Evaluating the Impact of the COVID-19 Pandemic on New Cancer Diagnoses and Oncology Care in Manitoba
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Study Design and Population
2.3. Data Sources
2.4. Outcomes
2.5. Statistical Analysis
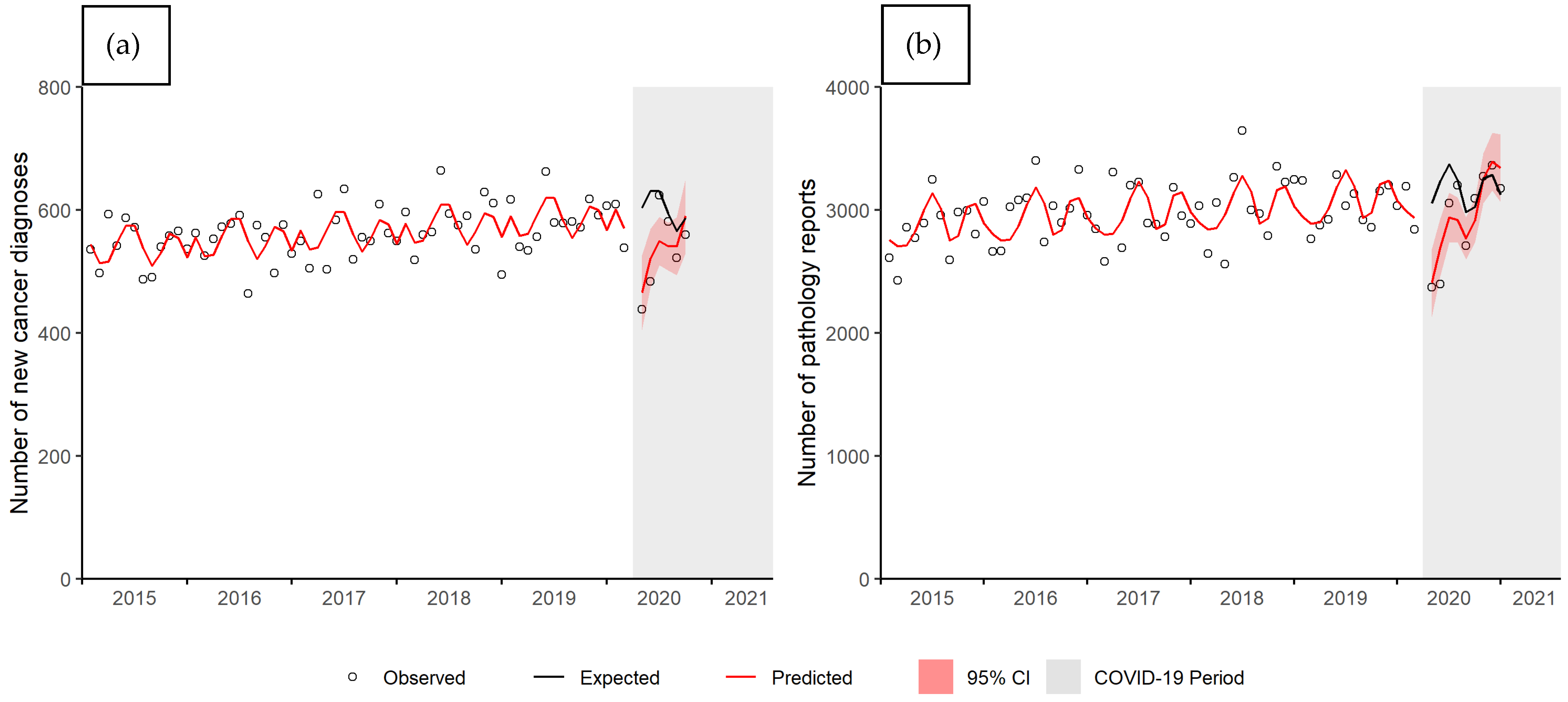
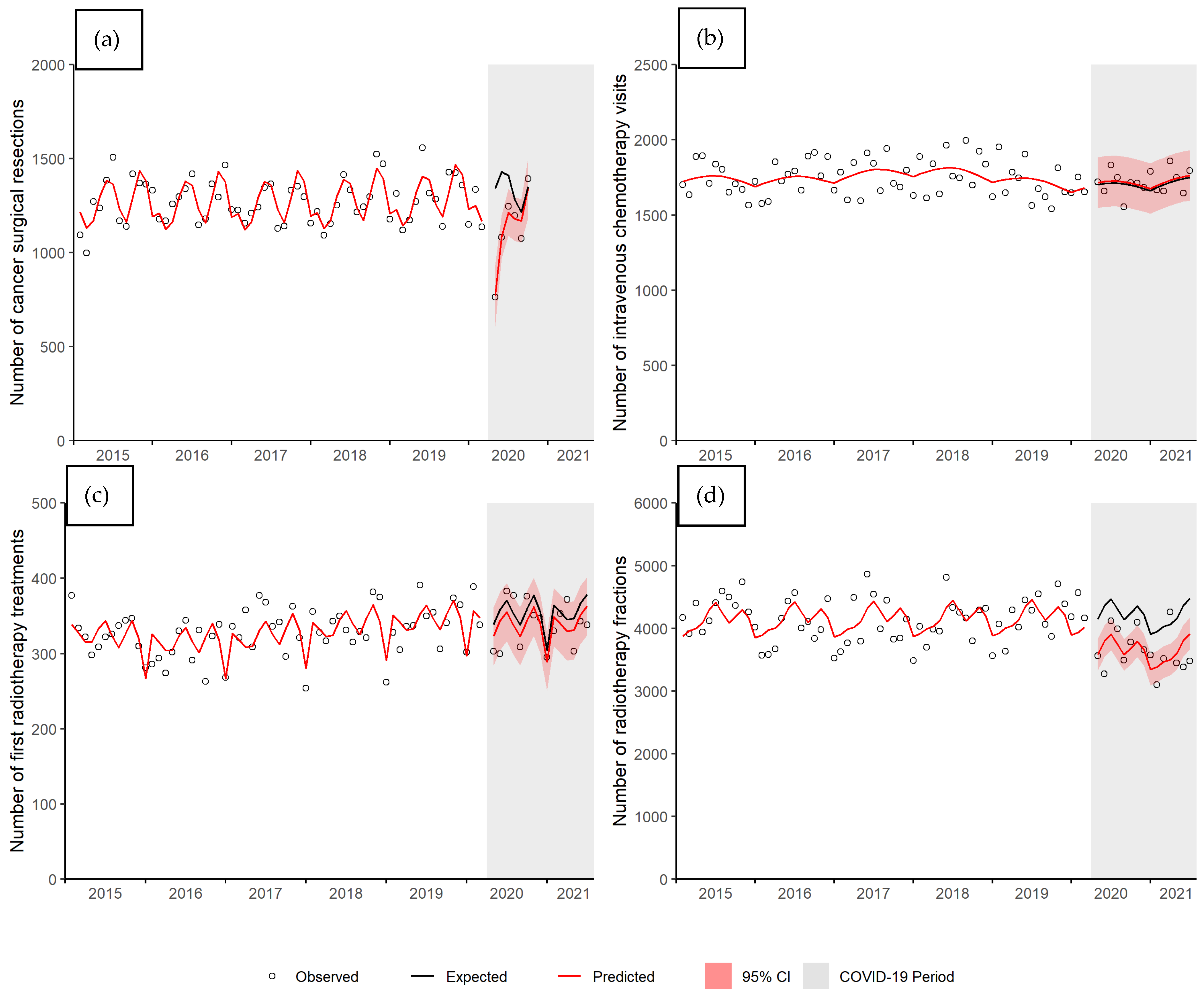
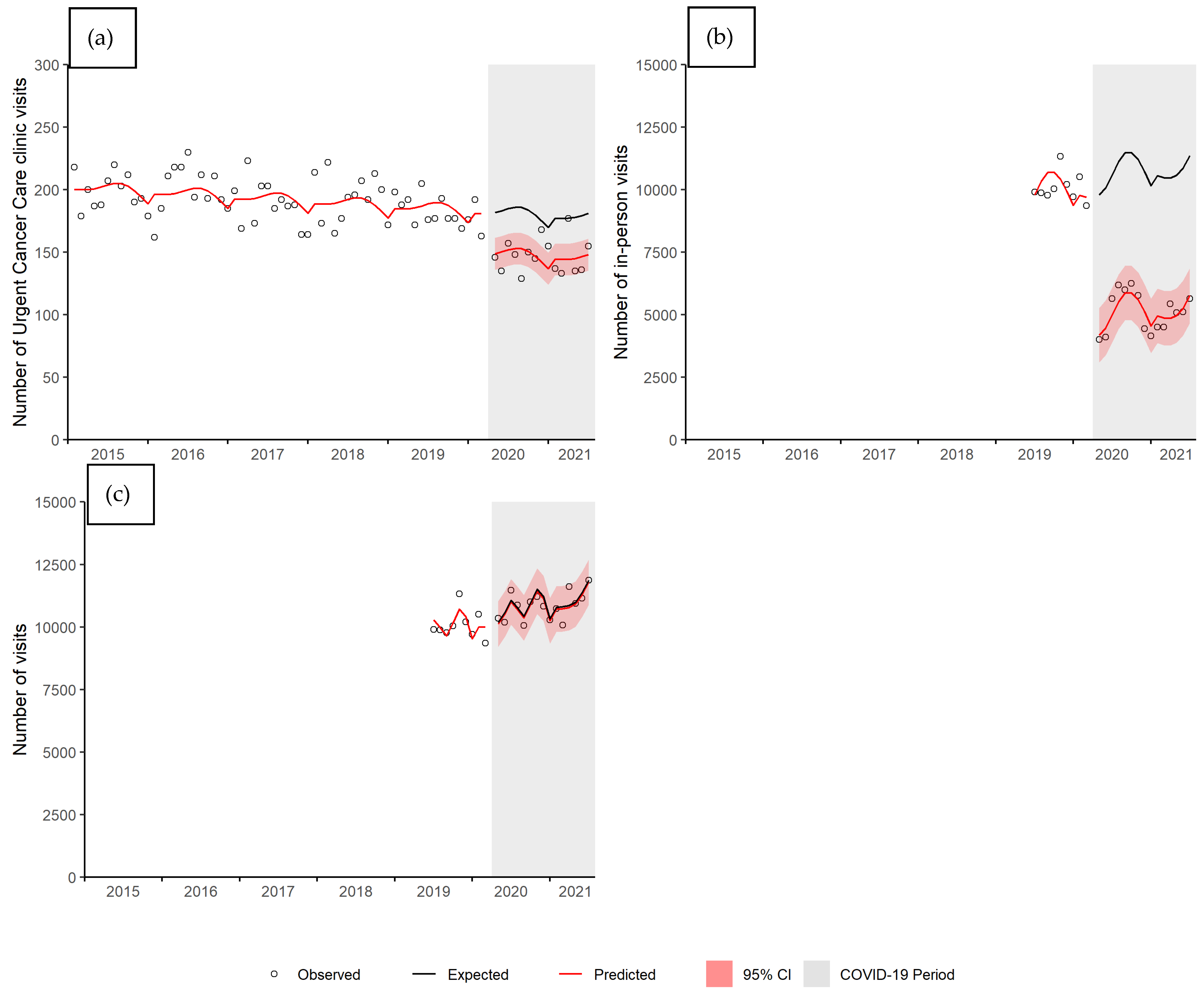
3. Results
4. Discussion
4.1. Main Findings
4.2. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liang, W.; Guan, W.; Chen, R.; Wang, W.; Li, J.; Xu, K.; Li, C.; Ai, Q.; Lu, W.; Liang, H.; et al. Cancer patients in SARS-CoV-2 infection: A nationwhide analysis in China. Lancet Oncol. 2020, 21, 335–337. [Google Scholar] [CrossRef]
- Dai, M.; Liu, D.; Liu, M.; Zhou, F.; Li, G.; Chen, Z.; Zhang, Z.; You, H.; Wu, M.; Zheng, Q.; et al. Patients with cancer appear more vulnerable to SARS-COV-2: A multi-centre study during the COVID-19 outbreak. Cancer Discov. 2020. [Google Scholar] [CrossRef] [PubMed]
- Williamson, E.; Walker, A.J.; Bhaskaran, K.; Bacon, S.; Bates, C.; Morton, C.E.; Curtis, H.J.; Mehrkar, A.; Evans, D.; Inglesby, P.; et al. OpenSAFELY: Factors associated with COVID-19 related hospital deaths in the linked electronic health records of 17 million adult NHS patients. medRxiv 2020. [Google Scholar] [CrossRef]
- Kuderer, N.M.; Chouveiir, T.K.; Shah, D.P.; Shyr, Y.; Rubinstein, S.M.; Rivera, D.R.; Shete, S.; Hsu, C.-Y.; Desai, A.; de Lima Lopes, G., Jr.; et al. Clinical impact of COVID-19 on patient with cancer (CC19): A cohort study. Lancet 2020, 395, 1907–1918. [Google Scholar] [CrossRef]
- Al-Shamsi, H.O.; Alhazzani, W.; Alhuraiji, A.; Coomes, E.A.; Chemaly, R.F.; Almuhanna, M.; Wolff, R.A.; Ibrahim, N.K.; Chua, M.L.; Hotte, S.J.; et al. A practical approach to the management of cancer patients during the novel Cononavirus Disease 2019 (COVID-10) pandemic: An International Collaborative Group. Oncologist 2020, 25, e936–e945. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rittberg, R.; Mann, A.; Desautels, D.; Earle, C.C.; Navaratnam, S.; Pitz, M. Canadian cancer centre response to COVID-19 pandemic: A national and provincial response. Curr. Oncol. 2020, 28, 233–251. [Google Scholar] [CrossRef] [PubMed]
- Jazieh, A.R.; Akbulat, H.; Curigliano, G.; Rogado, A.; Alsharm, A.A.; Razis, E.D.; Mula-Hussain, L.; Errihani, H.; Khattak, A.; De Guzman, R.B.; et al. Impact of the COVID-19 pandemic on cancer care: A global collaborative study. JCO Glob. Oncol. 2020, 6, 1428–1438. [Google Scholar] [CrossRef] [PubMed]
- Riera, R.; Bagattini, A.M.; Pacheco, R.L.; Pachito, D.V.; Roitberg, F.; Ibawi, A.I. Delays and distruptions in cancer health care due to COVID-19 pandemic: Systematic review. JCO Glob. Oncol. 2021, 7, 311–323. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Vahid, S.; Eberg, M.; Milroy, S.; Milkovich, J.; Wright, F.C.; Hunter, A.; Kalladeen, R.; Zanchetta, C.; Wijeysundera, H.C.; et al. Clearing the surgical backlog caused by COVID-19 in Ontario: A time series modelling study. CMAJ 2020, 192, E1347–E1356. [Google Scholar] [CrossRef] [PubMed]
- De Jonge, L.; Worthington, J.; van Wifferen, F.; Iragorri, N.; Peterse, E.F.P.; Lew, J.-B.; Greuter, M.J.E.; Smith, H.A.; Feletto, E.; Yong, J.H.E.; et al. Impact of the COVID-19 pandemic on faecal immunochemical test-based colorectal cancer screening programmes in Australia, Canada, and the Netherlands: A comparative modelling study. Lancet Gastroenterol. Hepatol. 2021, 6, 304–314. [Google Scholar] [CrossRef]
- Wong, L.E.; Hawkins, J.E.; Langness, S.; Murrell, K.L.; Iris, P.; Sammann, A. Where are all the patients? Addressing COVID-19 fear to encourage sick patients to seek emergency care. NEJM Catal. 2020, 1, 1–12. [Google Scholar]
- Jeffery, M.M.; D’Onofrio, G.; Paek, H.; Platts-Mills, T.F.; Soares, I.I.I.W.E.; Hoppe, J.A.; Genes, N.; Nath, B.; Melncik, E.R. Trends in emergency department visits and hospital admissions in health care systems in 5 States in the first month of the COVID-19 pandemic in the US. JAMA Intern. Med. 2020, 180, 1328–1333. [Google Scholar] [CrossRef] [PubMed]
- Rathod, S.; Dubey, A.; Chowdury, A.; Bashir, B.; Koul, R. A call for a radiation oncology model based on new 4Rs during the COVID-19 pandemic. Adv. Rad. Oncol. 2020, 5, 608–609. [Google Scholar] [CrossRef] [PubMed]
- Lopez Bernal, J.; Cummins, S.; Gasparrini, A. Interrupted time series regression for the evaluation of public health interventions: A tutorial. Int. J. Epidemiol. 2017, 46, 348–355. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Decker, K.; Lambert, P.; Galloway, K.; Bucher, O.; Pitz, M.; Goldenberg, B.; Singh, H.; Kristjanson, M.; Fatoye, T.; Bow, E.J. Predictors of Urgent Cancer Care Clinic and Emergency Department Visits for Individuals Diagnosed with Cancer. Curr. Oncol. 2021, 28, 1773–1778. [Google Scholar] [CrossRef] [PubMed]
- Generalized Linar Models. 4. A Model for Overdispersed Count Data. Available online: https://data.princeton.edu/wws509/r/overdispersion (accessed on 2 June 2021).
- DHARMa: Residual Diagnostics for Hierarchical (Multi-Level/Mixed) Regression Models. Available online: https://cran.r-project.org/web/packages/DHARMa/vignettes/DHARMa.html (accessed on 2 June 2021).
- Hanna, T.P.; King, W.D.; Thibodeau, S.; Jalink, M.; Paulin, G.A.; Harvey-Jones, E.; O’Sullivan, D.E.; Booth, C.M.; Sullivan, R.; Aggarwal, A. Mortality due to cancer treatment delay: Systematic review and meta-analysis. BMJ 2020, 371, m4087. [Google Scholar] [CrossRef] [PubMed]
- Overview: COVID-19’s Impact on Health Care Systems. Available online: https://cihi.ca/en/covid-19-resources/impact-of-covid-19-on-canada-health-care-systems/overview-covid-19s-impact-on (accessed on 26 July 2021).
- Rathod, S.; Dubey, A.; Bashir, B.; Sivananthan, G.; Leylek, A.; Chowdury, A.; Koul, R. Bracing for impact with new 4Rs in the COVID-19 pandemic—A provincial thoracic radiation oncology consensus. Radiother. Oncol. 2020, 19, 124–127. [Google Scholar] [CrossRef] [PubMed]
- Canadian Emergency Department Visits Drop by 25% in Early Weeks of COVID-19 Pandemic. Available online: cihi.ca/en/canadian-emergency-department-visits-drop-25-in-early-weeks-of-covid-19-pandemic (accessed on 2 June 2021).
- Glazier, R.H.; Green, M.E.; Wu, F.C.; Frymire, E.; Kopp, A.; Kiran, T. Shifts in office and virtual primary care during the early COVID-19 pandemic in Ontario, Canada. CMAJ 2021, 193, E200–E210. [Google Scholar] [CrossRef] [PubMed]
- Gomez, D.; Simpson, A.N.; Sue-Chue-Lam, C.; de Mestral, C.; Dossa, F.; Nantais, J.; Wilton, A.S.; Urbach, D.; Austin, P.C.; Baxter, N.N. A population-based analysis of the impact of the COVID-19 pandemic on common abdominal and gynecological emergency department visits. CMAJ 2021, 193, E753–E760. [Google Scholar] [CrossRef] [PubMed]
- Patzer, R.E.; Fayanju, O.M.; Kelz, R.R. Using health services research to address the unique challenges of the COVID-19 pandemic. JAMA Surg. 2021. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Decker, K.M.; Lambert, P.; Feely, A.; Bucher, O.; Kim, J.O.; Hebbard, P.; Thiessen, M.; Fatoye, T.; Pitz, M.; Koul, R.; et al. Evaluating the Impact of the COVID-19 Pandemic on New Cancer Diagnoses and Oncology Care in Manitoba. Curr. Oncol. 2021, 28, 3081-3090. https://doi.org/10.3390/curroncol28040269
Decker KM, Lambert P, Feely A, Bucher O, Kim JO, Hebbard P, Thiessen M, Fatoye T, Pitz M, Koul R, et al. Evaluating the Impact of the COVID-19 Pandemic on New Cancer Diagnoses and Oncology Care in Manitoba. Current Oncology. 2021; 28(4):3081-3090. https://doi.org/10.3390/curroncol28040269
Chicago/Turabian StyleDecker, Kathleen M., Pascal Lambert, Allison Feely, Oliver Bucher, Julian O. Kim, Pamela Hebbard, Maclean Thiessen, Tunji Fatoye, Marshall Pitz, Rashmi Koul, and et al. 2021. "Evaluating the Impact of the COVID-19 Pandemic on New Cancer Diagnoses and Oncology Care in Manitoba" Current Oncology 28, no. 4: 3081-3090. https://doi.org/10.3390/curroncol28040269
APA StyleDecker, K. M., Lambert, P., Feely, A., Bucher, O., Kim, J. O., Hebbard, P., Thiessen, M., Fatoye, T., Pitz, M., Koul, R., & Czaykowski, P. (2021). Evaluating the Impact of the COVID-19 Pandemic on New Cancer Diagnoses and Oncology Care in Manitoba. Current Oncology, 28(4), 3081-3090. https://doi.org/10.3390/curroncol28040269




