Adenomesenteritis following SARS-CoV-2 Vaccination in Children: A Case Report and Review of The Literature
Abstract
:1. Introduction
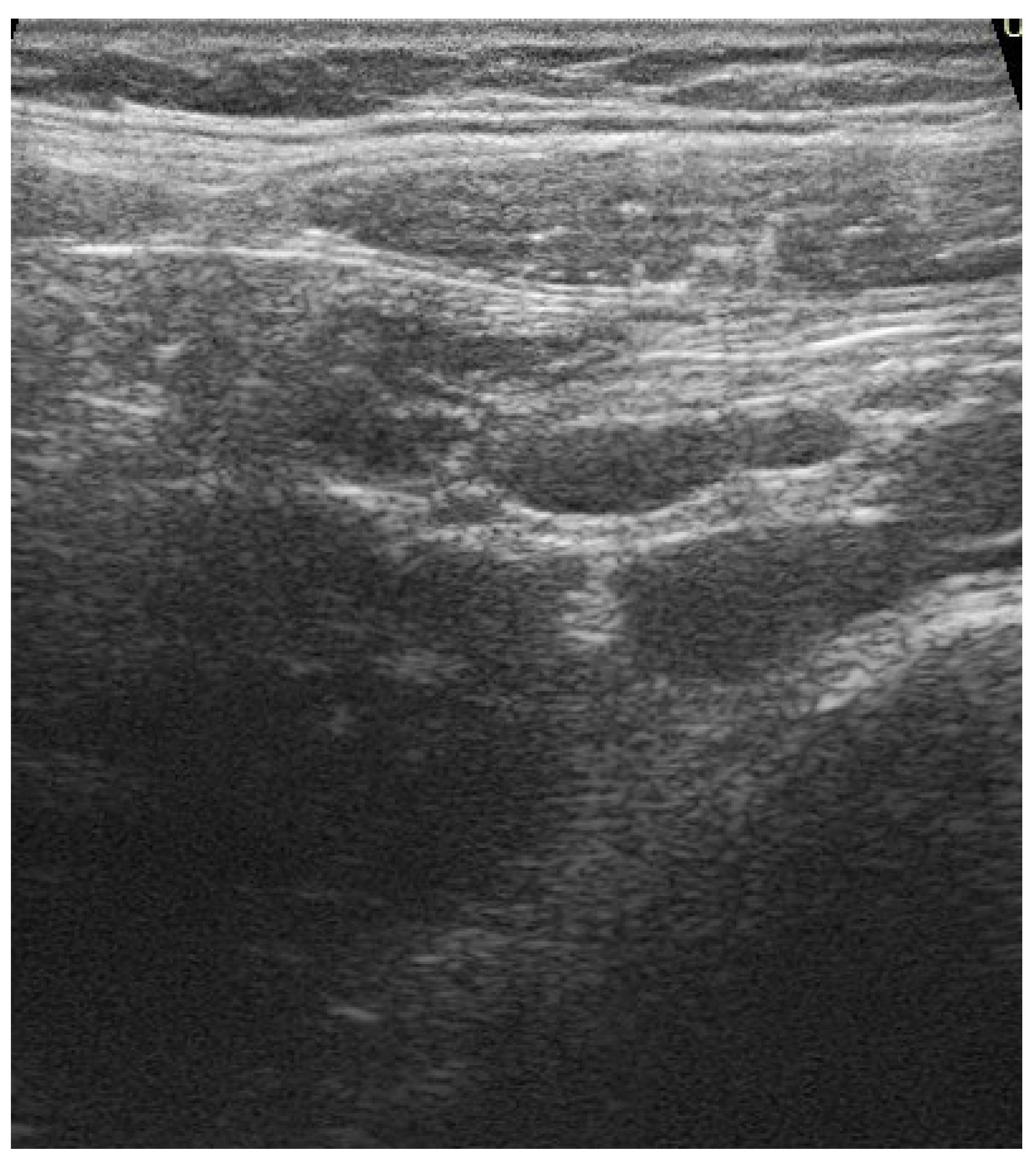
2. Case History
2.1. Differential Diagnosis, Investigations and Treatment
2.2. Outcome and Follow-Up
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Soleimanpour, S.; Yaghoubi, A. COVID-19 vaccine: Where are we now and where should we go? Expert Rev. Vaccines 2021, 20, 23–44. [Google Scholar] [CrossRef] [PubMed]
- Randolph, H.E.; Barreiro, L.B. Herd Immunity: Understanding COVID-19. Immunity 2020, 52, 737–741. [Google Scholar] [CrossRef]
- Murchu, O.E.; Byrne, P.; Walsh, K.A.; Carty, P.G.; Connolly, M.; De Gascun, C.; Jordan, K.; Keoghan, M.; O’Brien, K.K.; O’Neill, M.; et al. Immune response following infection with SARS-CoV-2 and other coronaviruses: A rapid review. Rev. Med. Virol. 2021, 23, e2162. [Google Scholar] [CrossRef]
- Zhou, W.; Xu, X.; Chang, Z.; Wang, H.; Zhong, X.; Tong, X.; Liu, T.; Li, Y. The dynamic changes of serum IgM and IgG against SARSCoV-2 in patients with COVID-19. J. Med. Virol. 2021, 93, 924–933. [Google Scholar] [CrossRef] [PubMed]
- Seow, J.; Graham, C.; Merrick, B.; Acors, S.; Pickering, S.; Kja, S.; Hemmings, O.; O’Byrne, A.; Kouphou, N.; Galao, R.P.; et al. Longitudinal observation and decline of neutralizing antibody responses in the three months following SARS-CoV-2 infection in humans. Nat. Microbiol. 2021, 5, 159. [Google Scholar] [CrossRef] [PubMed]
- Bloise, S.; Marcellino, A.; Testa, A.; Dilillo, A.; Mallardo, S.; Isoldi, S.; Martucci, V.; Sanseviero, M.T.; del Giudice, E.; Iorfida, D.; et al. Serum IgG levels in children 6 months after SARS-CoV-2 infection and comparison with adults. Eur. J. Pediatr. 2021, 180, 3335–3342. [Google Scholar] [CrossRef]
- Heald-Sargent, T.; Muller, W.J.; Zheng, X.; Rippe, J.; Patel, A.B.; Kociolek, L.K. Age-related differences in nasopharyngeal severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) levels in patients with mild to moderate coronavirus disease 2019 (COVID-19). JAMA Pediatr. 2020, 174, 902–903. [Google Scholar] [CrossRef]
- Kam, K.Q.; Yung, C.F.; Cui, L.; Tzer Pin Lin, R.; Mak, T.M.; Maiwald, M.; Li, J.; Chong, C.Y.; Nadua, K.; Tan, N.W.H.; et al. A well infant with coronavirus disease 2019 with high viral load. Clin. Infect. Dis. 2020, 71, 847–849. [Google Scholar] [CrossRef]
- Davies, N.G.; Klepac, P.; Liu, Y.; Prem, K.; Jit, M.; Eggo, R.M. CMMID COVID-19 working group. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat. Med. 2020, 26, 1205–1211. [Google Scholar] [CrossRef]
- Esposito, S.; Principi, N. Debates around the role of school closures in the coronavirus 2019 pandemic-reply. JAMA Pediatr. 2021, 175, 107–108. [Google Scholar] [CrossRef]
- Isoldi, S.; Mallardo, S.; Marcellino, A.; Bloise, S.; Dilillo, A.; Iorfida, D.; Testa, A.; del Giudice, E.; Martucci, V.; Sanseviero, M.; et al. The comprehensive clinic, laboratory, and instrumental evaluation of children with COVID-19: A 6-months prospective study. J. Med. Virol. 2021, 93, 3122–3132. [Google Scholar] [CrossRef] [PubMed]
- Castagnoli, R.; Votto, M.; Licari, A.; Brambilla, I.; Bruno, R.; Perlini, S.; Rovida, F.; Baldanti, F.; Marseglia, G.L. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection in Children and Adolescents: A Systematic Review. JAMA Pediatr. 2020, 174, 882–889. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lubrano, R.; Villani, A.; Berrettini, S.; Caione, P.; Chiara, A.; Costantino, A.; Formigari, R.; Franzoni, E.; Gattinara, G.C.; Giustardi, A.; et al. Point of view of the Italians pediatric scientific societies about the pediatric care during the COVID-19 lockdown: What has changed and future prospects for restarting. Ital. J. Pediatr. 2020, 46, 142. [Google Scholar] [CrossRef] [PubMed]
- Eberhardt, C.S.; Siegrist, C.A. Is there a role for childhood vaccination against COVID-19? Pediatr. Allergy Immunol. 2021, 32, 9–16. [Google Scholar] [CrossRef]
- Lubrano, R.; Bloise, S.; Testa, A.; Marcellino, A.; Dilillo, A.; Mallardo, S.; Isoldi, S.; Martucci, V.; Sanseviero, M.; del Giudice, E.; et al. Assessment of Respiratory Function in Infants and Young Children Wearing Face Masks During the COVID-19 Pandemic. JAMA Netw. Open. 2021, 4, e210414. [Google Scholar] [CrossRef]
- Lubrano, R.; Bloise, S.; Marcellino, A.; Ciolli, C.P.; Testa, A.; De Luca, E.; Dilillo, A.; Mallardo, S.; Isoldi, S.; Martucci, V.; et al. Effects of N95 Mask Use on Pulmonary Function in Children. J Pediatr. 2021, 237, 143–147. [Google Scholar] [CrossRef]
- Bloise, S.; Isoldi, S.; Marcellino, A.; De Luca, E.; Dilillo, A.; Mallardo, S.; Martucci, V.; Sanseviero, M.; del Giudice, E.; Iorfida, D.; et al. Clinical picture and long-term symptoms of SARS-CoV-2 infection in an Italian pediatric population. Ital. J. Pediatr. 2022, 48, 79. [Google Scholar] [CrossRef]
- FDA takes key action in fight against COVID-19 by issuing emergency use authorization for first COVID-19 vaccine. In News Release of the Food and Drug Administration; Silver Spring MD: San Jose, CA, USA. Available online: https://www.fda.gov/news-events/press-announcements/fda-takes-key-action-fight-against-covid-19-issuing-emergency-use-authorization-first-covid-19 (accessed on 11 December 2020).
- Coronavirus (COVID-19) update: FDA authorizes Pfizer-BioNTech COVID-19 vaccine for emergency use in adolescents in another important action in fight against pandemic. In News Release of the Food and Drug Administration; Silver Spring MD: San Jose, CA, USA. Available online: https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-pfizer-biontech-covid-19-vaccine-emergency-use (accessed on 10 May 2021).
- The FDA Expands Emergency Use Authorization of the Pfizer-BioNTech COVID-19 Vaccine to Include Children 5 through 11 Years of Age. Available online: https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/covid-19-vaccines (accessed on 29 October 2021).
- Comirnaty COVID-19 Vaccine: EMA Recommends Approval for Children Aged 5 to 11. Available online: https://www.ema.europa.eu/en/news/comirnaty-covid-19-vaccine-ema-recommends-approval-children-aged-5-11 (accessed on 29 October 2021).
- AIFA Approves Comirnaty Vaccine for Ages 5 to 11. Available online: https://www.aifa.gov.it/en/-/aifa-approva-il-vaccino-comirnaty-per-la-fascia-di-et%C3%A0-5-11-anni (accessed on 29 October 2021).
- Circolare Ministero della Salute 0056429-07/12/2021-DGPRE-DGPRE-P recante. Estensione di indicazione di utilizzo del vaccino Comirnatyn (BioNTech/Pfizer) per la Fascia di età 5-11 anni. Available online: https://www.ordinemedicifc.it/2021/12/10/circolare-ministero-della-salute-0056429-07-12-2021-dgpre-dgpre-p-recante-estensione-di-indicazione-di-utilizzo-del-vaccino-comirnatyn-biontech-pfizer-per-la-fascia-di-eta-5-11-anni/ (accessed on 7 December 2021).
- Frenck, R.W., Jr.; Klein, N.P.; Kitchin, N.; Gurtman, A.; Absalon, J.; Lockhart, S.; Perez, J.L.; Walter, E.B.; Senders, S.; Bailey, R.; et al. Safety, Immunogenicity, and Efficacy of the BNT162b2 Covid-19 Vaccine in Adolescents. N. Engl. J. Med. 2021, 385, 239–250. [Google Scholar] [CrossRef]
- Hause, A.M.; Gee, J.; Baggs, J.; Abara, W.E.; Marquez, P.; Thompson, D.; Su, J.R.; Licata, C.; Rosenblum, H.G.; Myers, T.R.; et al. COVID-19 Vaccine Safety in Adolescents Aged 12–17 Years-United States, 14 December 2020–16 July 2021. MMWR Morb. Mortal Wkly. Rep. 2021, 70, 1053–1058. [Google Scholar] [CrossRef]
- Freedman, A.G.; Hershkovitz, Y.; Kaufman, Z.; Dichtiar, R.; Keinan-Boker, L.; Bromberg, M. Effectiveness of BNT162b2 vaccine in adolescents during outbreak of SARS-CoV-2 delta variant infection, Israel, 2021. Emerg. Infect. Dis. 2021, 27, 2919–2922. [Google Scholar] [CrossRef]
- Ali, K.; Berman, G.; Zhou, H.; Deng, W.; Faughnan, V.; Coronado-Voges, M.; Ding, B.; Dooley, J.; Girard, B.; Hillebrand, W.; et al. Evaluation of mRNA-1273 SARS-CoV-2 vaccine in adolescents. N. Engl. J. Med. 2021, 385, 2241–2251. [Google Scholar] [CrossRef] [PubMed]
- Walter, E.B.; Talaat, K.R.; Sabharwal, C.; Gurtman, A.; Lockhart, S.; Paulsen, G.C.; Barnett, E.D.; Muñoz, F.M.; Maldonado, Y.; Pahud, B.A.; et al. Evaluation of the BNT162b2 Covid-19 Vaccine in Children 5 to 11 Years of Age. N. Engl. J. Med. 2022, 386, 35–46. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.J.; Wang, X.C.; Feng, L.Z.; Xie, Z.D.; Jiang, Y.; Lu, G. Expert consensus on COVID-19 vaccination in children. World J. Pediatr. 2021, 17, 449–457. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.; Tang, J.; Chen, C.; Wang, C.; Wen, W.; Cheng, Y.; Zhou, M.; Wu, Q.; Zhang, X.; Feng, Z.; et al. Safety and efficacy of the COVID-19 vaccine in children and/or adolescents: A meta-analysis. J. Infect. 2022, 84, 722–746. [Google Scholar] [CrossRef]
- Gargano, J.W.; Wallace, M.; Hadler, S.C.; Langley, G.; Su, J.R.; Oster, M.E.; Broder, K.R.; Gee, J.; Weintraub, E.; Shimabukuro, T.; et al. Use of mRNA COVID-19 Vaccine After Reports of Myocarditis among Vaccine Recipients: Update from the Advisory Committee on Immunization Practices-United States, June 2021. MMWR Morb. Mortal Wkly. Rep. 2021, 70, 977–982. [Google Scholar] [CrossRef]
- Israelian Ministry of Health. Surveillance of Myocarditis (Inflammation of the Heart Muscle) Cases between December 2020 and May 2021 (Including). Available online: https://www.gov.il/en/departments/news/01062021-03 (accessed on 24 July 2021).
- Bozkurt, B.; Kamat, I.; Hotez, P.J. Myocarditis with COVID-19 mRNA vaccines. Circulation 2021, 144, 471–484. [Google Scholar] [CrossRef]
- Mevorach, D.; Anis, E.; Cedar, N.; Bromberg, M.; Haas, E.J.; Nadir, E.; Olsha-Castell, S.; Arad, D.; Hasin, T.; Levi, N.; et al. Myocarditis after BNT162b2 mRNA vaccine against Covid-19 in Israel. N. Engl. J. Med. 2021, 385, 2140–2149. [Google Scholar] [CrossRef]
- Witberg, G.; Barda, N.; Hoss, S.; Richter, I.; Wiessman, M.; Aviv, Y.; Grinberg, T.; Auster, O.; Dagan, N.; Balicer, R.D.; et al. Myocarditis after Covid-19 vaccination in a large health care organization. N. Engl. J. Med. 2021, 385, 2132–2139. [Google Scholar] [CrossRef]
- Advisory Committee on Immunization Practices (ACIP), Centers for Disease Control and Prevention. COVID-19 Vaccine Saftey Updates. Available online: https://www.cdc.gov/vaccines/acip/meetings/slides-2021-06.html (accessed on 27 July 2021).
- Jain, S.S.; Steele, J.M.; Fonseca, B.; Huang, S.; Shah, S.; Maskatia, S.A.; Buddhe, S.; Misra, N.; Ramachandran, P.; Gaur, L.; et al. COVID-19 Vaccination-Associated myocarditis in adolescents. Pediatrics 2021. [Google Scholar] [CrossRef]
- Klein, N.P.; Lewis, N.; Goddard, K.; Fireman, B.; Zerbo, O.; Hanson, K.E.; Donahue, J.G.; Kharbanda, E.O.; Naleway, A.; Nelson, J.C.; et al. Surveillance for adverse events after COVID-19 mRNA vaccination. JAMA 2021, 326, 1390–1399. [Google Scholar] [CrossRef]
- Cocco, G.; Delli Pizzi, A.; Fabiani, S.; Cocco, N.; Boccatonda, A.; Frisone, A.; Scarano, A.; Schiavone, C. Lymphadenopathy after the Anti-COVID-19 Vaccine: Multiparametric Ultrasound Findings. Biology 2021, 10, 652. [Google Scholar] [CrossRef] [PubMed]
- Granata, V.; Fusco, R.; Setola, S.V.; Galdiero, R.; Picone, C.; Izzo, F.; D’Aniello, R.; Miele, V.; Grassi, R.; Grassi, R.; et al. Lymphadenopathy after BNT162b2 Covid-19 Vaccine: Preliminary Ultrasound Findings. Biology 2021, 10, 214. [Google Scholar] [CrossRef] [PubMed]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Marc, G.P.; Moreira, E.D.; Zerbini, C.; et al. Safety and efficacy of the BNT162b2 mRNA. Covid-19 vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef] [PubMed]
- Cohen, D.; Krauthammer, S.H.; Wolf, I.; Even-Sapir, E. Hypermetabolic lymphadenopathy following administration of BNT162b2 mRNA Covid-19 vaccine: Incidence assessed by. [18F] FDG PET-CT and relevance to study interpretation. Eur. J. Nucl. Med. Mol. Imaging. 2021, 48, 1854–1863. [Google Scholar] [CrossRef]
- Soub, H.A.; Ibrahim, W.; Maslamani, M.A.; Ali, G.A.; Ummer, W.; Abu-Dayeh, A. Kikuchi-Fujimoto disease following SARS CoV2 vaccination: Case report. IDCases 2021, 25, e01253. [Google Scholar] [CrossRef]
- Morparia, K.; Park, M.J.; Kalyanaraman, M.; McQueen, D.; Bergel, M.; Phatak, T. Abdominal Imaging Findings in Critically Ill Children with Multisystem Inflammatory Syndrome Associated With COVID. Pediatr. Infect. Dis. J. 2021, 40, e82–e83. [Google Scholar] [CrossRef]
- Akobeng, A.K.; Grafton-Clarke, C.; Abdelgadir, I.; Twum-Barimah, E.; Gordon, M. Gastrointestinal manifestations of COVID-19 in children: A systematic review and meta-analysis. Frontline Gastroenterol. 2020, 12, 332–337. [Google Scholar] [CrossRef]
- Bolia, R.; Dhanesh Goel, A.; Badkur, M.; Jain, V. Gastrointestinal Manifestations of Pediatric Coronavirus Disease and Their Relationship with a Severe Clinical Course: A Systematic Review and Meta-analysis. J. Trop. Pediatr. 2021, 67, fmab051. [Google Scholar] [CrossRef]
- Lo Vecchio, A.; Garazzino, S.; Smarrazzo, A.; Venturini, E.; Poeta, M.; Berlese, P.; Denina, M.; Meini, A.; Bosis, S.; Galli, L.; et al. Factors Associated with Severe Gastrointestinal Diagnoses in Children With SARS-CoV-2 Infection or Multisystem Inflammatory Syndrome. JAMA Netw. Open 2021, 4, e2139974. [Google Scholar] [CrossRef]
- Pizuorno, A.; Brim, H.; Ashktorab, H. Gastrointestinal manifestations and SARS-CoV-2 infection. Curr. Opin. Pharmacol. 2021, 61, 114–119. [Google Scholar] [CrossRef]
- Shehab, M.; Alrashed, F.; Shuaibi, S.; Alajmi, D.; Barkun, A. Gastroenterological and hepatic manifestations of patients with COVID-19, prevalence, mortality by country, and intensive care admission rate: Systematic review and meta-analysis. BMJ Open Gastroenterol. 2021, 8, e000571. [Google Scholar] [CrossRef] [PubMed]
- Merola, E.; Armelao, F.; de Pretis, G. Prevalence of gastrointestinal symptoms in coronavirus disease 2019: A meta-analysis. Acta Gastroenterol. Belg. 2020, 83, 603–615. [Google Scholar] [PubMed]
- Dorrell, R.D.; Dougherty, M.K.; Barash, E.L.; Lichtig, A.E.; Clayton, S.B.; Jensen, E.T. Gastrointestinal and hepatic manifestations of COVID-19: A systematic review and meta-analysis. JGH Open. 2020, 5, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Rokkas, T. Gastrointestinal involvement in COVID-19: A systematic review and meta-analysis. Ann. Gastroenterol. 2020, 33, 355–365. [Google Scholar] [CrossRef] [PubMed]
- Tullie, L.; Ford, K.; Bisharat, M.; Watson, T.; Thakkar, H.; Mullassery, D.; Giuliani, S.; Blackburn, S.; Cross, K.; de Coppi, K.C.; et al. Gastrointestinal features in children with COVID-19: An observation of varied presentation in eight children. Lancet Child Adolesc. Health 2020, 4, e19–e20. [Google Scholar] [CrossRef]
- Saeed, U.; Sellevoll, H.B.; Young, V.S.; Sandbaek, G.; Glomsaker, T.; Mala, T. Covid-19 may present with acute abdominal pain. Br. J. Surg. 2020, 107, e186–e187. [Google Scholar] [CrossRef]
- Abdalhadi, A.; Alkhatib, M.; Mismar, A.Y.; Awouda, W.; Albarqouni, L. Can COVID 19 present like appendicitis? IDCases 2020, 21, e00860. [Google Scholar] [CrossRef]


| Study | Population | Study Type | Vaccine | All Person | Controls | Vaccine Efficacy (95%CI) | The Most Common Adverse Events after First and Second Dose |
|---|---|---|---|---|---|---|---|
| Frenck et al. [24] | 5–11 years | Randomized controlled trial | BNT162b2 mRNA | 2260 | 1129 | 100% (95% CI, 78.1 to 100) | -injection site reactions (86%/79%) -fatigue (60%/66%) -headache (55%/65%) |
| Hause et al. [25] | 12–17 years | observational study | BNT162b2 mRNA | 66,550 | / | / | -injection site reactions (63.9%/62.4%) -fatigue (27.4%/44.6%) -headache (25.2%/43.7%) |
| Freedman et al. [26] | 12–15 years | observational study | BNT162b2 mRNA | 187,707 | / | 91.5% (95% CI 88.2–93.9% | / |
| Ali et al. [27] | 12–17 years | Randomized controlled trial | mRNA-1273 | 3732 | 1243 | 98.8(95%CI = 97.0 to 99.7) | -injection site reactions (93.1%/92.4%) -fatigue (47.9%/67.8%) -headache (38.5%30.2%%) |
| Walter et al. [28] | 5–11 years | Randomized controlled trial | BNT162b2 mRNA | 2268 | 750 | 90.7% (95% CI, 67.7–98.3) | -injection site reactions -Fatigue -Headache |
| Children | ||||
|---|---|---|---|---|
| Study | Study Type | Number of Patients | Most Common Gastrointestinal Symptoms Reported | Other Findings |
| Akobeng AK et al. [45] | systematic review and metanalysis | 280 | -diarrhea (12.6%) -vomit (10.3%) -abdominal pain (5.4%) | / |
| Bolia R et al. [46] | systematic review and meta-analysis | 4369 | -abdominal pain (20.3%) -nausea/vomit (19.7) -diarrhea (19.08) | The presence of diarrhea was significantly associated with a severe clinical course |
| Isoldi S et al. [11] | cohort study | 15 | -diarrhea (26.7%) -abdominal pain (13.3%) -nausea/vomit (6.7%) | Abdominal Ultrasounds performed in all patients were negative |
| Lo Vecchio et al. [47] | retrospective cohort study | 685 | -diarrhea (55.7%) -vomit (30.2%) -abdominal pain (20.3%) | The presence of GI symptoms was associated with a higher chance of hospitalization and intensive care unit admission |
| Adult | ||||
| Pizuorno A et al. [48] | retrospective cohort study | 1607 | -diarrhea (21.3%) -vomit (18%) -abdominal pain (4.5%) | / |
| Shehab M et al. [49] | systematic review and meta-analysis | 78,798 | -diarrhea (16.5%) -nausea (9.7%) -elevated liver enzymes (5.6%) | The presence of GI symptoms/elevated liver enzymes does not influence to mortality or intensive care unit admission rate |
| Merola E et al. [50] | systematic review and meta-analysis | 4434 | -diarrhea (7.78%) -nausea/vomit (3.57%) -poor appetite (2.39%) | The authors showed the positivity for COVID-19 in stool samples in 41.50% of cases. |
| Dorrell RD et al. [51] | systematic review | 17,776 | -anorexia (21%) -diarrhea (13%) -nausea/vomit (8%) | Gatrointestinal symptoms were associated with severe COVID-19 disease |
| Rokkas T et al. Ann Gastroenterol. 2020. [52] | systematic review and meta-analysis | 5601 | -diarrhea (10.4%) -nausea/vomit (7.7%) -abdominal pain (6.9%) | / |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bloise, S.; Marcellino, A.; Martucci, V.; Sanseviero, M.; Testa, A.; Del Giudice, E.; Spatuzzo, M.; Sermoneta, D.; Ventriglia, F.; Lubrano, R. Adenomesenteritis following SARS-CoV-2 Vaccination in Children: A Case Report and Review of The Literature. Children 2022, 9, 993. https://doi.org/10.3390/children9070993
Bloise S, Marcellino A, Martucci V, Sanseviero M, Testa A, Del Giudice E, Spatuzzo M, Sermoneta D, Ventriglia F, Lubrano R. Adenomesenteritis following SARS-CoV-2 Vaccination in Children: A Case Report and Review of The Literature. Children. 2022; 9(7):993. https://doi.org/10.3390/children9070993
Chicago/Turabian StyleBloise, Silvia, Alessia Marcellino, Vanessa Martucci, Mariateresa Sanseviero, Alessia Testa, Emanuela Del Giudice, Mattia Spatuzzo, Daniel Sermoneta, Flavia Ventriglia, and Riccardo Lubrano. 2022. "Adenomesenteritis following SARS-CoV-2 Vaccination in Children: A Case Report and Review of The Literature" Children 9, no. 7: 993. https://doi.org/10.3390/children9070993
APA StyleBloise, S., Marcellino, A., Martucci, V., Sanseviero, M., Testa, A., Del Giudice, E., Spatuzzo, M., Sermoneta, D., Ventriglia, F., & Lubrano, R. (2022). Adenomesenteritis following SARS-CoV-2 Vaccination in Children: A Case Report and Review of The Literature. Children, 9(7), 993. https://doi.org/10.3390/children9070993






