Severe Coronary Artery Ectasia and Abdominal Aortic Aneurysm
Abstract
Zusammenfassung
Introduction
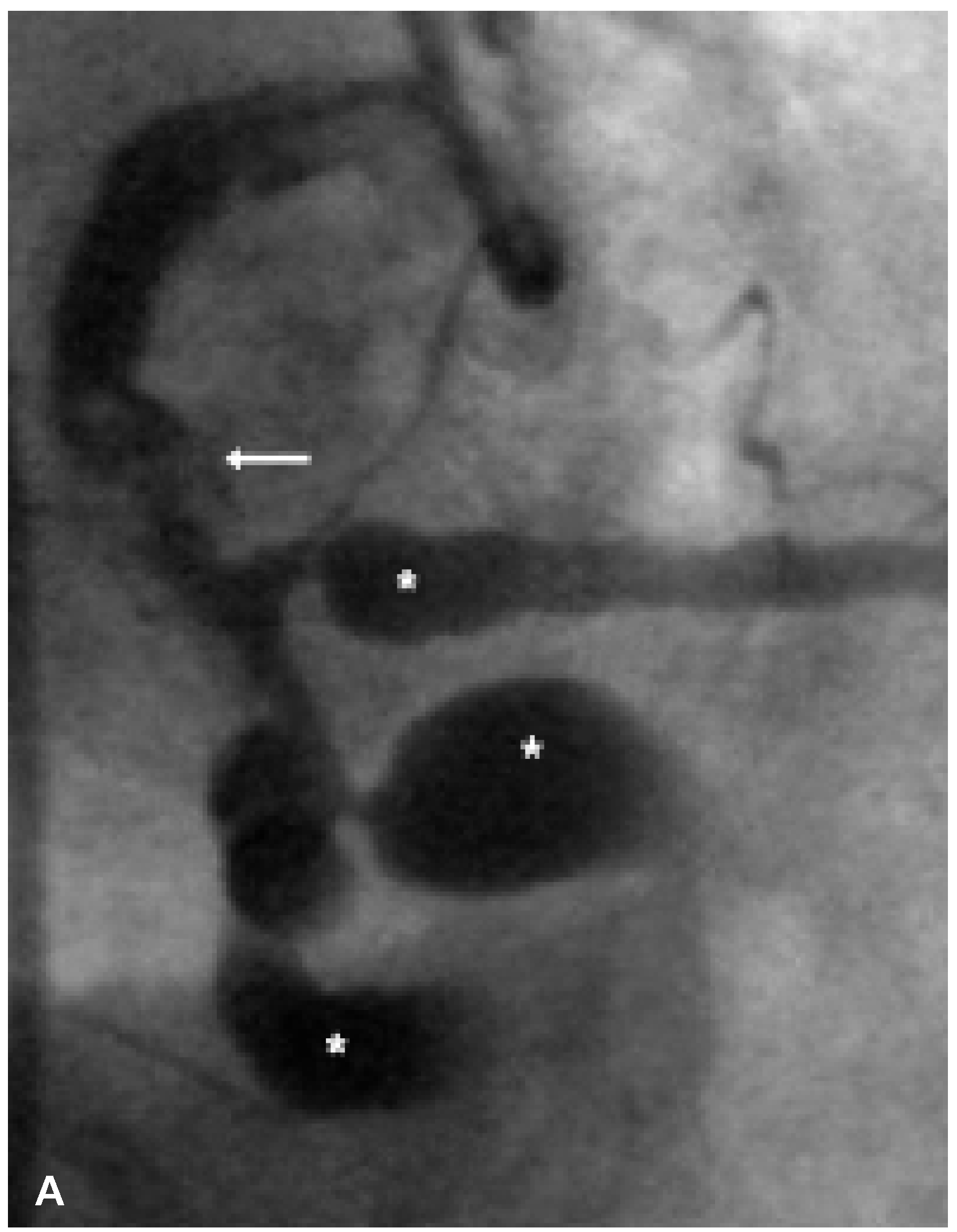
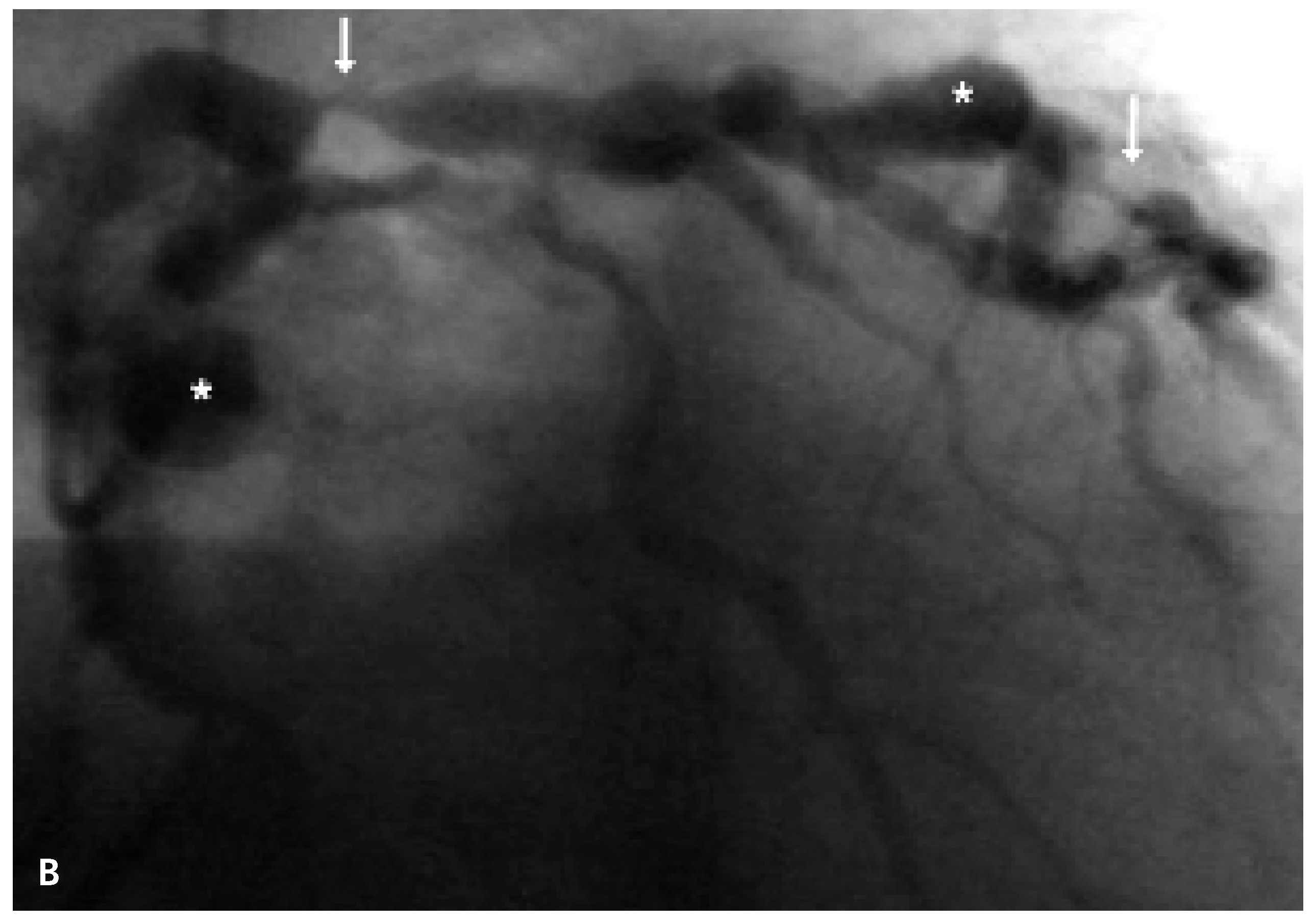
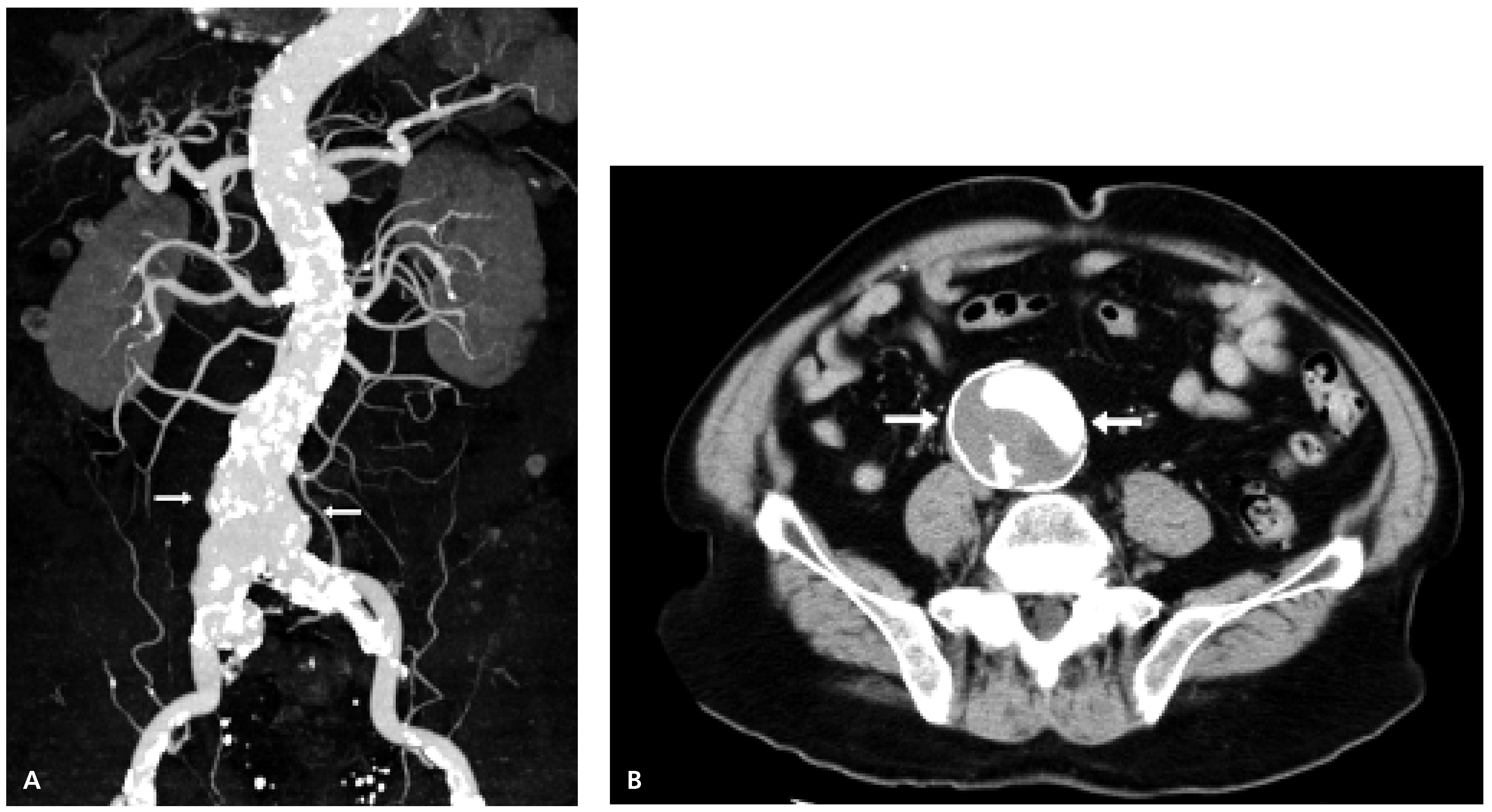
Case Report
Discussion
References
- Hartnell, G.G.; Parnell, B.M.; Pridie, R.B. Coronary artery ectasia—Its prevalence and clinical significance in 4993 patients. Br Heart J 1985, 54, 392–395. [Google Scholar] [CrossRef]
- Markis, J.E.; Joffe, C.D.; Cohn, P.F.; Feen, D.J.; Herman, M.V.; Gorlin, R. Clinical significance of coronary arterial ectasia. Am J Cardiol 1976, 37, 217–222. [Google Scholar] [PubMed]
- Swaye, P.S.; Fisher, L.D.; Litwin, P.; Vignola, P.A.; Judkins, M.P.; Kemp, H.G.; et al. Aneurysmal coronary artery disease. Circulation 1983, 67, 134–138. [Google Scholar] [CrossRef] [PubMed]
- Androulakis, A.E.; Andrikopoulos, G.K.; Kartalis, A.N.; Stougiannos, P.N.; Katsaros, A.A.; Syrogiannidis, D.N.; et al. Relation of coronary artery ectasia to diabetes mellitus. Am J Cardiol 2004, 93, 1165–1167. [Google Scholar] [CrossRef] [PubMed]
- Tilson, M.D. Aortic aneurysm and atherosclerosis. Circulation 1992, 85, 378–379. [Google Scholar] [CrossRef]
- Fine, L.G. Abdominal aortic aneurysm: A report of a meeting of physicians and scientists, University College London Medical School. Lancet 1993, 341, 215–220. [Google Scholar]
- Stajduhar, K.C.; Laird, J.R.; Rogan, K.M.; Wortham, D.C. Coronary arterial ectasia: Increased prevalence in patients with abdominal aortic aneurysm as compared to occlusive atherosclerotic peripheral vascular disease. Am Heart J 1993, 125, 86–92. [Google Scholar] [CrossRef]
- Kishi, K.; Ito, S.; Hiasa, Y. Risk factors and incidence of coronary artery lesions in patients with abdominal aortic aneurysms. Intern Med 1997, 36, 384–388. [Google Scholar]
- Swanton, R.H.; Lea Thomas, M.; Coltart, D.J.; Jenkins, B.S.; WebbPeploe, M.M.; Williams, B.T. Coronary artery ectasia—A variant of occlusive coronary arteriosclerosis. Br Heart J 1978, 40, 393–400. [Google Scholar] [CrossRef]
- Reed, D.; Reed, C.; Stemmermann, G.; Hayashi, T. Are aortic aneurysms caused by atherosclerosis? Circulation 1992, 85, 205–11. [Google Scholar] [CrossRef]
- Tunick, P.A.; Slater, J.; Kronzon, I.; Glassman, E. Acquired coronary arterial aneurysms: An autopsy study of 52 patients. Hum Pathol 1986, 17, 575–583. [Google Scholar]
- Lopez-Candales, A.; Holmes, D.R.; Liao, S.; Scott, M.J.; Wickline, S.A.; Thompson, R.W. Decreased vascular smooth muscle cell density in medial degeneration of human abdominal aortic aneurysms. Am J Pathol. 1997, 150, 993–1007. [Google Scholar]
- Isner, J.M.; Donaldson, R.F.; Fortin, A.H.; Tischler, A.; Clarke, R.H. Attenuation of the media of coronary arteries in advanced atherosclerosis. Am J Cardiol 1986, 58, 937–939. [Google Scholar] [CrossRef]
- Hansson, G.K. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med 2005, 352, 1685–1695. [Google Scholar] [CrossRef]
- Thompson, R.W.; Geraghty, P.J.; Lee, J.K. Abdominal aortic aneurysms: Basic mechanisms and clinical implications. Curr Probl Surg 2002, 39, 110–230. [Google Scholar] [CrossRef]
- Wassef, M.; Baxter, T.; Chisholm, R.L.; Dalman, R.L.; Fillinger, M.F.; et al. Pathogenesis of abdominal aortic aneurysms. J Vasc Surg 2001, 34, 730–738. [Google Scholar] [CrossRef]
- Galis, Z.S.; Khatri, J.J. Matrix metalloproteinases in vascular remodelling and atherogenesis. Circu Res 2002, 90, 251–262. [Google Scholar] [CrossRef]
- Rohde, L.E.; Arroyo, L.H.; Rifai, N.; Creager, M.A.; Libby, P.; Ridker, P.M.; et al. Plasma concentrations of interleukin-6 and abdominal aortic diameter among subjects without aortic dilatation. Arterioscler Thromb Vasc Biol 1999, 19, 1695–1699. [Google Scholar] [CrossRef]
- Tokgozoglu, L.; Ergene, O.; Kinay, O.; Nazli, C.; Hascelik, G.; Hoscan, Y. Plasma interleukin-6 levels are increased in coronary artery ectasia. Acta Cardiol 2004, 59, 515–519. [Google Scholar] [CrossRef]
- Chakrabarti, S.; Thomas, E.; Wright, J.G.C.; Vettukattil, J.J. Congenital coronary artery dilatation. Heart 2003, 89, 595–599. [Google Scholar] [CrossRef]
- Imahori, S.; Bannerman, R.M.; Graf, C.J.; Brennan, J.C. EhlersDanlos Syndrome with multiple arterial lesions. Am J Med 1969, 47, 967–977. [Google Scholar] [CrossRef]
- England, J.F. Herbicides and coronary artery ectasia. M J Aust 1981, 2, 140. [Google Scholar]
- Fischer, M.; Broeckel, U.; Holmer, S.; Baessler, A.; Hengstenberg, C.; Mayer, B.; et al. Distinct heritable patterns of angiographic coronary artery disease in families with myocardial infarction. Circulation 2005, 111, 855–862. [Google Scholar] [CrossRef] [PubMed]
- Baird, P.A.; Sadovnick, A.D.; Yee, I.M.L.; Cole, C.W.; Cole, L. Sibling risks of abdominal aortic aneurysm. Lancet 1995, 346, 601–604. [Google Scholar] [CrossRef] [PubMed]
- Blanchard, J.F.; Armenian, H.K.; Friesen, P.P. Risk factors for abdominal aortic aneurysms: Results of a case-control study. Am J Epidemiol 2000, 151, 575–583. [Google Scholar] [CrossRef]
- Kuzuya, M.; Asai, T.; Kanda, S.; Maeda, K.; Cheng, X.W.; Iguchi, A. Glycation cross-links inhibit matrix metalloproteinase-2 activaton in vascular smooth muscle cells cultured on collagen lattice. Diabetologica 2001, 44, 433–436. [Google Scholar] [CrossRef][Green Version]
- Vavuranakis, M.; Stefanadis, C.; Toutouzas, K.; Pitsavos, C.; Spanos, V.; Toutouzas, P. Impaired compensatory coronary artery enlargement in atherosclerosis contributes contributes to the development of coronary artery stenosis in diabetic patients. An in vivo intracoronary ultrasound study. Eur Heart J 1997, 18, 1090–1094. [Google Scholar][Green Version]
- Sudhir, K.; Ports, T.A.; Amidon, T.M.; Goldberger, J.J.; Bhushan, V.; Kane, J.P.; et al. Coronary heart disease / platelet activation / myocardial infarction: Increased prevalence of coronary ectasia in heterozygous familial hypercholesterolemia. Circulation 1995, 91, 1375–1380. [Google Scholar] [CrossRef]
© 2006 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
von Dahlen, R.; Kiencke, S.; Kaiser, C.; Rickenbacher, P. Severe Coronary Artery Ectasia and Abdominal Aortic Aneurysm. Cardiovasc. Med. 2006, 9, 348. https://doi.org/10.4414/cvm.2006.01199
von Dahlen R, Kiencke S, Kaiser C, Rickenbacher P. Severe Coronary Artery Ectasia and Abdominal Aortic Aneurysm. Cardiovascular Medicine. 2006; 9(10):348. https://doi.org/10.4414/cvm.2006.01199
Chicago/Turabian Stylevon Dahlen, Ruth, Stephanie Kiencke, Christoph Kaiser, and Peter Rickenbacher. 2006. "Severe Coronary Artery Ectasia and Abdominal Aortic Aneurysm" Cardiovascular Medicine 9, no. 10: 348. https://doi.org/10.4414/cvm.2006.01199
APA Stylevon Dahlen, R., Kiencke, S., Kaiser, C., & Rickenbacher, P. (2006). Severe Coronary Artery Ectasia and Abdominal Aortic Aneurysm. Cardiovascular Medicine, 9(10), 348. https://doi.org/10.4414/cvm.2006.01199



