The Etiology and Epidemiology of Pediatric Facial Fractures in North-Western Romania: A 10-Year Retrospective Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Considerations
2.2. Participants and Data Collection
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Manodh, P.; Prabhu Shankar, D.; Pradeep, D.; Santhosh, R.; Murugan, A. Incidence and patterns of maxillofacial trauma-a retrospective analysis of 3611 patients—An update. Oral Maxillofac. Surg. 2016, 20, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Juncar, M.; Tent, P.A.; Juncar, R.I.; Harangus, A.; Mircea, R. An epidemiological analysis of maxillofacial fractures: A 10-year cross-sectional cohort retrospective study of 1007 patients. BMC Oral Health 2021, 21, 128. [Google Scholar] [CrossRef] [PubMed]
- Chukwulebe, S.; Hogrefe, C. The Diagnosis and Management of Facial Bone Fractures. Emerg. Med. Clin. N. Am. 2019, 37, 137–151. [Google Scholar] [CrossRef] [PubMed]
- Vyas, R.M.; Dickinson, B.P.; Wasson, K.L.; Roostaeian, J.; Bradley, J.P. Pediatric facial fractures: Current national incidence, distribution, and health care resource use. J. Craniofac. Surg. 2008, 19, 339–349. [Google Scholar] [CrossRef]
- Boyette, J.R. Facial fractures in children. Otolaryngol. Clin. N. Am. 2014, 47, 747–761. [Google Scholar] [CrossRef]
- Gassner, R.; Tuli, T.; Hächl, O.; Moreira, R.; Ulmer, H. Craniomaxillofacial trauma in children: A review of 3,385 cases with 6060 injuries in 10 years. J. Oral Maxillofac. Surg. 2004, 62, 399–407. [Google Scholar] [CrossRef]
- Nardis Ada, C.; Costa, S.A.; da Silva, R.A.; Kaba, S.C. Patterns of paediatric facial fractures in a hospital of São Paulo, Brazil: A retrospective study of 3 years. J. Craniomaxillofac. Surg. 2013, 41, 226–229. [Google Scholar] [CrossRef]
- Dobitsch, A.A.; Oleck, N.C.; Liu, F.C.; Halsey, J.N.; Hoppe, I.C.; Lee, E.S.; Granick, M.S. Sports-Related Pediatric Facial Trauma: Analysis of Facial Fracture Pattern and Concomitant Injuries. Surg. J. 2019, 5, e146–e149. [Google Scholar] [CrossRef]
- Montovani, J.C.; de Campos, L.M.; Gomes, M.A.; de Moraes, V.R.; Ferreira, F.D.; Nogueira, E.A. Etiology and incidence facial fractures in children and adults. Braz. J. Otorhinolaryngol. 2006, 72, 235–241. [Google Scholar] [CrossRef] [Green Version]
- Berthold, O.; Frericks, B.; John, T.; Clemens, V.; Fegert, J.M.; Moers, A.V. Abuse as a Cause of Childhood Fractures. Dtsch. Arztebl. Int. 2018, 115, 769–775. [Google Scholar] [CrossRef]
- Bakardjiev, A.; Pechalova, P. Maxillofacial fractures in Southern Bulgaria—A retrospective study of 1706 cases. J. Craniomaxillofac. Surg. 2007, 35, 147–150. [Google Scholar] [CrossRef]
- Cole, P.; Kaufman, Y.; Hollier, L.H., Jr. Managing the pediatric facial fracture. Craniomaxillofac. Trauma Reconstr. 2009, 2, 77–83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goth, S.; Sawatari, Y.; Peleg, M. Management of pediatric mandible fractures. J. Craniofac. Surg. 2012, 23, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Hatef, D.A.; Cole, P.D.; Hollier, L.H., Jr. Contemporary management of pediatric facial trauma. Curr. Opin. Otolaryngol. Head Neck Surg. 2009, 17, 308–314. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, C.E.; Troulis, M.J.; Kaban, L.B. Pediatric facial fractures: Recent advances in prevention, diagnosis and management. Int. J. Oral Maxillofac. Surg. 2006, 35, 2–13. [Google Scholar] [CrossRef] [PubMed]
- Imahara, S.D.; Hopper, R.A.; Wang, J.; Rivara, F.P.; Klein, M.B. Patterns and outcomes of pediatric facial fractures in the United States: A survey of the National Trauma Data Bank. J. Am. Coll. Surg. 2008, 207, 710–716. [Google Scholar] [CrossRef] [Green Version]
- Grunwaldt, L.; Smith, D.M.; Zuckerbraun, N.S.; Naran, S.; Rottgers, S.A.; Bykowski, M.; Kinsella, C.; Cray, J.; Vecchione, L.; Saladino, R.A.; et al. Pediatric facial fractures: Demographics, injury patterns, and associated injuries in 772 consecutive patients. Plast. Reconstr. Surg. 2011, 128, 1263–1271. [Google Scholar] [CrossRef] [PubMed]
- Alcalá-Galiano, A.; Arribas-García, I.J.; Martín-Pérez, M.A.; Romance, A.; Montalvo-Moreno, J.J.; Juncos, J.M. Pediatric facial fractures: Children are not just small adults. Radiographics 2008, 28, 441–461, quiz 618. [Google Scholar] [CrossRef]
- Braun, T.L.; Xue, A.S.; Maricevich, R.S. Differences in the Management of Pediatric Facial Trauma. Semin. Plast. Surg. 2017, 31, 118–122. [Google Scholar] [CrossRef] [Green Version]
- Al-Tairi, N.; Al-Radom, J. Prevalence and Etiology of Pediatric Maxillofacial Fractures in a Group of Yemeni Children and Adolescents. Open J. Stomatol. 2021, 11, 179–187. [Google Scholar] [CrossRef]
- Almahdi, H.M.; Higzi, M.A. Maxillofacial fractures among Sudanese children at Khartoum Dental Teaching Hospital. BMC Res. Notes 2016, 9, 120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ashrafullah; Pandey, R.K.; Mishra, A. The incidence of facial injuries in children in Indian population: A retrospective study. J. Oral Biol. Craniofac. Res. 2018, 8, 82–85. [Google Scholar] [CrossRef] [PubMed]
- Segura-Palleres, I.; Sobrero, F.; Roccia, F.; de Oliveira Gorla, L.F.; Pereira-Filho, V.A.; Gallafassi, D.; Faverani, L.P.; Romeo, I.; Bojino, A.; Copelli, C.; et al. Characteristics and age-related injury patterns of maxillofacial fractures in children and adolescents: A multicentric and prospective study. Dent. Traumatol. 2022, 38, 213–222. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, R.; Gopalkrishnan, K.; Anand, J. Pediatric Facial Fractures: A 10-year Study. J. Maxillofac. Oral Surg. 2018, 17, 158–163. [Google Scholar] [CrossRef]
- Posnick, J.C.; Wells, M.; Pron, G.E. Pediatric facial fractures: Evolving patterns of treatment. J. Oral Maxillofac. Surg. 1993, 51, 836Y844. [Google Scholar] [CrossRef]
- Jaworska, N.; MacQueen, G. Adolescence as a unique developmental period. J. Psychiatry Neurosci. 2015, 40, 291–293. [Google Scholar] [CrossRef]
- Johnson, S.B.; Jones, V.C. Adolescent development and risk of injury: Using developmental science to improve interventions. Inj. Prev. 2011, 17, 50–54. [Google Scholar] [CrossRef] [Green Version]
- Iizuka, T.; Thoren, H.; Annino, D.J.; Hallikainen, D.; Lindqvist, C. Midfacial fractures in pediatric patients. Frequency, characteristics, and causes. Arch. Otolaryngol. Head Neck Surg. 1995, 121, 1366Y1371. [Google Scholar] [CrossRef]
- Haug, R.H.; Foss, J. Maxillofacial injuries in the pediatric patient. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2000, 90, 126–134. [Google Scholar] [CrossRef]
- Mukherjee, C.G.; Mukherjee, U. Maxillofacial trauma in children. Int. J. Clin. Pediatr. Dent. 2012, 5, 231–236. [Google Scholar] [CrossRef]
- Kim, S.H.; Lee, S.H.; Cho, P.D. Analysis of 809 facial bone fractures in a pediatric and adolescent population. Arch. Plast. Surg. 2012, 39, 606–611. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shetawi, A.S.; Lim, C.A.; Singh, Y.K.; Portnof, J.E.; Blumberg, S.M. Pediatric maxillofacial trauma: A review of 156 patients. J. Oral Maxillofacial. Surg. 2016, 74, 1420. [Google Scholar] [CrossRef] [PubMed]
- Hong, K.; Jeong, J.; Susson, Y.N.; Abramowicz, S. Patterns of Pediatric Facial Fractures. Craniomaxillofac. Trauma Reconstr. 2021, 14, 325–329. [Google Scholar] [CrossRef] [PubMed]
- Gadicherla, S.; Sasikumar, P.; Gill, S.S.; Bhagania, M.; Kamath, A.T.; Pentapati, K.C. Mandibular Fractures and Associated Factors at a Tertiary Care Hospital. Arch. Trauma Res. 2016, 5, e30574. [Google Scholar] [CrossRef] [Green Version]
- Ferreira, P.; Marques, M.; Pinho, C.; Rodrigues, J.; Reis, J.; Amarante, J. Midfacial fractures in children and adolescents: A review of 492 cases. Br. J. Oral Maxillofac. Surg. 2004, 42, 501–505. [Google Scholar] [CrossRef]
- Hyman, D.A.; Saha, S.; Nayar, H.S.; Doyle, J.F.; Agarwal, S.K.; Chaiet, S.R. Patterns of facial fractures and protective device use in motor vehicle collisions from 2007 to 2012. JAMA Facial Plast. Surg. 2016, 18, 455–461. [Google Scholar] [CrossRef] [Green Version]
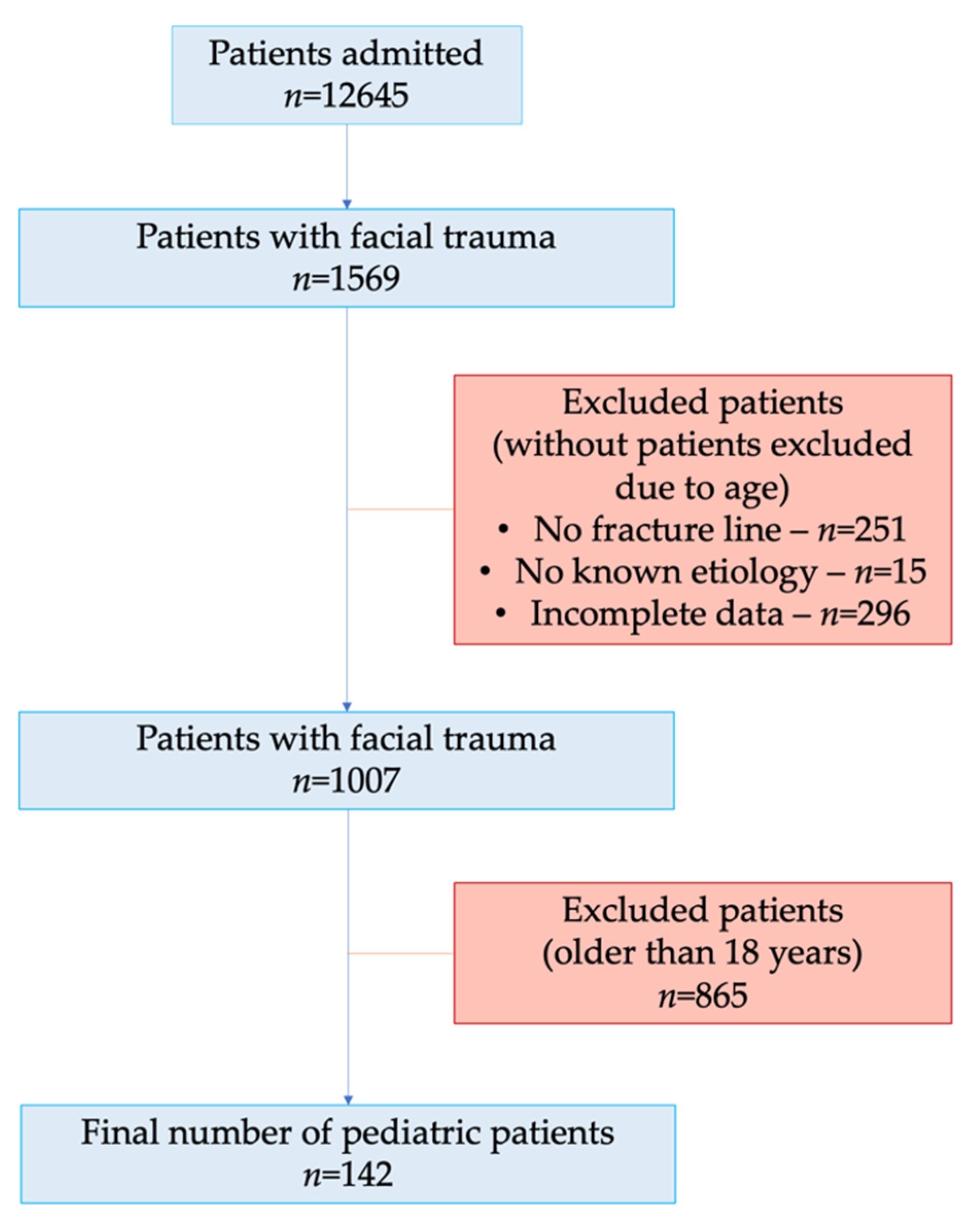


| Variable | Value |
|---|---|
| Age (n, %) | |
| >18 years | 865 (85.9%) |
| ≤18 years | 142 (14.1%) |
| Age groups (n, %) | |
| 0–6 years | 8 (5.6%) (0.8% from all facial fractures) |
| 7–12 years | 22 (15.5%) (2.2% from all facial fractures) |
| 13–18 years | 112 (78.9%) (11.1% from all facial fractures) |
| Gender (n, %) | |
| Girls | 17 (12%) |
| Boys | 125 (88%) |
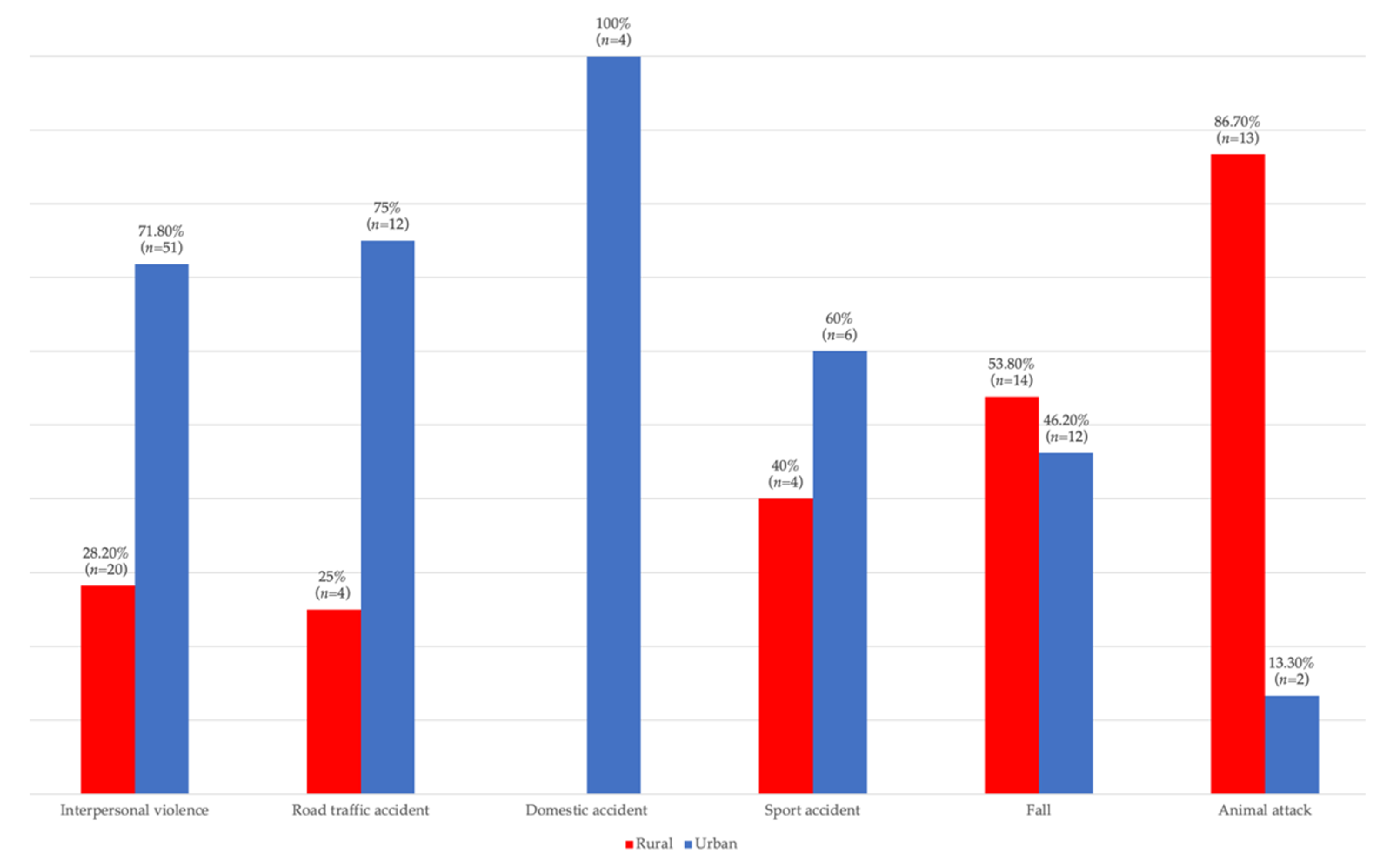
| Living environment (n, %) | |
| Rural | 55 (38.7%) |
| Urban | 87 (61.3%) |
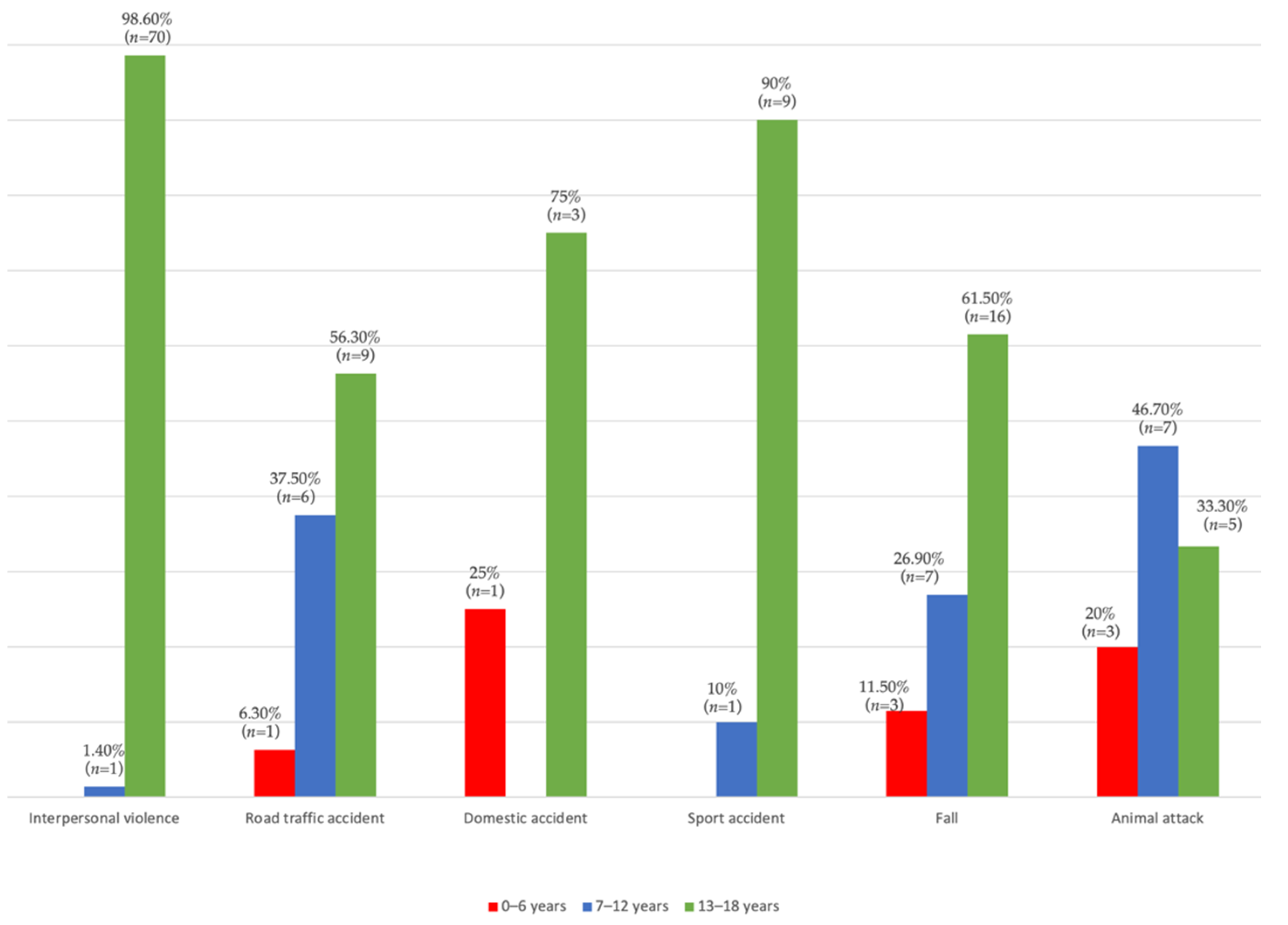
| Etiology (n, %) | |
| Interpersonal violence | 71 (50%) |
| Fall | 26 (18.3%) |
| Road traffic accident | 16 (11.3%) |
| Animal attack | 15 (10.6%) |
| Sport accident | 10 (7%) |
| Domestic accident | 4 (2.8%) |
| Fracture line location (n, %) | |
| Mandibular fractures | 94 (66.2%) |
| Midface fractures | 36 (25.3%) |
| Combined fractures | 12 (8.5%) |
| Soft tissue associated lesions (n, %) | |
| Hematomas | 62 (43.7%) |
| Lacerations | 40 (28.2%) |
| Abrasions | 47 (33.1%) |
| Etiology | Interpersonal Violence | Road Traffic Accident | Domestic Accident | Sport Accident | Fall | Animal Attack | p * | |
|---|---|---|---|---|---|---|---|---|
| Hematomas | ||||||||
| No | n | 56 | 3 | 2 | 4 | 12 | 3 | <0.001 |
| % | 78.9% | 18.8% | 50% | 40% | 46.2% | 20% | ||
| Yes | n | 15 | 13 | 2 | 6 | 14 | 12 | |
| % | 21.1% | 81.3% | 50% | 60% | 53.8% | 80% | ||
| Lacerations | ||||||||
| No | n | 64 | 7 | 2 | 10 | 13 | 6 | <0.001 |
| % | 90.1% | 43.8% | 50% | 100% | 50% | 40% | ||
| Yes | n | 7 | 9 | 2 | 0 | 13 | 9 | |
| % | 9.9% | 56.3% | 50% | 0% | 50% | 60% | ||
| Abrasions | ||||||||
| No | n | 61 | 3 | 2 | 10 | 13 | 6 | <0.001 |
| % | 85.9% | 18.8% | 50% | 100% | 50% | 40% | ||
| Yes | n | 10 | 13 | 2 | 0 | 13 | 9 | |
| % | 14.1% | 81.3% | 50% | 0% | 50% | 60% | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Țenț, P.A.; Juncar, R.I.; Moca, A.E.; Moca, R.T.; Juncar, M. The Etiology and Epidemiology of Pediatric Facial Fractures in North-Western Romania: A 10-Year Retrospective Study. Children 2022, 9, 932. https://doi.org/10.3390/children9070932
Țenț PA, Juncar RI, Moca AE, Moca RT, Juncar M. The Etiology and Epidemiology of Pediatric Facial Fractures in North-Western Romania: A 10-Year Retrospective Study. Children. 2022; 9(7):932. https://doi.org/10.3390/children9070932
Chicago/Turabian StyleȚenț, Paul Andrei, Raluca Iulia Juncar, Abel Emanuel Moca, Rahela Tabita Moca, and Mihai Juncar. 2022. "The Etiology and Epidemiology of Pediatric Facial Fractures in North-Western Romania: A 10-Year Retrospective Study" Children 9, no. 7: 932. https://doi.org/10.3390/children9070932
APA StyleȚenț, P. A., Juncar, R. I., Moca, A. E., Moca, R. T., & Juncar, M. (2022). The Etiology and Epidemiology of Pediatric Facial Fractures in North-Western Romania: A 10-Year Retrospective Study. Children, 9(7), 932. https://doi.org/10.3390/children9070932








