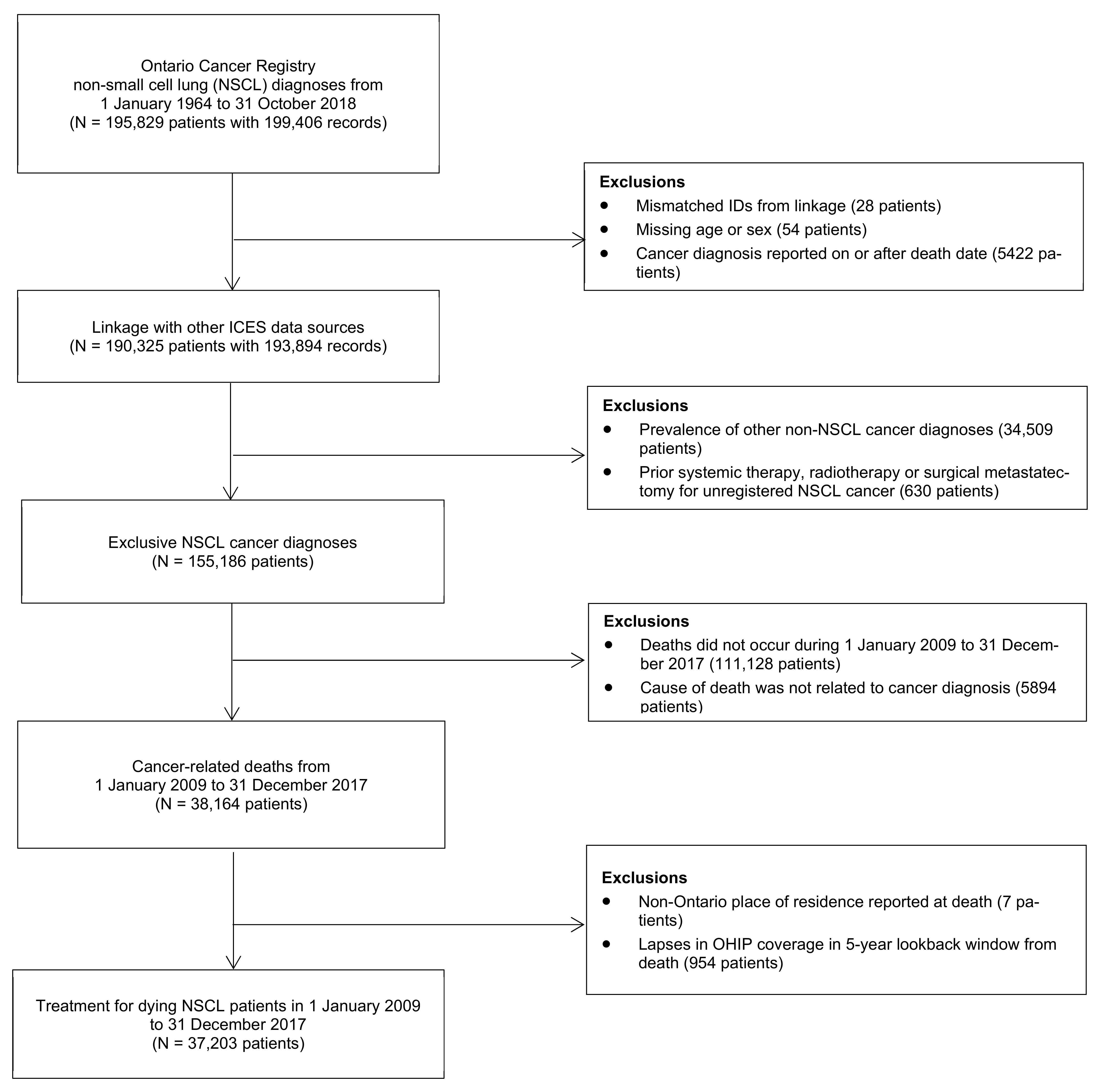
2.1. Study Population
2.2. Data Sources
2.3. Classification of Independent Variables
2.4. Classification of Dependent Variables
2.5. Statistical Analysis
3. Results
3.1. Cohort Description and Patient Demographics
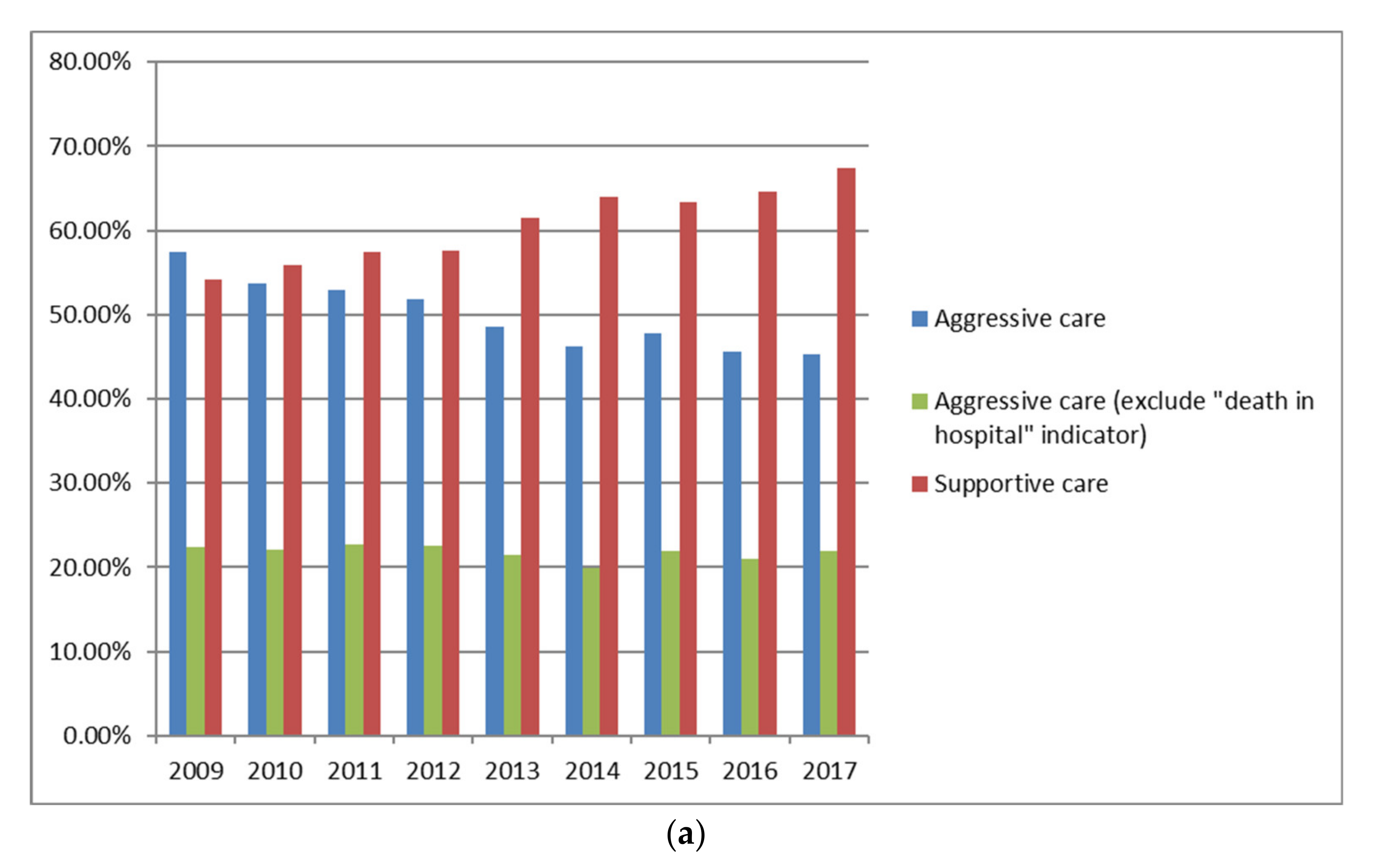
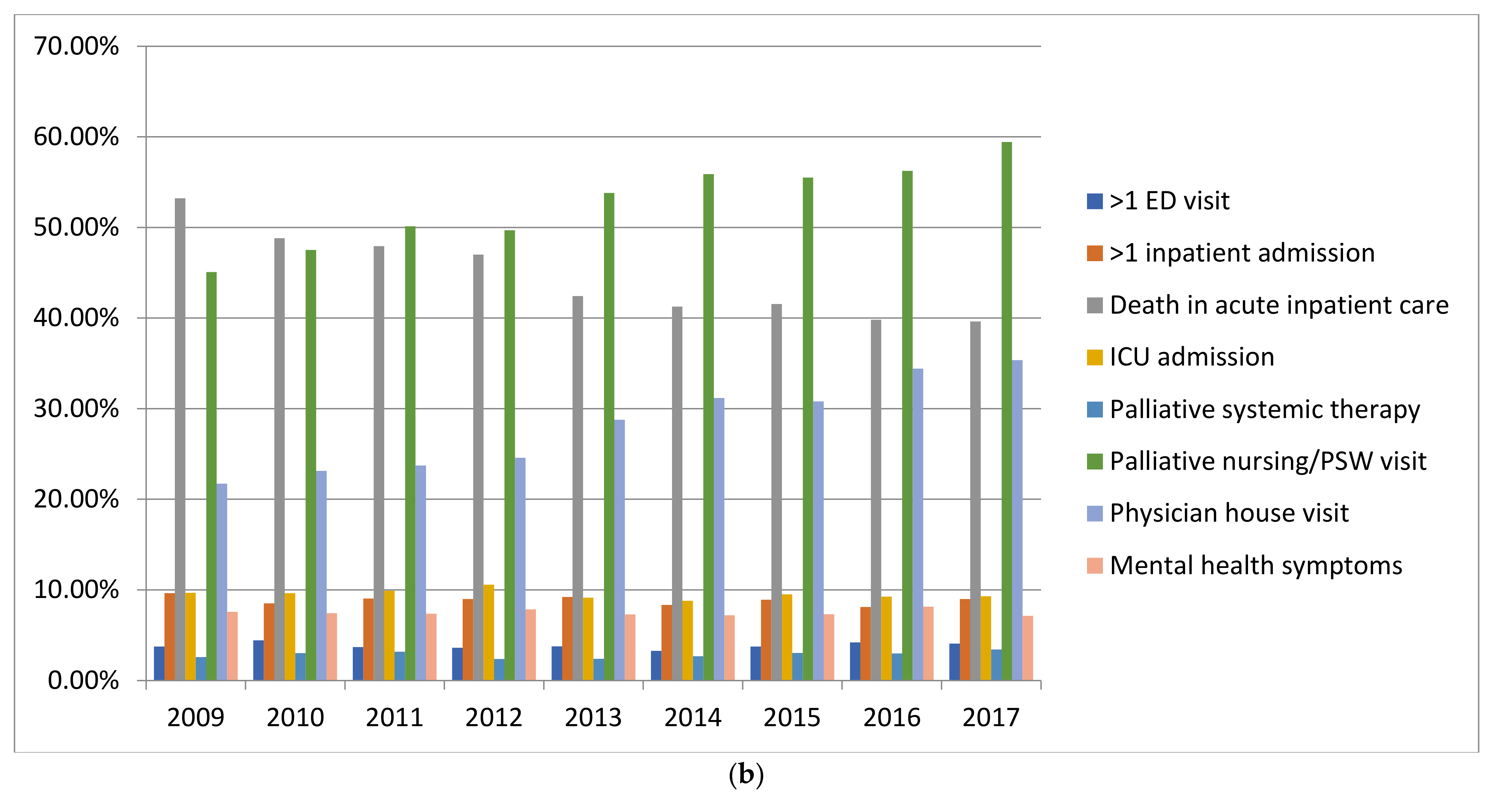
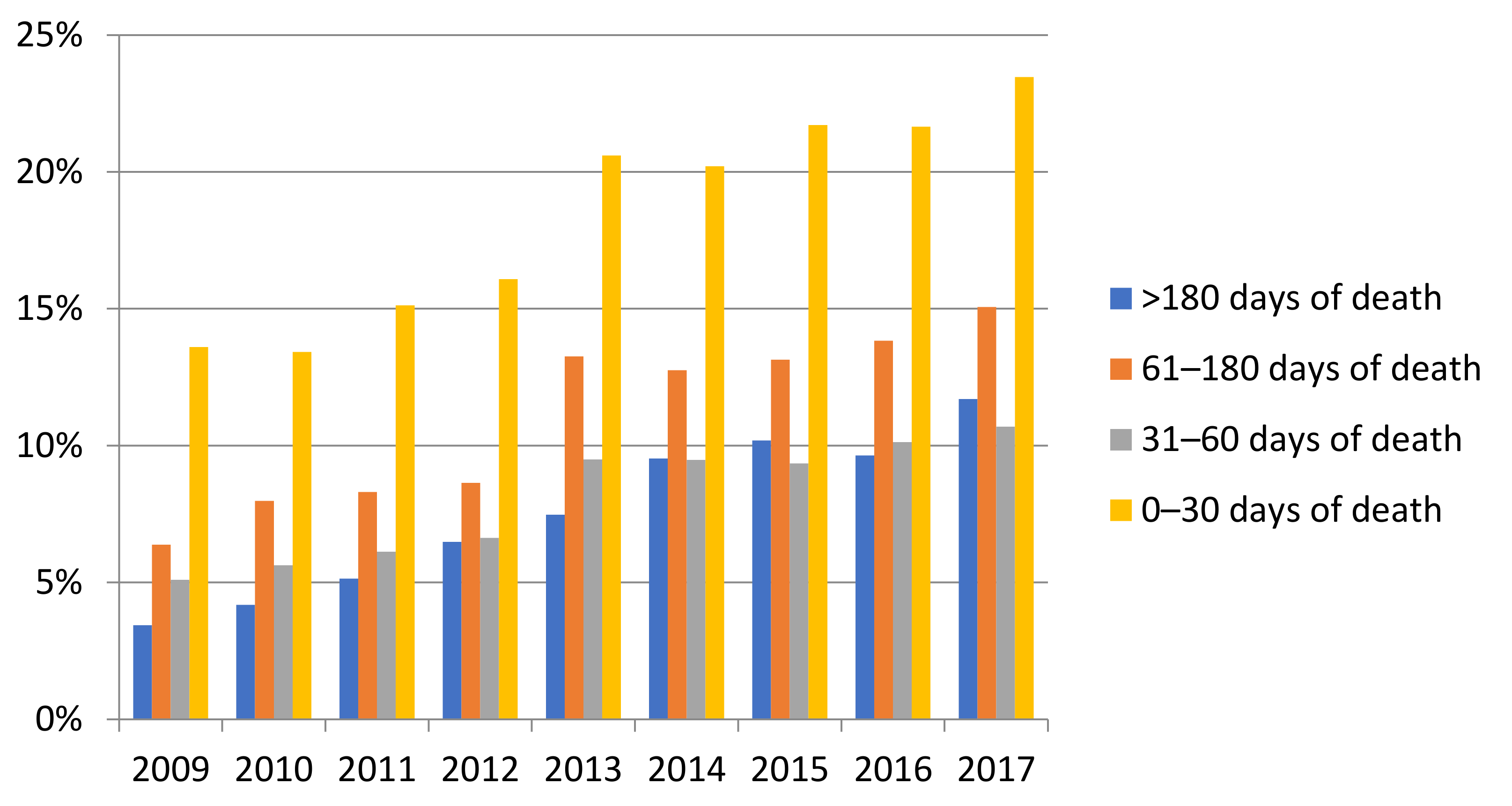
3.2. End of Life Health Service Quality Indicators
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| ICD-O-3 | Term |
|---|---|
| 8000/3 | Neoplasm, malignant |
| 8001/3 | Tumour cells, malignant |
| 8004/3 | Malignant tumour, fusiform cell type |
| 8010/3 | Carcinoma NOS |
| 8012/3 | Large cell carcinoma NOS |
| 8020/3 | Carcinoma, undifferentiated NOS |
| 8021/3 | Carcinoma, anaplastic NOS |
| 8022/3 | Pleomorphic carcinoma |
| 8030/3 | Giant cell and spindle cell carcinoma |
| 8031/3 | Giant cell carcinoma |
| 8032/3 | Spindle cell carcinoma |
| 8034/3 | Polygonal cell carcinoma |
| 8050/3 | Papillary carcinoma NOS |
| 8051/3 | Verrucous carcinoma NOS |
| 8052/3 | Papillary squamous cell carcinoma |
| 8070/3 | Squamous cell carcinoma NOS |
| 8070/6 | Squamous cell carcinoma, metastatic NOS |
| 8071/3 | Squamous cell carcinoma, keratinizing NOS |
| 8072/3 | Squamous cell carcinoma, large cell, nonkeratinizing |
| 8073/3 | Squamous cell carcinoma, small cell, nonkeratinizing |
| 8074/3 | Squamous cell carcinoma, spindle cell |
| 8075/3 | Adenoid squamous cell carcinoma |
| 8076/3 | Squamous cell carcinoma, microinvasive |
| 8082/3 | Lymphoepithelial carcinoma |
| 8094/3 | Basosquamous carcinoma |
| 8120/3 | Transitional cell carcinoma NOS |
| 8130/3 | Papillary transitional cell carcinoma |
| 8140/3 | Adenocarcinoma NOS |
| 8140/6 | Adenocarcinoma, metastatic NOS |
| 8141/3 | Scirrhous adenocarcinoma |
| 8143/3 | Superficial spreading adenocarcinoma |
| 8144/3 | Adenocarcinoma, intestinal type |
| 8145/3 | Carcinoma, diffuse type |
| 8190/3 | Trabecular adenocarcinoma |
| 8200/3 | Adenoid cystic carcinoma |
| 8201/3 | Cribriform carcinoma |
| 8210/3 | Adenocarcinoma in adenomatous polyp |
| 8211/3 | Tubular adenocarcinoma |
| 8230/3 | Solid carcinoma NOS |
| 8231/3 | Carcinoma simplex |
| 8250/3 | Bronchioloalveolar adenocarcinoma |
| 8251/3 | Alveolar adenocarcinoma |
| 8260/3 | Papillary adenocarcinoma NOS |
| 8261/3 | Adenocarcinoma in villous adenoma |
| 8263/3 | Adenocarcinoma in tubulovillous adenoma |
| 8290/3 | Oxyphilic adenocarcinoma |
| 8310/3 | Clear cell adenocarcinoma NOS |
| 8323/3 | Mixed cell adenocarcinoma |
| 8330/3 | Follicular adenocarcinoma NOS |
| 8340/3 | Papillary carcinoma, follicular variant |
| 8380/3 | Endometrioid carcinoma |
| 8401/3 | Apocrine adenocarcinoma |
| 8410/3 | Sebaceous adenocarcinoma |
| 8420/3 | Ceruminous adenocarcinoma |
| 8430/3 | Mucoepidermoid carcinoma |
| 8440/3 | Cystadenocarcinoma NOS |
| 8441/3 | Serous cystadenocarcinoma NOS |
| 8442/3 | Serous cystadenoma, borderline malignancy |
| 8462/3 | Papillary serous cystadenoma, borderline malignancy |
| 8470/3 | Mucinous cystadenocarcinoma NOS |
| 8472/3 | Mucinous cystadenoma, borderline malignancy |
| 8480/3 | Mucinous adenocarcinoma |
| 8481/3 | Mucin-producing adenocarcinoma |
| 8490/3 | Signet ring cell carcinoma |
| 8490/6 | Metastatic signet ring cell carcinoma |
| 8500/3 | Infiltrating duct carcinoma |
| 8510/3 | Medullary carcinoma NOS |
| 8550/3 | Acinar cell carcinoma |
| 8560/3 | Adenosquamous carcinoma |
| 8562/3 | Epithelial-myoepithelial carcinoma |
| 8570/3 | Adenocarcinoma with squamous metaplasia |
| 8572/3 | Adenocarcinoma with spindle cell metaplasia |
| 8802/3 | Giant cell sarcoma |
| 8980/3 | Carcinosarcoma NOS |
| ICD-O-3 | Term |
| C34.0 | Main bronchus |
| C34.1 | Upper lobe, lung |
| C34.2 | Middle lobe, lung (right lung only) |
| C34.3 | Lower lobe, lung |
| C34.8 | Overlapping lesion of lung |
| C34.9 | Lung, NOS |
References
- Brenner, D.R.; Weir, H.K.; Demers, A.A.; Ellison, L.F.; Louzado, C.; Shaw, A.; Turner, D.; Woods, R.R.; Smith, L.M. Projected estimates of cancer in Canada in 2020. Can. Med. Assoc. J. 2020, 192, E199–E205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ontario Health (Cancer Care Ontario). Ontario Cancer Statistics 2020; Ontario Cancer Statistics: Toronto, ON, Canada, 2020; ISBN 978-1-4868-3681-9. [Google Scholar]
- Temel, J.S.; Greer, J.A.; Muzikansky, A.; Gallagher, E.R.; Admane, S.; Jackson, V.A.; Dahlin, C.M.; Blinderman, C.D.; Jacobsen, J.; Pirl, W.F.; et al. Early Palliative Care for Patients with Metastatic Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2010, 363, 733–742. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Y.; Van Dam, A.; Slaven, M.; Ellis, K.J.; Goffin, J.R.; Juergens, R.A.; Ellis, P.M. Resource use in the last three months of life by lung cancer patients in southern Ontario. Curr. Oncol. 2019, 26, 247–252. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whitney, R.L.; Bell, J.F.; Tancredi, D.J.; Romano, P.S.; Bold, R.J.; Joseph, J.G. Hospitalization Rates and Predictors of Rehospitalization among Individuals with Advanced Cancer in the Year after Diagnosis. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2017, 35, 3610–3617. [Google Scholar] [CrossRef] [Green Version]
- Iyer, S.; Taylor-Stokes, G.; Roughley, A. Symptom burden and quality of life in advanced non-small cell lung cancer patients in France and Germany. Lung Cancer 2013, 81, 288–293. [Google Scholar] [CrossRef]
- Farbicka, P.; Nowicki, A. Palliative care in patients with lung cancer. Contemp. Oncol. 2013, 17, 238–245. [Google Scholar] [CrossRef] [Green Version]
- Ramirez, R.A.; Lu, J.; Thomas, K.E.H. Quality of life for non-small cell lung cancer patients in the age of immunotherapy. Transl. Lung Cancer Res. 2018, 7, S149–S152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Henson, L.A.; Edmonds, P.; Johnston, A.; Johnson, H.E.; Ng Yin Ling, C.; Sklavounos, A.; Ellis-Smith, C.; Gao, W. Population-Based Quality Indicators for End-of-Life Cancer Care: A Systematic Review. JAMA Oncol. 2020, 6, 142–150. [Google Scholar] [CrossRef]
- Barbera, L.; Seow, H.; Sutradhar, R.; Chu, A.; Burge, F.; Fassbender, K.; McGrail, K.; Lawson, B.; Liu, Y.; Pataky, R.; et al. Quality Indicators of End-of-Life Care in Patients with Cancer: What Rate Is Right? J. Oncol. Pract. 2015, 11, e279–e287. [Google Scholar] [CrossRef]
- Barbera, L.; Seow, H.; Sutradhar, R.; Chu, A.; Burge, F.; Fassbender, K.; McGrail, K.; Lawson, B.; Liu, Y.; Pataky, R.; et al. Quality of end-of-life cancer care in Canada: A retrospective four-province study using administrative health care data. Curr. Oncol. 2015, 22, 341–355. [Google Scholar] [CrossRef] [Green Version]
- Bekelman, J.E.; Halpern, S.D.; Blankart, C.R.; Bynum, J.P.; Cohen, J.; Fowler, R.; Kaasa, S.; Kwietniewski, L.; Melberg, H.O.; Onwuteaka-Philipsen, B.; et al. Comparison of Site of Death, Health Care Utilization, and Hospital Expenditures for Patients Dying with Cancer in 7 Developed Countries. JAMA J. Am. Med. Assoc. 2016, 315, 272–283. [Google Scholar] [CrossRef] [PubMed]
- Cheung, M.C.; Earle, C.C.; Rangrej, J.; Ho, T.H.; Liu, N.; Barbera, L.; Saskin, R.; Porter, J.; Seung, S.J.; Mittmann, N. Impact of aggressive management and palliative care on cancer costs in the final month of life. Cancer 2015, 121, 3307–3315. [Google Scholar] [CrossRef] [PubMed]
- Ho, T.H.; Barbera, L.; Saskin, R.; Lu, H.; Neville, B.A.; Earle, C.C. Trends in the aggressiveness of end-of-life cancer care in the universal health care system of Ontario, Canada. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2011, 29, 1587–1591. [Google Scholar] [CrossRef] [Green Version]
- Wang, S.Y.; Hall, J.; Pollack, C.E.; Adelson, K.; Bradley, E.H.; Long, J.B.; Gross, C.P. Trends in end-of-life cancer care in the Medicare program. J. Geriatr. Oncol. 2016, 7, 116–125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gonsalves, W.I.; Tashi, T.; Krishnamurthy, J.; Davies, T.; Ortman, S.; Thota, R.; Aldoss, I.; Ganta, A.; Kalaiah, M.; Didwaniya, N.; et al. Effect of palliative care services on the aggressiveness of end-of-life care in the Veteran’s Affairs cancer population. J. Palliat. Med. 2011, 14, 1231–1235. [Google Scholar] [CrossRef]
- Michael, N.; Beale, G.; O’Callaghan, C.; Melia, A.; DeSilva, W.; Costa, D.; Kissane, D.; Shapiro, J.; Hiscock, R. Timing of palliative care referral and aggressive cancer care toward the end-of-life in pancreatic cancer: A retrospective, single-center observational study. BMC Palliat. Care 2019, 18, 13. [Google Scholar] [CrossRef]
- Scibetta, C.; Kerr, K.; McGuire, J.; Rabow, M.W. The Costs of Waiting: Implications of the Timing of Palliative Care Consultation among a Cohort of Decedents at a Comprehensive Cancer Center. J. Palliat. Med. 2016, 19, 69–75. [Google Scholar] [CrossRef]
- Jang, R.W.; Krzyzanowska, M.K.; Zimmermann, C.; Taback, N.; Alibhai, S.M. Palliative care and the aggressiveness of end-of-life care in patients with advanced pancreatic cancer. J. Natl. Cancer Inst. 2015, 107, dju424. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. WHO Definition of Palliative Care. Available online: http://www.who.int/cancer/palliative/definition/en/ (accessed on 24 August 2021).
- Haun, M.W.; Estel, S.; Rucker, G.; Friederich, H.C.; Villalobos, M.; Thomas, M.; Hartmann, M. Early palliative care for adults with advanced cancer. Cochrane Database Syst. Rev. 2017, 6, CD011129. [Google Scholar] [CrossRef]
- Irwin, K.E.; Greer, J.A.; Khatib, J.; Temel, J.S.; Pirl, W.F. Early palliative care and metastatic non-small cell lung cancer. Chronic Respir. Dis. 2013, 10, 35–47. [Google Scholar] [CrossRef]
- Howie, L.; Peppercorn, J. Early palliative care in cancer treatment: Rationale, evidence and clinical implications. Ther. Adv. Med. Oncol. 2013, 5, 318–323. [Google Scholar] [CrossRef] [Green Version]
- Zimmermann, C.; Swami, N.; Krzyzanowska, M.; Hannon, B.; Leighl, N.; Oza, A.; Moore, M.; Rydall, A.; Rodin, G.; Tannock, I.; et al. Early palliative care for patients with advanced cancer: A cluster-randomised controlled trial. Lancet 2014, 383, 1721–1730. [Google Scholar] [CrossRef]
- Yoong, J.; Park, E.R.; Greer, J.A.; Jackson, V.A.; Gallagher, E.R.; Pirl, W.F.; Back, A.L.; Temel, J.S. Early palliative care in advanced lung cancer: A qualitative study. JAMA Intern. Med. 2013, 173, 283–290. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hui, D.; Kim, S.H.; Roquemore, J.; Dev, R.; Chisholm, G.; Bruera, E. Impact of timing and setting of palliative care referral on quality of end-of-life care in cancer patients. Cancer 2014, 120, 1743–1749. [Google Scholar] [CrossRef] [PubMed]
- Canadian Cancer Society. Right to Care: Palliative Care for All Canadians; Canadian Cancer Society: Toronto, ON, Canada, 2016; pp. 1–34. [Google Scholar]
- Khandelwal, N.; Brumback, L.C.; Halpern, S.D.; Coe, N.B.; Brumback, B.; Curtis, J.R. Evaluating the Economic Impact of Palliative and End-of-Life Care Interventions on Intensive Care Unit Utilization and Costs from the Hospital and Healthcare System Perspective. J. Palliat. Med. 2017, 20, 1314–1320. [Google Scholar] [CrossRef]
- Pilkey, J.; Downar, J.; Dudgeon, D.; Herx, L.; Oneschuk, D.; Schroder, C.; Schulz, V. Palliative Medicine—Becoming a Subspecialty of the Royal College of Physicians and Surgeons of Canada. J. Palliat. Care 2017, 32, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Clarke, E.A.; Marrett, L.D.; Kreiger, N. Cancer registration in Ontario: A computer approach. IARC Sci. Publ. 1991, 95, 246–257. [Google Scholar]
- Kralj, B. Measuring Rurality—RIO2008 BASIC: Methodology and Results. 2008. Available online: http://www.eriestclairlhin.on.ca/Page.aspx?id=11606 (accessed on 24 August 2021).
- Southern, D.A.; Quan, H.; Ghali, W.A. Comparison of the Elixhauser and Charlson/Deyo Methods of Comorbidity Measurement in Administrative Data. Med. Care 2004, 42, 355–360. [Google Scholar] [CrossRef]
- Parr, J.D.; Zhang, B.; Nilsson, M.E.; Wright, A.; Balboni, T.; Duthie, E.; Paulk, E.; Prigerson, H.G. The influence of age on the likelihood of receiving end-of-life care consistent with patient treatment preferences. J. Palliat. Med. 2010, 13, 719–726. [Google Scholar] [CrossRef] [Green Version]
- Verleye, L.; De Gendt, C.; Vrijens, F.; Schillemans, V.; Camberlin, C.; Silversmit, G.; Stordeur, S.; Van Eycken, E.; Dubois, C.; Robays, J.; et al. Patterns of care for non-small cell lung cancer patients in Belgium: A population-based study. Eur. J. Cancer Care 2018, 27, e12747. [Google Scholar] [CrossRef]
- Philip, J.; Hudson, P.; Bostanci, A.; Street, A.; Horey, D.E.; Aranda, S.; Zordan, R.; Rumbold, B.D.; Moore, G.; Sundararajan, V. Metastatic non-small cell lung cancer: A benchmark for quality end-of-life cancer care? Med. J. Aust. 2015, 202, 139–143. [Google Scholar] [CrossRef] [Green Version]
- Bylicki, O.; Rivière, F.; Tournier, C.; Canoui-Poitrine, F.; Grassin, F.; Margery, J.; Prodel, M.; Vainchtock, A.; Assié, J.B.; Chouaïd, C. Factors Associated with Aggressiveness of End-of-Life Care for Lung Cancer Patients and Associated Costs of Care. Clin. Lung Cancer 2021, 22, e320–e328. [Google Scholar] [CrossRef]
- Lehto, R.H.; Miller, S.E.L.; Flanigan, M.; Wyatt, G. Mental health in patients with advanced cancer at the end of life: Evaluation of evidence and future directions. Expert Rev. Qual. Life Cancer Care 2018, 3, 73–94. [Google Scholar] [CrossRef]
- Park, T.; Hegadoren, K.; Workun, B. Working at the Intersection of Palliative End-of-Life and Mental Health Care: Provider Perspectives. J. Palliat. Care 2020. [Google Scholar] [CrossRef]
- Rosenstein, D.L. Depression and end-of-life care for patients with cancer. Dialogues Clin. Neurosci. 2011, 13, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Vodermaier, A.; Linden, W.; MacKenzie, R.; Greig, D.; Marshall, C. Disease stage predicts post-diagnosis anxiety and depression only in some types of cancer. Br. J. Cancer 2011, 105, 1814–1817. [Google Scholar] [CrossRef] [PubMed]
- Lo, C.; Zimmermann, C.; Rydall, A.; Walsh, A.; Jones, J.M.; Moore, M.J.; Shepherd, F.A.; Gagliese, L.; Rodin, G. Longitudinal study of depressive symptoms in patients with metastatic gastrointestinal and lung cancer. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2010, 28, 3084–3089. [Google Scholar] [CrossRef] [PubMed]
- Kroschinsky, F.; Stölzel, F.; von Bonin, S.; Beutel, G.; Kochanek, M.; Kiehl, M.; Schellongowski, P.; on behalf of the Intensive Care in Hematological and Oncological Patients (iCHOP) Collaborative Group. New drugs, new toxicities: Severe side effects of modern targeted and immunotherapy of cancer and their management. Crit. Care 2017, 21, 89. [Google Scholar] [CrossRef] [Green Version]
- Louie, A.V.; Li, L.; Jenkyn, K.B.; Allen, B.; Rodrigues, G.B.; Warner, A.; Palma, D.A.; Shariff, S.Z. A population-based analysis of outcomes after radiotherapy in intensive care unit patients with lung cancer. J. Thorac. Dis. 2018, 10, 1440–1448. [Google Scholar] [CrossRef] [Green Version]
- Shokar, S.; Buldo, E.; Siu, L.L.; Hansen, A.R.; Spreafico, A.; Doi, J.; Carlsson, L.; Bedard, P.L. Patient knowledge, attitudes, and expectations of cancer immunotherapies. J. Clin. Oncol. 2018, 36, e18551. [Google Scholar] [CrossRef]
- Sharma, R.K.; Prigerson, H.G.; Penedo, F.J.; Maciejewski, P.K. Male-female patient differences in the association between end-of-life discussions and receipt of intensive care near death. Cancer 2015, 121, 2814–2820. [Google Scholar] [CrossRef] [Green Version]
- Earle, C.C.; Landrum, M.B.; Souza, J.M.; Neville, B.A.; Weeks, J.C.; Ayanian, J.Z. Aggressiveness of cancer care near the end of life: Is it a quality-of-care issue? J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2008, 26, 3860–3866. [Google Scholar] [CrossRef] [PubMed]
- Hales, S.; Chiu, A.; Husain, A.; Braun, M.; Rydall, A.; Gagliese, L.; Zimmermann, C.; Rodin, G. The Quality of Dying and Death in Cancer and Its Relationship to Palliative Care and Place of Death. J. Pain Symptom Manag. 2014, 48, 839–851. [Google Scholar] [CrossRef] [PubMed]
- Monier, P.A.; Chrusciel, J.; Ecarnot, F.; Bruera, E.; Sanchez, S.; Barbaret, C. Duration of palliative care involvement and cancer care aggressiveness near the end of life. BMJ Support. Palliat. Care 2020. [Google Scholar] [CrossRef] [PubMed]
- Colombet, I.; Bouleuc, C.; Piolot, A.; Vilfaillot, A.; Jaulmes, H.; Voisin-Saltiel, S.; Goldwasser, F.; Vinant, P. Multicentre analysis of intensity of care at the end-of-life in patients with advanced cancer, combining health administrative data with hospital records: Variations in practice call for routine quality evaluation. BMC Palliat. Care 2019, 18, 35. [Google Scholar] [CrossRef] [PubMed]
| All Patients (N = 37,203) | Palliative Treatment (Systemic Therapy, Radiotherapy, Metastasis Surgery) (N = 19,668) | Non-Palliative Treatment (N = 17,535) | ||||
|---|---|---|---|---|---|---|
| Characteristics | Frequency | Percent (%) | Frequency | Percent (%) | Frequency | Percent (%) |
| Socio-demographics | ||||||
| Age | ||||||
| 20–49 | 853 | 2.29 | 660 | 3.36 | 193 | 1.10 |
| 50–59 | 4382 | 11.78 | 3139 | 15.96 | 1243 | 7.09 |
| 60–69 | 9773 | 26.27 | 6299 | 32.03 | 3474 | 19.81 |
| 70–79 | 12,337 | 33.16 | 6480 | 32.95 | 5857 | 33.40 |
| 80+ | 9858 | 26.50 | 3090 | 15.71 | 6768 | 38.60 |
| Sex | ||||||
| Male | 19,701 | 52.96 | 10,408 | 52.92 | 9293 | 53.00 |
| Female | 17,502 | 47.04 | 9260 | 47.08 | 8242 | 47.00 |
| Neighborhood income quintile at death date | ||||||
| Missing | 121 | 0.33 | 52 | 0.26 | 69 | 0.39 |
| 1 (Lowest) | 9277 | 24.94 | 4625 | 23.52 | 4652 | 26.53 |
| 2 | 8306 | 22.33 | 4360 | 22.17 | 3946 | 22.50 |
| 3 | 7286 | 19.58 | 3921 | 19.94 | 3365 | 19.19 |
| 4 | 6485 | 17.43 | 3540 | 18.00 | 2945 | 16.79 |
| 5 (Highest) | 5728 | 15.40 | 3170 | 16.12 | 2558 | 14.59 |
| Place of residence (LHIN) at death date | ||||||
| Erie St. Clair | 2329 | 6.26 | 1216 | 6.18 | 1113 | 6.35 |
| South West | 3021 | 8.12 | 1517 | 7.71 | 1504 | 8.58 |
| Waterloo Wellington | 1912 | 5.14 | 1019 | 5.18 | 893 | 5.09 |
| Hamilton Niagara Halimand Brant | 4902 | 13.18 | 2363 | 12.01 | 2539 | 14.48 |
| Central West | 1356 | 3.64 | 770 | 3.91 | 586 | 3.34 |
| Mississauga Halton | 2081 | 5.59 | 1157 | 5.88 | 924 | 5.27 |
| Toronto Central | 2547 | 6.85 | 1406 | 7.15 | 1141 | 6.51 |
| Central | 3251 | 8.74 | 1857 | 9.44 | 1394 | 7.95 |
| Central East | 4563 | 12.27 | 2341 | 11.90 | 2222 | 12.67 |
| South East | 2219 | 5.96 | 1220 | 6.20 | 999 | 5.70 |
| Champlain | 3764 | 10.12 | 2138 | 10.87 | 1626 | 9.27 |
| North Simcoe Muskoka | 1669 | 4.49 | 785 | 3.99 | 884 | 5.04 |
| North East | 2711 | 7.29 | 1468 | 7.46 | 1243 | 7.09 |
| North West | 878 | 2.36 | 411 | 2.09 | 467 | 2.66 |
| Rurality status at death date | ||||||
| Missing | 26 | 0.07 | 10 | 0.05 | 16 | 0.09 |
| Yes | 5850 | 15.72 | 2906 | 14.78 | 2944 | 16.79 |
| No | 31,327 | 84.21 | 16,752 | 85.17 | 14,575 | 83.12 |
| Type of environment at death date | ||||||
| NA/Missing | 429 | 1.15 | 208 | 1.06 | 221 | 1.26 |
| Urban (RIO < 10) | 22,948 | 61.68 | 12,543 | 63.77 | 10,405 | 59.34 |
| Suburban (10 ≤ RIO < 40) | 9531 | 25.62 | 4839 | 24.60 | 4692 | 26.76 |
| Rural (40 ≤ RIO) | 4295 | 11.54 | 2078 | 10.57 | 2217 | 12.64 |
| General health characteristics | ||||||
| Chronic comorbidities prior to death | ||||||
| Asthma | 6445 | 17.32 | 3172 | 16.13 | 3273 | 18.67 |
| Chronic obstructive pulmonary disease | 22,152 | 59.54 | 10,801 | 54.92 | 11,351 | 64.73 |
| Congestive heart failure | 6627 | 17.81 | 2482 | 12.62 | 4145 | 23.64 |
| Elixhauser comorbidity index * | ||||||
| 0–1 | 18,373 | 49.39 | 10,776 | 54.79 | 7597 | 43.32 |
| 2–3 | 11,854 | 31.86 | 6000 | 30.51 | 5854 | 33.38 |
| 4+ | 6976 | 18.75 | 2892 | 14.70 | 4084 | 23.29 |
| Disease and treatment characteristics | ||||||
| Best stage of first cancer diagnosis | ||||||
| Missing | 4909 | 13.20 | 962 | 4.89 | 3947 | 22.51 |
| 0/I | 2866 | 7.70 | 1153 | 5.86 | 1713 | 9.77 |
| II | 1877 | 5.05 | 933 | 4.74 | 944 | 5.38 |
| III | 7090 | 19.06 | 4065 | 20.67 | 3025 | 17.25 |
| IV | 20,405 | 54.85 | 12,517 | 63.64 | 7888 | 44.98 |
| Multiple primaries | 56 | 0.15 | 38 | 0.19 | 18 | 0.10 |
| Number of months from first cancer diagnosis to death | ||||||
| 0–<1 | 5692 | 15.30 | 582 | 2.96 | 5110 | 29.14 |
| 1–<2 | 4382 | 11.78 | 1765 | 8.97 | 2617 | 14.92 |
| 2–<3 | 3245 | 8.72 | 1783 | 9.07 | 1462 | 8.34 |
| 3–<6 | 5769 | 15.51 | 3711 | 18.87 | 2058 | 11.74 |
| 6–<12 | 5854 | 15.74 | 4053 | 20.61 | 1801 | 10.27 |
| 12+ | 12,261 | 32.96 | 7774 | 39.53 | 4487 | 25.59 |
| Number of months from first cancer diagnosis to palliative intent treatment | ||||||
| No treatment | 17,535 | 47.13 | 0 | 0.00 | 17,535 | 100 |
| 0–<1 | 6777 | 18.22 | 6777 | 34.46 | 0 | 0.00 |
| 1–<2 | 4809 | 12.93 | 4809 | 24.45 | 0 | 0.00 |
| 2–<3 | 1819 | 4.89 | 1819 | 9.25 | 0 | 0.00 |
| 3–<6 | 1601 | 4.30 | 1601 | 8.14 | 0 | 0.00 |
| 6–<12 | 1460 | 3.92 | 1460 | 7.42 | 0 | 0.00 |
| 12+ | 3202 | 8.61 | 3202 | 16.28 | 0 | 0.00 |
| Prior adjuvant systemic therapy or concurrent chemoradiation | ||||||
| Prior to death date | 2845 | 7.65 | 1833 | 9.32 | 1012 | 5.77 |
| All Patients N = 37,203 | Palliative Intent Treatment N = 19,668 | No Palliative Intent Treatment N = 17,535 | p-Value | ||||
|---|---|---|---|---|---|---|---|
| Outcome | Frequency | Percent (%) | Frequency | Percent (%) | Frequency | Percent (%) | |
| Aggressive care * | 18,692 | 50.26 | 8962 | 45.58 | 9730 | 55.51 | <0.001 |
| Aggressive care £ | 7833 | 21.81 | 3937 | 20.59 | 3896 | 23.20 | <0.001 |
| Supportive care ** | 20,515 | 60.30 | 13,139 | 70.30 | 7376 | 48.11 | <0.001 |
| Individual indicators of aggressive care | |||||||
| >1 Emergency department visit **** | 1372 | 3.84 | 773 | 4.05 | 599 | 3.59 | 0.025 |
| >1 Hospital inpatient admission **** | 3174 | 8.88 | 1524 | 7.99 | 1650 | 9.90 | <0.001 |
| ICU admission **** | 3556 | 9.56 | 1311 | 6.67 | 2245 | 12.80 | <0.001 |
| Death in hospital | 16,756 | 45.04 | 7731 | 39.31 | 9025 | 51.47 | <0.001 |
| Palliative systemic therapy *** | 1056 | 2.84 | 1056 | 5.37 | 0 | 0.00 | <0.001 |
| Individual indicators of supportive care | |||||||
| Palliative nursing or PSW home visit ***** | 19,385 | 52.15 | 12,562 | 63.89 | 6823 | 38.97 | <0.001 |
| Physician home visit *** | 9070 | 27.82 | 5686 | 32.05 | 3384 | 22.77 | <0.001 |
| Other | |||||||
| Mental health symptoms **** | 2786 | 7.49 | 1427 | 7.26 | 1359 | 7.75 | 0.070 |
| Number of days from first access to palliative care consultation ¥ to death | |||||||
| >180 | 2703 | 7.27 | 2086 | 10.61 | 617 | 3.52 | <0.001 |
| 61–180 | 4000 | 10.75 | 2897 | 14.73 | 1103 | 6.29 | |
| 31–60 | 2930 | 7.88 | 1975 | 10.04 | 955 | 5.45 | |
| ≤30 | 6725 | 18.08 | 3481 | 17.70 | 3244 | 18.50 | |
| None | 20,845 | 56.03 | 9229 | 46.92 | 11,616 | 66.24 | |
| Characteristics | Aggressive Care | Supportive Care | ||||
|---|---|---|---|---|---|---|
| Yes | No | Adjusted Stepwise Model | Yes | No | Adjusted Stepwise Model | |
| N = 18,692 (%) | N = 18,499 (%) | Odds Ratio (95% CI) | N = 20,515 (%) | N = 13,507 (%) | Odds Ratio (95% CI) | |
| Socio-demographics | ||||||
| Death year * | ||||||
| Mean ± SD | 2012.56 ± 2.56 | 2012.95 ± 2.54 | 0.96 (0.95–0.97) | 2012.97 ± 2.55 | 2012.53 ± 2.53 | 1.03 (1.02–1.04) |
| Age at death date | ||||||
| 20–49 | 523 (2.80) | 330 (1.78) | Reference | 514 (2.51) | 274 (2.03) | |
| 50–59 | 2392 (12.80) | 1990 (10.76) | 0.69 (0.59–0.81) | 2695 (13.14) | 1382 (10.23) | |
| 60–69 | 5192 (27.78) | 4576 (24.74) | 0.56 (0.48–0.66) | 5656 (27.57) | 3366 (24.92) | |
| 70–79 | 6217 (33.26) | 6114 (33.05) | 0.45 (0.39–0.53) | 6797 (33.13) | 4408 (32.63) | |
| 80+ | 4368 (23.37) | 5489 (29.67) | 0.31 (0.27–0.36) | 4853 (23.66) | 4077 (30.18) | |
| Sex | ||||||
| Female | 8218 (43.97) | 9277 (50.15) | Reference | 9961 (48.55) | 6164 (45.64) | Reference |
| Male | 10,474 (56.03) | 9222 (49.85) | 1.21 (1.16–1.26) | 10,554 (51.45) | 7343 (54.36) | 0.95 (0.91–1.00) |
| Neighborhood income quintile at death date | ||||||
| 1 Lowest | 4747 (25.40) | 4528 (24.48) | 4820 (23.50) | 3645 (26.99) | Reference | |
| 2 | 4227 (22.61) | 4079 (22.05) | 4583 (22.34) | 3007 (22.26) | 1.13 (1.06–1.22) | |
| 3 | 3658 (19.57) | 3623 (19.58) | 4105 (20.01) | 2580 (19.10) | 1.15 (1.07–1.23) | |
| 4 | 3214 (17.19) | 3268 (17.67) | 3673 (17.90) | 2246 (16.63) | 1.19 (1.11–1.29) | |
| 5 Highest | 2781 (14.88) | 2945 (15.92) | 3284 (16.01) | 1973 (14.61) | 1.18 (1.09–1.27) | |
| Place of residence at death date | ||||||
| Erie St. Clair | 1012 (5.41) | 1316 (7.11) | 0.60 (0.53–0.69) | 1469 (7.16) | 732 (5.42) | 2.09 (1.81–2.41) |
| South West | 1660 (8.88) | 1360 (7.35) | 0.97 (0.86–1.09) | 1605 (7.82) | 1124 (8.32) | 1.41 (1.24–1.61) |
| Waterloo Wellington | 784 (4.19) | 1128 (6.10) | 0.71 (0.62–0.80) | 1372 (6.69) | 465 (3.44) | 2.86 (2.47–3.32) |
| Hamilton Niagara Halimand Brant | 2105 (11.26) | 2797 (15.12) | 0.68 (0.61–0.76) | 2870 (13.99) | 1698 (12.57) | 1.92 (1.71–2.15) |
| Central West | 824 (4.41) | 532 (2.88) | 1.57 (1.36–1.80) | 697 (3.40) | 492 (3.64) | 1.35 (1.15–1.58) |
| Mississauga Halton | 1045 (5.59) | 1036 (5.60) | 1.15 (1.01–1.29) | 1213 (5.91) | 675 (5.00) | 1.68 (1.46–1.93) |
| Toronto Central | 1210 (6.47) | 1337 (7.23) | Reference | 1251 (6.10) | 1040 (7.70) | Reference |
| Central | 1591 (8.51) | 1660 (8.97) | 1.09 (0.98–1.22) | 1577 (7.69) | 1325 (9.81) | 0.87 (0.77–0.98) |
| Central East | 2709 (14.49) | 1854 (10.02) | 1.46 (1.31–1.62) | 2326 (11.34) | 1778 (13.16) | 1.11 (0.99–1.25) |
| South East | 1143 (6.11) | 1075 (5.81) | 0.82 (0.72–0.94) | 980 (4.78) | 1074 (7.95) | 0.88 (0.77–1.01) |
| Champlain | 1714 (9.17) | 2047 (11.07) | 0.70 (0.63–0.78) | 2237 (10.90) | 1268 (9.39) | 1.78 (1.57–2.01) |
| North Simcoe Muskoka | 830 (4.44) | 839 (4.54) | 0.73 (0.64–0.84) | 1036 (5.05) | 535 (3.96) | 2.13 (1.82–2.48) |
| North East | 1599 (8.55) | 1107 (5.98) | 1.02 (0.90–1.15) | 1539 (7.50) | 879 (6.51) | 1.99 (1.73–2.28) |
| North West | 466 (2.49) | 411 (2.22) | 0.91 (0.76–1.08) | 343 (1.67) | 422 (3.12) | 0.66 (0.55–0.80) |
| Rurality status at death date | ||||||
| Yes | 3524 (18.85) | 2322 (12.55) | 1.09 (1.00–1.20) | 3089 (15.06) | 2166 (16.04) | 0.94 (0.88–1.00) |
| Type of environment at death date | ||||||
| Urban (RIO < 10) | 10,737 (57.44) | 12,209 (66.00) | 0.59 (0.53–0.66) | 12,620 (61.52) | 8397 (62.17) | 0.82 (0.75–0.89) |
| Suburban (10 ≤ RIO < 40) | 4990 (26.70) | 4536 (24.52) | 0.73 (0.66–0.81) | 5434 (26.49) | 3373 (24.97) | 1.00 (0.92–1.10) |
| Rural (40 ≤ RIO) | 2711 (14.50) | 1580 (8.54) | Reference | 2250 (10.97) | 1563 (11.57) | Reference |
| General health characteristics | ||||||
| Chronic comorbidities prior to death | ||||||
| Asthma | 3283 (17.56) | 3156 (17.06) | 3464 (16.89) | 2399 (17.76) | ||
| Chronic obstructive pulmonary disease | 11,397 (60.97) | 10,743 (58.07) | 1.05 (1.00–1.10) | 11,889 (57.95) | 8326 (61.64) | 0.96 (0.91–1.01) |
| Congestive heart failure | 3643 (19.49) | 2984 (16.13) | 1.12 (1.05–1.19) | 3084 (15.03) | 2795 (20.69) | 0.88 (0.82–0.94) |
| Elixhauser comorbidity index ** | ||||||
| 0–1 | 8389 (44.88) | 9982 (53.96) | Reference | 11,086 (54.04) | 6106 (45.21) | Reference |
| 2–3 | 6371 (34.08) | 5478 (29.61) | 1.46 (1.39–1.54) | 6149 (29.97) | 4547 (33.66) | 0.76 (0.72–0.81) |
| 4+ | 3932 (21.04) | 3039 (16.43) | 1.66 (1.55–1.77) | 3280 (15.99) | 2854 (21.13) | 0.68 (0.64–0.74) |
| Disease and treatment characteristics | ||||||
| Number of months from first cancer diagnosis to death | ||||||
| 0–<1 | 4100 (21.93) | 1592 (8.61) | Reference | 1233 (6.01) | 3618 (26.79) | Reference |
| 1–<2 | 2216 (11.86) | 2164 (11.70) | 0.41 (0.37–0.45) | 1988 (9.69) | 1824 (13.50) | 2.59 (2.35–2.85) |
| 2–<3 | 1512 (8.09) | 1731 (9.36) | 0.39 (0.35–0.42) | 1878 (9.15) | 1068 (7.91) | 3.69 (3.31–4.10) |
| 3–<6 | 2617 (14.00) | 3150 (17.03) | 0.38 (0.35–0.42) | 3754 (18.30) | 1638 (12.13) | 4.37 (3.97–4.81) |
| 6–<12 | 2700 (14.44) | 3153 (17.04) | 0.39 (0.36–0.43) | 3977 (19.39) | 1556 (11.52) | 4.75 (4.31–5.23) |
| 12+ | 5547 (29.68) | 6709 (36.27) | 0.37 (0.35–0.41) | 7685 (37.46) | 3803 (28.16) | 4.04 (3.71–4.41) |
| Prior adjuvant systemic therapy for thoracic tumour resection or curative concurrent chemoradiation | ||||||
| Prior to death date | 1463 (7.83) | 1382 (7.47) | 1.18 (1.08–1.28) | 1752 (8.54) | 905 (6.70) | 0.83 (0.76–0.92) |
| Palliative intent systemic therapy, radiotherapy and metastasis surgery | ||||||
| Prior to death date | 8962 (47.95) | 10,700 (57.84) | 0.87 (0.83–0.92) | 13,139 (64.05) | 5551 (41.10) | 1.49 (1.41–1.57) |
| Number of days from first access to palliative care consultation *** to death | ||||||
| >180 | 983 (5.26) | 1719 (9.29) | 0.56 (0.51–0.62) | 2165 (10.55) | 467 (3.46) | 3.46 (3.09–3.88) |
| 61–180 | 1334 (7.14) | 2665 (14.41) | 0.49 (0.46–0.53) | 3189 (15.54) | 674 (4.99) | 3.41 (3.10–3.76) |
| 31–60 | 1024 (5.48) | 1906 (10.30) | 0.53 (0.49–0.58) | 2121 (10.34) | 625 (4.63) | 2.75 (2.49–3.04) |
| ≤30 | 3764 (20.14) | 2959 (16.00) | 1.06 (0.99–1.12) | 3454 (16.84) | 2510 (18.58) | 1.55 (1.45–1.66) |
| None | 11,587 (61.99) | 9250 (50.00) | Reference | 9586 (46.73) | 9231 (68.34) | Reference |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goldie, C.L.; Nguyen, P.; Robinson, A.G.; Goldie, C.E.; Kircher, C.E.; Hanna, T.P. Quality of End-of-Life Care for People with Advanced Non-Small Cell Lung Cancer in Ontario: A Population-Based Study. Curr. Oncol. 2021, 28, 3297-3315. https://doi.org/10.3390/curroncol28050286
Goldie CL, Nguyen P, Robinson AG, Goldie CE, Kircher CE, Hanna TP. Quality of End-of-Life Care for People with Advanced Non-Small Cell Lung Cancer in Ontario: A Population-Based Study. Current Oncology. 2021; 28(5):3297-3315. https://doi.org/10.3390/curroncol28050286
Chicago/Turabian StyleGoldie, Catherine L., Paul Nguyen, Andrew G. Robinson, Craig E. Goldie, Colleen E. Kircher, and Timothy P. Hanna. 2021. "Quality of End-of-Life Care for People with Advanced Non-Small Cell Lung Cancer in Ontario: A Population-Based Study" Current Oncology 28, no. 5: 3297-3315. https://doi.org/10.3390/curroncol28050286
APA StyleGoldie, C. L., Nguyen, P., Robinson, A. G., Goldie, C. E., Kircher, C. E., & Hanna, T. P. (2021). Quality of End-of-Life Care for People with Advanced Non-Small Cell Lung Cancer in Ontario: A Population-Based Study. Current Oncology, 28(5), 3297-3315. https://doi.org/10.3390/curroncol28050286






