Global Prevalence of Isolated Systolic, Isolated Diastolic, and Systodiastolic Hypertension: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Design
2.2. Search Strategy
2.3. Selection Criteria
- Observational studies, primarily of cross-sectional design.
- Studies were included if they reported prevalence of hypertension subtypes (ISH, IDH, or SDH) based on direct blood pressure measurements.
- Studies where hypertension classification relied on measured blood pressure values rather than self-reported diagnosis or antihypertensive medication use. This criterion was implemented to minimize misclassification bias, as participants on effective antihypertensive treatment may have altered blood pressure profiles that do not reflect their underlying hypertension subtype. Studies that explicitly reported, including only untreated participants, or that did not specify treatment status but used measured blood pressure for classification, were considered eligible.
- Studies using the following standardized cut-off points for HTN subtypes:
- ◦
- ISH: SBP ≥ 140 mmHg and DBP < 90 mmHg;
- ◦
- IDH: DBP ≥ 90 mmHg and SBP < 140 mmHg;
- ◦
- SDH: SBP ≥ 140 mmHg and DBP ≥ 90 mmHg.
- Studies with probabilistic or non-probabilistic sampling methods.
- No publication language restrictions.
- Studies focused on specific subpopulations (pregnant women, individuals with specific comorbidities, or captive groups);
- Case reports, letters to the editor, systematic reviews, and bibliometric reviews;
- Publications without original data;
- Studies not representing the general population.
2.4. Study Selection Process
2.5. Risk of Bias Assessment
2.6. Statistical Analysis
3. Results
3.1. Selection of Articles in the Flow Diagram
3.2. Characteristics of Selected Studies
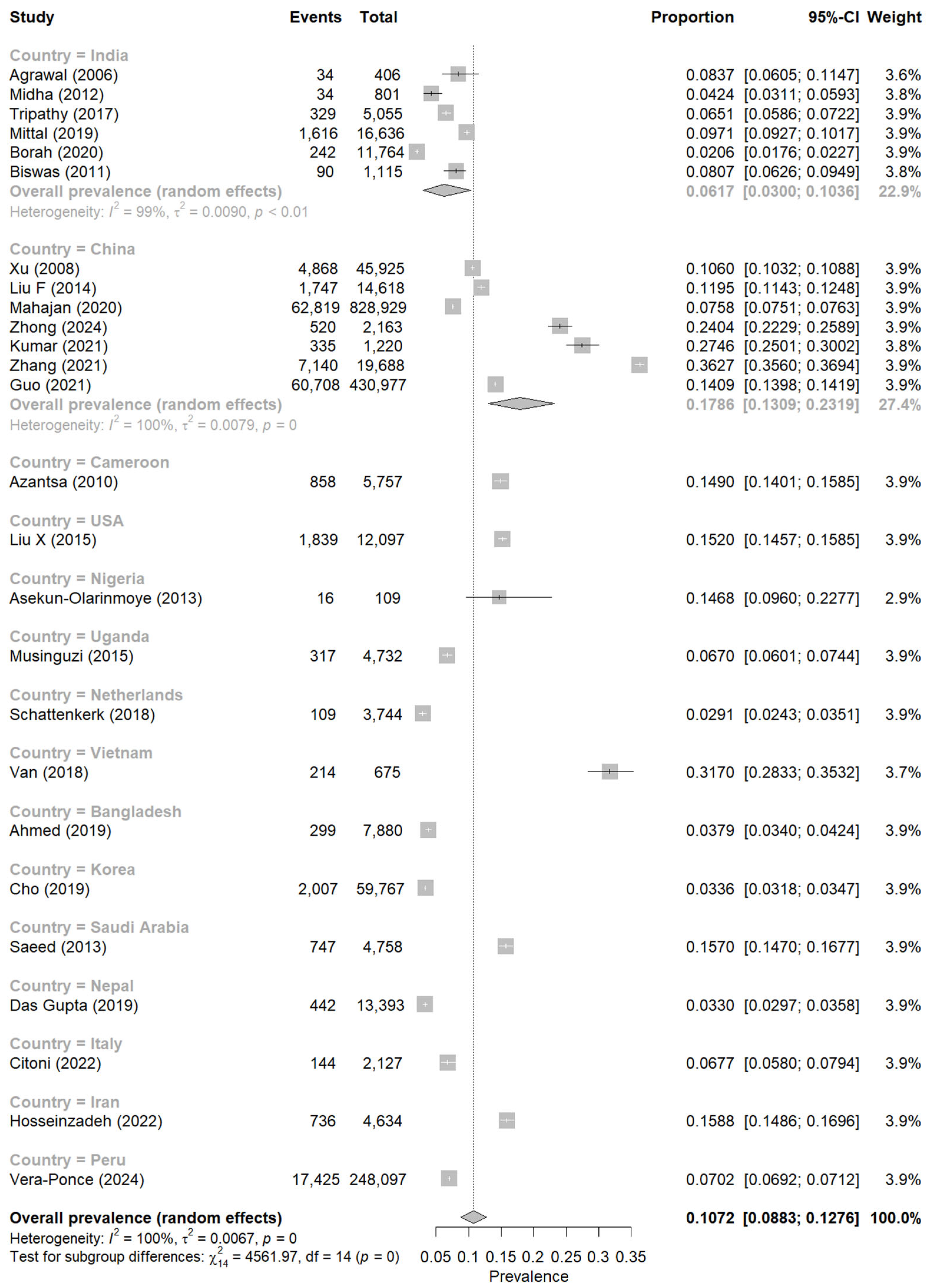
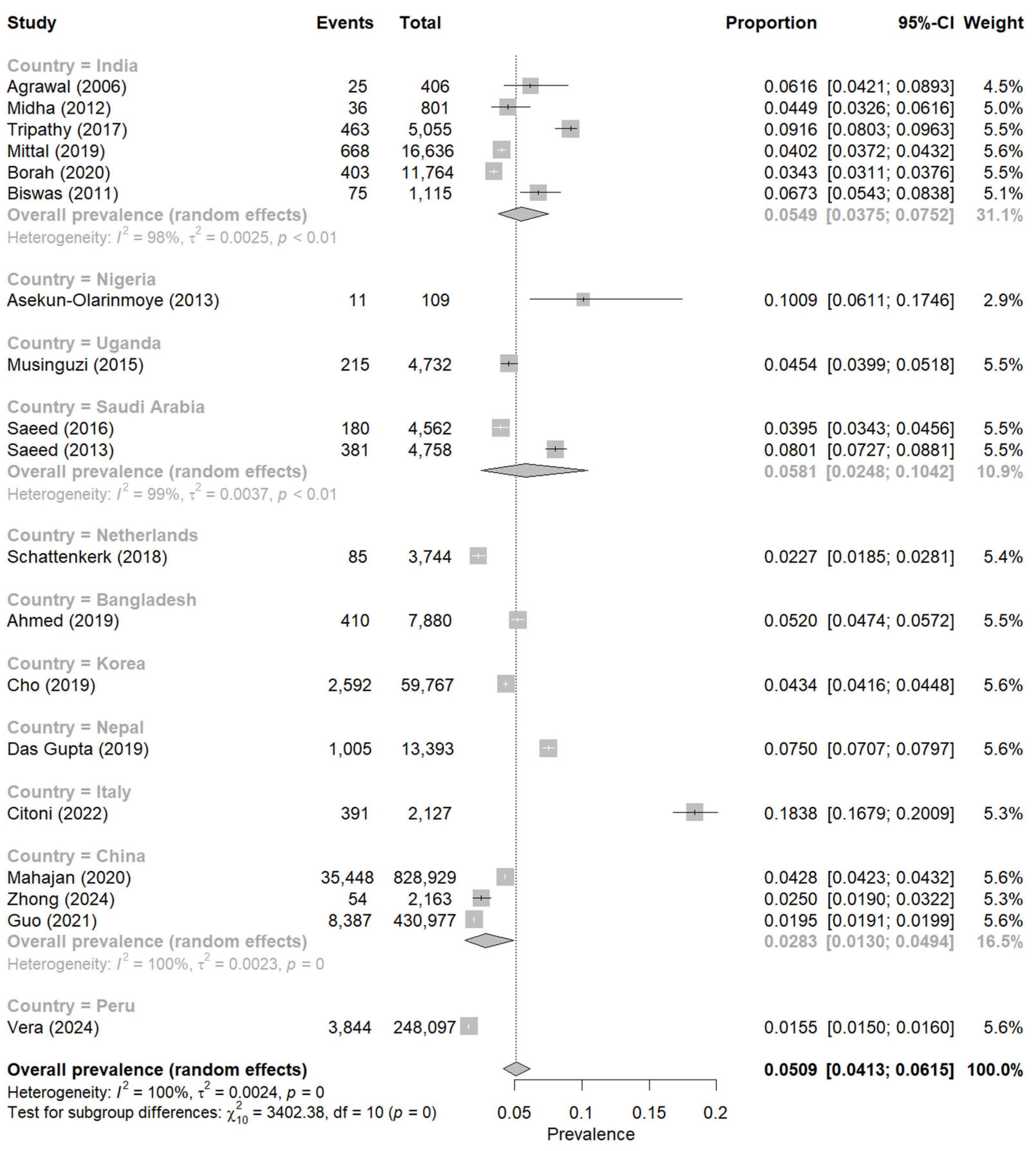
3.3. Meta-Analysis of ISH, IDH, and SDH
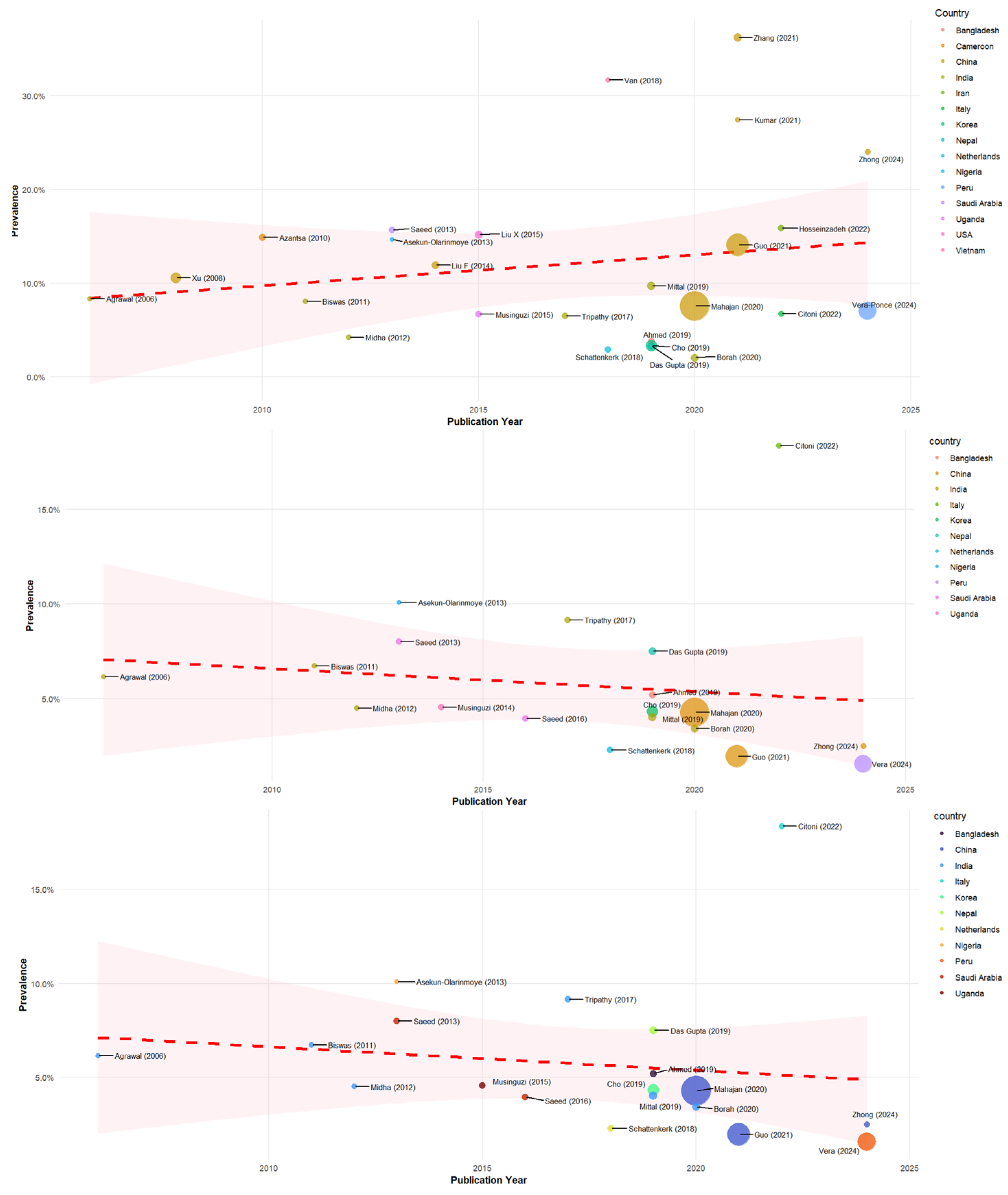
3.4. Meta-Regression of ISH, IDH, and SDH
3.5. Publication Bias Assessment
4. Discussion
4.1. Summary of Main Findings
4.2. Comparison with Previous Literature
4.3. Factors Explaining Variability
4.4. Clinical and Public Health Implications
4.5. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McEvoy, J.W.; McCarthy, C.P.; Bruno, R.M.; Brouwers, S.; Canavan, M.D.; Ceconi, C.; Christodorescu, R.M.; Daskalopoulou, S.S.; Ferro, C.J.; Gerdts, E.; et al. 2024 ESC Guidelines for the management of elevated blood pressure and hypertension. Eur. Heart J. 2024, 45, 3912–4018. [Google Scholar] [CrossRef]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: A pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021, 398, 957–980. [Google Scholar] [CrossRef]
- GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1223–1249. [Google Scholar] [CrossRef]
- Forouzanfar, M.H.; Liu, P.; Roth, G.A.; Ng, M.; Biryukov, S.; Marczak, L.; Alexander, L.; Estep, K.; Abate, K.H.; Akinyemiju, T.F.; et al. Global Burden of Hypertension and Systolic Blood Pressure of at Least 110 to 115 mm Hg, 1990–2015. JAMA 2017, 317, 165–182. [Google Scholar] [CrossRef]
- Olsen, M.H.; Angell, S.Y.; Asma, S.; Boutouyrie, P.; Burger, D.; Chirinos, J.A.; Damasceno, A.; Delles, C.; Gimenez-Roqueplo, A.-P.; Hering, D.; et al. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: The Lancet Commission on hypertension. Lancet 2016, 388, 2665–2712. [Google Scholar] [CrossRef]
- Feitosa, A.D.M.; Mota-Gomes, M.A.; Barroso, W.S.; Miranda, R.D.; Barbosa, E.C.D.; Pedrosa, R.P.; Oliveira, P.C.; Feltosa, C.L.; Brandão, A.A.; Lima-Filho, J.L.; et al. Relationship between office isolated systolic or diastolic hypertension and white-coat hypertension across the age spectrum: A home blood pressure study. J. Hypertens. 2020, 38, 663–670. [Google Scholar] [CrossRef]
- Global Hearts Initiative. Available online: https://www.who.int/news/item/15-09-2016-global-hearts-initiative (accessed on 27 May 2025).
- Bourdillon, M.T.; Song, R.J.; Musa Yola, I.; Xanthakis, V.; Vasan, R.S. Prevalence, Predictors, Progression, and Prognosis of Hypertension Subtypes in the Framingham Heart Study. J. Am. Heart Assoc. Cardiovasc. Cerebrovasc. Dis. 2022, 11, e024202. [Google Scholar] [CrossRef]
- Cesena, F.H.Y.; Nary, F.C.; Santos, R.D.; Bittencourt, M.S. The contribution of the systolic and diastolic components for the diagnosis of arterial hypertension under the 2017 ACC/AHA Guideline and metabolic heterogeneity among individuals with Stage 1 hypertension. J. Clin. Hypertens. 2020, 22, 1192–1199. [Google Scholar] [CrossRef] [PubMed]
- Unger, T.; Borghi, C.; Charchar, F.; Khan, N.A.; Poulter, N.R.; Prabhakaran, D.; Ramirez, A.; Schlaich, M.; Stergiou, G.S.; Tomaszewski, M.; et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension 2020, 75, 1334–1357. [Google Scholar] [CrossRef]
- Mills, K.T.; Stefanescu, A.; He, J. The global epidemiology of hypertension. Nat. Rev. Nephrol. 2020, 16, 223–237. [Google Scholar] [CrossRef]
- Geldsetzer, P.; Manne-Goehler, J.; Marcus, M.-E.; Ebert, C.; Zhumadilov, Z.; Wesseh, C.S.; Tsabedze, L.; Supiyev, A.; Sturua, L.; Bahendeka, S.K.; et al. The state of hypertension care in 44 low-income and middle-income countries: A cross-sectional study of nationally representative individual-level data from 1·1 million adults. Lancet 2019, 394, 652–662. [Google Scholar] [CrossRef] [PubMed]
- Yano, Y.; Stamler, J.; Garside, D.B.; Daviglus, M.L.; Franklin, S.S.; Carnethon, M.R.; Liu, K.; Greenland, P.; Lloyd-Jones, D.M. Isolated systolic hypertension in young and middle-aged adults and 31-year risk for cardiovascular mortality: The Chicago Heart Association Detection Project in Industry study. J. Am. Coll. Cardiol. 2015, 65, 327–335. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinica3l Practice Guidelines. Hypertension 2018, 71, 1269–1324. [Google Scholar] [CrossRef]
- Munn, Z.; Moola, S.; Lisy, K.; Riitano, D.; Tufanaru, C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int. J. Evid. Based Healthc. 2015, 13, 147–153. [Google Scholar] [CrossRef]
- Schwarzer, G.; Carpenter, J.R.; Rücker, G. Meta-Analysis with R; Springer International Publishing: Cham, Switzerland, 2015. [Google Scholar] [CrossRef]
- Freeman, M.F.; Tukey, J.W. Transformations Related to the Angular and the Square Root. Ann. Math. Stat. 1950, 21, 607–611. [Google Scholar] [CrossRef]
- Barendregt, J.J.; Doi, S.A.; Lee, Y.Y.; Norman, R.E.; Vos, T. Meta-analysis of prevalence. J. Epidemiol. Community Health 2013, 67, 974–978. [Google Scholar] [CrossRef]
- Wilson, E.B. Probable Inference, the Law of Succession, and Statistical Inference. J. Am. Stat. Assoc. 1927, 22, 209–212. [Google Scholar] [CrossRef]
- Newcombe, R.G. Two-sided confidence intervals for the single proportion: Comparison of seven methods. Stat. Med. 1998, 17, 857–872. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control Clin. Trials. 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.T.; Rothstein, H.R. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res. Synth. Methods 2010, 1, 97–111. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T. Commentary: Heterogeneity in meta-analysis should be expected and appropriately quantified. Int. J. Epidemiol. 2008, 37, 1158–1160. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, V.K.; Basannar, D.R.; Sing, R.P.; Dutt, M.; Abraham, D.; Mustafa, M.S. Coronary risk factors in a rural community. Indian J. Public Health 2006, 50, 19–23. [Google Scholar] [PubMed]
- Xu, C.; Sun, Z.; Zheng, L.; Zhang, D.; Li, J.; Zhang, X.; Liu, S.; Zhao, F.; Hu, D.; Sun, Y. Prevalence of and risk factors for isolated systolic hypertension in the rural adult population of Liaoning Province, China. J. Int. Med. Res. 2008, 36, 353–356. [Google Scholar] [CrossRef]
- Biswas, M.; Manna, C.K. Prevalence of hypertension and sociodemographic factors within the Scheduled Caste community of the District Nadia, West Bengal, India. High Blood Press. Cardiovasc. Prev. Off. J. Ital. Soc. Hypertens. 2011, 18, 179–185. [Google Scholar] [CrossRef]
- Midha, T.; Lalchandani, A.; Nath, B.; Kumari, R.; Pandey, U. Prevalence of isolated diastolic hypertension and associated risk factors among adults in Kanpur, India. Indian Heart J. 2012, 64, 374–379. [Google Scholar] [CrossRef]
- Asekun-Olarinmoye, E.O.; Akinwusi, P.O.; Adebimpe, W.O.; Isawumi, M.A.; Hassan, M.B.; Olowe, O.A.; Makanjuola, O.B.; Alebiosu, C.O.; Adewole, T.A. Prevalence of hypertension in the rural adult population of Osun State, southwestern Nigeria. Int. J. Gen. Med. 2013, 6, 317–322. [Google Scholar] [CrossRef]
- Liu, F.; Ma, Y.-T.; Yang, Y.-N.; Zhen, Y.-J.; Xie, X.; Li, X.-M.; Ma, X.; Chen, B.-D.; Huang, Y.; Shan, C.-F.; et al. The prevalence of isolated systolic hypertension in adult populations from the Han, Uygur and Kazakh ethnic groups in Xinjiang, China. Blood Press. 2014, 23, 154–159. [Google Scholar] [CrossRef]
- Liu, X.; Rodriguez, C.J.; Wang, K. Prevalence and trends of isolated systolic hypertension among untreated adults in the United States. J. Am. Soc. Hypertens. 2015, 9, 197–205. [Google Scholar] [CrossRef]
- Tripathy, G.; Van Geertruyden, J.-P.; Bastiaens, H.; Nuwaha, F. Uncontrolled hypertension in Uganda: A comparative cross-sectional study. J. Clin. Hypertens. 2015, 17, 63–69. [Google Scholar] [CrossRef]
- Boris, A.K.G.; Huguette, Y.M.C.; Laure, N.J.; Oben, J.E. The effect of body weight on the incidence and prevalence of hypertension in Yaoundé. J. Diabetes Endocrinol. 2010, 1, 006–012. [Google Scholar]
- Saeed, A.A.; Al-Hamdan, N.A. Isolated Diastolic Hypertension among Adults in Saudi Arabia: Prevalence, Risk Factors, Predictors and Treatment. Results of a National Survey. Balk. Med. J. 2016, 33, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Tripathy, J.P.; Thakur, J.S.; Jeet, G.; Chawla, S.; Jain, S. Alarmingly high prevalence of hypertension and pre-hypertension in North India-results from a large cross-sectional STEPS survey. PLoS ONE 2017, 12, e0188619. [Google Scholar] [CrossRef] [PubMed]
- Eeftinck Schattenkerk, D.W.; van Gorp, J.; Vogt, L.; Peters, R.J.; van den Born, B.-J.H. Isolated systolic hypertension of the young and its association with central blood pressure in a large multi-ethnic population. The HELIUS study. Eur. J. Prev. Cardiol. 2018, 25, 1351–1359. [Google Scholar] [CrossRef] [PubMed]
- Van, N.B.; Van, Q.P.; Hoang, L.V.; Van, T.B.; Hoang, N.N.; Nam, K.D.; Chu, D.-T. Prevalence and Risk Factors of Hypertension in Two Communes in the Vietnam Northern Mountainous, 2017. BioMed Res Int. 2018, 2018, 7814195. [Google Scholar] [CrossRef]
- Ahmed, S.; Pervin, S.; Biswas, T.; Chowdhury, M.A.H.; Hasnat, M.A.; Shuvra, M.M.R. Undiagnosed Isolated Systolic and Diastolic Hypertension Subtypes and Their Correlates in Bangladesh: A Nationwide Survey. Osong Public Health Res. Perspect. 2019, 10, 12–19. [Google Scholar] [CrossRef]
- Cho, S.M.J.; Lee, H.; Kim, H.C. Differences in prevalence of hypertension subtypes according to the 2018 Korean Society of Hypertension and 2017 American College of Cardiology/American Heart Association guidelines: The Korean National Health and Nutrition Examination Survey, 2007–2017 (KNHANES IV-VII). Clin. Hypertens. 2019, 25, 26. [Google Scholar] [CrossRef]
- Saeed, A.A.; Al-Hamdan, N.A. Anthropometric risk factors and predictors of hypertension among Saudi adult population—A national survey. J. Epidemiol. Glob. Health 2013, 3, 197–204. [Google Scholar] [CrossRef]
- Mittal, C.; Singh, M.; Bakhshi, T.; Ram Babu, S.; Rajagopal, S.; Ram, C.V.S. Isolated diastolic hypertension and its risk factors in semi-rural population of South India. Indian Heart J. 2019, 71, 272–276. [Google Scholar] [CrossRef]
- Gupta, R.D.; Talukdar, A.; Haider, S.S.; Haider, M.R. Prevalence and Associated Factors of Hypertension Subtypes Among the Adult Population in Nepal: Evidence from Demographic and Health Survey Data. Osong Public Health Res. Perspect. 2019, 10, 327–336. [Google Scholar] [CrossRef]
- Borah, P.K.; Mahanta, J.; Kalita, H.C.; Bhattacharjee, C.K. Distribution of hypertension subtypes in a hill tribe of Mizoram, Northeast India. Indian Heart J. 2020, 72, 398–402. [Google Scholar] [CrossRef]
- Mahajan, S.; Feng, F.; Hu, S.; Lu, Y.; Gupta, A.; Murugiah, K.; Gao, Y.; Lu, J.; Liu, J.; Zheng, X.; et al. Assessment of Prevalence, Awareness, and Characteristics of Isolated Systolic Hypertension Among Younger and Middle-Aged Adults in China. JAMA Netw. Open. 2020, 3, e209743. [Google Scholar] [CrossRef]
- Kumar, S.; Kant, R.; Yadav, P.; Natarajan, K.; Bahurupi, Y.; Mishra, A. A Community-Based Study on Waist-to-Height Ratio: An Indicator for Systolic Hypertension in a Rural Community of Hilly Region. Cureus 2021, 13, e16014. [Google Scholar] [CrossRef]
- Guo, J.; Lv, J.; Guo, Y.; Bian, Z.; Zheng, B.; Wu, M.; Yang, L.; Chen, Y.; Su, J.; Zhang, J.; et al. Association between blood pressure categories and cardiovascular disease mortality in China. PLoS ONE 2021, 16, e0255373. [Google Scholar] [CrossRef] [PubMed]
- Hosseinzadeh, A.; Ebrahimi, H.; Khosravi, A.; Emamian, M.H.; Hashemi, H.; Fotouhi, A. Isolated systolic hypertension and its associated risk factors in Iranian middle age and older population: A population-based study. BMC Cardiovasc. Disord. 2022, 22, 425. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Liu, S.; Jiao, Y.; Zheng, L.; Sun, Y.; Sun, Z. Association of isolated diastolic hypertension based on different guideline definitions with incident cardiovascular risk in a Chinese rural cohort. J. Clin. Hypertens. 2022, 24, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Citoni, B.; Figliuzzi, I.; Presta, V.; Cesario, V.; Miceli, F.; Bianchi, F.; Ferrucci, A.; Volpe, M.; Tocci, G. Prevalence and clinical characteristics of isolated systolic hypertension in young: Analysis of 24 h ambulatory blood pressure monitoring database. J. Hum. Hypertens. 2022, 36, 40–50. [Google Scholar] [CrossRef]
- Zhong, H.; Li, H.; Xu, D.; Dong, Y.; Pan, C.; Li, J.; Chen, L. The prevalence and risk factors associated with hypertension subtypes among ethnic Dai adults in rural China. Prev. Med. Rep. 2024, 47, 102886. [Google Scholar] [CrossRef]
- Vera-Ponce, V.J.; Zuzunaga-Montoya, F.E.; Vásquez-Romero, L.E.M.; Loayza-Castro, J.A.; Gutierrez De Carrillo, C.I.; Vigil-Ventura, E. Prevalence, trends, and associated factors of isolated systolic, diastolic, and systolic-diastolic hypertension in Peru: A nine-year analysis of the Demographic and Family Health Survey. Hipertens. Riesgo Vasc. 2025, 42, 18–28. [Google Scholar] [CrossRef]
- Mitchell, G.F.; Hwang, S.-J.; Vasan, R.S.; Larson, M.G.; Pencina, M.J.; Hamburg, N.M.; Vita, J.A.; Levy, D.; Benjamin, E.J. Arterial stiffness and cardiovascular events: The Framingham Heart Study. Circulation 2010, 121, 505–511. [Google Scholar] [CrossRef]
- Franklin, S.S.; Gustin, W., 4th; Wong, N.D.; Larson, M.G.; Weber, M.A.; Kannel, W.B.; Levy, D. Hemodynamic patterns of age-related changes in blood pressure. The Framingham Heart Study. Circulation 1997, 96, 308–315. [Google Scholar] [CrossRef]
- Safar, M.E.; Asmar, R.; Benetos, A.; Blacher, J.; Boutouyrie, P.; Lacolley, P.; Laurent, S.; London, G.; Pannier, B.; Protogerou, A.; et al. Interaction Between Hypertension and Arterial Stiffness. Hypertension 2018, 72, 796–805. [Google Scholar] [CrossRef]
- Zieman, S.J.; Melenovsky, V.; Kass, D.A. Mechanisms, pathophysiology, and therapy of arterial stiffness. Arterioscler Thromb Vasc Biol. 2005, 25, 932–943. [Google Scholar] [CrossRef] [PubMed]
- McEniery, C.M.; Yasmin; Wallace, S.; Maki-Petaja, K.; McDonnell, B.; Sharman, J.E.; Retallick, C.; Franklin, S.S.; Brown, M.J.; Lloyd, R.C.; et al. Increased stroke volume and aortic stiffness contribute to isolated systolic hypertension in young adults. Hypertension 2005, 46, 221–226. [Google Scholar] [CrossRef] [PubMed]
- Franklin, S.S.; Jacobs, M.J.; Wong, N.D.; L’Italien, G.J.; Lapuerta, P. Predominance of isolated systolic hypertension among middle-aged and elderly US hypertensives: Analysis based on National Health and Nutrition Examination Survey (NHANES) III. Hypertension 2001, 37, 869–874. [Google Scholar] [CrossRef] [PubMed]
- Muntner, P.; Shimbo, D.; Carey, R.M.; Charleston, J.B.; Gaillard, T.; Misra, S.; Myers, M.G.; Ogedegbe, G.; Schwartz, J.E.; Townsend, R.R.; et al. Measurement of Blood Pressure in Humans: A Scientific Statement from the American Heart Association. Hypertension 2019, 73, e35–e66. [Google Scholar] [CrossRef]
- Stergiou, G.S.; Palatini, P.; Parati, G.; O’Brien, E.; Januszewicz, A.; Lurbe, E.; Persu, A.; Mancia, G.; Kreutz, R. 2021 European Society of Hypertension practice guidelines for office and out-of-office blood pressure measurement. J. Hypertens. 2021, 39, 1293–1302. [Google Scholar] [CrossRef]
- Ruan, Y.; Guo, Y.; Zheng, Y.; Huang, Z.; Sun, S.; Kowal, P.; Shi, Y.; Wu, F. Cardiovascular disease (CVD) and associated risk factors among older adults in six low-and middle-income countries: Results from SAGE Wave 1. BMC Public Health 2018, 18, 778. [Google Scholar] [CrossRef]
- Prabhakaran, D.; Jeemon, P.; Ghosh, S.; Shivashankar, R.; Ajay, V.S.; Kondal, D.; Gupta, R.; Ali, M.K.; Mohan, D.; Mohan, V.; et al. Prevalence and incidence of hypertension: Results from a representative cohort of over 16,000 adults in three cities of South Asia. Indian Heart J. 2017, 69, 434–441. [Google Scholar] [CrossRef]
- Wang, Z.; Chen, Z.; Zhang, L.; Wang, X.; Hao, G.; Zhang, Z.; Shao, L.; Tian, Y.; Dong, Y.; Zheng, C.; et al. Status of Hypertension in China: Results From the China Hypertension Survey, 2012–2015. Circulation 2018, 137, 2344–2356. [Google Scholar] [CrossRef]
- Egan, B.M.; Li, J.; Hutchison, F.N.; Ferdinand, K.C. Hypertension in the United States, 1999 to 2012: Progress toward Healthy People 2020 goals. Circulation 2014, 130, 1692–1699. [Google Scholar] [CrossRef]
- Mills, K.T.; Bundy, J.D.; Kelly, T.N.; Reed, J.E.; Kearney, P.M.; Reynolds, K.; Chen, J.; He, J. Global Disparities of Hypertension Prevalence and Control: A Systematic Analysis of Population-based Studies from 90 Countries. Circulation 2016, 134, 441–450. [Google Scholar] [CrossRef]
- Flint, A.C.; Conell, C.; Ren, X.; Banki, N.M.; Chan, S.L.; Rao, V.A.; Melles, R.B.; Bhatt, D.L. Effect of Systolic and Diastolic Blood Pressure on Cardiovascular Outcomes. N. Engl. J. Med. 2019, 381, 243–251. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vera-Ponce, V.J.; Valladolid-Sandoval, L.A.M.; Ballena-Caicedo, J.; Zuzunaga-Montoya, F.E. Global Prevalence of Isolated Systolic, Isolated Diastolic, and Systodiastolic Hypertension: A Systematic Review and Meta-Analysis. Cardiovasc. Med. 2025, 28, 3. https://doi.org/10.3390/cardiovascmed28010003
Vera-Ponce VJ, Valladolid-Sandoval LAM, Ballena-Caicedo J, Zuzunaga-Montoya FE. Global Prevalence of Isolated Systolic, Isolated Diastolic, and Systodiastolic Hypertension: A Systematic Review and Meta-Analysis. Cardiovascular Medicine. 2025; 28(1):3. https://doi.org/10.3390/cardiovascmed28010003
Chicago/Turabian StyleVera-Ponce, Víctor Juan, Lupita Ana Maria Valladolid-Sandoval, Jhosmer Ballena-Caicedo, and Fiorella E. Zuzunaga-Montoya. 2025. "Global Prevalence of Isolated Systolic, Isolated Diastolic, and Systodiastolic Hypertension: A Systematic Review and Meta-Analysis" Cardiovascular Medicine 28, no. 1: 3. https://doi.org/10.3390/cardiovascmed28010003
APA StyleVera-Ponce, V. J., Valladolid-Sandoval, L. A. M., Ballena-Caicedo, J., & Zuzunaga-Montoya, F. E. (2025). Global Prevalence of Isolated Systolic, Isolated Diastolic, and Systodiastolic Hypertension: A Systematic Review and Meta-Analysis. Cardiovascular Medicine, 28(1), 3. https://doi.org/10.3390/cardiovascmed28010003





