The Associations of Suspected COVID-19 Symptoms with Anxiety and Depression as Modified by Hemodialysis Dietary Knowledge: A Multi-Dialysis Center Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Sample
2.2. Measurements
2.2.1. Suspected COVID-19 Symptoms
2.2.2. Anxiety
2.2.3. Depression
2.2.4. Hemodialysis Dietary Knowledge
2.2.5. Covariates
2.3. Data Collection Procedure
2.4. Data Analysis
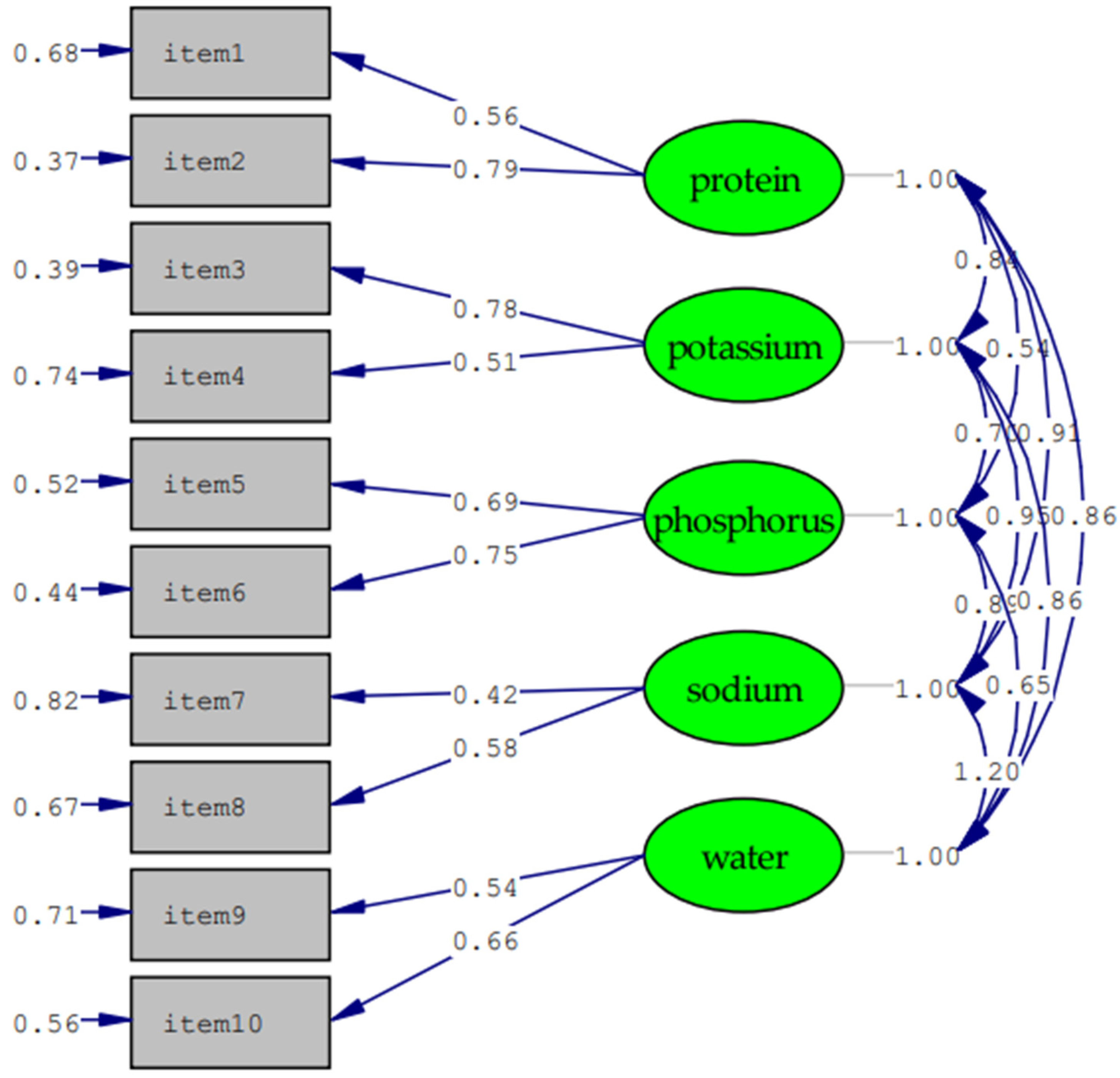
2.4.1. Psychometric Properties of the HDK
2.4.2. Associated Factors for Anxiety, Depression and Effect Modification of HDK
3. Results
3.1. Participants’ Socio-Demographics
3.2. Psychometric Properties of Hemodialysis Dietary Knowledge
3.3. Associated Factors of Anxiety and Depression
3.4. Modification Impacts of Hemodialysis Dietary Knowledge
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Goh, Z.S.; Griva, K. Anxiety and depression in patients with end-stage renal disease: Impact and management challenges—A narrative review. Int. J. Nephrol. Renov. Dis. 2018, 11, 93–102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ng, H.J.; Tan, W.J.; Mooppil, N.; Newman, S.; Griva, K. Prevalence and patterns of depression and anxiety in hemodialysis patients: A 12-month prospective study on incident and prevalent populations. Br. J. Health Psychol. 2015, 20, 374–395. [Google Scholar] [CrossRef]
- Alencar, S.B.V.; de Lima, F.M.; Dias, L.D.A.; Dias, V.D.A.; Lessa, A.C.; Bezerra, J.M.; Apolinário, J.F.; de Petribu, K.C. Depression and quality of life in older adults on hemodialysis. Rev. Bras. De Psiquiatr. 2020, 42, 195–200. [Google Scholar] [CrossRef] [Green Version]
- Brito, D.C.S.; Machado, E.L. Depression and anxiety among patients undergoing dialysis and kidney transplantation: A cross-sectional study. Sao Paulo Med. J. 2019, 137, 137–147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marthoenis, M.; Syukri, M.; Abdullah, A.; Tandi, T.M.R.; Putra, N.; Laura, H.; Setiawan, A.; Sofyan, H.; Schouler-Ocak, M. Quality of life, depression, and anxiety of patients undergoing hemodialysis: Significant role of acceptance of the illness. Int. J Psychiatry Med. 2021, 56, 40–50. [Google Scholar] [CrossRef]
- Khan, A.; Khan, A.H.; Adnan, A.S.; Sulaiman, S.A.S.; Mushtaq, S. Prevalence and predictors of depression among hemodialysis patients: A prospective follow-up study. BMC Public Health 2019, 19, 531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kauric-Klein, Z. Depression and Medication Adherence in Patients on Hemodialysis. Curr. Hypertens. Rev. 2017, 13, 138–143. [Google Scholar] [CrossRef]
- Schouten, R.W.; Haverkamp, G.L.; Loosman, W.L.; Chandie Shaw, P.K.; van Ittersum, F.J.; Smets, Y.F.C.; Vleming, L.J.; Dekker, F.W.; Honig, A.; Siegert, C.E.H. Anxiety Symptoms, Mortality, and Hospitalization in Patients Receiving Maintenance Dialysis: A Cohort Study. Am. J. Kidney Dis. 2019, 74, 158–166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, P.H.; Lin, M.Y.; Huang, T.H.; Lin, Y.T.; Hung, C.C.; Yeh, Y.C.; Kuo, H.T.; Chiu, Y.W.; Hwang, S.J.; Tsai, J.C.; et al. Depression amongst patients commencing maintenance dialysis is associated with increased risk of death and severe infections: A nationwide cohort study. PLoS ONE 2019, 14, e0218335. [Google Scholar] [CrossRef] [PubMed]
- Farrokhi, F.; Abedi, N.; Beyene, J.; Kurdyak, P.; Jassal, S.V. Association between depression and mortality in patients receiving long-term dialysis: A systematic review and meta-analysis. Am. J. Kidney Dis. 2014, 63, 623–635. [Google Scholar] [CrossRef]
- Keskin, G.; Engin, E. The evaluation of depression, suicidal ideation and coping strategies in haemodialysis patients with renal failure. J. Clin. Nurs. 2011, 20, 2721–2732. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.K.; Tsai, Y.C.; Hsu, H.J.; Wu, I.W.; Sun, C.Y.; Chou, C.C.; Lee, C.C.; Tsai, C.R.; Wu, M.S.; Wang, L.J. Depression and suicide risk in hemodialysis patients with chronic renal failure. Psychosomatics 2010, 51, 528–528.e6. [Google Scholar] [CrossRef]
- Hedayati, S.S.; Yalamanchili, V.; Finkelstein, F.O. A practical approach to the treatment of depression in patients with chronic kidney disease and end-stage renal disease. Kidney Int. 2012, 81, 247–255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patel, M.P.; Kute, V.B.; Prasad, N.; Agarwal, S.K.; COVID-19 Working Group of Indian Society of Nephrology. COVID 19 and Hemodialysis Anxiety. Indian J. Nephrol. 2020, 30, 174–175. [Google Scholar] [CrossRef] [PubMed]
- Ghonimi, T.A.L.; Alkad, M.M. Mortality and associated risk factors of COVID-19 infection in dialysis patients in Qatar: A nationwide cohort study. PLoS ONE 2021, 16, e0254246. [Google Scholar] [CrossRef]
- Creput, C.; Fumeron, C.; Toledano, D.; Diaconita, M.; Izzedine, H. COVID-19 in Patients Undergoing Hemodialysis: Prevalence and Asymptomatic Screening During a Period of High Community Prevalence in a Large Paris Center. Kidney Med. 2020, 2, 716–723.e1. [Google Scholar] [CrossRef]
- Rodríguez-Espinosa, D.; Broseta, J.J. Prevalence of COVID-19 Infection in Hemodialysis Patients Detected Using Serologic Screening. J. Am. Soc. Nephrol. 2020, 31, 2966–2967. [Google Scholar] [CrossRef]
- Chen, C.Y.; Shao, S.C.; Chen, Y.T.; Hsu, C.K.; Hsu, H.J.; Lee, C.C.; Sun, C.Y.; Chen, Y.C.; Hung, M.J.; Wu, I.W. Incidence and Clinical Impacts of COVID-19 Infection in Patients with Hemodialysis: Systematic Review and Meta-Analysis of 396,062 Hemodialysis Patients. Healthcare 2021, 9, 47. [Google Scholar] [CrossRef]
- Delgado-Domínguez, C.J.; Sanz-Gómez, S. Influence of Depression and Anxiety on Hemodialysis Patients: The Value of Multidisciplinary Care. Int. J. Environ. Res. Public Health 2021, 18, 3544. [Google Scholar] [CrossRef]
- Hou, Y.; Li, X.; Yang, L.; Liu, C.; Wu, H.; Xu, Y.; Yang, F.; Du, Y. Factors associated with depression and anxiety in patients with end-stage renal disease receiving maintenance hemodialysis. Int. Urol. Nephrol. 2014, 46, 1645–1649. [Google Scholar] [CrossRef]
- Theofilou, P. Depression and anxiety in patients with chronic renal failure: The effect of sociodemographic characteristics. Int. J. Nephrol. 2011, 2011, 514070. [Google Scholar] [CrossRef] [Green Version]
- Mosleh, H.; Alenezi, M.; Al Johani, S.; Alsani, A.; Fairaq, G.; Bedaiwi, R. Prevalence and Factors of Anxiety and Depression in Chronic Kidney Disease Patients Undergoing Hemodialysis: A Cross-sectional Single-Center Study in Saudi Arabia. Cureus 2020, 12, e6668. [Google Scholar] [CrossRef] [Green Version]
- Al Naamani, Z.; Gormley, K.; Noble, H.; Santin, O.; Al Maqbali, M. Fatigue, anxiety, depression and sleep quality in patients undergoing haemodialysis. BMC Nephrol. 2021, 22, 157. [Google Scholar] [CrossRef]
- Hao, W.; Tang, Q.; Huang, X.; Ao, L.; Wang, J.; Xie, D. Analysis of the prevalence and influencing factors of depression and anxiety among maintenance dialysis patients during the COVID-19 pandemic. Int. Urol. Nephrol. 2021, 53, 1453–1461. [Google Scholar] [CrossRef]
- Nguyen, M.H.; Pham, T.T.M.; Pham, L.V.; Phan, D.T.; Tran, T.V.; Nguyen, H.C.; Nguyen, H.C.; Ha, T.H.; Dao, H.K.; Nguyen, P.B.; et al. Associations of Underlying Health Conditions with Anxiety and Depression Among Outpatients: Modification Effects of Suspected COVID-19 Symptoms, Health-Related and Preventive Behaviors. Int. J. Public Health 2021, 66, 634904. [Google Scholar] [CrossRef]
- Nguyen, H.C.; Nguyen, M.H.; Do, B.N. People with Suspected COVID-19 Symptoms Were More Likely Depressed and Had Lower Health-Related Quality of Life: The Potential Benefit of Health Literacy. J. Clin. Med. 2020, 9, 965. [Google Scholar] [CrossRef] [Green Version]
- Kauric-Klein, Z. Sodium Knowledge, Beliefs, and Behaviors in Patients on Chronic Hemodialysis. Blood Purif. 2020, 49, 25–32. [Google Scholar] [CrossRef]
- Zhang, X.; Chen, B.; Jia, P.; Han, J. Locked on salt? Excessive consumption of high-sodium foods during COVID-19 presents an underappreciated public health risk: A review. Environ. Chem. Lett. 2021, 19, 3583–3595. [Google Scholar] [CrossRef]
- Cheikh Ismail, L.; Osaili, T.M.; Mohamad, M.N.; Al Marzouqi, A.; Jarrar, A.H.; Zampelas, A.; Habib-Mourad, C.; Omar Abu Jamous, D.; Ali, H.I.; Al Sabbah, H.; et al. Assessment of eating habits and lifestyle during the coronavirus 2019 pandemic in the Middle East and North Africa region: A cross-sectional study. Br. J. Nutr. 2020, 126, 757–766. [Google Scholar] [CrossRef]
- Pham, K.M.; Pham, L.V.; Phan, D.T.; Tran, T.V.; Nguyen, H.C.; Nguyen, M.H.; Nguyen, H.C.; Ha, T.H.; Dao, H.K.; Nguyen, P.B.; et al. Healthy Dietary Intake Behavior Potentially Modifies the Negative Effect of COVID-19 Lockdown on Depression: A Hospital and Health Center Survey. Front. Nutr. 2020, 7, 581043. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Editorial Team. Overview of Novel Coronavirus. BMJ Best Practice: 2020. Available online: https://bestpractice.bmj.com/topics/en-gb/3000165 (accessed on 10 February 2020).
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [Green Version]
- Alshraifeen, A.; Alnuaimi, K.; Al-Rawashdeh, S.; Ashour, A.; Al-Ghabeesh, S.; Al-Smadi, A. Spirituality, Anxiety and Depression Among People Receiving Hemodialysis Treatment in Jordan: A Cross-Sectional Study. J. Relig. Health 2020, 59, 2414–2429. [Google Scholar] [CrossRef] [PubMed]
- Luong, T.C.; Pham, T.T.M.; Nguyen, M.H.; Do, A.Q.; Pham, L.V.; Nguyen, H.C.; Nguyen, H.C.; Ha, T.H.; Dao, H.K.; Trinh, M.V.; et al. Fear, anxiety and depression among pregnant women during COVID-19 pandemic: Impacts of healthy eating behaviour and health literacy. Ann. Med. 2021, 53, 2120–2131. [Google Scholar] [CrossRef]
- Mughal, A.Y.; Stockton, M.A.; Bui, Q.; Go, V.; Ha, T.V.; Pence, B.W.; Gaynes, B.N. Validation of screening tools for common mental health disorders in the methadone maintenance population in Hanoi, Vietnam. BMC Psychiatry 2021, 21, 488. [Google Scholar] [CrossRef]
- Plummer, F.; Manea, L.; Trepel, D.; McMillan, D. Screening for anxiety disorders with the GAD-7 and GAD-2: A systematic review and diagnostic metaanalysis. Gen. Hosp. Psychiatry 2016, 39, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Nguyen, N.; An, P.; Tien, N. Reliability and Validity of Vietnamese Version of Patient Health Questionnaire 9 Items (PHQ-9) Among UMP Medical Freshmen. In International Conference on the Development of Biomedical Engineering in Vietnam; Springer: Berlin/Heidelberg, Germany, 2022; pp. 901–923. [Google Scholar] [CrossRef]
- Trotter, T.L.; Denny, D.L.; Evanson, T.A. Reliability and Validity of the Patient Health Questionnaire-9 as a Screening Tool for Poststroke Depression. J. Neurosci. Nurs. 2019, 51, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Thomas, Z.; Novak, M.; Platas, S.G.T.; Gautier, M.; Holgin, A.P.; Fox, R.; Segal, M.; Looper, K.J.; Lipman, M.; Selchen, S.; et al. Brief Mindfulness Meditation for Depression and Anxiety Symptoms in Patients Undergoing Hemodialysis: A Pilot Feasibility Study. Clin. J. Am. Soc. Nephrol. 2017, 12, 2008–2015. [Google Scholar] [CrossRef]
- Ryu, H.; Jeon, H.J.; Sun, H.-K.; Han, K.H.; Whang, C.G.; Han, S.Y. Repeated education improves diet compliance in maintenance Hemodialysis Patients. Int. Urol. Nephrol. 2014, 2, 63–68. [Google Scholar]
- Nguyen, T.T.; Nguyen, M.H.; Pham, T.T.M.; Le, V.T.; Nguyen, T.T.; Luong, T.C.; Do, B.N.; Dao, H.K.; Nguyen, H.C.; Ha, T.H.; et al. Negative Impacts of COVID-19 Induced Lockdown on Changes in Eating Behavior, Physical Activity, and Mental Health as Modified by Digital Healthy Diet Literacy and eHealth Literacy. Front. Nutr. 2021, 8, 774328. [Google Scholar] [CrossRef] [PubMed]
- Hemmelgarn, B.R.; Manns, B.J.; Quan, H.; Ghali, W.A. Adapting the Charlson Comorbidity Index for use in patients with ESRD. Am. J. Kidney Dis. 2003, 42, 125–132. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [Green Version]
- Pham, T.; Bui, L.; Nguyen, A.; Nguyen, B.; Tran, P. The prevalence of depression and associated risk factors among medical students: An untold story in Vietnam. PLoS ONE 2019, 14, e0221432. [Google Scholar] [CrossRef]
- Nguyen, L.T.K.; Do, B.N. Physical Activity and Diet Quality Modify the Association between Comorbidity and Disability among Stroke Patients. Nutrients 2021, 13, 1641. [Google Scholar] [CrossRef]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.H.; Stewart, S.M. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): A systematic review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duong, T.V.; Aringazina, A.; Kayupova, G.; Nurjanah; Pham, T.V.; Pham, K.M.; Truong, T.Q.; Nguyen, K.T.; Oo, W.M.; Su, T.T.; et al. Development and Validation of a New Short-Form Health Literacy Instrument (HLS-SF12) for the General Public in Six Asian Countries. Health Lit. Res. Pract. 2019, 3, e91–e102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duong, T.V.; Pham, K.M. Digital Healthy Diet Literacy and Self-Perceived Eating Behavior Change during COVID-19 Pandemic among Undergraduate Nursing and Medical Students: A Rapid Online Survey. Int. J. Environ. Res. Public Health 2020, 17, 7185. [Google Scholar] [CrossRef]
- HLS-EU Consortium. Comparative Report of Health Literacy in Eight EU Member States. The European Health Literacy Project 2009–2012. Available online: https://www.healthliteracyeurope.net/hls-eu (accessed on 22 October 2012).
- WHO. Coronavirus Disease (COVID-19) Technical Guidance: Infection Prevention and Control/Wash. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/infection-prevention-and-control (accessed on 20 May 2020).
- Jöreskog, K.G.; Sörbom, D. LISREL 8.80 for Windows [Computer Software]; Scientific Software International, Inc.: Lincolnwood, IL, USA, 2006. [Google Scholar]
- Hooper, D.; Coughlan, J.; Mullen, M.R. Structural Equation Modelling: Guidelines for Determining Model Fit. Electron. J. Bus. Res. Methods 2008, 6, 53–60. [Google Scholar]
- Joreskog, K.G.; Sorbom, D. LISREL 7: User’s Reference Guide; Scientific Software: Chicago, IL, USA, 1989. [Google Scholar]
- Kimberlin, C.L.; Winterstein, A.G. Validity and reliability of measurement instruments used in research. Am. J. Health Syst. Pharm. 2008, 65, 2276–2284. [Google Scholar] [CrossRef]
- Terwee, C.B.; Bot, S.D.; de Boer, M.R.; van der Windt, D.A.; Knol, D.L.; Dekker, J.; Bouter, L.M.; de Vet, H.C. Quality criteria were proposed for measurement properties of health status questionnaires. J. Clin. Epidemiol. 2007, 60, 34–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- George, D.; Mallery, P. SPSS for Windows Step by Step: A Simple Guide and Reference, 4th ed.; Allyn & Bacon: Boston, MA, USA, 2003. [Google Scholar]
- Maldonado, G.; Greenland, S. Simulation study of confounder-selection strategies. Am. J. Epidemiol. 1993, 138, 923–936. [Google Scholar] [CrossRef] [Green Version]
- Oginni, O.A.; Oloniniyi, I.O.; Ibigbami, O.; Ugo, V.; Amiola, A.; Ogunbajo, A. Depressive and anxiety symptoms and COVID-19-related factors among men and women in Nigeria. PLoS ONE 2021, 16, e0256690. [Google Scholar] [CrossRef]
- Ejaz, H.; Alsrhani, A.; Zafar, A.; Javed, H.; Junaid, K.; Abdalla, A.E.; Abosalif, K.O.A.; Ahmed, Z.; Younas, S. COVID-19 and comorbidities: Deleterious impact on infected patients. J. Infect. Public Health 2020, 13, 1833–1839. [Google Scholar] [CrossRef] [PubMed]
- Pafili, Z.; Maridaki, M.; Giannaki, C.D.; Karatzaferi, C.; Liakopoulos, V.; Eleftheriadis, T.; Stefanidis, I.; Sakkas, G.K. Phosphorus nutritional knowledge among dialysis health care providers and patients: A multicenter observational study. Clin. Nutr. ESPEN 2019, 31, 33–37. [Google Scholar] [CrossRef] [PubMed]
- Montazeri, R.; Sharifi, N. Evaluation of Nutritional Knowledge in Terms of Dietary Sources of Protein, Phosphorous, Potassium and Fluids Restriction in Hemodialysis Patients. Available online: https://brieflands.com/articles/jjcmb-21832.html (accessed on 19 May 2022).
- Noori, N.; Kalantar-Zadeh, K.; Kovesdy, C.P.; Murali, S.B.; Bross, R.; Nissenson, A.R.; Kopple, J.D. Dietary potassium intake and mortality in long-term hemodialysis patients. Am. J. Kidney Dis. 2010, 56, 338–347. [Google Scholar] [CrossRef] [Green Version]
- Noori, N.; Kalantar-Zadeh, K.; Kovesdy, C.P.; Bross, R.; Benner, D.; Kopple, J.D. Association of dietary phosphorus intake and phosphorus to protein ratio with mortality in hemodialysis patients. Clin. J. Am. Soc. Nephrol. 2010, 5, 683–692. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gebrie, M.H.; Ford, J. Depressive symptoms and dietary non-adherence among end stage renal disease patients undergoing hemodialysis therapy: Systematic review. BMC Nephrol. 2019, 20, 429. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ebrahimi, H.; Sadeghi, M.; Amanpour, F.; Dadgari, A. Influence of nutritional education on hemodialysis patients’ knowledge and quality of life. Saudi. J. Kidney Dis. Transplant. 2016, 27, 250–255. [Google Scholar] [CrossRef]
- Mafra, D.; Cardozo, L.F.M.F.; Moraes, C.; Moreira, L.S.G.; Teixeira, K.T.R.; Reis, D.C.M.V.; Fanton, S.; Salarolli, R.; Kalantar-Zadeh, K.; Burrowe, J.D. Coronavirus Disease 2019: Quick Diet and Nutrition Guide for Patients with Chronic Kidney Disease. J. Ren. Nutr. 2021, 31, 39–42. [Google Scholar] [CrossRef]
- Dodson, S.; Osicka, T.; Huang, L.; McMahon, L.P.; Roberts, M.A. Multifaceted Assessment of Health Literacy in People Receiving Dialysis: Associations with Psychological Stress and Quality of Life. J. Health Commun. 2016, 21, 91–98. [Google Scholar] [CrossRef]
- Skoumalova, I.; Geckova, A.M. Does Depression and Anxiety Mediate the Relation between Limited Health Literacy and Diet Non-Adherence? Int. J. Environ. Res. Public Health 2020, 17, 7913. [Google Scholar] [CrossRef]
- Tran, T.V.; Nguyen, H.C.; Pham, L.V.; Nguyen, M.H.; Nguyen, H.C.; Ha, T.H.; Phan, D.T.; Dao, H.K.; Nguyen, P.B.; Trinh, M.V.; et al. Impacts and interactions of COVID-19 response involvement, health-related behaviours, health literacy on anxiety, depression and health-related quality of life among healthcare workers: A cross-sectional study. BMJ Open 2020, 10, e041394. [Google Scholar] [CrossRef] [PubMed]
- Alemayehu, Y.H.; Seylania, K.; Bahramnezhad, F. The relationship between health literacy and quality of life among hemodialysis patients: An integrative review. Hum. Antib. 2020, 28, 75–81. [Google Scholar] [CrossRef]
- Li, Y.N.; Shapiro, B.; Kim, J.C.; Zhang, M.; Porszasz, J.; Bross, R.; Feroze, U.; Upreti, R.; Martin, D.; Kalantar-Zadeh, K.; et al. Association between quality of life and anxiety, depression, physical activity and physical performance in maintenance hemodialysis patients. Chronic Dis. Transl. Med. 2016, 2, 110–119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cavanaugh, K.L.; Wingard, R.L.; Hakim, R.M.; Eden, S.; Shintani, A.; Wallston, K.A.; Huizinga, M.M.; Elasy, T.A.; Rothman, R.L.; Ikizler, T.A. Low health literacy associates with increased mortality in ESRD. J. Am. Soc. Nephrol. 2010, 21, 1979–1985. [Google Scholar] [CrossRef] [Green Version]
- Khamis, S.; Emara, M.; Elnashar, M.; Khalil, M.; Kasemy, Z. Development of Health Literacy for Regular Hemodialysis Patients in Menoufia Governorate: A Cross-Sectional Study. Open J. Nephrol. 2021, 11, 199–216. [Google Scholar] [CrossRef]
- Dziubek, W.; Kowalska, J.; Kusztal, M.; Rogowski, Ł.; Gołębiowski, T.; Nikifur, M.; Szczepańska-Gieracha, J.; Zembroń-Łacny, A.; Klinger, M.; Woźniewski, M. The Level of Anxiety and Depression in Dialysis Patients Undertaking Regular Physical Exercise Training--a Preliminary Study. Kidney Blood Press. Res. 2016, 41, 86–98. [Google Scholar] [CrossRef]
- Puccinelli, P.J.; da Costa, T.S.; Seffrin, A.; de Lira, C.A.B.; Vancini, R.L.; Nikolaidis, P.T.; Knechtle, B.; Rosemann, T.; Hill, L.; Andrade, M.S. Reduced level of physical activity during COVID-19 pandemic is associated with depression and anxiety levels: An internet-based survey. BMC Public Health 2021, 21, 425. [Google Scholar] [CrossRef]
- Kandola, A.; Ashdown-Franks, G.; Hendrikse, J.; Sabiston, C.M.; Stubbs, B. Physical activity and depression: Towards understanding the antidepressant mechanisms of physical activity. Neurosci. Biobehav. Rev. 2019, 107, 525–539. [Google Scholar] [CrossRef]
- Chung, Y.C.; Yeh, M.L.; Liu, Y.M. Effects of intradialytic exercise on the physical function, depression and quality of life for haemodialysis patients: A systematic review and meta-analysis of randomised controlled trials. J. Clin. Nurs. 2017, 26, 1801–1813. [Google Scholar] [CrossRef]
- Pu, J.; Jiang, Z.; Wu, W.; Li, L.; Zhang, L.; Li, Y.; Liu, Q.; Ou, S. Efficacy and safety of intradialytic exercise in haemodialysis patients: A systematic review and meta-analysis. BMJ Open 2019, 9, e020633. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gerogianni, G.; Lianos, E.; Kouzoupis, A.; Polikandrioti, M.; Grapsa, E. The role of socio-demographic factors in depression and anxiety of patients on hemodialysis: An observational cross-sectional study. Int. Urol. Nephrol. 2018, 50, 143–154. [Google Scholar] [CrossRef]

| Variables | Total n (%) | GAD < 8 (n = 577) | GAD ≥ 8 (n = 298) | p | PHQ < 10 (n = 509) | PHQ ≥ 10 (n = 366) | p |
|---|---|---|---|---|---|---|---|
| Age | 0.315 a | 0.082 a | |||||
| 18–59 | 534 (61.0) | 359 (62.2) | 175 (58.7) | 323 (63.5) | 211 (57.7) | ||
| 60–85 | 345 (39.0) | 218 (37.8) | 123 (41.3) | 186 (36.5) | 155 (42.3) | ||
| Gender | 0.128 a | 0.079 a | |||||
| Male | 475 (54.3) | 324 (56.4) | 151 (51.0) | 289 (57.1) | 186 (51.1) | ||
| Female | 395 (45.1) | 250 (43.6) | 145 (49.0) | 217 (42.9) | 178 (48.9) | ||
| Education | 0.840 a | 0.905 a | |||||
| Illiterate or elementary | 353 (43.6) | 237 (44.1) | 116 (42.5) | 207 (44.0) | 146 (42.9) | ||
| Junior high school | 256 (31.6) | 170 (31.7) | 86 (31.5) | 149 (31.7) | 107 (31.5) | ||
| Senior high school or above | 201 (24.8) | 130 (24.2) | 71 (26.0) | 114 (24.3) | 87 (25.6) | ||
| Working status | 0.365 a | 0.118 a | |||||
| Not working | 311 (35.5) | 199 (34.5) | 112 (37.6) | 170 (33.4) | 141 (38.5) | ||
| Working | 564 (64.5) | 378 (65.5) | 186 (62.4) | 339 (66.6) | 225 (61.5) | ||
| Married status | 0.026 a | 0.098 a | |||||
| Never married | 76 (8.7) | 59 (10.2) | 17 (5.7) | 51 (10.0) | 25 (6.8) | ||
| Ever married | 799 (91.3) | 518 (89.8) | 281 (94.3) | 458 (90.0) | 341 (93.2) | ||
| Social status | <0.001 a | <0.001 a | |||||
| Low | 233 (26.6) | 120 (20.8) | 113 (37.9) | 99 (19.4) | 134 (36.6) | ||
| Middle & high | 642 (73.4) | 457 (79.2) | 185 (62.1) | 410 (80.6) | 232 (63.4) | ||
| Medication payment ability | <0.001 a | <0.001 a | |||||
| Very or fairly difficult | 660 (76.7) | 388 (68.4) | 272 (92.5) | 328 (65.5) | 332 (92.2) | ||
| Very or fairly easy | 201 (23.3) | 179 (31.6) | 22 (7.5) | 173 (34.5) | 28 (7.8) | ||
| S-COVID-19-S | <0.001 a | <0.001 a | |||||
| Without S-COVID-19-S | 286 (32.7) | 248 (43.0) | 38 (12.8) | 233 (45.8) | 53 (14.5) | ||
| With S-COVID-19-S | 589 (67.3) | 329 (57.0) | 260 (87.2) | 276 (54.2) | 313 (85.5) | ||
| BMI, kg/m2 | 0.478 a | 0.049 a | |||||
| BMI < 24 | 790 (90.3) | 518 (89.8) | 272 (91.3) | 451 (88.6) | 339 (92.6) | ||
| BMI ≥ 24 | 85 (9.7) | 59 (10.2) | 26 (8.7) | 58 (11.4) | 27 (7.4) | ||
| Edema | <0.001 a | <0.001 a | |||||
| No | 467 (53.4) | 331 (57.4) | 136 (45.6) | 305 (59.9) | 162 (44.3) | ||
| Yes | 408 (46.6) | 246 (42.6) | 162 (54.4) | 204 (40.1) | 204 (55.7) | ||
| Hyperthyroidism | 0.981 a | 0.414 a | |||||
| No | 839 (96.0) | 553 (96.0) | 286 (96.0) | 490 (96.5) | 349 (95.4) | ||
| Yes | 35 (4.0) | 23 (4.0) | 12 (4.0) | 18 (3.5) | 17 (4.6) | ||
| Hospitalization within one month | 0.679 a | 0.106 a | |||||
| No | 817 (93.5) | 537 (93.2) | 280 (94.0) | 469 (92.3) | 348 (95.1) | ||
| Yes | 57 (6.5) | 39 (6.8) | 18 (6.0) | 39 (7.7) | 18 (4.9) | ||
| Physical activity, MET-min/wk | <0.001 a | <0.001 a | |||||
| Tertile 1 (MET ≤ 178) | 204 (31.6) | 105 (23.0) | 99 (52.4) | 72 (17.6) | 132 (55.7) | ||
| Tertile 2 (178 < MET ≤ 960) | 224 (34.7) | 185 (40.5) | 39 (20.6) | 175 (42.8) | 49 (20.7) | ||
| Tertile 3 (MET > 960) | 218 (33.7) | 167 (36.5) | 51 (27.0) | 162 (39.6) | 56 (23.6) | ||
| HD vintage, years (Median, IQR) | 4.2 (2.1, 7.2) | 4.2 (2.0, 7.2) | 4.1 (2.6, 7.4) | 0.540 b | 4.5 (1.9, 7.2) | 4.1 (2.6, 7.2) | 0.517 b |
| CCI (Median, IQR) | 1.0 (0.0, 2.0) | 1.0 (0.0, 2.0) | 1.0 (1.0, 4.0) | <0.001 b | 1.0 (0.0, 2.0) | 1.0 (1.0, 3.0) | <0.001 b |
| HL index (Mean ± SD) | 25.2 ± 9.2 | 26.8 ± 9.3 | 22.1 ± 7.9 | <0.001 c | 26.8 ± 8.9 | 22.9 ± 9.1 | <0.001 c |
| DDL index (Mean ± SD) | 24.1 ± 11.4 | 25.4 ± 11.7 | 21.5 ± 10.4 | <0.001 c | 25.4 ± 11.4 | 22.3 ± 11.2 | <0.001 c |
| HDK (Mean ± SD) | 5.4 ± 2.5 | 5.9 ± 2.3 | 4.4 ± 2.67 | <0.001 c | 5.9 ± 2.3 | 4.6 ± 2.7 | <0.001 c |
| HDK Scale | Values |
|---|---|
| Absolute fit indices | |
| RMSEA | 0.09 |
| GFI | 0.96 |
| AGFI | 0.90 |
| SRMR | 0.05 |
| Incremental fit indices | |
| NFI | 0.96 |
| CFI | 0.96 |
| Parsimony fit indices | |
| PGFI | 0.43 |
| Item-scale convergent validity, mean of rho a (range) | 0.51 (0.37–0.59) |
| Criterion validity | |
| Correlation with HL, rho b | 0.22 ** |
| Correlation with DDL, rho b | 0.19 ** |
| Internal consistency, Cronbach’s alpha | 0.70 |
| Floor effect, % | 6.17 |
| Ceiling effect, % | 5.26 |
| Variables | Anxiety (GAD ≥ 8) | Depression (PHQ ≥ 10) | ||||||
|---|---|---|---|---|---|---|---|---|
| Bivariate | Multivariate | Bivariate | Multivariate | |||||
| OR (95%CI) | p | OR (95%CI) | p | OR (95%CI) | p | OR (95%CI) | p | |
| Age | ||||||||
| 23–59 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 60–85 | 1.16 (0.87, 1.54) | 0.315 | 0.85 (0.54, 1.34) | 0.484 | 1.28 (0.97, 1.68) | 0.082 | 1.06 (0.68, 1.65) | 0.804 |
| Gender | ||||||||
| Male | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Female | 1.25 (0.94, 1.65) | 0.128 | 0.92 (0.59, 1.44) | 0.710 | 1.28 (0.97, 1.67) | 0.079 | 0.92 (0.60, 1.43) | 0.723 |
| Education | ||||||||
| Illiterate or elementary | 1.00 | 1.00 | ||||||
| Junior high school | 1.03 (0.74, 1.45) | 0.850 | 1.02 (0.74, 1.41) | 0.914 | ||||
| Senior high school or above | 1.12 (0.78, 1.61) | 0.556 | 1.08 (0.76, 1.54) | 0.659 | ||||
| Working status | ||||||||
| Not working | 1.00 | 1.00 | 1.00 | |||||
| Working | 0.87 (0.65, 1.17) | 0.365 | 0.80 (0.61, 1.06) | 0.118 | 1.32 (0.80, 2.19) | 0.275 | ||
| Married status | ||||||||
| Never | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Ever | 1.88 (1.08, 3.29) | 0.026 | 1.67 (0.65, 4.29) | 0.284 | 1.52 (0.92, 2.50) | 0.100 | 0.99 (0.41, 2.37) | 0.980 |
| Social status | ||||||||
| Low | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Middle or high | 0.43 (0.32, 0.59) | <0.001 | 0.54 (0.33, 0.88) | 0.014 | 0.42 (0.31, 0.57) | <0.001 | 0.45 (0.27, 0.74) | 0.002 |
| Medication payment ability | ||||||||
| Very or fairly easy | 1.00 | 1.00 | ||||||
| Very or fairly difficulty | 5.70 (3.57, 9.12) | <0.001 | 6.25 (4.08, 9.59) | <0.001 | ||||
| S-COVID-19-S | ||||||||
| Without S-COVID-19-S | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| With S-COVID-19-S | 5.16 (3.53, 7.53) | <0.001 | 20.76 (8.85, 48.70) | <0.001 | 4.99 (3.56, 7.00) | <0.001 | 12.95 (6.67, 25.14) | <0.001 |
| BMI, kg/m2 | ||||||||
| BMI < 24 | 1.00 | 1.00 | 1.00 | |||||
| BMI ≥ 24 | 0.84 (0.52, 1.36) | 0.478 | 0.62 (0.38, 0.99) | 0.049 | 0.50 (0.25, 1.00) | 0.050 | ||
| Edema | ||||||||
| No | 1.00 | 1.00 | ||||||
| Yes | 1.60 (1.21, 2.12) | <0.001 | 1.88 (1.43, 2.47) | <0.001 | ||||
| Hyperthyroidism | ||||||||
| No | 1.00 | 1.00 | ||||||
| Yes | 1.01 (0.49, 2.06) | 0.981 | 1.33 (0.67, 2.61) | 0.414 | ||||
| Hospitalization within one month | ||||||||
| No | 1.00 | 1.00 | 1.00 | |||||
| Yes | 0.89 (0.50, 1.58) | 0.679 | 0.62 (0.35, 1.11) | 0.106 | 0.38 (0.11, 1.36) | 0.137 | ||
| Physical activity, MET-min/wk. | ||||||||
| Tertile 1 (MET ≤ 178) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Tertile 2 (178 < MET ≤ 960) | 0.22 (0.14, 0.35) | <0.001 | 0.31 (0.18; 0.52) | <0.001 | 0.15 (0.10, 0.23) | <0.001 | 0.21 (0.12; 0.35) | <0.001 |
| Tertile 3 (MET > 960) | 0.32 (0.21, 0.49) | <0.001 | 0.50 (0.29; 0.87) | 0.014 | 0.19 (0.12, 0.29) | <0.001 | 0.26 (0.15; 0.45) | <0.001 |
| HD vintage | 1.01 (0.98, 1.04) | 0.670 | 1.01 (0.97, 1.04) | 0.743 | ||||
| CCI | 1.12 (1.07, 1.17) | <0.001 | 1.10 (1.05, 1.15) | <0.001 | ||||
| HL index | 0.94 (0.93, 0.96) | <0.001 | 0.96 (0.93, 0.98) | 0.001 | 0.95 (0.94, 0.97) | <0.001 | 0.97 (0.95, 0.99) | 0.024 |
| DDL index | 0.97 (0.96, 0.99) | <0.001 | 0.98 (0.97, 0.99) | <0.001 | ||||
| HDK | 0.79 (0.74, 0.84) | <0.001 | 0.70 (0.64, 0.77) | <0.001 | 0.80 (0.76, 0.85) | <0.001 | 0.72 (0.66, 0.79) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dang, L.T.; Luong, T.C.; Nguyen, D.H.; Hoang, T.A.; Nguyen, H.T.; Nguyen, H.C.; Duong, T.H.; Tran, T.T.; Pham, L.V.; Ngo, T.V.; et al. The Associations of Suspected COVID-19 Symptoms with Anxiety and Depression as Modified by Hemodialysis Dietary Knowledge: A Multi-Dialysis Center Study. Nutrients 2022, 14, 2364. https://doi.org/10.3390/nu14122364
Dang LT, Luong TC, Nguyen DH, Hoang TA, Nguyen HT, Nguyen HC, Duong TH, Tran TT, Pham LV, Ngo TV, et al. The Associations of Suspected COVID-19 Symptoms with Anxiety and Depression as Modified by Hemodialysis Dietary Knowledge: A Multi-Dialysis Center Study. Nutrients. 2022; 14(12):2364. https://doi.org/10.3390/nu14122364
Chicago/Turabian StyleDang, Loan T., Thuc C. Luong, Dung H. Nguyen, Trung A. Hoang, Hoai T. Nguyen, Hoang C. Nguyen, Thai H. Duong, Tu T. Tran, Linh V. Pham, Tuan V. Ngo, and et al. 2022. "The Associations of Suspected COVID-19 Symptoms with Anxiety and Depression as Modified by Hemodialysis Dietary Knowledge: A Multi-Dialysis Center Study" Nutrients 14, no. 12: 2364. https://doi.org/10.3390/nu14122364
APA StyleDang, L. T., Luong, T. C., Nguyen, D. H., Hoang, T. A., Nguyen, H. T., Nguyen, H. C., Duong, T. H., Tran, T. T., Pham, L. V., Ngo, T. V., Nguyen, H. T., Trieu, N. T., Do, T. V., Trinh, M. V., Ha, T. H., Phan, D. T., Do, B. N., Yang, S.-H., Wang, T.-J., & Duong, T. V. (2022). The Associations of Suspected COVID-19 Symptoms with Anxiety and Depression as Modified by Hemodialysis Dietary Knowledge: A Multi-Dialysis Center Study. Nutrients, 14(12), 2364. https://doi.org/10.3390/nu14122364










