In 2002, the Working Group for Echocardiography of the Swiss Society of Cardiology Awards, with the support of Menarini Switzerland, created a prize to promote echocardiography and support young cardiologists in Switzerland. It is awarded each year to the first author of the best abstracts presented at the annual scientific meeting of the SSC, after assessment and grading by an independent scientific committee.
Last year in Lausanne, on June 15–17 2005, the Menarini Prize was awarded to:
- ‒
1st Prize: Dr. Haran Burri, Geneva
- ‒
2nd Prize: Dr. Marco Studer, Basel
- ‒
3rd Prize: Dr. Beat A. Kaufmann, Basel
The three laureates were invited to present their work as an abstract in Kardiovaskuläre Medizin.
Measuring Ventricular Asynchrony Using Standard Echocardiography or Tissue Doppler Imaging: Do the Results Agree?
Haran Burri, Hajo Muller, Henri Sunthorn, Dipen Shah, René Lerch
Service de Cardiologie, Hôpitaux Universitaires de Genève, Genève
Background: Presence of ventricular asynchrony may affect response to biventricular pacing. Asynchrony may be measured using either standard echocardiography with pulsed-wave Doppler (PWD) and M-mode (MM), or pulsed-wave tissue Doppler imaging (TDI). Our aim was to evaluate whether these methods provide concordant results.
Material and methods: 42 consecutive patients in sinus rhythm with a LVEF of ≤0.35 were included. Interventricular asynchrony was evaluated by PWD by calculating difference in pulmonary and aortic pre-ejection intervals, whereas this was measured by TDI by calculating the maximal difference between the Q-Sm intervals measured at the basal right ventricular free wall and any of four basal segments of the left ventricle. Intraventricular asynchrony was evaluated using MM by looking for delayed contraction of the posterior basal wall after onset of ventricular filling, and by TDI by calculating the maximal difference of Q-Sm intervals between four basal segments of the left ventricle. A control group of 39 subjects with normal systolic function was also studied, in order to determine cut-off values for these parameters (interventricular asynchrony was thus defined as a delay of ≥40 ms by conventional echo and ≥30 ms by TDI; intraventricular asynchrony was present if the delay by TDI was >20 ms).
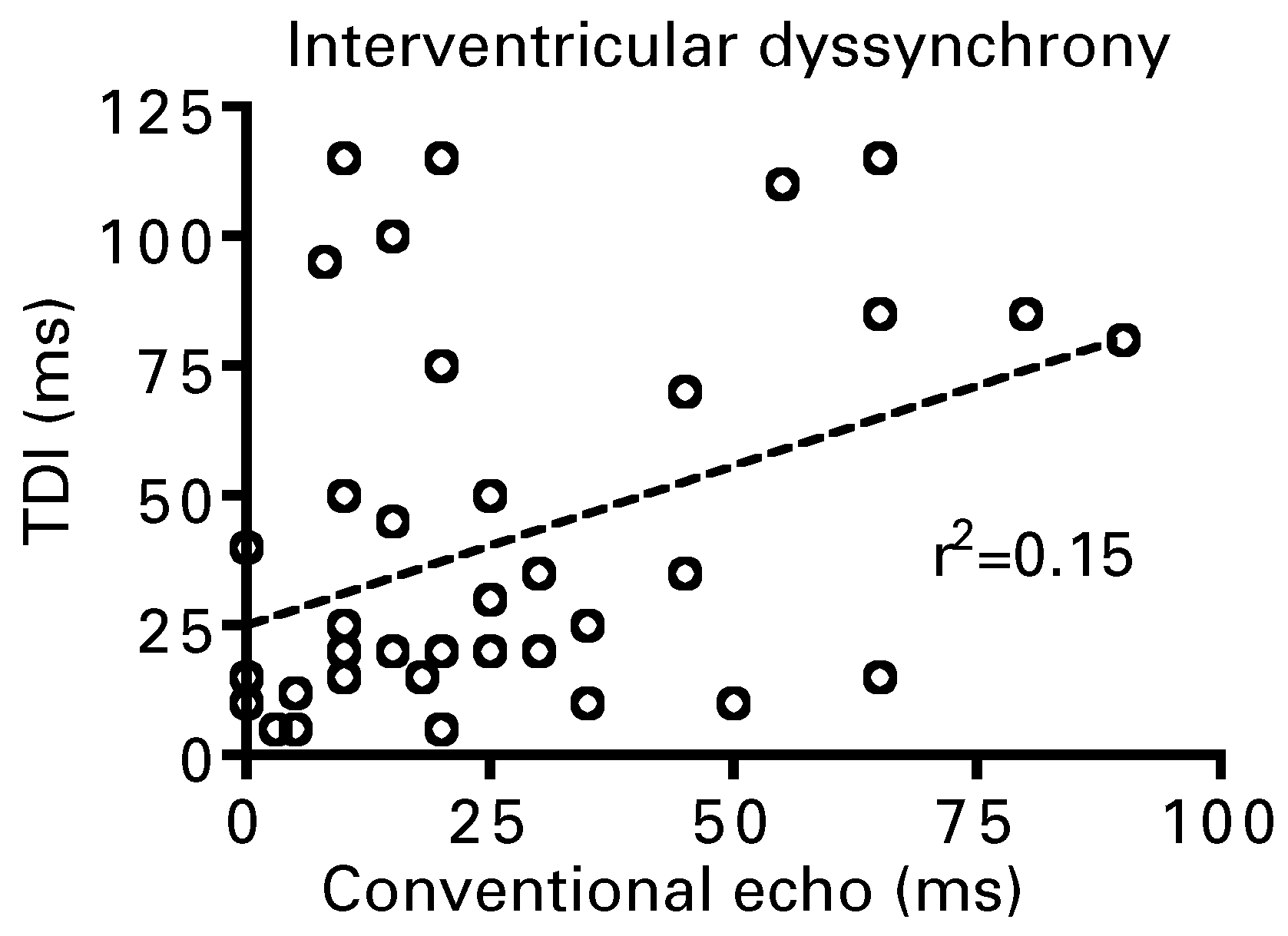
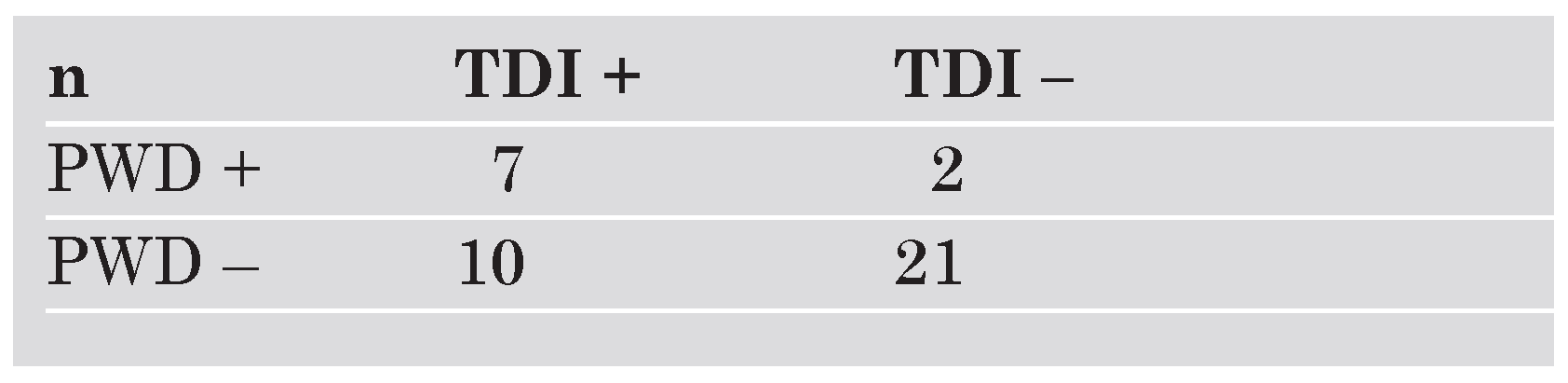
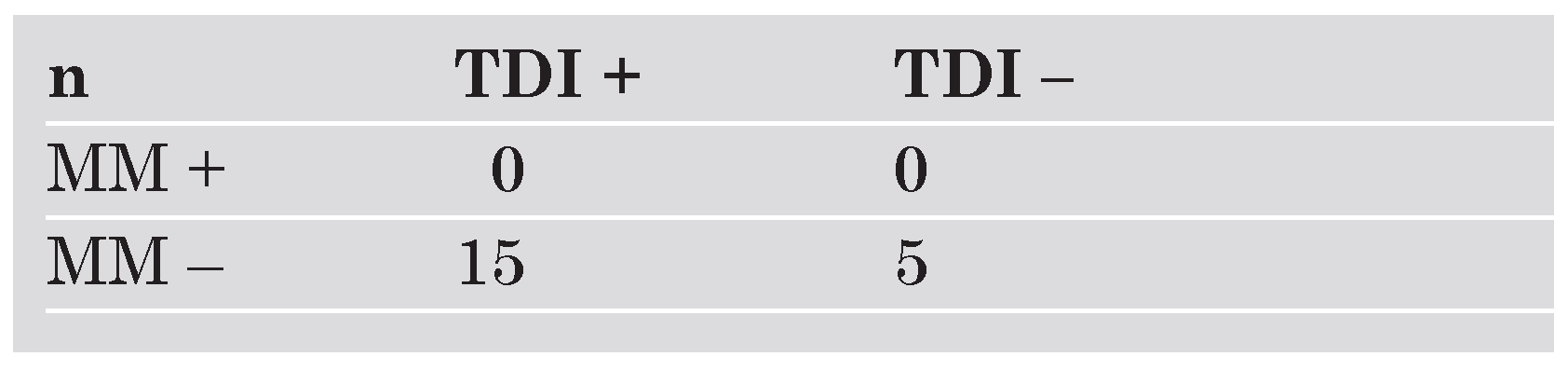
Results: 2/42 patients were eliminated due to uninterpretable TDI studies. Interventricular asynchrony was present in 9/40 (23%) of patients using PWD, and in 17/40 (43%) of patients using TDI (k = 0.35). There was poor correlation between the two methods for the degree of asynchrony (r2 = 0.15). Intra-ventricular asynchrony was not detected by MM in any of the patients, whereas TDI showed evidence of asynchrony in 15/40 (38%) of patients (
Table 1 and
Table 2;
Figure 1).
Conclusions: Results differ considerably according to whether ventricular asynchrony is evaluated by standard echocardiography or by TDI. Standard echocardiography is less likely to show evidence of asynchrony, especially as concerns intraventricular asynchrony. This may have implications for patient selection for cardiac resynchronization therapy.
Long-Term Risk Prediction by Echocardiography Versus Clinical Risk Scoring in a Prospectively Recruited Cohort
M. Studer, C. Imsand, M. Siegemund, P. Buser, S. Marsch, P. Hunziker
Medical Intensive Care Unit, University Hospital Basel, Basel
Background: An important goal in cardiovascular examination is risk prediction for death and major adverse events in an individual. To justify the use of an imaging technique for risk assessment, its incremental value to clinically available information is important. Direct quantification of atherosclerotic burden, the fundamental anatomic substrate causing most cardiovascular events, is pathophysiologically appealing for risk stratification. It has been shown to be easily measurable at the bedside / in the cardiologic practice setting using echocardiography [
1], has shown to strongly predict cardiovascular risk in prospective study, and can improve patient selection for statin prophylaxis [
2], we studied long-term risk stratification by echocardiography and compared it to conventional risk assessment in a prospective study.
Study design: The prognostic and incremental value of echocardiography was studied in a prospectively recruited cohort of individuals referred for echocardiography for any reason from 1998 to 1999. Determined were age, sex, and classical risk factors, from which the Framingham score was computed; echocardiographically measured were left ventricular dimensions, left ventricular ejection fraction, left ventricular mass index, as well as echo-derived atherosclerotic burden, using a validated methodology described in detail at website:
http://www.koronarsyndrom.ch. Outcome was assessed at seven years by telephone interview of patients and contact persons, supplemented by hospital chart-review.
Results: In 336 patients, there were 84 deaths overall, of which 42 were attributable to atherosclerosis. A history of prior events (p = 0.03), age (p <0.001) and classical risk factors (Framingham score, p <0.001) and left ventricular ejection fraction (p = 0.008) were significantly predictive of atherosclerotic death, as well as of major adverse cardiovascular events, although the Framingham score added no incremental information to age alone. The most important echocardiographic predictor of atherosclerotic mortality (p <0.001) and MACE (p = 0.001) was echocardiographically determined atherosclerotic burden, while trends for LV mass and left ventricular diameters missed the significance threshold. Notably, in stepwise multivariate models using age, event history, risk factors, and echo findings, the key predictors of death were age, event history, and echocardiographic atherosclerosis burden, each adding incremental information to risk prediction.
Conclusion: For long-term risk individual risk prediction in a noninvasive setting, the combination of age, event history and echocardiographic atherosclerosis quantification is best.
Implementation in the practice setting: Based on these results, a Swiss prospective study assessing the value of noninvasive echo quantification of atherosclerosis in the cardiologic practice has been initiated; practicing cardiologists willing to apply this method in their patients and to profit from easy tools to measure and report atherosclerosis severity are invited to visit website:
http://www.koronarsyndrom.ch.
Preliminary Data on Myocardial Blood Flow Reserve in High-Altitude Pulmonary Edema Susceptible Mountaineers and Healthy Volunteers
B. A. Kaufmanna, A. Bernheima, S. Kienckea, M. Fischlerb, H. Mairbäurlc, M. Maggiorinib, H. P. Brunner La Roccaa
a Cardiology, University Hospital Basel
b Intensive Care Unit, DIM, University Hospital, Zurich
c Medical Clinic VII, Sports Medicine, University of Heidelberg
Background: High altitude pulmonary edema (HAPE) is a potentially fatal condition occurring in predisposed individuals rapidly ascending to high altitude. The pathogenesis of HAPE is incompletely understood, but reduced availability of nitric oxide leading to excessive increase in pulmonary artery and capillary pressures and consecutive inflammatory response seems to be a central mechanism. This may result in dysfunction of the alveolar epithelium and vascular endothelium. The latter may not only take place in the pulmonary, but also in the systemic vasculature. We hypothesised that myocardial blood flow reserve as a measure of endothelial function might be altered in mountaineers developing HAPE.
Methods: Healthy HAPE-susceptible mountaineers and control subjects were examined at low (490 m) and high altitude (4559 m). Low mechanical index contrast (Sonovue) stress-echocardiography was performed at rest and 40% of peak exercise capacity. Sonovue is a gas-filled microbubble with a lipid shell that remains entirely within the vascular space and has a similar rheology as red blood cells. The radial oscillation of microbubbles in the ultrasound field generates accoustic signals which are stronger than signals from tissue and can be displayed as videointensity on a screen. The dynamics of the increase in videointensity (VI) in the midventricular septum were measured after destruction of microbubbles by a high intensity ultrasound pulse. The rise of VI is proportional to myocardial blood velocity and the plateau of maximal VI is proportional to myocardial blood volume. The product of the two is proportional to blood flow and the ratio from rest to exercise reflects myocardial blood flow reserve. The investigator evaluating perfusion was blinded for the clinical outcome of subjects.
Results: 26 persons were evaluated for inclusion in the study. Of these, 2 developed HAPE before examination at 4559 m, and in 7 echocardiographic images were not suitable for evaluation, thus leaving 17 for inclusion in the study (4 female, age 40 ± 10 years). 10 (59%) were HAPE-susceptible, of which 4 developed HAPE within 24 h after examination. Mean myocardial blood flow reserve (MBFr) at low altitude was 2.1 ± 0.9, not different between HAPE-susceptibles and controls. At high altitude, subjects who did not develop HAPE had a mean MBFr of 2.6 ± 1.0, whereas it was 2.2 ± 1.0 for the 4 subjects with HAPE. MBFr increased by 38 ± 46 in those without HAPE, but decreased by 16 ± 33 in those developing HAPE (p <0.05). Conclusions: Our data suggest that MBFr is impaired in subjects developing HAPE, reflecting dysfunction of not only pulmonary endothelium and the alveolar epithelium, but also the vasculature of the myocardium. However, a substantial number of subjects could not be evaluated due to technical reasons, showing the technical limitations of measuring MBFr with contrast echocardiography during bicycle ergometry and at high altitude.