Frequency, Etiology, Mortality, Cost, and Prevention of Respiratory Tract Infections—Prospective, One Center Study
Abstract
:1. Introduction
2. Material and Methods
2.1. Design and Settings
2.2. Ethical Approval
2.3. Clinical Diagnosis of RTIs
2.4. Microbiological Diagnosis of RTI
2.5. Sepsis Diagnosis
2.6. Data Collection
2.7. Epidemiological Indicators
2.8. Extra Length of Stay and Additional Cost of Therapy
2.9. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- Infections of the respiratory tract constitute a serious epidemiological problem in patients admitted and treated in ICU, as they affect one-third of patients, and pneumonia affects one-fourth of patients.
- Hospital-acquired pneumonia was found more frequently than community-acquired pneumonia and had an influence on the length of stay prolongation at the ICU, increasing therapy cost and mortality.
- Due to the department profile, nosocomial pneumonia VAP was found more often in surgical patients than in internal medicine patients, while NV-HAP was more often found in internal medicine patients admitted from other hospital wards, which requires increased monitoring and the prevention of NV-HAP in internal medicine departments.
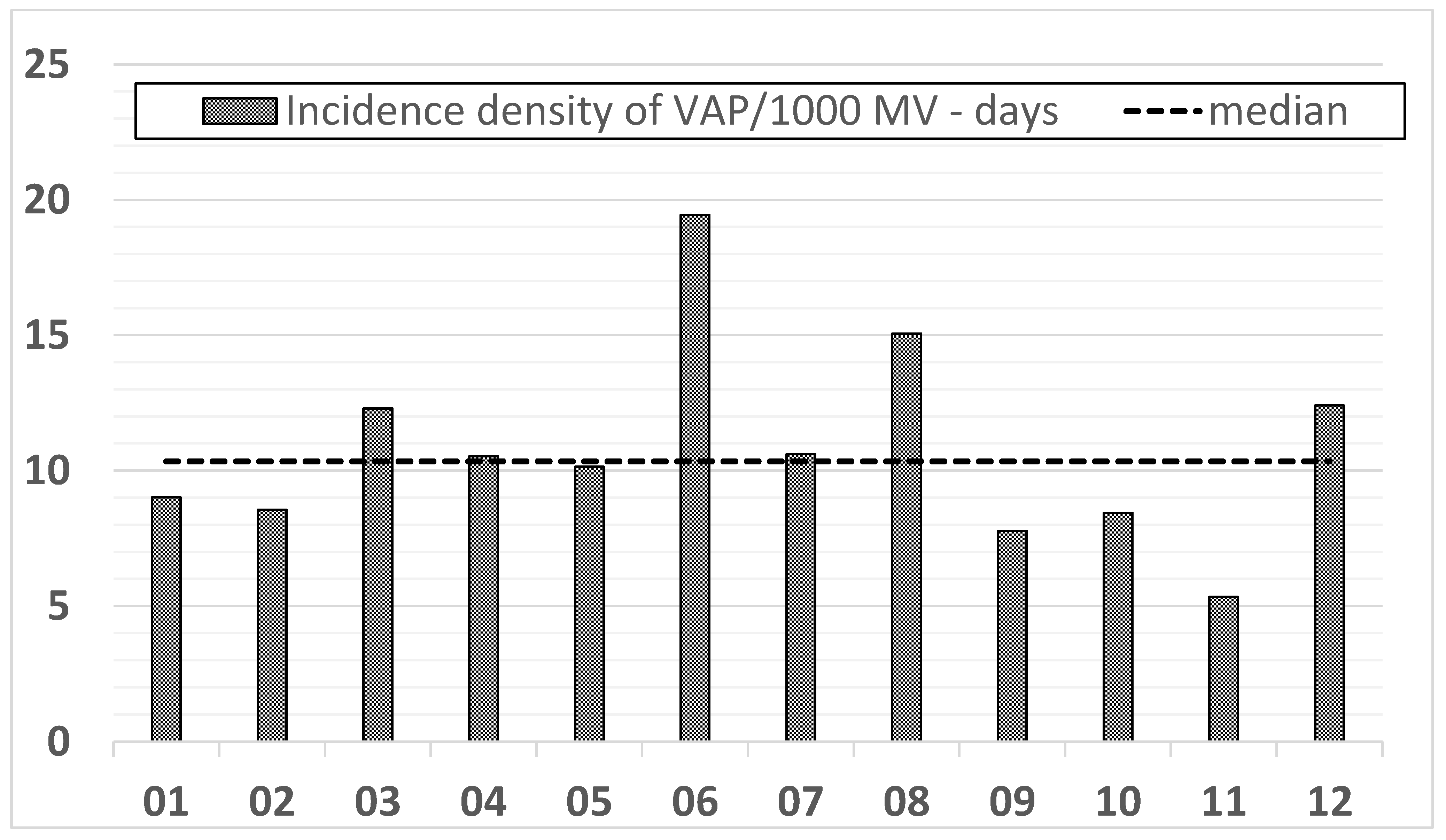
- The frequency and density of VAP occurrence remains high and requires clarification of the cause, tightening the discipline of compliance with preventive packages and elements not included in the study, such as hand hygiene control and an estimation of the number of nursing staff per one patient.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Blot, S.; Koulenti, D.; Dimopoulos, G.; Martin, C.; Komnos, A.; Krueger, W.A.; Spina, G.; Armaganidis, A.; Rello, J.; EU-VAP Study Investigators. Prevalence, risk factors, and mortality for ventilator-associated pneumonia in middle-aged, old, and very old critically ill patients. Crit. Care Med. 2014, 42, 601–609. [Google Scholar] [CrossRef] [PubMed]
- Kalanuria, A.; Zai, W.; Mirski, M. Ventilator-associated pneumonia in the ICU. Annu. Update Intensive Care Emerg. Med. 2014, 18, 208. [Google Scholar] [CrossRef] [Green Version]
- Duszyńska, W.; Rosenthal, V.D.; Dragan, B.; Węgrzyn, P.; Mazur, A.; Wojtyra, P.; Tomala, A.; Kübler, A. Ventilator-associated pneumonia monitoring according to the INICC project at one centre. Anaesthesiol. Intensive Ther. 2015, 47, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Rosenthal, V.D.; Rodrigues, C.; Álvarez-Moreno, C.; Madani, N.; Mitrev, Z.; Ye, G.; Salomao, R.; Ulger, F.; Guanche-Garcell, H.; Kanj, S.S.; et al. Effectiveness of a multidimensional approach for prevention of ventilator-associated pneumonia in adult intensive care units from 14 developing countries of four continents. Crit. Care Med. 2012, 40, 3121–3128. [Google Scholar] [CrossRef] [PubMed]
- Koulenti, D.; Tsigou, E.; Rello, J. Nosocomial pneumonia in 27 ICUs in Europe: Perspectives from the EU-VAP/CAP study. Eur. J. Clin. Microbiol. 2016, 36, 1999–2006. [Google Scholar] [CrossRef]
- Baker, D.; Quinn, B. Hospital Acquired Pneumonia Prevention Initiative-2: Incidence of nonventilator hospital-acquired pneumonia in the United States. Am. J. Infect. Control 2018, 46, 2–7. [Google Scholar] [CrossRef] [Green Version]
- Ji, W.; McKenna, C.; Ochoa, A.; Batlle, H.R.; Young, J.; Zhang, Z.; Rhee, C.; Clark, R.; Shenoy, E.S.; Hooper, D.; et al. Development and Assessment of Objective Surveillance Definitions for Nonventilator Hospital-Acquired Pneumonia. JAMA Netw. Open 2019, 2, e1913674. [Google Scholar] [CrossRef]
- Vincent, J.-L.; Bihari, D.J.; Suter, P.M.; Bruining, H.A.; White, J.; Nicolas-Chanoin, M.-H.; Wolff, M.; Spencer, R.C.; Hemmer, M. The Prevalence of Nosocomial Infection in Intensive Care Units in Europe. JAMA 1995, 274, 639–644. [Google Scholar] [CrossRef]
- Dudeck, M.A.; Weiner, L.M.; Allen-Bridson, K.; Malpiedi, P.J.; Peterson, K.D.; Pollock, D.A.; Sievert, D.M.; Edwards, J.R. National Healthcare Safety Network (NHSN) report, data summary for 2012, Device-associated module. Am. J. Infect. Control 2013, 41, 1148–1166. [Google Scholar] [CrossRef] [Green Version]
- Tomaszewski, D.; Rybicki, Z.; Duszyńska, W. The Polish Prevalence of Infection in Intensive Care (PPIC): A one-day point prevalence multicenter study. Adv. Clin. Exp. Med. 2019, 28, 907–912. [Google Scholar] [CrossRef] [Green Version]
- Rosenthal, V.D.; Al-Abdely, H.M.; El-Kholy, A.A.; AlKhawaja, S.A.A.; Leblebicioglu, H.; Mehta, Y.; Rai, V.; Hung, N.V.; Kanj, S.S.; Salama, M.F.; et al. International Nosocomial Infection Control Consortium report, data summary of 50 countries for 2010–2015: Device-associated module. Am. J. Infect. Control 2016, 44, 1495–1504. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Healthcare-associated infections acquired in intensive care units. In ECDC Annual Epidemiological Report for 2016; ECDC: Stockholm, Sweden, 2018; Available online: https://www.ecdc.europa.eu/sites/default/files/documents/AER_for_2016-HAI.pdf (accessed on 4 May 2018).
- Vincent, J.L.; Rello, J.; Marshall, J.; Silva, E.; Anzueto, A.; Martin, C.D.; Moreno, R.; Lipman, J.; Gomersall, C.; Sakr, Y.; et al. International study of the prevalence and outcomes of infection in intensive care units. JAMA 2009, 302, 2323–2329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kollef, M.H.; Hamilton, C.W.; Ernst, F.R. Economic Impact of Ventilator-Associated Pneumonia in a Large Matched Cohort. Infect. Control Hosp. Epidemiol. 2012, 33, 250–256. [Google Scholar] [CrossRef]
- Davis, J.; Finley, E. A second breadth: Hospital-acquired pneumonia in Pennsylvania, nonventilated versus ventilated patients. PA Patient Saf. Advis. 2018, 15, 48–59. [Google Scholar]
- European Centre for Disease Prevention and Control. Healthcare-associated infections acquired in intensive care units. In ECDC Annual Epidemiological Report for 2017; ECDC: Stockholm, Sweden, 2019; Available online: http://www.ecdc.europa.eu/en/publications-data/healthcare-associated-infections-intensive-care-units-annual-epidemiological-1 (accessed on 10 October 2019).
- Weiner, L.M.; Webb, A.K.; Limbago, B.; Dudeck, M.A.; Patel, J.; Kallen, A.J.; Edwards, J.R.; Sievert, D.M. Antimicrobial-resistant pathogens associated with healthcare-associated infections: Summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2011–2014. Infect. Control. Hosp. Epidemiol. 2016, 37, 1288–1301. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wałaszek, M.; Różańska, A.; Wałaszek, M.Z.; Wójkowska-Mach, J. Epidemiology of Ventilator-Associated Pneumonia, microbiological diagnostics and the length of antimicrobial treatment in the Polish Intensive Care Units in the years 2013–2015. BMC Infect. Dis. 2018, 18, 308. [Google Scholar] [CrossRef] [Green Version]
- Duszynska, W.; Rosenthal, V.D.; Szczesny, A.; Zajaczkowska, K.; Fulek, M.; Tomaszewski, J. Device associated –health care associated infections monitoring, prevention and cost assessment at intensive care unit of University Hospital in Poland (2015–2017). BMC Infect. Dis. 2020, 20, 761. [Google Scholar] [CrossRef]
- Blot, S.; Koulenti, D.; Dimopoulos, G.; Coppadoro, A.; Bittner, E.; Berra, L. Novel preventive strategies for ventilator-associated pneumonia. Crit. Care 2012, 16, 210. [Google Scholar] [CrossRef] [Green Version]
- Berenholtz, S.M.; Pham, J.C.; Thompson, D.A.; Needham, D.M.; Lubomski, L.H.; Hyzy, R.C.; Welsh, R.; Cosgrove, S.E.; Sexton, J.B.; Colantuoni, E.; et al. Collaborative Cohort Study of an Intervention to Reduce Ventilator-Associated Pneumonia in the Intensive Care Unit. Infect. Control Hosp. Epidemiol. 2011, 32, 305–314. [Google Scholar] [CrossRef] [Green Version]
- Álvarez-Lerma, F.; Palomar-Martínez, M.; Sánchez-García, M.; Martínez-Alonso, M.; Rodríguez, J.; Lorente, L.; Arias-Rivera, S.; García, R.; Gordo, F.; Añón, J.M.; et al. Prevention of Ventilator-Associated Pneumonia. Crit. Care Med. 2018, 46, 181–188. [Google Scholar] [CrossRef] [Green Version]
- European Centre for Disease Prevention and Control. European Surveillance of Healthcare Associated Infections in Intensive Care Units-HAI-Net ICU Protocol, Version 1.02; ECDC: Stockholm, Sweden, 2015. Available online: http://ecdc.europa.eu/sites/portal/files/media/en/publications/Publications/health-care-associated-infections-HAI-ICU-protocol.pdf. (accessed on 13 June 2017).
- De Pascale, G.; Ranzani, O.T.; Nseir, S.; Chastre, J.; Welte, T.; Antonelli, M.; Navalesi, P.; Garofalo, E.; Bruni, A.; Coelho, L.M.; et al. Intensive care unit patients with lower respiratory tract nosocomial infections: The ENIRRIs project. ERJ Open Res. 2017, 3, 00092–2017. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lei, Y.; Hudcova, J.; Rashid, J.; Sarwar, A.; Gillespie, W.; Finn, C.; Goggin, M.; Omran, M.B.; Boroda, E.; Craven, D.E. Natural History, Outcomes and Antibiotic Treatment for Ventilator-Associated Tracheobronchitis in Critical Ill Patients. Mod. Res. Inflamm. 2016, 5, 1–11. [Google Scholar] [CrossRef]
- EUCAST. Breakpoint Tables for Interpretation of MICs and Zone Diameters, Version 6.0. 2016. Available online: http://www.eucast.org/clinical_breakpoints/ (accessed on 1 January 2016).
- Rhodes, A.; Evans, L.E.; Alhazzani, W.; Levy, M.M.; Antonelli, M.; Ferrer, R.; Kumar, A.; Sevransky, J.E.; Sprung, C.L.; Nunnally, M.E.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017, 43, 304–377. [Google Scholar] [CrossRef] [PubMed]
- Vincent, J.-L.; Sakr, Y.; Singer, M.; Martin-Loeches, I.; Machado, F.R.; Marshall, J.C.; Finfer, S.; Pelosi, P.; Brazzi, L.; Aditianingsih, D.; et al. Prevalence and Outcomes of Infection Among Patients in Intensive Care Units in 2017. JAMA 2020, 323, 1478–1487. [Google Scholar] [CrossRef] [PubMed]
- Kübler, A.; Duszynska, W.; Rosenthal, V.D.; Fleischer, M.; Kaiser, T.; Szewczyk, E.; Barteczko-Grajek, B. Device-associated infection rates and extra length of stay in an intensive care unit of a university hospital in Wroclaw, Poland: International Nosocomial Infection Control Consortium’s (INICC) findings. J. Crit. Care 2012, 27, 105.e5–105.e10. [Google Scholar] [CrossRef]
- Rosenthal, V.D.; Bat-Erdene, I.; Gupta, D.; Belkebir, S.; Rajhans, P.; Zand, F.; Myatra, S.N.; Afeef, M.; Tanzi, V.L.; Muralidharan, S.; et al. International Nosocomial Infection Control Consortium (INICC) report, data summary of 45 countries for 2012-2017: Device-associated module. Am. J. Infect. Control. 2020, 48, 423–432. [Google Scholar] [CrossRef]
- Karvouniaris, M.; Makris, D.; Manoulakas, E.; Zygoulis, P.; Mantzarlis, K.; Triantaris, A.; Chatzi, M.; Zakynthinos, E. Ventilator-Associated Tracheobronchitis Increases the Length of Intensive Care Unit Stay. Infect. Control Hosp. Epidemiol. 2013, 34, 800–808. [Google Scholar] [CrossRef]
- Martin-Loeches, I.; Povoa, P.; Rodríguez, A.; Curcio, D.; Suarez, D.; Mira, J.P.; Cordero, M.L.; Lepecq, R.; Girault, C.; Candeias, C.; et al. Incidence and prognosis of ventilator-associated tracheobronchitis (TAVeM): A multicentre, prospective, observational study. Lancet Respir. Med. 2015, 3, 859–868. [Google Scholar] [CrossRef]
- Kaczorowska, M.; Kübler, A.; Maciejewski, D.; Adamik, B. Mechanical ventilation in ICUs in Poland: A multi-center point-prevalence study. Med. Sci. Monit. 2013, 19, 424–429. [Google Scholar] [CrossRef] [Green Version]
- Kołpa, M.; Wałaszek, M.; Gniadek, A.; Wolak, Z.; Dobroś, W. Incidence, Microbiological Profile and Risk Factors of Healthcare-Associated Infections in Intensive Care Units: A 10 Year Observation in a Provincial Hospital in Southern Poland. Int. J. Environ. Res. Public Health 2018, 15, 112. [Google Scholar] [CrossRef] [Green Version]
- Duszyńska, W.; Barteczko, B.; Kübler, A. Monitoring of nosocomial infections using the HELICS network. Anaesthesiol. Intensive Ther. 2008, 40, 17. [Google Scholar]
- Rosenthal, V.D.; Duszynska, W.; Ider, B.-E.; Gurskis, V.; Al-Ruzzieh, M.A.; Myatra, S.N.; Gupta, D.; Belkebir, S.; Upadhyay, N.; Zand, F.; et al. International Nosocomial Infection Control Consortium (INICC) report, data summary of 45 countries for 2013–2018, Adult and Pediatric Units, Device-associated Module. Am. J. Infect. Control 2021, 49, 1267–1274. [Google Scholar] [CrossRef] [PubMed]
- CDC-NHSN. The 2019 National and State Healthcare-Associated Infections (HAI) Progress Report. Available online: https://www.cdc.gov/nhsn/datastat/index.html (accessed on 17 February 2021).
- Vincent, J.-L.; Sakr, Y.; Sprung, C.L.; Ranieri, V.M.; Reinhart, K.; Gerlach, H.; Moreno, R.; Carlet, J.; Le Gall, J.-R.; Payen, D. Sepsis in European intensive care units: Results of the SOAP study*. Crit. Care Med. 2006, 34, 344–353. [Google Scholar] [CrossRef] [PubMed]
- Kübler, A.; Adamik, B.; Durek, G.; Mayzner-Zawadzka, E.; Gaszyński, W.; Karpel, E.; Duszynska, W. Wyniki rejestru przypadków ciężkiej sepsy na oddziałach intensywnej terapii w Polsce w latach 2003−2009. Anaesthesiol. Intensive Ther. 2015, 47, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Duszynska, W.; Litwin, A.; Rojek, S.; Szczesny, A.; Ciasullo, A.; Gozdzik, W. Analysis of Acinetobacter baumannii hospital infections in patients treated at the intensive care unit of the University Hospital, Wroclaw, Poland: A 6-year, single-center, retrospective study. Infect. Drug Resist. 2018, 11, 629–635. [Google Scholar] [CrossRef] [Green Version]
- Litwin, A.; Fedorowicz, O.; Duszynska, W. Characteristics of Microbial Factors of Healthcare-Associated Infections Including Multidrug-Resistant Pathogens and Antibiotic Consumption at the University Intensive Care Unit in Poland in the years 2011–2018. Int. J. Environ. Res. Public Health 2020, 17, 6943. [Google Scholar] [CrossRef]
- Dallas, J.; Skrupky, L.; Abebe, N.; Boyle, W.A.; Kollef, M.H. Ventilator-Associated Tracheobronchitis in a Mixed Surgical and Medical ICU Population. Chest 2011, 139, 513–518. [Google Scholar] [CrossRef]
- Deptuła, A.; Trejnowska, E.; Ozorowski, T.; Hryniewicz, W. Risk factors for healthcare-associated infection in light of two years of experience with the ECDC point prevalence survey of healthcare-associated infection and antimicrobial use in Poland. J. Hosp. Infect. 2015, 90, 310–315. [Google Scholar] [CrossRef]
- Bundle VAP/Institute for Healthcare Improvement. Available online: http://www.ihi.org/knowledge/Pages/Changes/ImplementtheVentilatorBundle.aspx. (accessed on 28 September 2013).
- Morris, A.C.; Hay, A.W.; Swann, D.G.; Everingham, K.; McCulloch, C.; McNulty, J.; Brooks, O.; Laurenson, I.F.; Cook, B.; Walsh, T.S. Reducing ventilator-associated pneumonia in intensive care: Impact of implementing a care bundle. Crit. Care Med. 2011, 39, 2218–2224. [Google Scholar] [CrossRef] [Green Version]
| Year | 2018 |
| Total number of hospitalized patients; n | 578 |
| Women; n (%) | 219 (37.9) |
| Men; n (%) | 359 (62.1) |
| Surgical patients; n (%) | 382 (66.1) |
| Internal medicine patients; n (%) | 196 (33.9) |
| Total number of patients-day; (n) | 5829 |
| Number of patients died; n (%) | 160 (27.68) |
| Clinical Kinds of RTI | RTI at Admission at ICU n (%) | RTI during Hospital Stay at ICU n (%) |
|---|---|---|
| CAP | 34 (5.88) | - |
| NV-HAP | 42 (7.3) | 10 (1.7) |
| VAP | - | 50 (8.65) |
| VAT | - | 35 (6) |
| RTI total | 76 (13.18) | 95 (16.4) |
| Number of Patients | CAP n, %, (95%CI) | p | NV-HAP n, %, (95% CI) | p | VAP n, %, (95% CI) | p | VAT n, %, (95% CI) | p | |
|---|---|---|---|---|---|---|---|---|---|
| Surgical patients | 382 | 10, 2.62 (1.26–4.76) | 0 | 26, 6.81 (4.49–9.81) | 0.006 | 35, 9.16 (6.46–12.51) | 0.0946 | 25, 6.54 (4.28–9.51) | 0.4913 |
| Internal medicine patients | 196 | 24, 12.24 (8.01–17.67) | 26, 13.26 (8.85–18.83) | 15, 7.65 (4.35–12,31) | 10, 5.1 (2.47–9.18) | ||||
| Women | 219 | 14, 6.39 (3.54–10,49) | 0.603 | 17, 7.76 (4.59–12.14) | 0.500 | 11, 5.02 (2.53–8.81) | 0.0154 | 11, 5.02 (2.53–8.81) | 0.416 |
| Men | 359 | 20, 5.57 (3.44–8.47) | 35, 9.75 (6.89–13.30) | 39, 10.86 (7.84–14.55) | 24, 6.68 (4.33–9.78) | ||||
| ≥65 years | 255 | 15, 5.88 (5.49–12.77) | 1.0 | 29, 11.37 (7.75–15.92) | 0.076 | 18, 7.06 (4.24–10.93) | 0.2265 | 13, 5.10 (2.74–8.56) | 0.391 |
| <65 years | 323 | 19, 5.88 (3.58–9.03) | 23, 7.12 (4.57–10.49) | 32, 9.91 (6.88–13.7) | 22, 6.81 (4.32–10.13) |
| CAP | NV-HAP | VAP | VAT |
|---|---|---|---|
| MSSA 18; 37% | Acinetobacter baumannii 17; 22% including MDR 12; 15% | Acinetobacter baumanii MDR 33; 45% | Acinetobacter baumannii 20; 42% including MDR 15; 31% |
| Escherichia coli 7; 14% | Klebsiella pneumoniae/oxytoca 16; 20% including ESBL(+) 8; 10% | Klebsiella pneum. ESBL+ 10; 14% | Klebsiella pneum. 9; 19% including ESBL(+) 4; 8% |
| Enterobacter spp. 5; 10% | MSSA 12; 15% | MSSA 7; 9% | Pseudomonas aeruginosa 4; 8% including 1; 2% MDR |
| Klebsiella pneum. 4; 6% including ESBL(+); 2% | MRSA 7; 9% | Pseudomonas aeruginosa 6; 8% | Enterobacteriacae 4; 8% including ESBL(+) 2; 4% |
| Streptococcus pneumoniae 3; 6% | Pseudomonas aeruginosa 4; 5% | Enterobacteriacae 6; 8% including ESBL4; 5% | MRSA2; 4% |
| Pseudomonas aeruginosa 2; 4% | Enterobacter cloacae 6; 8% including ESBL(+)2; 2% | MRSA 6; 8% | MSSA2; 4% |
| Enterococcus faecalis 2; 4% | E coli 5; 6% including ESBL(+)1; 1% | Enterococcus faecium 1; 1% | Serratia marcescens 2; 4% |
| Others 8; 16% | Others 12; 15% | Others 5; 7% | Others 6; 12% including ESBL(+) 1; 2% |
| Type of Observation | Percentage of Implementation of Recommendations (%) |
|---|---|
| Raising the head of the bed 30–50% | 94.18% |
| Subglacial suction | 5% |
| Tracheostomy tube balloon pressure >20 cmH20 | 81.7% |
| Prevention of stress ulcers | 70.79% |
| Oral rinse with disinfectant | 83.24% |
| Ventilation ducts devoid of bronchial secretions | 95.5% |
| Antithrombotic prophylaxis | 84.75% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duszynska, W.; Idziak, M.; Smardz, K.; Burkot, A.; Grotowska, M.; Rojek, S. Frequency, Etiology, Mortality, Cost, and Prevention of Respiratory Tract Infections—Prospective, One Center Study. J. Clin. Med. 2022, 11, 3764. https://doi.org/10.3390/jcm11133764
Duszynska W, Idziak M, Smardz K, Burkot A, Grotowska M, Rojek S. Frequency, Etiology, Mortality, Cost, and Prevention of Respiratory Tract Infections—Prospective, One Center Study. Journal of Clinical Medicine. 2022; 11(13):3764. https://doi.org/10.3390/jcm11133764
Chicago/Turabian StyleDuszynska, Wieslawa, Marta Idziak, Klaudia Smardz, Anna Burkot, Malgorzata Grotowska, and Stanislaw Rojek. 2022. "Frequency, Etiology, Mortality, Cost, and Prevention of Respiratory Tract Infections—Prospective, One Center Study" Journal of Clinical Medicine 11, no. 13: 3764. https://doi.org/10.3390/jcm11133764
APA StyleDuszynska, W., Idziak, M., Smardz, K., Burkot, A., Grotowska, M., & Rojek, S. (2022). Frequency, Etiology, Mortality, Cost, and Prevention of Respiratory Tract Infections—Prospective, One Center Study. Journal of Clinical Medicine, 11(13), 3764. https://doi.org/10.3390/jcm11133764






