Results from a Theory-Guided Survey to Support Breast Cancer Trial Participation: Barriers, Enablers, and What to Do about them
Abstract
1. Introduction
2. Methods
2.1. Reporting and Ethics
2.2. Survey Development
2.3. Survey Content
2.4. Recruitment and Sample Frame
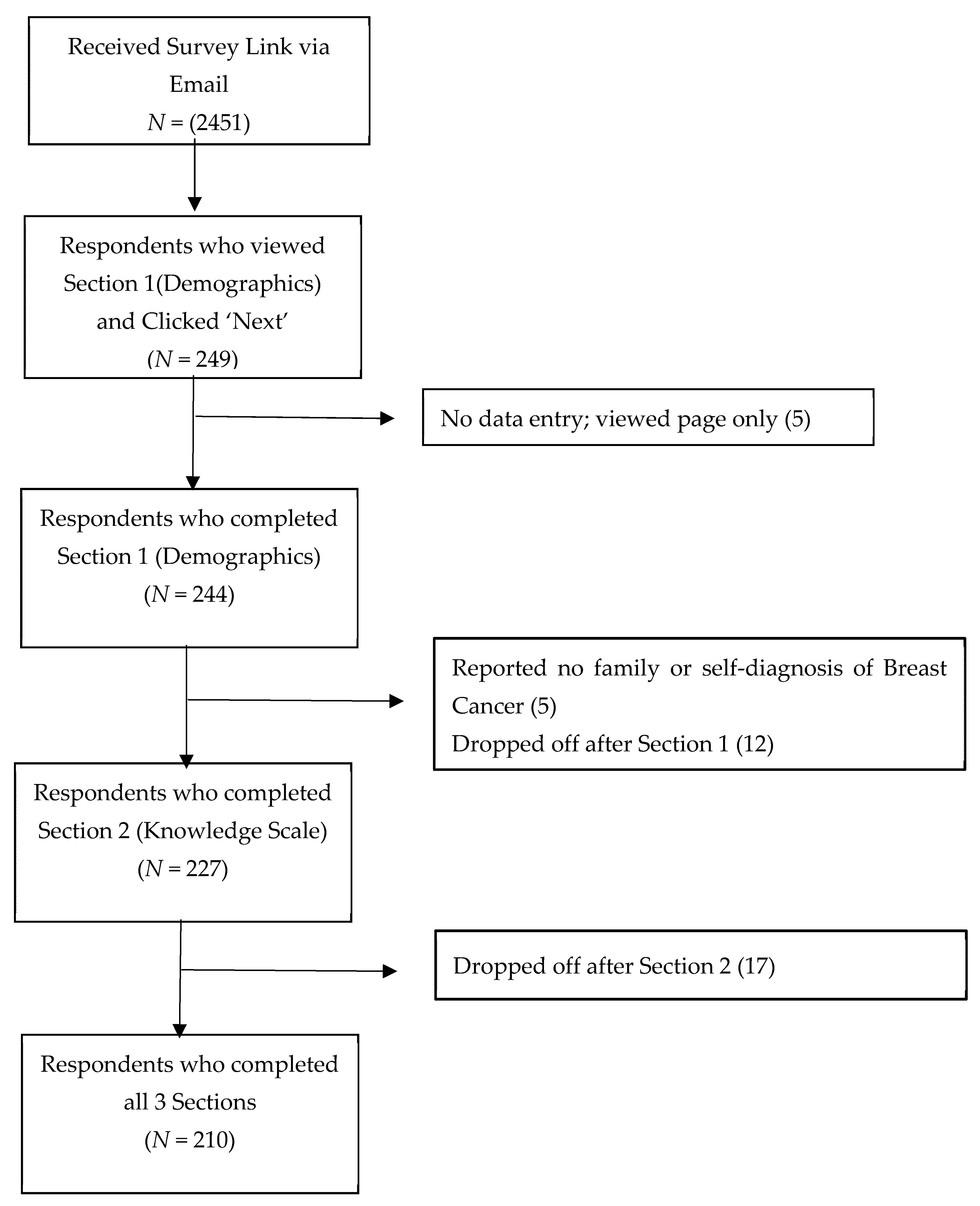
2.5. Survey Administration
2.6. Data Cleaning
2.7. Analysis
3. Results
4. Discussion
Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| TDF | Theoretical Domains Framework |
| CBCN | Canadian Breast Cancer Network |
| CTO | Clinical Trials Ontario |
| QuIC | Quality of Informed Consent |
References
- Galea, S.; Tracy, M. Participation rates in epidemiologic studies. Ann. Epidemiol. 2007, 17, 643–653. [Google Scholar] [CrossRef] [PubMed]
- Curtin, R.; Presser, S.; Singer, E. Changes in telephone survey nonresponse over the past quarter century. Public Opin. Q. 2005, 69, 87–98. [Google Scholar] [CrossRef]
- Scoggins, J.F.; Ramsey, S.D. A national cancer clinical trials system for the 21st century: Reinvigorating the NCI Cooperative Group Program. J. Natl. Cancer Inst. 2010, 102, 1371. [Google Scholar] [CrossRef] [PubMed]
- Treweek, S.; Pitkethly, M.; Cook, J.; Fraser, C.; Mitchell, E.; Sullivan, F.; Jackson, C.; Taskila, T.K.; Gardner, H. Strategies to improve recruitment to randomised trials. Cochrane Database Syst. Rev. 2018, 2, MR000013. [Google Scholar] [CrossRef] [PubMed]
- Lemieux, J.; Goodwin, P.J.; Pritchard, K.I.; Gelmon, K.A.; Bordeleau, L.J.; Duchesne, T.; Camden, S.; Speers, C.H. Identification of cancer care and protocol characteristics associated with recruitment in breast cancer clinical trials. J. Clin. Oncol. 2008, 26, 4458–4465. [Google Scholar] [CrossRef] [PubMed]
- Williams, R.J.; Tse, T.; DiPiazza, K.; Zarin, D.A. Terminated Trials in the ClinicalTrials.gov Results Database: Evaluation of Availability of Primary Outcome Data and Reasons for Termination. PLoS ONE 2015, 10, e0127242. [Google Scholar] [CrossRef] [PubMed]
- Frew, P.M.; Hou, S.I.; Davis, M.; Chan, K.; Horton, T.; Shuster, J.; Hixson, B.; del Rio, C. The likelihood of participation in clinical trials can be measured: The Clinical Research Involvement Scales. J. Clin. Epidemiol. 2010, 63, 1110–1117. [Google Scholar] [CrossRef]
- Walsh, E.; Sheridan, A. Factors affecting patient participation in clinical trials in Ireland: A narrative review. Contemp. Clin. Trials Commun. 2016, 3, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Spears, P. Patient barriers to participation in breast cancer clinical trials. Breast Cancer Manag. 2020, 9, BMT35. [Google Scholar] [CrossRef]
- Kaur, G.; Smyth, R.L.; Williamson, P. Developing a survey of barriers and facilitators to recruitment in randomized controlled trials. Trials 2012, 13, 218. [Google Scholar] [CrossRef]
- Kurt, A.; Semler, L.; Jacoby, J.; Johnson, M.; Careyva, B.; Stelb, B.; Friel, T.; Knouse, M.; Kincaid, H.; Smullian, J. Racial differences among factors assoicated with particpation in clinical research trials. J. Racial Ethnic Health Disparitites 2017, 4, 827–836. [Google Scholar] [CrossRef] [PubMed]
- Moorcraft, S.Y.; Marriott, C.; Peckitt, C.; Cunningham, D.; Chau, I.; Starling, N.; Watkins, D.; Rao, S. Patients’ willingness to participate in clinical trials and their views on aspects of cancer research: Results of a prospective patient survey. Trials 2016, 17, 17. [Google Scholar] [CrossRef] [PubMed]
- Gadegbeku, C.A.; Stillman, P.K.; Huffman, M.D.; Jackson, J.S.; Kusek, J.W.; Jamerson, K.A. Factors associated with enrollment of African Americans into a clinical trial: Results from the African American study of kidney disease and hypertension. Contemp. Clin. Trials 2008, 29, 837–842. [Google Scholar] [CrossRef]
- Lim, Y.; Lim, J.M.; Jeong, W.J.; Lee, K.H.; Keam, B.; Kim, T.Y.; Kim, T.M.; Han, S.W.; Oh, D.Y.; Kim, D.W.; et al. Korean Cancer Patients’ Awareness of Clinical Trials, Perceptions on the Benefit and Willingness to Participate. Cancer Res. Treat. Off. J. Korean Cancer Assoc. 2017, 49, 1033–1043. [Google Scholar] [CrossRef] [PubMed]
- Jones, C.W.; Braz, V.A.; McBride, S.M.; Roberts, B.W.; Platts-Mills, T.F. Cross-sectional assessment of patient attitudes towards participation in clinical trials: Does making results publicly available matter? BMJ Open 2016, 6, e013649. [Google Scholar] [CrossRef] [PubMed]
- Bergenmar, M.; Johansson, H.; Wilking, N. Levels of knowledge and perceived understanding among participants in cancer clinical trials—Factors related to the informed consent procedure. Clin. Trials 2011, 8, 77–84. [Google Scholar] [CrossRef]
- Michie, S.; Johnston, M.; Abraham, C.; Lawton, R.; Parker, D.; Walker, A.; Psychological Theory, G. Making psychological theory useful for implementing evidence based practice: A consensus approach. Qual. Saf. Health Care 2005, 14, 26–33. [Google Scholar] [CrossRef]
- Cane, J.; O’Connor, D.; Michie, S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement. Sci. 2012, 7, 37. [Google Scholar] [CrossRef]
- French, S.D.; Green, S.E.; O’Connor, D.A.; McKenzie, J.E.; Francis, J.J.; Michie, S.; Buchbinder, R.; Schattner, P.; Spike, N.; Grimshaw, J.M. Developing theory-informed behaviour change interventions to implement evidence into practice: A systematic approach using the Theoretical Domains Framework. Implement. Sci. 2012, 7, 38. [Google Scholar] [CrossRef]
- Brehaut, J.C.; Carroll, K.; Presseau, J.; Richards, D.P.; Gordon, J.; Benard, A.; Hudek, N.; Graham, I.D.; Fergusson, D.A.; Marlin, S. A patient-focused, theory-guided approach to survey design identified barriers to and drivers of clinical trial participation. J. Clin. Epidemiol. 2021, 132, 106–115. [Google Scholar] [CrossRef]
- Michie, S.; Johnston, M.; Francis, J.; Hardeman, W.; Eccles, M. From Theory to Intervention: Mapping Theoretically Derived Behavioural Determinants to Behaviour Change Techniques. Appl. Psychol. 2008, 57, 660–680. [Google Scholar] [CrossRef]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef] [PubMed]
- Eysenbach, G. Improving the quality of Web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e34. [Google Scholar] [CrossRef]
- Joffe, S.; Cook, E.F.; Cleary, P.D.; Clark, J.W.; Weeks, J.C. Quality of Informed Consent: A New Measure of Understanding Among Research Subjects. J. Natl. Cancer Inst. 2001, 93, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Dillman, D.A. Mail and Internet Surveys: The Tailored Design; John Wiley & Sons Inc.: New York, NY, USA, 2000. [Google Scholar]
- IBM SPSS Statistics. SPSS (Version 26). Available online: http://www.spss.com (accessed on 21 May 2021).
- Atkins, L.; Francis, J.; Islam, R.; O’Connor, D.; Patey, A.; Ivers, N.; Foy, R.; Duncan, E.M.; Colquhoun, H.; Grimshaw, J.M.; et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implement. Sci. 2017, 12, 77. [Google Scholar] [CrossRef] [PubMed]
| N | Percent | ||
|---|---|---|---|
| Gender | Male | 2 | 0.8% |
| Female | 238 | 97.5% | |
| Transgender/non-binary | 0 | 0% | |
| Prefer not to answer | 0 | 0% | |
| Missing | 4 | 1.6% | |
| Age | Range (31–84) | Mean (SD) 57.0 (11.5) | |
| Geographic location | Ontario | 100 | 41.0% |
| Western Canada | 68 | 27.9% | |
| Eastern Canada | 41 | 16.8% | |
| Quebec/Northern Canada | 33 | 13.5% | |
| Missing | 2 | 0.8% | |
| Education | Some high school | 4 | 1.6% |
| High school diploma | 13 | 5.3% | |
| Some university/college | 42 | 17.2% | |
| College diploma/BA degree | 122 | 50.0% | |
| Graduate degree | 30 | 12.3% | |
| Doctoral degree | 8 | 3.3% | |
| Professional degree | 12 | 4.8% | |
| Other | 2 | 0.8% | |
| Prefer not to answer | 2 | 0.8% | |
| Missing | 9 | 3.7% | |
| Household income | Less than $50,000 | 40 | 16.4% |
| $50,000 or more but less than $100,000 | 81 | 33.2% | |
| $100,000 or more but less than $150,000 | 26 | 10.7% | |
| $150,000 or more | 30 | 12.3% | |
| Prefer not to answer | 52 | 21.3% | |
| Missing | 15 | 6.1% | |
| Ethnicity | White/Caucasian | 223 | 91.4% |
| Asian | 3 | 1.2% | |
| South Asian | 3 | 1.2% | |
| Black | 2 | 0.8% | |
| Arab/West Asian | 0 | 0% | |
| First Nations/Indigenous | 4 | 1.6% | |
| Filipino | 0 | 0% | |
| Latin American | 1 | 0.4% | |
| Other (e.g., participant reported) | 5 | 2.0% | |
| Prefer not to answer | 3 | 1.2% | |
| Months in Canada previous year | 9 Plus months | 233 | 95.5% |
| 6–9 months | 3 | 1.2% | |
| Less than 3 months | 2 | 0.8% | |
| Prefer not to answer | 3 | 1.2% | |
| Missing | 3 | 1.2% | |
| Language spoken at home | English | 179 | 73.4% |
| French | 41 | 16.8% | |
| Other | 19 | 7.8% | |
| Missing | 5 | 2.0% | |
| Employment | Retired | 94 | 38.5% |
| Full-time employment | 66 | 27.0% | |
| Long-term disability | 37 | 15.2% | |
| Self employed | 20 | 8.2% | |
| Part-time employment | 19 | 7.8% | |
| Other | 24 | 9.8% | |
| Prefer not to answer | 6 | 2.5% | |
| Respondents with breast cancer | 225 | 92.2% | |
| Early stage | 104 | 46.2% | |
| Late stage | 91 | 40.4% | |
| Don’t know | 22 | 9.8% | |
| Missing/no response | 8 | 3.6% | |
| Respondents were family member with breast cancer | 14 | 5.7% | |
| Question | N (% Total) |
|---|---|
| Responded ‘no’ to being approached for research | 129 (54.0%) |
| Responded ‘yes’ to being approached for research | 97 (40.6%) |
| Responded ‘no’ to ever participating in research | 134 (56.1%) |
| Responded ‘yes’ to ever participating in research | 91 (38.1%) |
| What did participation involve? | |
| Clinical trial | 43 (47.3%) |
| Survey | 52 (57.1%) |
| Interview | 20 (22.0%) |
| Database study | 40 (44.0%) |
| Don’t know | 0 (0.0%) |
| Other | 12 (13.2%) |
| Confidence in clinical trial knowledge? | |
| Not at all confident | 13 (5.4%) |
| Not very confident | 24 (10.0%) |
| Somewhat confident | 115 (48.1%) |
| Completely confident | 83 (34.7%) |
| Missing | 4 (1.7%) |
| Responded ‘yes’ to having actively looked for a clinical trial | 65 (27.2%) |
| Searched online | 57 (87.7%) |
| Asked a health care provider | 37(56.9%) |
| Spoke to other patients | 16 (24.6%) |
| Other | 5 (7.7%) |
| Responded ‘yes’ to having help in search | 16 (24.6%) |
| Help from doctor | 6 (37.5%) |
| Help from other patients | 2 (12.5%) |
| Other help | 7 (43.8%) |
| Missing | 1 (6.3%) |
| Responded ‘yes’ to finding a study to participate in | 13 (20.0%) |
| Responded ‘yes’ to desire for search navigator | 53 (81.5%) |
| Statement | Perceived as Barrier | Perceived as Enabler | |||
|---|---|---|---|---|---|
| A Lot | A Little | No Effect | A Little | A Lot | |
| Social Influences | |||||
| If the investigators provided regular study updates | 1 (0.5%) | 0 (0%) | 10 (4.9%) | 89 (43.2%) | 106 (51.5%) |
| If my physician (s) thought I should participate | 0 (0%) | 0 (0%) | 13 (6.3%) | 76 (37.1%) | 116 (56.6%) |
| If there were helpful people on hand to help you make your participation decision | 0 (0%) | 2 (1.0%) | 17 (8.2%) | 96 (46.4%) | 92 (44.4%) |
| If my family thought I should participate | 0 (0%) | 1 (0.5%) | 39 (19.1) | 100 (49.0%) | 64 (31.4%) |
| If my physician was paid to recruit patients into the study | 122 (59.5%) | 41 (20.0%) | 38 (18.5%) | 3 (1.5%) | 1 (0.5%) |
| My feelings about whether the trial funders can be trusted | 23 (11.3%) | 31 (15.2%) | 46 (22.5%) | 46 (22.5%) | 58 (28.4%) |
| My worry that participation would mean that others would find out about my condition | 8 (3.9%) | 9 (4.4%) | 175 (85.4%) | 9 (4.4%) | 4 (2.0%) |
| Belief about Consequences | |||||
| My hope that participation will help me with my condition | 0 (0%) | 0 (0%) | 3 (1.5%) | 33 (16.1%) | 169 (82.4%) |
| My belief that participating would help others | 0 (0%) | 0 (0%) | 5 (2.5%) | 85 (41.9%) | 113 (55.7%) |
| My belief that participating would contribute to science | 0 (0%) | 0 (0%) | 13 (6.3%) | 104 (50.0%) | 91 (43.8%) |
| My belief that I would receive better care if I participated | 1 (0.5%) | 0 (0%) | 31 (14.9%) | 101 (48.6%) | 75 (36.1%) |
| If I had to stay longer in hospital | 40 (19.5%) | 78 (38.0%) | 78 (38.0%) | 5 (2.4%) | 4 (2.0%) |
| If I had to have more biopsies | 28 (13.8%) | 63 (31.0%) | 99 (48.8%) | 5 (2.5%) | 8 (3.9%) |
| If I had to have more blood tests | 9 (4.4%) | 32 (15.7%) | 147 (72.1%) | 9 (4.4%) | 7 (3.4%) |
| Belief about Capabilities | |||||
| If I think my cancer prognosis is poor | 13 (6.2%) | 6 (2.9%) | 17 (8.1%) | 52 (24.9%) | 121 (57.9%) |
| My belief that participating would give me a sense of control over what is happening to me | 0 (0%) | 4 (2.0%) | 28 (13.7%) | 86 (42.0%) | 87 (42.4%) |
| If I think my health is good (other than my cancer) | 15 (7.2%) | 16 (7.7%) | 55 (26.3%) | 74 (35.4%) | 49 (23.4%) |
| My feelings about the quality of my drug plan | 12 (5.9%) | 29 (14.1%) | 112 (54.6%) | 30 (14.6%) | 21 (10.2%) |
| Reinforcement | |||||
| If I received the results of the study once it was complete | 1 (0.5%) | 3 (1.5%) | 14 (6.9%) | 84 (41.4%) | 101 (49.8%) |
| If I would gain access to new study drugs | 1 (0.5%) | 4 (1.9%) | 17 (8.3%) | 77 (37.7%) | 105 (51.5%) |
| If the study reimbursed expenses | 1 (0.5%) | 0 (0%) | 38 (18.2%) | 94 (45.0%) | 76 (36.4%) |
| My experience with previous trials | 2 (1.0%) | 9 (4.4%) | 138 (67.3%) | 27 (13.2%) | 29 (14.1%) |
| Goals | |||||
| If I think participation would affect my social life/family commitments | 37 (18.0%) | 106 (51.7%) | 58 (28.3%) | 2 (1.0%) | 2 (1.0%) |
| My belief that participation would prevent me from my other activities | 39 (18.7%) | 98 (46.9%) | 65 (31.1%) | 4 (1.9%) | 3 (1.4%) |
| My belief that participation would interfere with other goals of mine | 36 (17.6%) | 102 (49.0%) | 64 (31.4%) | 2 (1.0%) | 2 (1.0%) |
| If I think participation would interfere with my childcare responsibilities | 33 (16.1%) | 42 (20.5%) | 129 (62.9%) | 1 (0.5%) | 0 (0%) |
| Environmental Context and Resources | |||||
| If there were patient-friendly decision-making tools to help you make your participation decision | 0 (0%) | 1 (0.5%) | 28 (13.4%) | 107 (51.2%) | 73 (34.9%) |
| If the study provided transportation to/from study appointments | 0 (0%) | 1 (0.5%) | 75 (35.9%) | 63 (30.1%) | 70 (33.5%) |
| If I think there is a substantial time commitment | 31 (14.9%) | 79 (38.0%) | 80 (38.5%) | 11 (5.3%) | 7 (3.4%) |
| My feelings about the quality of the health care system | 11 (5.4%) | 30 (14.7%) | 103 (50.5%) | 43 (21.1%) | 17 (8.3%) |
| Skills | |||||
| If I find the trial documents hard to understand | 64 (30.8%) | 87 (41.8%) | 48 (23.1%) | 6 (2.9%) | 3 (1.4%) |
| If the consent documents describe probabilities of side effects and numbers of patients affected by them | 17 (8.1%) | 76 (36.4) | 62 (29.7%) | 36 (17.2%) | 18 (8.6%) |
| Social/Professional Role and Identity | |||||
| My belief that participating would give me a sense of purpose | 1 (0.5%) | 1 (0.5%) | 48 (23.1%) | 96 (46.2%) | 62 (29.8%) |
| My belief that participation is part of my role as a good citizen | 8 (3.9%) | 4 (1.9%) | 68 (32.9%) | 77 (37.2%) | 50 (24.2%) |
| Knowledge | |||||
| My belief that I’d learn more about my condition if I participated | 0 (0%) | 1 (0.5%) | 24 (11.5%) | 104 (50.0%) | 79 (38.0%) |
| Optimism | |||||
| My hope that participation would help find a cure | 0 (0.0%) | 1 (0.5%) | 4 (2.0%) | 54 (26.3%) | 146 (71.2%) |
| Memory, Attention and Decision Processes | |||||
| If the investigators provided telephone reminders about study appointments | 1 (0.5%) | 3 (1.4%) | 100 (48.1%) | 71 (34.1%) | 33 (15.9%) |
| Emotion | |||||
| My worry about unknown side effects | 50 (24.0%) | 119 (57.2%) | 30 (14.4%) | 7 (3.4%) | 2 (1.0%) |
| Reported Research Experience | Comparison (p Value) | ||
|---|---|---|---|
| Yes | No | ||
| Confidence in clinical trial knowledge, N = 234 | 91 | 143 | χ2 (1) = 6.77 (p = 0.009) |
| Yes | 84 (92.3%) | 114 (79.7%) | |
| No | 7 (7.7%) | 29 (20.3%) | |
| Knowledge about clinical trials score, M (SD) | 9.8 (1.5) | 8.8 (2.0) | t (223) = −3.90 (p = 0.000) |
| My belief that participation is part of my role as a good citizen, N = 205 | 81 | 124 | χ2 (2) = 7.81 (p = 0.02) |
| Enabler to trial participation | 59 (72.8%) | 68 (54.8%) | |
| Barrier to trial participation | 5 (6.2%) | 7 (5.6%) | |
| No effect | 17 (21.0%) | 49 (39.5%) | |
| If there was patient-friendly decision-making tools to help you make your participation decision, N = 207 | 82 | 125 | χ2 (2) = 11.32 (p = 0.003) |
| Enabler to trial participation | 63 (76.8%) | 115 (92.0%) | |
| Barrier to trial participation | 0 (0%) | 1 (0.8%) | |
| No effect | 19 (23.2%) | 9 (7.2%) | |
| My experience with previous trials, N = 203 | 80 | 123 | χ2 (2) = 23.27 (p = 0.000) |
| Enabler to trial participation | 37 (46.3%) | 19 (15.4%) | |
| Barrier to trial participation | 4 (5.0%) | 7 (5.7%) | |
| No effect | 39 (48.8%) | 97 (78.9%) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brehaut, J.C.; Carroll, K.; Gordon, J.; Presseau, J.; Richards, D.P.; Fergusson, D.A.; Graham, I.D.; Marlin, S. Results from a Theory-Guided Survey to Support Breast Cancer Trial Participation: Barriers, Enablers, and What to Do about them. Curr. Oncol. 2021, 28, 2014-2028. https://doi.org/10.3390/curroncol28030187
Brehaut JC, Carroll K, Gordon J, Presseau J, Richards DP, Fergusson DA, Graham ID, Marlin S. Results from a Theory-Guided Survey to Support Breast Cancer Trial Participation: Barriers, Enablers, and What to Do about them. Current Oncology. 2021; 28(3):2014-2028. https://doi.org/10.3390/curroncol28030187
Chicago/Turabian StyleBrehaut, Jamie C., Kelly Carroll, Jenn Gordon, Justin Presseau, Dawn P. Richards, Dean A. Fergusson, Ian D. Graham, and Susan Marlin. 2021. "Results from a Theory-Guided Survey to Support Breast Cancer Trial Participation: Barriers, Enablers, and What to Do about them" Current Oncology 28, no. 3: 2014-2028. https://doi.org/10.3390/curroncol28030187
APA StyleBrehaut, J. C., Carroll, K., Gordon, J., Presseau, J., Richards, D. P., Fergusson, D. A., Graham, I. D., & Marlin, S. (2021). Results from a Theory-Guided Survey to Support Breast Cancer Trial Participation: Barriers, Enablers, and What to Do about them. Current Oncology, 28(3), 2014-2028. https://doi.org/10.3390/curroncol28030187





